Notes
Article history
The research reported in this issue of the journal was funded by PGfAR as project number RP-PG-1210-12017. The contractual start date was in May 2013. The final report began editorial review in August 2018 and was accepted for publication in September 2020. As the funder, the PGfAR programme agreed the research questions and study designs in advance with the investigators. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PGfAR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2021. This work was produced by Forster et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2021 Queen’s Printer and Controller of HMSO
SYNOPSIS
Parts of this report have also been reproduced from Forster et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY NC) license, which permits others to distribute, remix, adapt and build upon this work, provided the original work is properly cited. See: https://creativecommons.org/licenses/by-nc/4.0/. The text includes minor additions and formatting changes to the original text.
Context and rationale for the programme
Over the past century, there has been a shift in the demographics of the world’s population. 2 There has been a particular expansion of the ≥ 85 years age group (i.e. the oldest old), and this trend is likely to continue as longevity in later life improves. 3 In the UK, the number of individuals belonging to this age group is expected to more than double between 2014 and 2034 to 3.2 million. 4
Although population ageing should be celebrated as one of humanity’s major achievements, the fact that increases in life expectancy are typically mirrored by extended periods of morbidity and disability cannot be overlooked. 5 Many disabling conditions, including cardiovascular diseases, musculoskeletal diseases, and mental and neurological disorders, are age-related. 5 Moreover, the incidence of multimorbidity increases sharply with age. 6,7 As a result, many older adults will experience complex and interacting health needs, and will ultimately require some form of support in their later years. 2 Although policy and service developments have emphasised alternatives to long-term care,8 recent estimates suggest that around one in four older people will spend some time in a care home (CH) in their last year of life. 9 Evidently, the need for such care will persist. 10
Residents of CHs are among the frailest individuals in the population, distinguishable from community-dwelling older adults of the same age because of their physical disability, multimorbidity, dependency on others and cognitive impairment. 11 For these individuals, their dependency and functional impairments will probably compound health difficulties by directly affecting their physical and psychological health, and will reduce opportunities to participate in social activities. Social isolation, in turn, has a negative impact on mood and self-esteem, which can then further adversely affect physical health. 12 Furthermore, the increasing health requirements of this expanding client group places considerable burden on the NHS. 11 Still, frailty may be considered a dynamic process; although it is likely that residents become frailer and are at higher risk of worsening disability, falls and admission to hospital, this deterioration is not immutable and there is scope to intervene. 13 Accordingly, it is important to explore factors that may help slow the progression in functional decline and also maintain or improve quality of life.
One factor known to have a positive impact on the ageing process and to contribute to the maintenance of health with rising age is physical activity (PA),14 defined here as a complex and multidimensional behaviour that involves skeletal muscle contraction and results in increased energy expenditure. 15 There is now a considerable body of evidence concerning the health and social benefits of engaging in PA for older adults. 16–18 With respect to CH residents specifically, engagement in PA has been shown to have favourable effects in terms of physical function19–21 and social engagement. 22 Nonetheless, a prominent finding from research conducted in a CH setting is that residents engage in very little PA and spend the majority of their time sedentary (a separate, albeit related, construct to PA, characterised by minimal movement and very low levels of energy expenditure). 23–25 This is particularly concerning as there is growing evidence (some of which postdates our programme) of the detrimental effect sedentary behaviour may have, independently of engagement in PA, on a number of parameters related to health,26 including cardiovascular risk,27 physical function28,29 and quality of life. 30,31 For CH residents in particular, substantial levels of sedentary behaviour may lead to increased incidence of pressure sores, contractures, cardiovascular deconditioning, urinary infections and loss of independence. 32
In the light of this evidence, we surmised that, for older adults residing in CHs, a recommendation to encourage engagement in PA and reduce sedentary time would be well placed. This is supported by the recent guidance for interpreting the UK PA guidelines,33 which states that frail older adults should strive to engage in some PA every day and minimise the amount of time they spend being sedentary for extended periods. Encouragingly, a Cochrane review34 addressing rehabilitation in long-term care facilities demonstrated that strategies to enhance PA can be implemented in CHs with reported benefits. However, many of the interventions evaluated were dependent on external resources (e.g. therapists) and gains were not sustained. 34
We reviewed the evidence for ways to increase PA in residents that may be of benefit. As part of programme development work, we also undertook observations and conducted interviews with staff and residents in two CHs to inform our understanding of current levels of PA and what might work in practice.
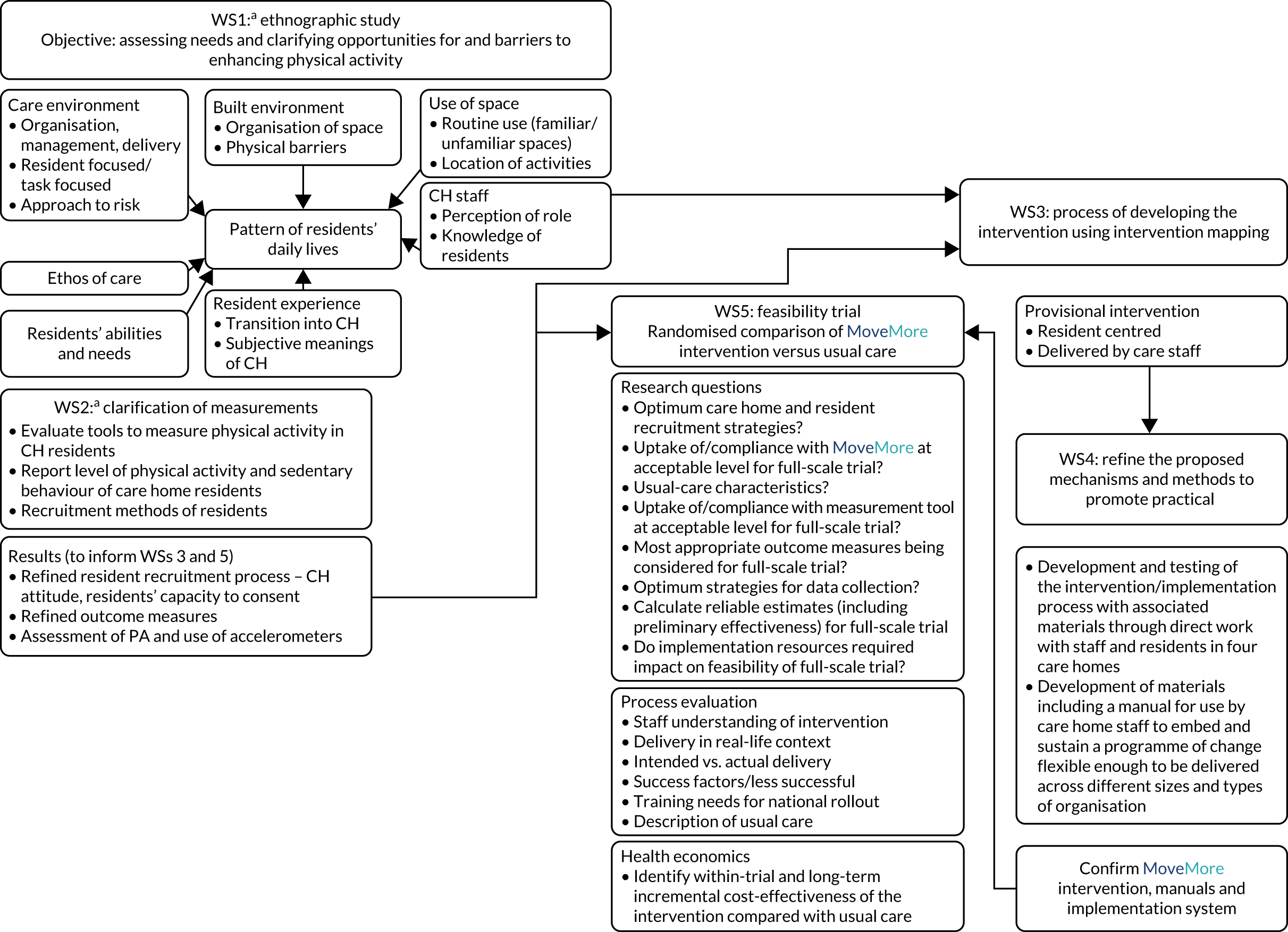
We have undertaken a research programme, delivered through five workstreams (WSs), in which we worked with CH staff and residents to develop and preliminarily test strategies to enhance PA in the daily life routines of CH residents to improve their physical, psychological and social well-being (Figure 1).
FIGURE 1.
Inter-relationship between the different WSs of the programme. a, WSs 1 and 2 were undertaken simultaneously.
Workstream 1: needs assessment and clarifying opportunities for and barriers to enhancing routine physical activity
Aims and objectives
The aim was to explore the potential for developing and delivering an intervention to increase PA in the daily life routines of CH residents, with the objective of assessing needs and clarifying opportunities for and barriers to PA.
Methods for data collection
This WS was implemented in accordance with the grant proposal and employed a mixed-methods research design in four CHs. The WS included three interlinked components:
-
ethnographic work (observations)
-
qualitative interviews with residents, relatives and friends (when appropriate) in each home
-
qualitative interviews with staff in each home.
See the protocol in Report Supplementary Material 1 for details of the data collection methods.
Data were anonymised; names are pseudonyms.
Sampling strategy
Four nursing and residential CHs, differing in size, setting and ownership, were purposively selected in the Bradford area and recruited to participate in WS1 and WS2: Bourneville CH, Eden Park CH, Hebble House and Rowntree Nursing Home.
All four CHs offered residential care (one specialised in dementia care); in addition, two offered nursing care. One was run by the local authority and three were run by private or family companies (one by a national company and one by a large international company). Sizes ranged from 20 to 55 beds. One CH was situated in the inner city; the others were in semi-urban, semi-rural or rural locations. See Appendix 2, Table 14, for full details of the CHs.
Ethnographic work (observations)
An ethnographic approach was adopted to understand how daily life is organised in relation to the resident profile and the physical and social environment within which care is delivered. This combined observation and informant interviewing in a naturalistic setting. Ethnographic work enabled us to further our understanding of potential linkages between CH culture, staff practices and residents’ engagement with different kinds of social and physical activities. A conceptual framework and methods for recording observations had been refined during our previous Programme Development Grant (PDG) work. 35
It was planned for researchers to spend 2 days per week in each home over 4 months. Observations were to include day, evening and weekend periods, to encompass different types of activities at different time points, as well as to facilitate contact with families and friends. 36,37
In the course of the observations, the researcher engaged in informal interviewing/conversation with both residents and staff. We looked to combine these informal interviews with formal interviews (see Qualitative interviews with residents and relatives). Observations, recorded in contemporaneous fieldnotes, focused on events, activities, interactions and conversations with residents, staff and relatives. A chronological fieldwork journal combined descriptive materials with reflective accounts of the meaning of what was observed, as well as hunches and working hypotheses. These included the researcher’s impressions and reactions to the observations.
Observations undertaken during the PDG work identified several emerging categories or preliminary hypotheses. These were explored further through more focused observation.
Particular emphasis was placed on what was typical, as well as what was idiosyncratic, within and between homes, and what distinguished homes that were more or less resident centred in their culture and care practices.
Qualitative interviews with residents and relatives
Formal, semistructured qualitative interviews were undertaken with a sample of residents, their relatives and friends in the four homes. The topic guide allowed for flexibility by allowing researchers to draw on their observations to inform the interviews and to ensure that they were as inclusive as possible. Interviews were conducted, when possible, in quiet private areas, were audio-recorded and were transcribed verbatim.
The aim of the interviews was to clarify the findings from the ethnographic work and to examine options, preferences and choice of (physical) activities, assessing needs as well as opportunities and barriers to their introduction.
Qualitative interviews with staff
A purposively varied sample of staff from each home was selected for interview. We drew on our observational data to identify individuals who played a significant role in the life of the home, including those who may have had experience/knowledge of potential barriers to increasing PA and those who may have been drivers of or barriers to change.
The interviews encompassed knowledge, perspectives and attitudes towards enhancing activities; exploring opportunities for and barriers to active interventions, including perceived benefits and risks; and the contexts in which they might work for residents with different abilities and preferences. In interviews with managers from each home, we additionally explored the current provision of social and exercise opportunities, facilities and the resources available. We also examined and discussed their routine data collection and recording systems.
All researchers were familiar with CH environments, owing to previous research conducted by the team. In addition, all researchers spent a period of time conducting orientation visits to the CHs to familiarise themselves with the care environments of the participating homes.
Data analysis
A modified grounded theory approach to data analysis (using NVivo, version 8, QSR International, Warrington, UK) was employed, using the method of constant comparison38 and iterative engagement with the research literature. The observations were analysed to identify actual and potential opportunities for enhancing activities, and possible opportunities for change.
Themes were identified and coded, and categories were developed. We examined within- and across-group similarities and differences, with a focus on exploring what shaped perceptions and behaviour, and opportunities for and barriers to, PA. The findings from all research participants shed light on those mechanisms or triggers in different care contexts that facilitated a shift in care practices and resident motivation to optimise opportunities for increasing PA/reducing sedentary behaviour in both activities of daily living (ADL) and leisure spaces. Further details are available in Hawkins et al. 39 (2018).
Data collected
Ethnographic observations
Ethnographic observations and ethnographic conversations40,41 were conducted by researchers in communal spaces, as planned, on approximately 2 days per week over approximately 4 months in each home; > 100 observations were undertaken between December 2012 and October 2013. Each session of observation took approximately 4 hours (with some flexibility at the discretion of the researcher, however, for them to sufficiently capture a variety of activities taking place in the CHs). Each researcher was allocated a particular CH (or CHs) in which to conduct their observations, as is standard practice in ethnographic work. Detailed fieldnotes were produced to capture the observations.
Interviews
Towards the end of the period of observation, 55 qualitative interviews were undertaken across the four participating CHs with staff members (n = 22), residents (n = 16) and relatives (n = 17).
Key findings
A number of interacting factors and social processes shaped and sustained the patterns of residents’ daily life and the routinisation of movement in the CH settings (Figure 2). These included the:
-
ethos of care
-
organisation, management and delivery of care
-
individual environment
-
physical environment
-
routine of residents’ daily life.
FIGURE 2.
Illustrative summary of the factors and social processes that shape and sustain the pattern of residents’ daily life.
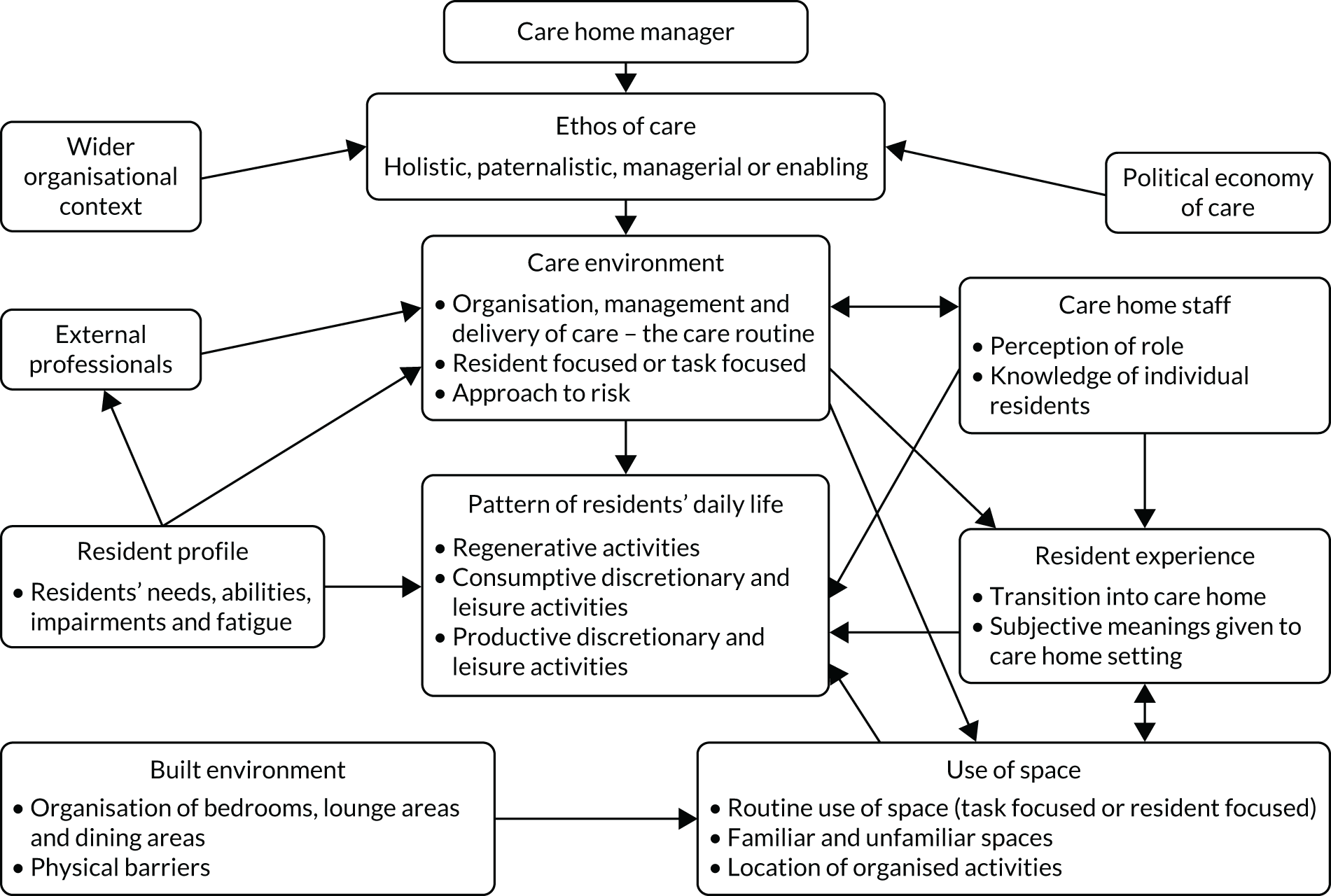
For a rich description of daily life and an in-depth exploration of the findings, see Appendix 1.
This ethnographic work enabled an understanding of the PA undertaken by CH residents in the context of daily routine life. It also allowed for an understanding of ways in which greater PA may be facilitated and provided an indication of the kinds of culturally specific changes that would be required to bring about such developments, given the characteristics of residents’ physical and mental health, as well as the processes by which health and social care services are delivered. A number of barriers to and opportunities for enhancing movement became apparent during the study.
In the organisation, management and delivery of care, the ethos of care shaped opportunities for occupation, PA and movement. If the CH adopted a more enabling or holistic care ethos, this often resulted in greater opportunities for residents to move. The tension between risk management and the promotion of independence, and how this was managed at an organisational level and at the point of care delivery, also had implications for residents’ daily routine, as did whether a resident- or task-focused approach to the delivery of care was facilitated and encouraged. In particular, how care assistants went about monitoring, curtailing and enabling residents’ movement, and whether or not care staff perceived their role to include spending time engaging with residents socially and in activities, was important.
The ability of the management team to translate the often abstract, espoused values of care into tangible care practices and to communicate such practices to care staff was important to residents’ routine movement. It was through the process of translation and communication that decisions were made regarding what was workable and acceptable in practice.
In addition, it was important that senior staff valued any practices arising from these decisions and that any trade-offs potentially arising were acknowledged (e.g. increased time needed for care tasks to enable residents to move more). It seemed especially important to be able to translate abstract values into care practices that promote independence, alongside resolving how these can work in practice, something potentially problematic for vulnerable adults and older people in the context of health and social care. 42,43
The role of formal and informal staff training and supervision in ensuring a consistent approach to care practice and allowing space for reflection and problem-solving is important. Supervision, leadership style, knowledge, skills and a solution-focused approach have been highlighted as important in relation to good-quality care practice in CHs. 44,45
The individual and physical environments were important. The routine use of space was an important factor in the residents’ ADL; how physical space was organised, whether there was a task-based or resident-focused approach to how residents use spaces/where they spent time, whether or not residents were enabled to move around space, and how residents expected each other to behave in semipublic spaces shaped their conduct in such settings.
Another factor was the residents’ familiarity and comfort with the CH space. Moving around the home and/or participating in activities were facilitated by the familiarity of the space, familiar faces and companionship, engaging occupation and activities, and encouragement, reassurance and support from care staff.
The meaning given to the CH setting by residents was also important: the transition of residents into the CH setting, their expectations of the CH and how they were supported to adapt to living in the CH setting shaped their routine. The subjective meanings residents attributed to the setting also shaped how they occupied themselves and moved around the CH.
In the CH daily routine, residents’ daily life created barriers and opportunities. For example, whether or not residents’ participation in occupation and PA was encouraged in a manner that demonstrated knowledge of residents’ abilities, likes or dislikes; whether or not activities were personally meaningful, familiar or had some connection to the life history of the group of residents; and the role that residents were enabled and supported to adopt (and whether that was an active or a passive role), in particular, opportunities for increasing residents’ involvement in domestic-type tasks.
We took steps to ensure the rigour of our data collection and analysis, including keeping detailed fieldwork notes and memos, purposively sampling participants for in-depth observation and interviews, regularly meeting with the research team and study management group, and undertaking collaborative analysis.
Limitation
We were permitted to conduct observations in the communal areas of the CHs only; therefore, we did not directly observe patterns of movement occurring in private spaces (e.g. residents’ bedrooms). However, by supplementing observation data with qualitative interviews, we attempted to address this gap, but we acknowledge that our analysis may have been limited.
Relationship with other parts of the programme
This WS, which encompassed a needs assessment and clarified the opportunities for and barriers to enhancing the PA of CH residents, forms a key component of the intervention mapping (IM) framework [see Workstream 3: development of an intervention to enhance physical activity, and appropriate methods of implementation (e.g. training materials) through a process of intervention mapping], which underpinned intervention development.
Organisational structures and processes are known to shape care practices in CHs. However, the relationship between those structures and practices is nuanced and dynamic. 45 By exploring the structures and processes in-depth, we have highlighted how the management processes, staff training and supervision, and care planning processes shape residents’ movement in care settings. Understanding how organisational factors shape routine movement among residents will inform the development of embedded and sustainable interventions that aim to enhance PA and reduce sedentary behaviour in CH settings.
Workstream 2: clarification of measurements
Aims
The primary aims of WS2 were to review the methods of data collection at the levels of the residents and CHs and to evaluate the methods and tools to measure PA in this population to inform outcome assessment. A secondary aim was to review and assess the method of recruiting CH residents to a research study. The intent was to inform the processes for the feasibility trial in WS5.
Methods/design
The study was divided into two phases:
-
Phase 1 – to explore the methods and content of routinely collecting data in CHs and to explore the appropriateness of different questionnaire assessments of physical function and mobility in a CH population.
-
Phase 2 – to explore different methods of measuring PA and sedentary behaviour in older CH residents. Phase 2 comprised three parts:
-
an observational study to assess the criterion validity of estimates of PA and sedentary time derived from hip- and wrist-worn accelerometers in largely inactive CH residents
-
the feasibility of assessing the PA and sedentary behaviour of CH residents over an extended period using the ActiGraph (ActiGraph, LLC, Pensacola, FL, USA) accelerometer
-
evaluation of the Assessment of Physical Activity in Frail Older People (APAFOP) questionnaire. 46
-
Recruitment of care homes
Care homes were purposively selected for both WS1 and WS2 (see Workstream 1: needs assessment and clarifying opportunities for and barriers to enhancing routine physical activity).
Recruitment of residents
We undertook a range of activities in the CHs to enhance recruitment, including attending staff and residents’ meetings, hosting a coffee morning to meet relatives/friends of residents and attending ‘open days’ in the home(s). All residents were screened for eligibility. Residents were excluded if they were acutely unwell, bedbound, receiving end-of-life care or if, in the opinion of the CH manager, they may have found the research distressing.
Recruitment procedures
For a full description of recruitment procedures, see the WS2 protocol in Report Supplementary Material 1.
Residents were approached for participation in the study by a research assistant if, in the opinion of the CH manager, the residents had the mental capacity to consent. Capacity to consent was confirmed by the researcher. Signed and dated consent (or witnessed verbal consent, if necessary) was obtained from residents wishing to participate. Personal consultees (PCs) of residents without capacity to consent were approached by letter about participation in the study. A consultee declaration form was provided for response. Nominated consultees were not used in this WS.
Methods for data collection and data analysis
For a full description of the methods for data collection and analysis, see the study protocol in Report Supplementary Material 1, and the WS2 report in Appendix 2, Data collection and Data analysis.
Data were assessed for normality; analyses varied depending on the data collected. Parametric and non-parametric statistics were employed, depending on the distribution of the data.
For ease of reference, we present the results of CH recruitment, resident recruitment and participant characteristics, before describing details of each phase of the study.
Care home and resident recruitment, and participant characteristics
Care home recruitment
As reported in Workstream 1: needs assessment and clarifying opportunities for and barriers to enhancing routine physical activity, four CHs were selected to participate in WSs 1 and 2. An additional two CHs were recruited in November 2013 for WS2 to assess the appropriateness of PA measures, as resident recruitment was lower than anticipated in the four CHs originally recruited. See Appendix 2, Table 14, for details of the CHs.
Resident recruitment
Of the 220 residents across the six CHs, 151 (69%) were eligible. Of these, 49 (32%) residents consented or had PC declaration, and 46 participated in the study (two residents died and one resident withdrew consent before/during data collection) (see Appendix 2, Recruitment of participants).
Participant characteristics
Sixty-seven per cent of participants were female; 55% were aged ≥ 85 years. Participants had resided in the CH for a median of 15 months. More than 40% had a diagnosis of dementia; more than one-third had fallen in the previous 6 months (see Appendix 2, Participant characteristics).
Phase 1: methods of routinely collecting data, and function and mobility questionnaires
Methods
The research team collected personal health data for residents participating in the study and explored the feasibility of using a range of tools designed to assess mobility and other outcomes. Specifically, these tools were as follows:
-
cognitive impairment – Six-item Cognitive Impairment Test (6-CIT)47
-
physical function –
Analysis
Descriptive statistics were used to describe outcomes. Participants were grouped according to age (< and ≥ 85 years), sex (male/female), functional walking ability (non-ambulatory, low ability, medium ability, high ability) and function (BI score of ≤ 11: dependence in ADL; BI score of ≥ 12: independence in ADL). 51 Differences between groups were examined using independent t-tests or Mann–Whitney U-tests. Alpha was accepted as a p-value of < 0.05.
Phase 2: assessment of physical activity and sedentary behaviour
Methods
The aim of this phase was to explore the feasibility of different methods of measuring PA and sedentary behaviour in older CH residents.
Part 1: observation of physical activity
The aims were to:
-
use the observations of residents’ activities as a reference to compare with the data captured by accelerometers to assess the validity of using accelerometers in a frail, elderly and largely inactive population
-
identify whether hip- or wrist-worn accelerometers were the most accurate in recording activities that CH residents typically engage in.
The ActiGraph GT3X and GT3X+ (ActiGraph, LLC) models, previously chosen in the PDG work,35 were used. Accelerometers are a direct and valid assessment of PA. At the suggestion of a reviewer, we also investigated the feasibility of a newer accelerometer, the GeneActiv (Activinsights Ltd, Kimbolton, UK).
Residents who had been recruited to WS2 were approached and asked if they would be prepared to participate in the observational study. Residents were invited to wear a hip- or wrist-worn accelerometer over a 2-hour ‘free-living’ period while being observed by the researcher.
The researcher used a predetermined list of activities to systematically record what the observed residents were doing every 15 seconds over the monitoring period. The list of activities included both PA and sedentary behaviours believed to be typical of CH residents.
Part 2: utilisation of accelerometers to assess physical activity over extended periods
The aims were to:
-
investigate both the feasibility of using accelerometers and the appropriateness of the wear criteria of at least 8 hours per day on at least 4 days52,53 in this population
-
describe the levels of PA and sedentary behaviour.
All recruited residents in the participating CHs were invited to wear a hip- or wrist-worn accelerometer for a period of up to 10 days while they continued with their usual routine. For all residents, it was required that a daily log of the time the accelerometer was put on and removed (i.e. wear time) was kept for the duration of the monitoring period. Staff were asked to assist by completing the log when residents were not able to complete it themselves. However, on collecting the first accelerometers, it became apparent that activity logs were not being completed. This, coupled with the largely sedentary profile of participants’ behaviour, made distinguishing actual wear time from non-wear time difficult. Consequently, as the study progressed, a more pragmatic approach was instituted:
-
Residents were asked to wear the accelerometers for as long as they were comfortable doing so. Sometimes this was taken on a day-by-day basis, with continuous support from the researcher (in assisting with administering the accelerometers and completing the activity logs during frequent visits to the home).
-
Accelerometers were collected once it was indicated that there was 5–7 days of data (not necessarily consecutive), or when residents indicated that they no longer wanted to wear the monitor.
Analysis
Observational study of physical activity
Raw activity count data were downloaded and reintegrated into 15-second epochs using appropriate ActiLife software 6.8.0 (ActiGraph, LLC) to allow for comparison with the observational pro forma data. Accelerometer data and observational data were categorised as either PA or sedentary behaviour. The agreement between the categorisation of PA and sedentary behaviour derived from the observational data and that derived from the accelerometer data was evaluated. Specifically, sensitivity, predictive value (PV), overall agreement and the kappa statistic were calculated.
Feasibility study: utilisation of accelerometers to assess physical activity over extended periods
Raw activity count data collected by the accelerometers were downloaded and reintegrated into 60-second epochs prior to analysis. Daily wear time of the accelerometers was determined, and the time spent engaged in, and the number and duration of ‘bouts’ of, PA and sedentary behaviour were calculated.
Part 3: the Assessment of Physical Activity in Frail Older People
The APAFOP is a PA questionnaire purposely developed for and tested for reliability with older people with and without cognitive impairment. 46 It is based on considerable development work, including a systematic review54 and robust psychometric testing. It is administered verbally by a researcher; the interviewee is asked to recall activities undertaken in the previous 24 hours, with a focus on ADL, making it potentially suitable for our work. 55 Although direct assessment of movement is not possible using this instrument, time spent in PA of differing metabolic-equivalent categories can be calculated. The instrument thus offers a more global assessment of habitual PA, which might have generic value for CHs once the efficacy of the whole-home intervention has been established. We explored content and face validity with CH residents.
Key findings
For a full description of the findings, see Appendix 2, Results.
Resident recruitment and participation
In anticipation of subsequently developing a ‘whole-home’ intervention, an inclusive approach to resident recruitment was adopted, with few exclusion criteria. In spite of this, only 49 (22.3%) of the 220 residents in the participating CHs were recruited: a lower rate than our provisional estimate of 80 recruited residents (20 per CH).
Over half of eligible residents did not have mental capacity confirmed by researchers. PC agreement was therefore sought for 75 residents (eight residents declined the approach to their PC). Twenty-two (29.3%) of the 75 PCs did not respond. Nominated consultees (NCs) were not used in the study because one of the CH managers objected to this approach, resulting in a loss of potential residents for recruitment. This influenced our approach to the feasibility trial in WS5, for which we adopted a number of strategies to enhance recruitment. This included:
-
encouraging CH managers to speak to as many relatives as possible in person about the study, prior to sending out information
-
ensuring that the research team was approachable and available, should relatives have any queries
-
attending resident/relative meetings and meetings for staff to increase awareness of the research
-
offering reassurance to CH managers regarding the process of consulting a NC.
Phase 1: outcome measures
The 6-CIT was attempted by 36 (78.3%) of the 46 residents participating in the study. Of these, five residents were able to complete the scale only partially. Twenty-two participants scored ≥ 8 points, indicating significant cognitive impairment. The measure provided indications of the level of cognitive impairment of the resident population. A review of alternative measures did not identify any that were more appropriate. We therefore included the 6-CIT in the data collection for the main trial.
The BI, the PAM-RC and functional walking ability were completed in conjunction with CH staff for all participants. There were only small differences between mobility assessment scores according to age and sex. According to the functional walking ability questionnaire, 12 (26.1%) residents were categorised as non-ambulatory, three (6.5%) were categorised as having a low level of ability, 12 (26.1%) were categorised as having a medium level of ability and 19 (41.3%) were categorised as having a high level of ability.
Staff reported that completing the BI, the PAM-RC and functional walking ability questionnaire was not onerous; this was reflected in the high completion rates. Proxy completion of the BI has been recommended as more valid than self-completion in older and cognitively impaired populations. 56 The PAM-RC is a relatively new scale, with little evidence yet for its use in research. However, it has face validity for this population and has been reported to have excellent test–retest reliability, internal consistency and good construct validity (Dr Julie Whitney, personal communication). The functional walking ability questionnaire was based on the FAC. 50 For this study, it was felt that the functional walking ability questionnaire was more accessible for CH staff. However, going forward to the feasibility trial in WS5, it was decided to use the full FAC to allow comparability with existing research.
Phase 2: assessment of physical activity
Part 1: observation of physical activity during a 2-hour ‘free-living’ period
Twelve observations of nine residents wearing accelerometers on the hip (n = 7), wrist (n = 4) or both hip and wrist (n = 1) were completed. Unfortunately, owing to a malfunction of the monitors, data for two of the accelerometers worn on the wrist were not available. A total of 19 hours and 45 minutes of resident activity data (mean 1 hour and 48 minutes per participant) were available for analysis.
Sensitivity for sedentary time and PV for PA time were higher for the hip counts than for the wrist counts (Table 1). Conversely, the sensitivity for PA time and PV for sedentary behaviour were higher for the wrist counts than for the hip counts. Overall agreement was better for the hip data than for those collected by the wrist-worn accelerometer. The kappa statistic indicated that the agreement for hip counts was moderate (0.47), whereas the agreement for the wrist counts was slight (0.08). 57
| Metric assessed | Accelerometer | |
|---|---|---|
| Hip (n = 8) | Wrist (n = 3) | |
| Sensitivity | ||
| PA time (%) | 42.22 | 64.63 |
| Sedentary time (%) | 96.93 | 63.25 |
| PV | ||
| PA time (%) | 75.57 | 10.29 |
| Sedentary time (%) | 88.18 | 96.48 |
| Overall agreement (%) | 86.56 | 62.92 |
| Kappa statistic | 0.47 | 0.08 |
Although the sensitivity for PA and the PV for sedentary behaviour was higher for the wrist than for the hip counts, all of the other measures used to assess criterion validity suggested that the hip counts were superior to the wrist counts. Indeed, both the overall agreement and the kappa statistic indicated that the classification agreement was considerably better when using the hip counts than when using the wrist counts. Thus, despite the suggestion that a wrist-worn accelerometer may provide more valid estimates of PA and sedentary behaviour than those derived from a hip-worn monitor in older CH residents, the results suggest that the hip remains the preferred wear location when using accelerometers in this population. However, these results must be treated with some caution because of the limited sample size.
Part 2: feasibility study – utilisation of accelerometers to assess physical activity over extended periods
Accelerometer wear time
Extended wear of accelerometers by residents was high: 41 (89.1%) of the 46 recruited residents undertook extended wear of an accelerometer. Thirty (73.2%) wore the accelerometer on the hip, 10 (24.4%) wore the accelerometer on the wrist and one resident was asked to wear a commercially available device so that we could explore the data collected by this device. Unfortunately, there are no published cut-off points validated in older adults for wrist monitor wear; thus, the data for wrist accelerometers were not subsequently analysed. In addition, the outcomes of the commercially available device were based on distance moved; therefore, we decided that these data were unlikely to be sufficiently accurate for our purposes in this population.
Twenty-two (73.3%) of the 30 residents wearing a hip accelerometer had valid data (≥ 8 hours on ≥ 4 days of the week) and wore the accelerometers for a mean of 6 days (range 4–9 days). The mean wear time per day was 12 hours 24 minutes [standard deviation (SD) 2 hours 36 minutes] (Table 2).
| CH | Resident data sets (n) | Daily wear time, mean (SD) |
|---|---|---|
| 2 | 5 | 12 h 33 min (2 h 34 min) |
| 3 | 1 | 15 h 50 min (2 h 7 min) |
| 4 | 2 | 11 h 31 min (2 h 28 min) |
| 5 | 10 | 11 h 40 min (2 h 11 min) |
| 6 | 4 | 13 h 14 min (2 h 36 min) |
| Total | 22 | 12 h 24 min (2 h 36 min) |
The proportion of residents meeting the criteria for valid wear time (73.3%) was lower than that found in the development work (84.8%). This may, however, be attributed to differences in participant characteristics, for example inclusion of those deemed to lack capacity in this study. Enabling residents with cognitive impairment to wear monitors may have required greater support from staff; this may not have been prioritised by staff, given their heavy workloads. Furthermore, over half of the potential participants (10/19, 52.6%) in the development work declined to take part in the study because they did not wish to wear an accelerometer for an extended time (5 days were needed for data to be considered valid). It may have been that those who did wear an accelerometer were not representative of a CH population.
Compared with more recent studies conducted in long-term care settings that have employed similar criteria to define valid wear time, a similar or greater proportion of residents in the current study had valid data. 23,58,59
Activity logs
Correct identification of accelerometer wear time is imperative to ensure that accelerometer data are interpreted and analysed correctly. 60 Although different methods of identifying accelerometer non-wear are used in the literature, automated algorithms and activity logs are the most common. However, both methods present limitations. Automated algorithms have not been developed with this population specifically, and, on examination of the first sets of data collected, it was apparent that sedentary time may be mistakenly categorised as non-wear time, thus underestimating wear time and incorrectly categorising sedentary time as non-wear time. Consequently, although it was acknowledged that completion of activity logs may be viewed as burdensome, much emphasis was placed on attempting to collect accurate information about accelerometer wear using an activity log.
Accordingly, activity logs were administered in a way in which the CH managers felt would result in the greatest success. Nevertheless, completion was poor and appeared onerous for staff, even after they were asked principally to record the times of administration and removal of the monitor, and advised that recording reasons for removal were optional.
Eight (19.5%) of the activity logs were fully completed for the time accelerometers were in the residents’ possession, 20 (48.8%) were partially completed and 13 (31.7%) were not completed at all. Only three (10.7%) of the logs were completed by residents; 12 (42.9%) were completed by CH staff with the assistance of the researcher and 13 (46.4%) were completed by the reseacher alone.
Given the importance of collecting accurate wear time information in this population, the activity log was amended. The amended activity log, in addition to strategies proposed to encourage completion, was to be trialled and further refined, if necessary, in WS4 prior to their use in WS5, the feasibility trial.
Levels of physical activity and sedentary behaviour
Mean daily time spent in engaging in PA was 1 hour 13 minutes (SD 1 hour 8 minutes) (Table 3), which equated to 9.5% (SD 8.3%) of accelerometer wear time (Figure 3).
| CH | Data sets (n) | Time, mean (SD) | ||||
|---|---|---|---|---|---|---|
| Sedentary | Low-intensity PA | Light-intensity PA | Moderate- to vigorous-intensity PA | Combined total PA categories | ||
| 2 | 5 | 11 h 17 min (3 h 1 min) | 1 h 12 min (1 h 00 min) | 0 h 4 min (0 h 5 min) | Negligible (–) | 1 h 16 min (1 h 3 min) |
| 3 | 1 | 13 h 0 min (1 h 51 min) | 2 h 38 min (0 h 54 min) | 0 h 12 min (0 h 7 min) | Negligible (–) | 2 h 50 min (0 h 59 min) |
| 4 | 2 | 10 h 24 min (2 h 13 min) | 1 h 0 min (0 h 43 min) | 0 h 6 min (0 h 7 min) | 0 h 1 min (0 h 1 min) | 1 h 7 min (0 h 50 min) |
| 5 | 10 | 10 h 54 min (2 h 7 min) | 0 h 41 min (0 h 37 min) | 0 h 5 min (0 h 8 min) | 0 h 1 min (0 h 2 min) | 0 h 46 min (0 h 44 min) |
| 6 | 4 | 11 h 33 min (1 h 50 min) | 1 h 36 min (1 h 30 min) | 0 h 5 min (0 h 5 min) | Negligible (–) | 1 h 41 min (1 h 31 min) |
| Total | 22 | 11 h 11 min (2 h 21 min) | 1 h 7 min (1 h 04 min) | 0 h 5 min (0 h 7 min) | 0 h 1 min (0 h 1 min) | 1 h 13 min (1 h 8 min) |
FIGURE 3.
Proportion of daily wear time spent sedentary and in combined low, light and moderate to vigorous PA levels in each individual CH and, on average, across all CHs (n = 22). SB, sedentary behaviour.
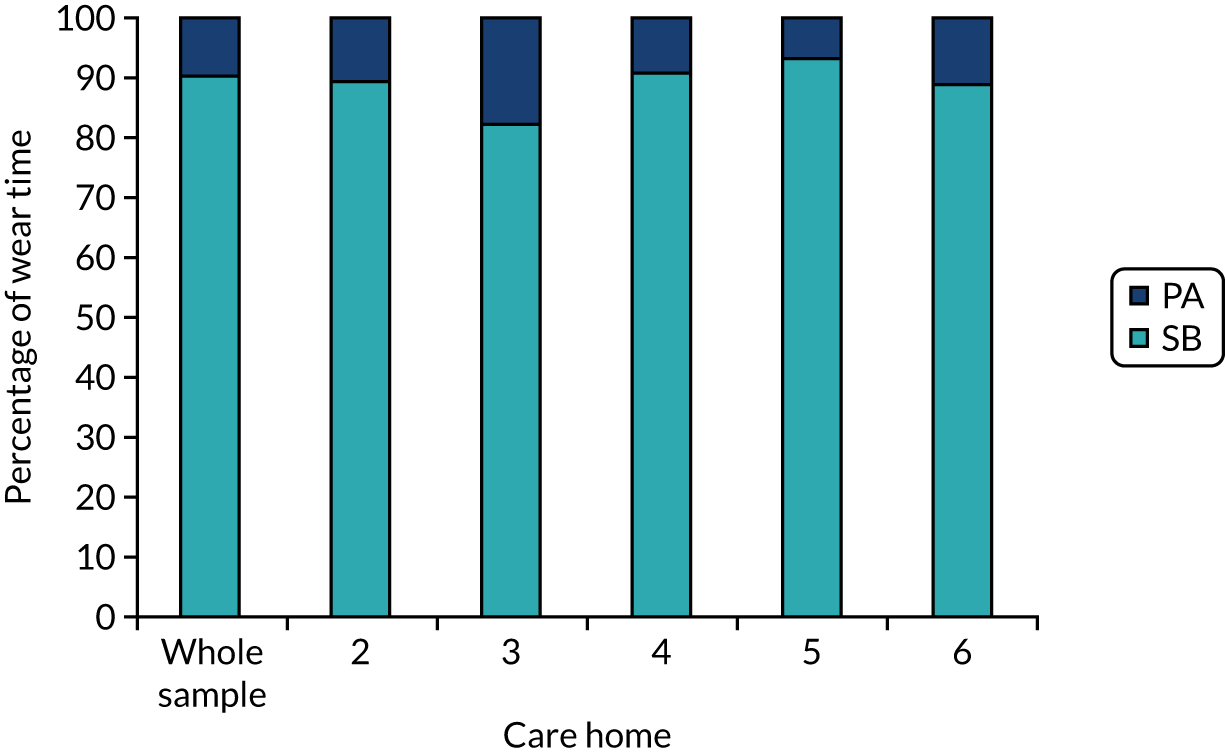
The majority of the time spent in PA was spent in low-intensity PA [1 hour 7 minutes (SD 1 hour 4 minutes); 8.7% (SD 7.7%) of wear time].
Patterns of physical activity and sedentary behaviour
Residents spent the majority of their time engaging in sedentary behaviours, and the little PA they did engage in was predominantly of low intensity (Figure 4).
FIGURE 4.
The proportion of accelerometer wear time residents (n = 22) spent engaging in PA of differing intensities and in sedentary behaviour.
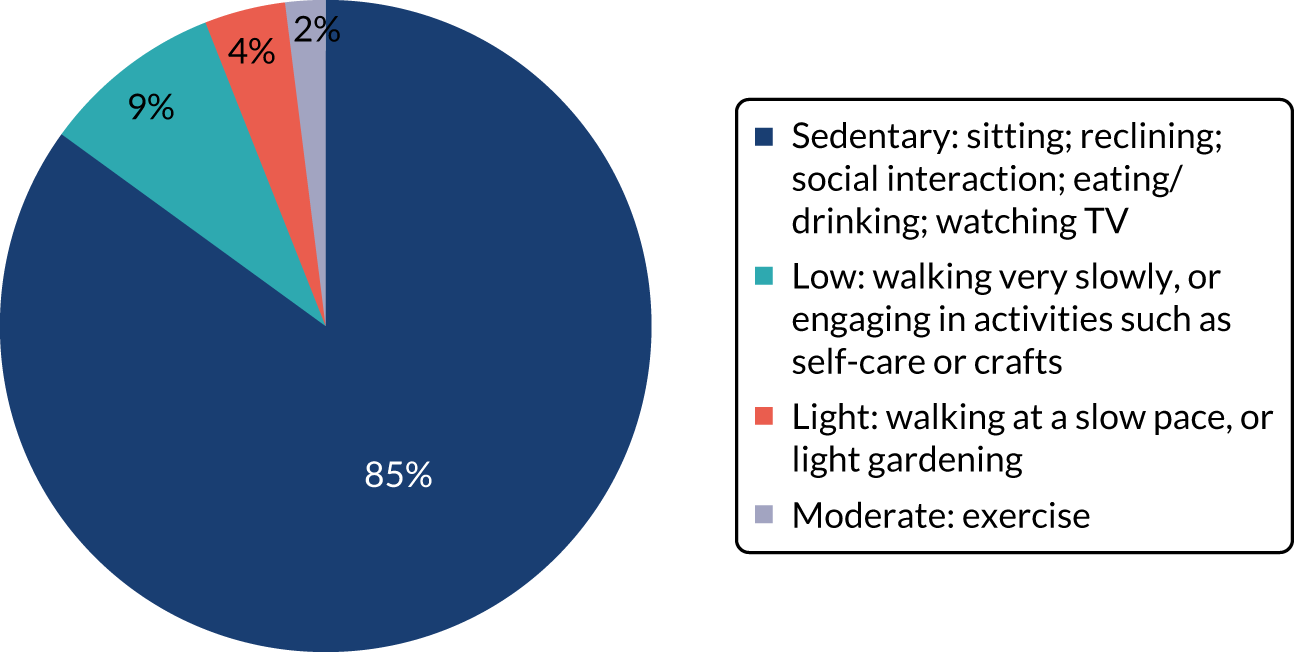
Two typical patterns of activity were apparent among residents:
-
Residents spent the majority of their time sedentary; the little PA engaged in was associated with self-care activities (getting out of bed and dressed in the morning and getting ready for bed in the evening) (Figure 5).
-
Residents engaged in more PA throughout the day and actually managed to accumulate continuous ‘bouts’ of low-intensity PA. Based on observational data, the main form of regular movement observed in all the CHs generally involved accessing the toilet or moving to a different location for meals/organised activities (Figure 6).
FIGURE 5.
The PA level of a resident in CH5 throughout the day, as demonstrated by accelerometer cpm: pattern of activity type 1. This resident was a 72-year-old male who was categorised as non-ambulatory (functional walking ability score = 0) and dependent in ADL (BI score = 7). cpm, counts per minute; LPA, light physical activity; LoPA, low physical activity; SB, sedentary behaviour.
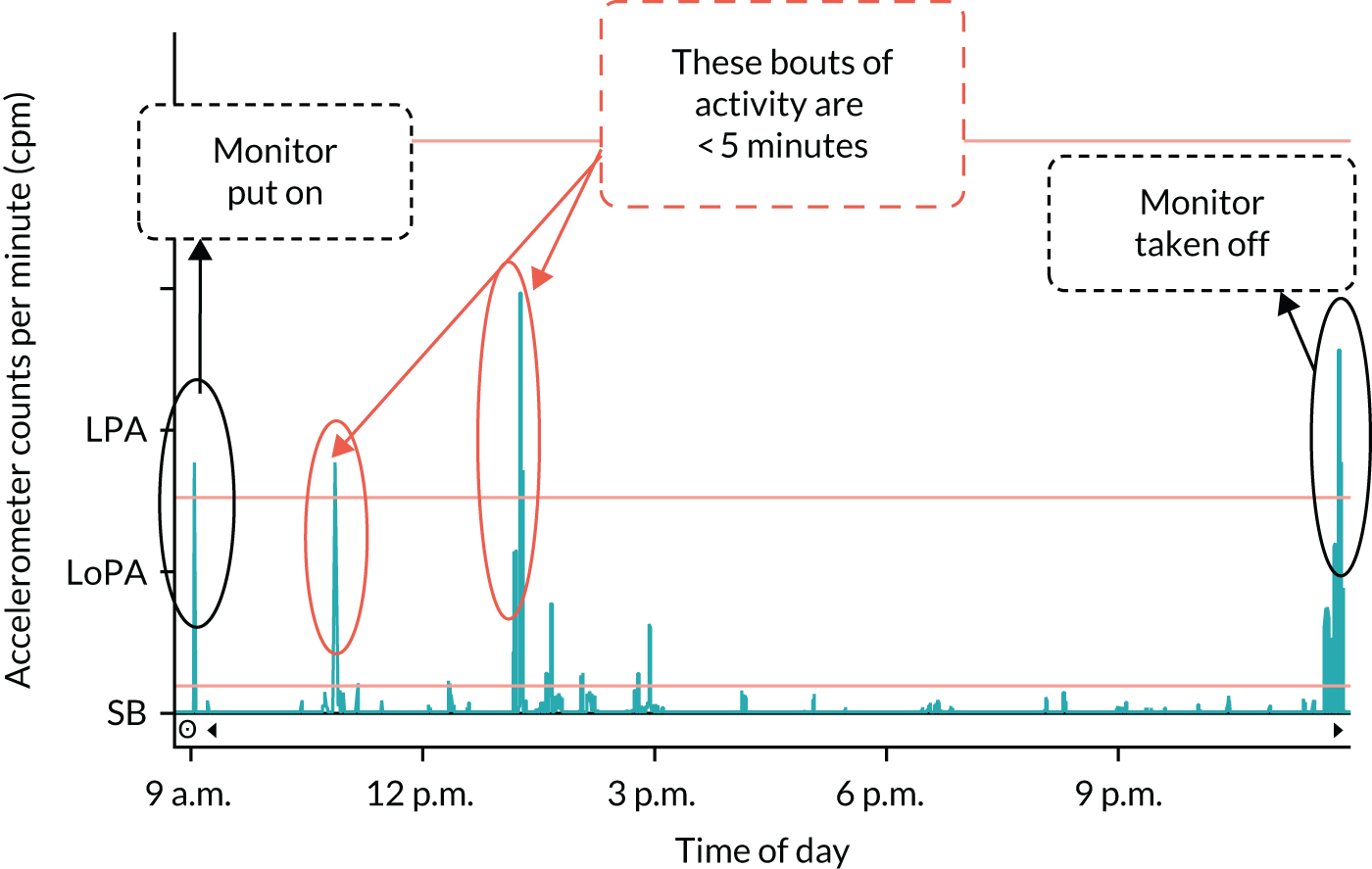
FIGURE 6.
The PA level of a resident in CH5 throughout the day, as demonstrated by accelerometer cpm: pattern of activity type 2. This resident was a 74-year-old female who was categorised as able to ambulate independently (functional walking ability score = 3) and independent in ADL (BI score = 15). cpm, counts per minute; LPA, light physical activity; LoPA, low physical activity; SB, sedentary behaviour.
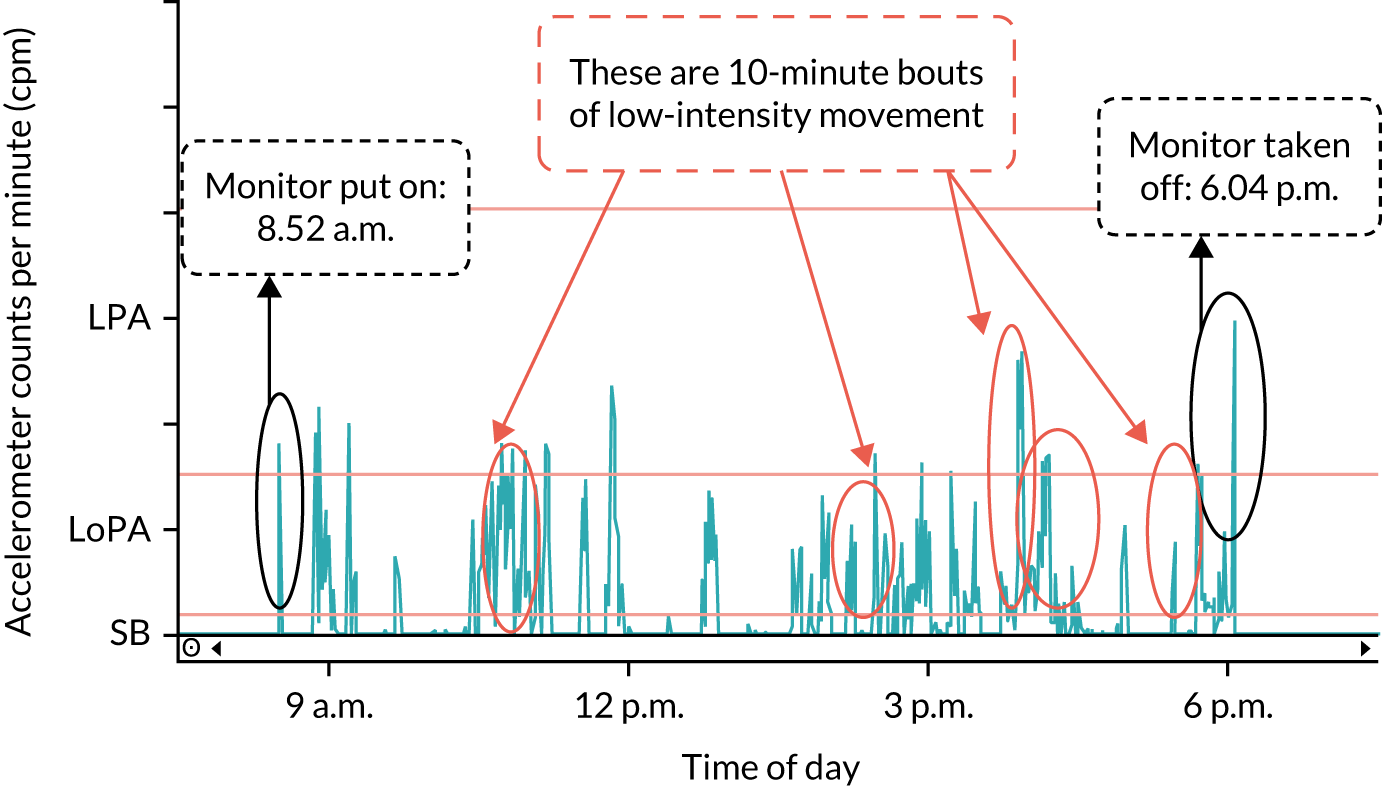
Initially, it would appear, therefore, that the conclusions from the initial development work still hold, namely that there are two key opportunities to increase PA in CH residents:
-
break up long sedentary periods with activity
-
increase the duration of bouts of PA towards a goal of 10-minute bouts of low to light activity and, finally, to an accumulation of 20–30 minutes of low to light PA on 5 days per week, as per guidance for interpreting the UK physical activity guidelines for frailer older people. 33
In addition, we have identified that there is opportunity to increase bouts of low-intensity activity.
Part 3: the Assessment of Physical Activity in Frail Older People
Unfortunately, the manual to implement the APAFOP46 was not available initially. After receiving it, we had concerns about the feasibility of administering the APAFOP and its validity in a population with high levels of cognitive impairment. We therefore decided to undertake a small feasibility assessment of the use of the APAFOP. The APAFOP was trialled in two purposively selected residents in one CH who had relatively strong capacity. Although administering the APAFOP was relatively straightforward with residents deemed to have capacity, questionnaire assessment of PA is unlikely to be feasible in residents with more severe cognitive impairment, as there would be issues relating to recall. Little walking or activities of any form were recorded. Both residents spent the majority of their time engaged in typically sedentary activities (sitting or lying). The sensitivity to change of the APAFOP in a population of CH residents was also questioned. Our observational work suggests that CH residents spend a considerable proportion of their time sedentary and the little PA they do engage in encompasses activities such as ADLs, which are unlikely to increase energy expenditure substantially. Thus, in the light of these limitations and following discussion among the applicant team, the APAFOP was considered to be unsuitable for our purpose.
Relationship with other parts of the programme
We optimised recruitment procedures going forward to subsequent WSs, including approaching appropriate NCs when there was no response from PCs.
We concluded that the 6-CIT, the BI, the PAM-RC and the FAC were suitable and feasible measures of physical function/mobility in this CH population.
The hip remains the preferred wear location when using accelerometers in this population group, and was used in subsequent WSs.
In the light of this, a more structured approach to the accelerometer data collection procedures was proposed for use in future WSs.
Accelerometers were to be administered more systematically (i.e. in batches) whenever possible, and the level of support for CH staff when assisting with accelerometers would be increased. This included a member from the research team visiting or telephoning the CH periodically (the frequency of visits/contacts based on perceived need) over the measurement period. In addition, it was decided to produce and provide a list of participants wearing an accelerometer and ‘reminder posters’ for CH staff to display prominently in the CH. The activity log was also amended in an attempt to make it less burdensome to complete and to ensure that accurate information around wear time was recorded.
Workstream 3: development of an intervention to enhance physical activity and appropriate methods of implementation (e.g. training materials) through a process of intervention mapping
Background: context and theoretical framework
Work undertaken in WSs 1 and 2 demonstrated that CH residents undertake little PA and spend many hours sedentary (see Figure 4). Activities organised in CHs are often not necessarily in line with residents’ wishes, setting up a cycle of low participation, reduction in activities organised and dissatisfaction for both staff and residents. Our work identified unmet needs and barriers to increasing PA, and indicated that there are opportunities to enhance residents’ movement within the daily routines of CHs.
Early WSs had highlighted the importance of PA for not only physical health, but also more general well-being. Encouraging residents to be more active could deliver benefits in terms of physical and psychological health and quality of life, as well as providing potential cost savings in health and social care. We identified a need for simple, practical strategies that could be used by care staff to increase residents’ movement throughout the day, without adding to existing workload, and for an effective implementation plan, which can be adapted to different types of CHs.
Given the number of different providers of CHs, the varied and multifactorial needs of residents, and the effect of a lack of PA/too much sedentary behaviour on health-related quality of life, interventions designed to address the needs of residents are likely to be complex and to involve multilevel strategies to produce system and individual changes that will improve outcomes. We undertook development and implementation of this complex intervention, in the context of the Medical Research Council’s framework for developing and evaluating complex interventions,61 guided by IM. 62 IM offers a systematic approach to the development of health interventions that target individual behaviour and environmental and organisational changes. Using this approach ensured that components of our intervention were based on research evidence, were shaped by expressed views of residents, relatives and staff, and were tailored to the CH environment.
The intent was to design an intervention to be delivered by CH staff that was sufficiently flexible to facilitate the participation of individuals with the range of physical and mental health care needs that form the population of CHs.
Aims
The aim was to develop an intervention to enhance the PA of residents in CHs and to develop appropriate methods of implementation (e.g. training materials) through a process of IM.
Method: intervention mapping
We used the IM framework62 to provide a systematic framework for identifying the components of an evidence-based complex intervention to enhance routine PA in residents of CHs for older people.
Advisory group
A stakeholder advisory group was convened to provide guidance through the IM process, especially in relation to the feasibility of this complex intervention in terms of successful implementation and acceptability to residents and staff. The advisory group consisted of CH managers/owners, activity co-ordinators who were also care assistants and residents, lay members, a physiotherapist and members of the research team. This group met on a regular basis (four meetings of all members, interspersed with six internal, small group meetings) to discuss specific issues with and through the IM structured process, and to consider changes that needed to happen to integrate PA (increased movement) and decrease sedentary behaviour in CH culture, systems and daily routines.
Intervention mapping
The IM protocol is a stepwise method to develop interventions systematically using relevant theory and evidence. 62 It enables specific behavioural change objectives to be targeted and decisions to be made regarding how to achieve changes, using behaviour change strategies that are most likely to effect the desired outcomes.
The IM process involved a number of defined steps. 62 We implemented the first four steps in the development of our intervention:
-
needs assessment
-
definition of the performance objectives, selection of behavioural determinants and definition of matrices of change objectives
-
selection of methods and behaviour change strategies
-
translation of these into an actual intervention programme.
These steps guided the schedule for the advisory group meetings (see Report Supplementary Material 2).
Needs assessment (workstream 1)
The intervention development process began in WS1, with a needs assessment undertaken through ethnographic work in four CHs (see Workstream 1: needs assessment and clarifying opportunities for and barriers to enhancing routine physical activity). This work provided insights into daily life in CHs (see Figure 2).
A number of consistent themes emerged from the needs assessment that guided the process of IM (see Figure 2):
-
The ethos of care shaped the opportunities for occupation, activity and movement.
-
If the CH adopted a more enabling or holistic approach to care, this often resulted in greater opportunities for movement.
-
-
The approach taken to risk had implications for daily routine.
-
How the tension between protecting residents from harm and promoting their independence was managed had implications for residents, including whether or not they were enabled to move around the home.
-
-
The care assistant role.
-
If care staff perceived interacting with and engaging residents in occupation to be an important part of their role, this led to greater opportunities for movement.
-
-
Residents’ experiences of the CH setting shaped their daily routine.
-
Residents attributed meanings to the setting and had different expectations of CH life
-
Residents’ daily routines were distinct if they established meaningful and active roles in the CH.
-
We also consulted the literature, which provided information about good practice and barriers to and facilitators of behaviour change.
Identification of outcomes, performance objectives and selection of determinants
Identification of outcomes and performance objectives
The target outcome was to enhance the PA levels of residents in CHs by embedding increased movement into the daily routine care of the home. The starting point for this was to produce an initial list of opportunities for and barriers to movement for residents in CHs using information collected from the ethnographic observations and interviews (see Appendix 3). To achieve our overall outcome, a number of subobjectives were identified; such objectives included increasing participation in ADL, making better use of time between meals and making more use of outdoor space.
The subobjectives were formally developed into a list of proximal performance objectives in consultation with the advisory group. The list of performance objectives targeted manager(s)/organisation, staff and residents (see Appendix 4). This list was essentially a checklist of ‘what needs to happen’ to achieve the target outcome: that ‘each resident can achieve their potential for movement (for the benefit of physical health and well-being)?’. Each performance objective was informed by our previous work and was refined and validated by the advisory group through an iterative process, involving constant comparison to existing CH practices and initiatives, regularly considering the feasibility of the objective. In parallel with the meetings of the advisory group of key stakeholders, we also convened an internal group of researchers who moved the agenda forward outside these meetings. This included referring to a comprehensive review of associated literature, referring to outcomes from previous studies, and consulting current toolkits and national recommendations related to increasing PA in CHs.
Selection of determinants
The next step in the IM process was to identify the theoretical methods and practical steps required to achieve each of the performance objectives. This involved the identification of ‘change objectives’ through the mapping of each of the performance objectives onto a set of theoretical determinants. We drew on Michie et al. ’s63 framework, consisting of 11 theoretical domains pertaining to determinants of behaviour change. Determinants are personal and external factors that may influence outcomes, and include the following.
List 1: explanatory determinants
-
Knowledge.
-
Environmental context and resources.
-
Motivation and goals (intention).
-
Beliefs about capabilities (self-efficacy).
-
Emotion.
-
Social influences (norms).
-
Skills.
-
Beliefs about consequences (anticipated outcomes).
-
Action-planning.
-
Memory, attention and decision processes.
-
Social and professional role and identity.
The result of this step of the IM process consisted of a matrix of cells that included the intersection of proximal performance objectives (rows of the table) with specified determinants (columns of the table) (see Appendix 5). From the intersecting cells, a statement or a learning or change objective was identified that would support the achievement of the proximal performance objective. This was achieved by scrutinising each performance objective individually to identify what barriers were associated with achieving each desired outcome. Our change objectives outlined specific challenges that staff, residents and relatives face in increasing regular movement, and the objectives could be clearly mapped to psychological determinants of behaviour (e.g. ‘intention’, ‘social influences’ and ‘skills’). For example, one of the determinants selected to be targeted in the intervention was knowledge. This was in recognition of the fact that baseline level of knowledge about what PA is, in the context of increasing everyday movement, rather than structured PA in exercise classes, and how staff might engage residents in increasing movement a little every day, was necessary.
Selection of strategies for behaviour change, incorporating suggestions from the advisory group
Following the above process and informed by previous work, appropriate theoretical methods were selected and translated into ideas for practical strategies. This involved identifying appropriate theoretical intervention techniques for each of the change objectives, and then considering how these would be delivered in practice. We used the described theoretical framework as a supporting process, which enabled suggested strategies to be operationalised. As an initial guide, we used the explanatory determinant list (see List 1: explanatory determinants) to select and combine behaviour change techniques (BCTs) and methods to achieve behaviour changes that were indicated to be effective. Here we drew on BCTs that had been mapped onto each of the 11 behavioural determinants, based on empirically supported theory. 63
The advisory group was purposely convened to lead us in the processes of selecting practical strategies and developing, refining and prioritising the techniques for each performance objective. (An example of how the concepts were presented to the advisory group is outlined in Report Supplementary Material 3.) The views of the group and our prior knowledge from the ethnographic work were invaluable in providing examples from existing practice. The practical strategies that we identified included provisional methods for implementation, some of which were appropriate to be applied at the level of the individual and some at the level of the home. The suggested practical applications, mapped to determinants, change objectives, performance objectives and BCTs, were then refined based on further discussion within the internal intervention group.
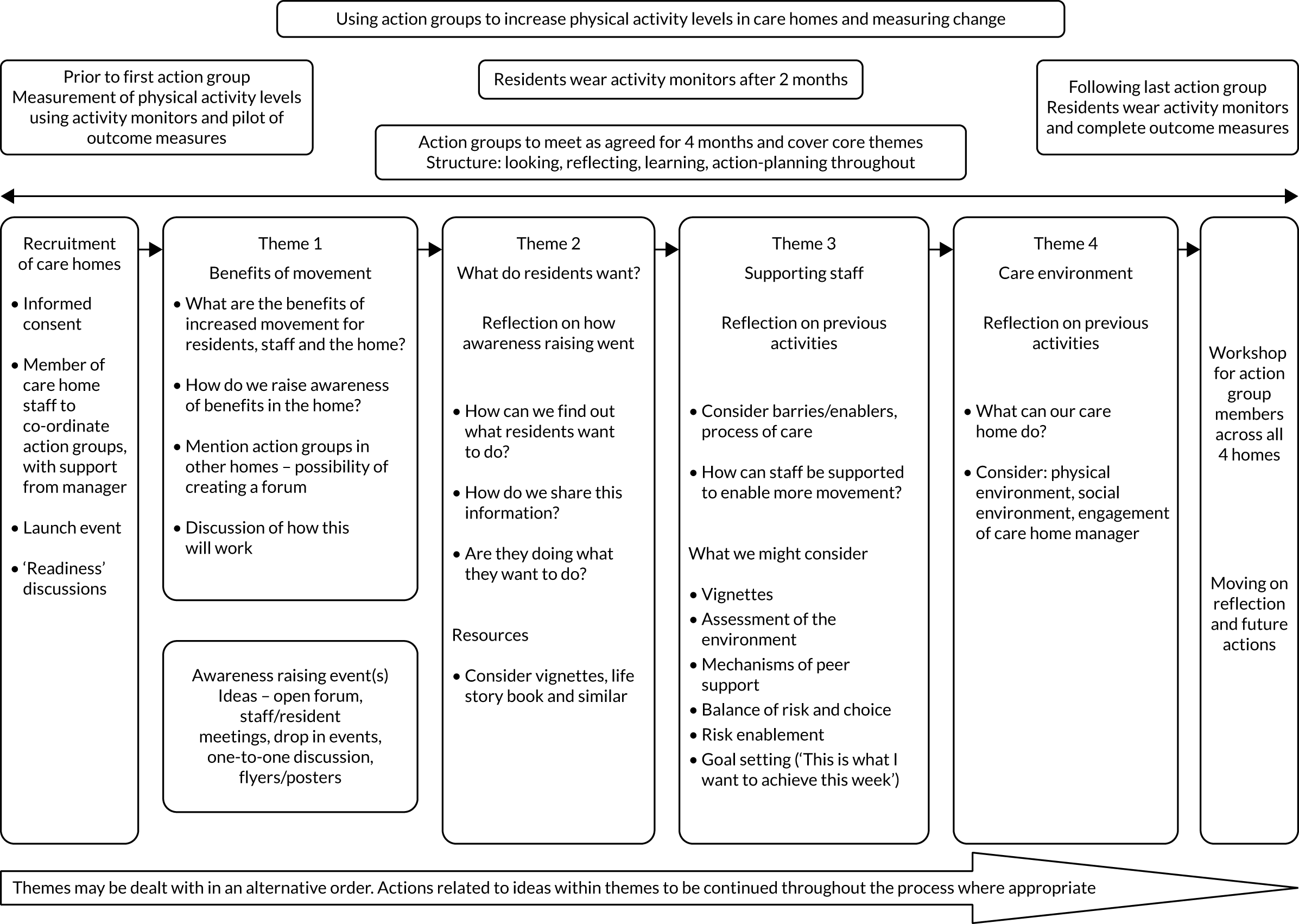
Developing and organising programme components and materials
The fourth step in the process involved designing and organising the programme to be implemented. We did this by broadly following Bartholomew et al. ’s62 recommendations of using the results of the needs assessment (step 1) and the theoretical and practical strategies from the targeted users (step 2) to design and organise the programme. In this case, this involved discussing and assessing the practical strategies for acceptability with members of the advisory group, and taking suggestions from these stakeholders for implementation of the intervention. We then grouped the emergent strategies into four key themes focusing on:
-
improving knowledge about movement and changing beliefs about consequences
-
finding out what residents want to do to move more
-
supporting staff to enable residents to move more
-
amending the environment to encourage PA.
This formed the basis for a schematic guide outlining suggested areas of change that might promote more regular routine daily movement for residents (Figure 7).
FIGURE 7.
Schematic guide to action groups.
Toolkits
In parallel with the advisory group meetings, we reviewed existing resources that had recently been produced relating to PA in CHs. We found that examples of practical strategies provided by the group were closely aligned with some existing resources (notably, resources produced by The Royal College of Occupational Therapists64 and The British Heart Foundation33). These resources (an ‘ideas bank’) were selected and collated based on decisions as to which change objective(s) would be addressed by the existing materials and what BCT(s) the existing materials represented (see Report Supplementary Materials 4 and 5). This ensured that all practical applications were based on sound theoretical methods. As a result, we produced a resource pack of selected materials, which was organised into the four themes.
Implementation would take the form of a stepwise process through supportive workshops to introduce and then embed the intervention into routine care delivery.
Delivery would be enhanced by a team of key stakeholders at the home (staff, relatives and residents), initially supported by researchers and professionals. Change would be implemented by the team using a cyclical process whereby goals would be developed from observations in the CH by stakeholders, and then progress would be reviewed.
Thus, a provisional intervention was developed. This consisted of the schematic guide focused on the four key themes and planned implementation through engagement of key stakeholders at the CH, with supportive workshops and a comprehensive set of resources (an ideas bank).
Key points
We successfully engaged with the stakeholder group and, through this, we developed a provisional intervention.
In creating the provisional intervention, we used a systematic and collaborative approach, guided by principles of IM. The IM process was useful as a planning template to incorporate our evidence base derived from previous research, theoretical components, practical strategies and other input from the advisory group. In this process, we established a need for better resources and implementation guidance in relation to increasing residents’ movement in CHs.
We have identified a number of specific enabling and limiting factors that we encountered in using IM to develop a complex intervention.
Strengths
Intervention mapping facilitated precision in determining which behaviours should be targeted and which change objectives (actions) were required to achieve the performance objectives and desired outcome (enhancing movement of residents in CHs). We found the early assessment of needs and involvement of relevant stakeholders in the intervention development process critical to developing the intervention. A number of strategies for behaviour change were intrinsically incorporated into various components of our intervention, based on the behavioural determinants identified in the IM process.
Limitations
Maintaining the focus of the advisory group was challenging, as the group was quick to suggest strategies and solutions without considering underlying determinants. This meant that the IM process did not always follow a linear format and the research team worked flexibly to capture all outputs.
Workstream 4: engaging care home staff and residents in intervention development and refinement of the intervention pack
Aims and objectives
The aims and objectives of this WS were to gain insight into the progress of the intervention implementation process (through implementation of action groups) by undertaking observations of meetings and daily life in the homes.
We also undertook additional related work to optimise the selection of outcome measures. This is reported in Appendix 6.
Methods
For a full description of the methods, see the protocol in Report Supplementary Material 6. The methods included the capture of action group activity and non-participant observations in CHs. Normalisation process theory (NPT) informed the refinement of strategies that were developed for implementation in CH routines.
Selection of homes
For a full description of recruitment procedures, see the study protocol in Report Supplementary Material 6. Briefly, four CHs in the Yorkshire area (different from those in previous WSs and the development work) were purposively selected.
The CHs varied in size from 19- to 96-bed facilities. One of the homes was designed to support residents with dementia and another (the largest home) had two of three units designated as specialist dementia resource. The homes varied in terms of their management/ownership: three were managed as part of large national private provider organisations and one was owned by a small local provider.
Action groups
Participative action-planning approach (action groups)
Action groups were established in each of the four homes, consisting of manager(s), care staff, residents, relatives/friends and a member of the research team, who acted as a facilitator. Twenty-nine individuals consented to participate in the action groups (nine residents, 18 staff and two relatives/friends of residents). We recognised that residents with the cognitive ability and willingness to participate may not be representative of the client group in that home; therefore, we sought innovative ways to involve the wider resident group.
Having developed a prototype for how an intervention might be delivered and a preliminary outline of issues that should be addressed (see Figure 7), an action research cycle of service improvement was employed to develop the intervention and engage staff and residents directly in the process of how to make change happen. 65
The action groups aimed to follow the provisional intervention developed in WS3. The purpose was to create a dialogue between researchers and these stakeholders about implementation strategies to increase PA/reduce sedentary time of residents, to try these strategies with staff and residents, and to review barriers to and opportunities for implementation in the real-life context of CHs that varied in terms of their resident profile and care environment.
Information about the importance of movement and some of our initial ideas were presented by a member of the research team and discussed with the group. Each action group was tasked with considering the current pattern of movement of residents, both in respect of the routines of daily living and during the leisure periods, and with exploring ways, through action plans, of increasing the PA/movement undertaken by residents in their CHs. At each action group meeting, progress in achieving action plans was reviewed through input/dialogue between members of the group. Barriers and solutions were identified, changes/refinements were made, depending on the progress achieved, and new action plans were developed to take the process of change forward through successive improvement cycles. The researchers also fed the group relevant data pertinent to contributing to the service improvement process. This included examples from observation, ‘ideas’ from the resource pack and emerging data systematically collected on the process of action-planning and the effects on staff and residents. In this way, we built up an ‘ideas bank’ of ‘what works, how and for whom’ in the real-life context of the home.
The proceedings of the action groups were, with participants’ permission, recorded and transcribed verbatim for analysis. Researchers also carried out observation of the process of implementation as it proceeded and contributed to the action cycle. Ethnographic observation and informant conversations between action group meetings built up a picture of the CH environment and the possibilities for change, and examined how and in what ways the strategies that were tried out affected residents.
Results of participative action-planning approach (action groups)
Action groups were successfully convened in all four homes, but sustaining engagement in the intervention implementation process as planned was challenging. The researchers successfully maintained engagement with the CHs, recorded group activities and collated observational data, as planned.
However, within the homes, there were practical difficulties in sustaining the action groups and maintaining interest in implementing change. These barriers included organisational turmoil, high rates of staff turnover, time constraints and a lack of senior management interest in supporting the process. On occasion, there were tensions between group members: between care staff and managers, between residents and care staff, and between researchers and care staff.
Challenge: there appeared to be a gap between our explanation of what the research was about and CH managers hearing what the study involved. The concept of increasing movement both at the level of daily life routines and in the leisure spaces appeared difficult for those working in the homes to understand; instead, movement was perceived of more in terms of PA/physical exercise.
Response: to ensure that, in the feasibility trial, the engagement in the study is not a one-off agreement but a sustained process of negotiation and to be very explicit about the focus of the research.
Challenge: on an organisational level, the difficulties of implementing change in CHs were highlighted. These included rapid unexpected changes of staff (and, in once case, ownership of the home), staff perceptions of the distinctive role of the activity co-ordinator and the work generated by Care Quality Commission (CQC) inspections.
Response: to consider what would support and drive the intervention and to ensure that implementation is sustained.
Response: it became clear in this WS that a more detailed implementation plan was required to optimise embedding the intervention in the CHs. Consideration was given to whether or not the intervention should be more prescriptive. This would not, however, take account of the very different circumstances and contexts of each CH, a key feature of the research in all of the CHs in the programme thus far. However, we did consider that there was an important difference between a more explicit process of implementation (what should happen and when in terms of making change) and the content of the changes, which should be home specific.
Response: training (interactive structured workshops, advice from experts, demonstration of strategies) could be incorporated into the implementation plan.
Challenge: a significant issue that emerged in three of the homes was the lack of engagement from care staff in activities around movement, as care staff perceived their role as primarily about the delivery of care. There appeared to be a divide between ‘care’ and ‘activities’, whereby movement is conceived of as part of ‘activities’ and is the realm of the staff charged with responsibility for ‘activities’ (i.e. the activity co-ordinator). This divide was perceived as a more active antagonism between some care staff and the activity co-ordinator in one of the CHs.
Response: to reconsider if we had clearly expressed in the presentation of the programme/intervention that the work of increasing movement embraces all staff. The materials and implementation process were amended to ensure that this key concept was fully captured.
Challenge: in two CHs, difficulties in knowing when to ‘push’ residents were expressed. Residents’ choices should be respected, so if they chose to remain in their rooms/have meals in their rooms this choice should be respected. There was also a lack of knowledge about how far to push residents, given their ill health.
Response: an experienced CH physiotherapist assisted with implementation of the intervention in the feasibility trial, specifically by providing a short introduction on the importance of movement.
Challenge: in the individual homes, some staff in the action groups were able to recognise that residents were sedentary, but in other homes there was a reluctance to acknowledge that any change could be achieved and staff were quite defensive. There was a perception from managers and carers that they were doing all they could to promote movement when they have enough time to do so.
Response: an important factor in engaging staff in a programme of change is to encourage them to take a close look at/reflect on what they currently do. In their CH, are residents encouraged to move? All residents? Some residents? In what aspects of CH life (self-care, walking about, organised leisure activities)? What works well? What does not work? And for whom? Staff need to be convinced that, in the context of their ‘home’, what is involved is more than what they currently do, and the value of the change is worth the work involved in making it happen. Difficulty in getting staff to recognise the potential of increasing PA prompted the further development of a short observational tool that staff were encouraged to complete. This enabled them to explore current practice and consider what might be done to effect change.
Supporting staff to take a step back enables them to have a different perspective, challenging taken-for-granted ideas and practices. The observational tool was designed to combine simple, short observation with critical appraisal (what actually happens), and follow quickly to actions. For example, staff members might spend 10 minutes observing, at a particular time of the day, particular residents and particular activities (personal care and daily life routines, moving about, individual and collective leisure activities). They could then more proactively engage in identifying problems/barriers and consider whether or not and how the activities are modifiable.
Facilitators: action groups and the ongoing engagement with the CHs during this WS provided a great opportunity to gain insight into staff perspectives. This enabled us to establish what modifications were needed in the content and delivery to improve the implementation and acceptability of the intervention and embed it into practice, as well as establishing what works, for whom, in what contexts.
The action groups were successful in identifying a number of actions, including rearranging chairs in communal areas to facilitate interaction, incorporating short walks into care routines and encouraging residents to participate in domestic tasks. Interventions for individual residents were undertaken and music was used to prompt PA/movement.
Response: These ideas were incorporated into the ‘ideas’ bank of the intervention.
Success: engagement with a local artist was particularly successful. Residents described their daily life to the artist and he depicted this in drawings (Figure 8). This succeeded in engaging residents with communication difficulties (e.g. from dementia, stroke) and stimulated lively discussion. The immediate outputs were displayed in the CHs and served as prompts to increase movement of residents and staff. The input of the artist became an integral component of the intervention.
FIGURE 8.
Artist’s drawings. Pictures developed through ‘movement’ discussions with staff and residents, facilitated by a researcher and in collaboration with a local artist, Tom Bailey, at one of the Workstream 4 homes.

Accessible summaries of the key findings were produced and fed back to staff and residents in each home (see examples in Report Supplementary Materials 7 and 8).
Through this careful iterative work (led by co-applicant Mary Godfrey), we successfully produced a defined intervention to be implemented to enhance the PA of residents in CHs, which was still focused on the four key themes identified [see Workstream 3: development of an intervention to enhance physical activity and appropriate methods of implementation (e.g. training materials) through a process of intervention mapping].
Key findings
Finalised intervention
The primary outcome of this WS and the previous WS was a finalised intervention called MoveMore. MoveMore consists of an intervention folder (manual) and supporting resources.
MoveMore is a whole-home intervention and implementation process, involving all CH staff, that is designed to encourage and support the movement of residents in each of four domains of daily routines:
-
independent/supervised movement to get about
-
introducing movement into organised social and leisure activities
-
providing opportunities for residents to engage in meaningful activities
-
encouraging them to do as much of their own self-care and instrumental ADL as possible.
MoveMore involves a change in how the work of the CH is understood and accomplished through organisational routines and practices. The content is flexible, shaped by the current pattern of movement and the resident profile.
Implementation of the programme involves a systematic approach, initially facilitated by researchers, and a set of steps to introduce and embed the intervention in routine care delivery. Implementation is led by the MoveMore team, comprising key stakeholders [staff, relatives and residents (if possible)], and facilitated by a senior member of staff. It requires both the active involvement of senior staff with the authority and legitimacy to drive change forward, thereby securing organisational commitment to introducing and embedding MoveMore, and the engagement of those directly involved in action to deliver the intervention. Implementation comprises a cyclical process of change, guidance and tools for staff to:
-
review current practice (observation)
-
identify goals and action plans to effect change (reflection and action-planning)
-
act (pursue action plans)
-
review progress (evaluate what has been achieved).
An intervention folder (manual) comprising observation tools, action plans, review sheets and an ideas bank of resources was supplied to all CHs. These materials and three interactive workshops aimed to provide both an understanding of the change process and to facilitate practise of the tools employed.
Following an overview of MoveMore, input from a physiotherapist and an introduction to the use of the observation tool in the first workshop, staff are encouraged to try it out in their CH. The experience of use is reflected on in the second workshop, and the observations that are carried out inform practice, with action-planning to be developed and pursued in the home. Support is offered in this workshop by an artist providing a visual representation of the team’s discussions. Action plans and a review of progress are brought back to the third workshop to evaluate what has been achieved, the barriers encountered and next steps. This process requires time and effort (Figure 9).
FIGURE 9.
Outline of MoveMore intervention delivered by CH staff.
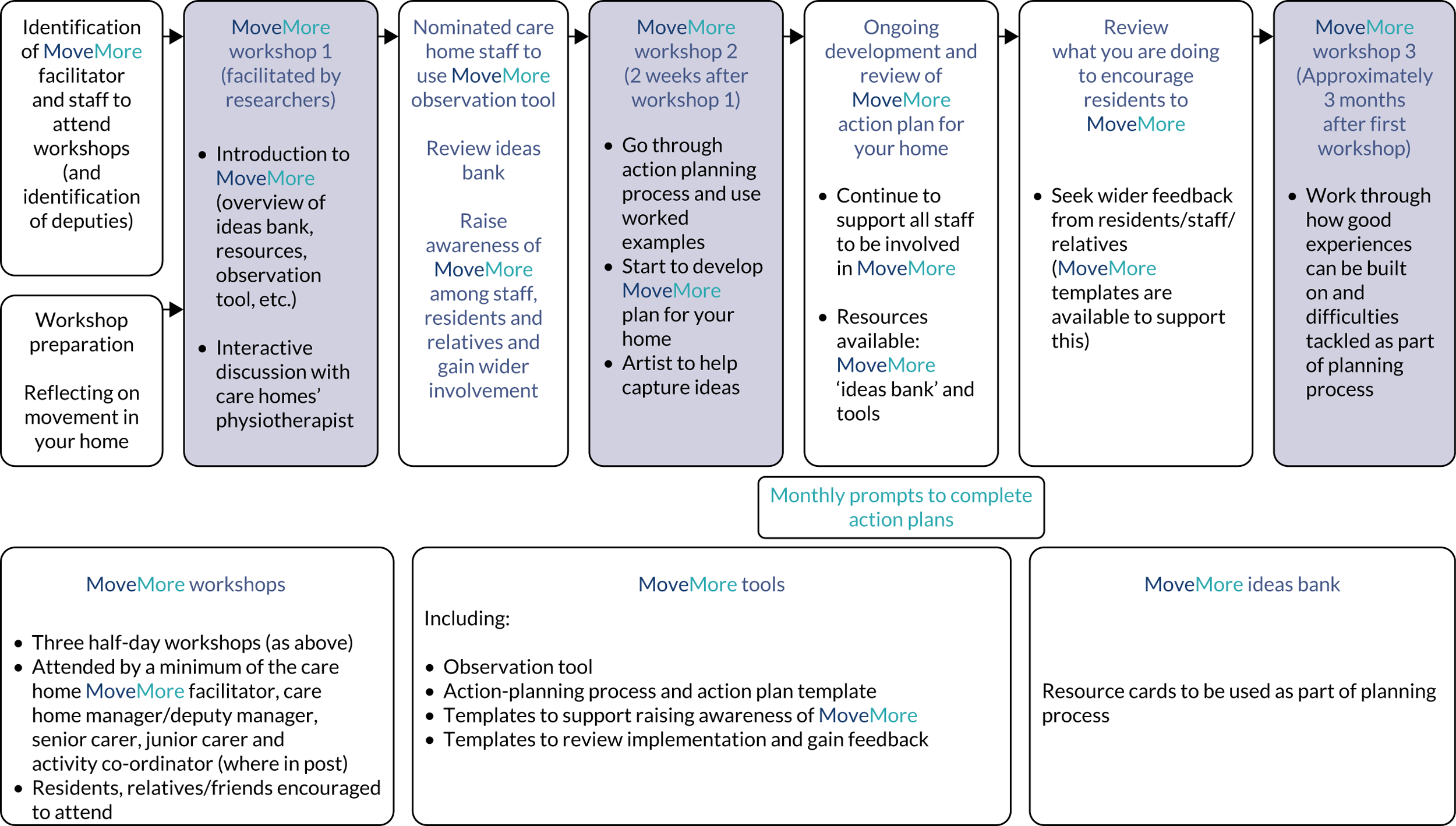
Prerequisites for success include staff understanding the value of movement for residents, wider staff team engagement with the process, residents being responsive to the changes initiated and demonstrable gains being shown for the work involved. Even so, contextual factors outside the intervention may mediate engagement with the programme.
The MoveMore intervention programme is an exemplar of a complex intervention, in that it contains ‘several interacting components’. 61 It is aimed at changing how the routine work of care staff is carried out, such that residents are encouraged and supported to move more in every facet of their day-to-day lives. Furthermore, it is targeted at several organisational levels (CH, multiple staff roles and individual staff), requiring ‘buy-in’ from staff at each level to make sustainable change happen. The heterogeneity of residents’ needs and circumstances, and the individual tailoring of the intervention to these differences, adds another level of complexity. Although seeking to modify the way that staff think, act and organise themselves on the one hand, on the other hand, the purpose is to initiate a process in the way residents think and act towards achieving the primary outcome of reducing the time residents spend sedentary.
Finalised outcome measures
We finalised the outcome measures to be used in the feasibility trial, as described in Appendix 6.
Workstream 5: feasibility cluster randomised controlled trial of MoveMore and usual care versus usual care
Parts of this section have been reproduced from Forster et al. 66 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Aim and research questions
The aim was to determine the feasibility of conducting a large-scale cluster randomised controlled trial (RCT) comparing the Research Exploring physical Activity in Care Homes (REACH) intervention (MoveMore) plus usual care (UC) with UC only for permanent residents living in residential CHs in the UK. We also aimed to evaluate the acceptability of the MoveMore intervention. The main research questions addressed were as follows:
-
What is the optimum strategy to facilitate recruitment at both the CH and resident level?
-
Is the uptake and compliance with the MoveMore intervention by CH staff at an acceptable level to be evaluated in a full-scale cluster RCT? If not, why not?
-
What are the characteristics of UC in residential CHs?
-
Is the uptake and compliance with the measurement tool to assess the proposed primary trial outcome (residents’ PA) at an acceptable level to be evaluated in a full-scale cluster RCT? What are the reasons for non-participation?
-
Are the most appropriate outcome measures being considered for the trial?
-
What are the optimum strategies for data collection?
-
To calculate reliable estimates to feed into sample size calculations for a full-scale RCT, including preliminary effectiveness estimates.
-
Do the implementation resources required affect the feasibility of conducting a full-scale cluster RCT?
Research questions/aims 1–7 were assessed via statistical analyses. Aims 2 and 3 were additionally evaluated via the embedded process evaluation (PE). Aim 8 was assessed via the PE and health economic data.
Summary of study design
The REACH feasibility trial was a cluster RCT taking place in 12 residential CHs in the Yorkshire region. CH staff introduced the trial concept to eligible residents who, if they agreed, spoke to a researcher who obtained their consent to participate. Alternative consent arrangements were made if a resident lacked capacity, in line with the Mental Capacity Act. 67 Following baseline assessment and registration of all consenting residents, CHs were randomised on a 1 : 1 basis either to implement the MoveMore intervention plus UC or to continue with UC only.
The MoveMore intervention was designed to be implemented by CH staff on an ongoing basis following randomisation. Implementation guidance was provided by the research team following randomisation, and support for implementation was available to all intervention homes thereafter, if required.
Care homes and residents were followed up at 3, 6 and 9 months post randomisation. CH staff and residents were (necessarily) aware of intervention allocation, but the collection of outcomes by researchers was undertaken blind to this knowledge whenever possible. Resident-reported and staff-reported outcome data, along with data collected from the CH manager, were collected at researcher visits. Adverse event data were collected by researchers from CHs on a monthly basis, via resident-/staff-reported data and via receipt of hospital attendance data from NHS Digital. The PE was undertaken on an ongoing basis in each CH throughout the study.
Full details of the trial are available in the protocol. 66
Recruitment
For a full description of recruitment procedures, see Forster et al. 66
Care homes
A sample of 12 residential CHs was required.
Care homes were considered eligible if the following two criteria were met:
-
Initial scoping indicated that there were sufficient numbers of permanent eligible residents to enable 8–12 permanent residents to be recruited (homes were later excluded if they were unable to obtain consent and baseline data for at least five residents).
-
There was a manager or nominated person who agreed to sign up to the trial protocol as research lead and to release staff time for data collection, including supporting the use of the accelerometers and, when appropriate, intervention implementation. Signed agreement was required from the CH manager and CH owner or representative.
Care homes were excluded if:
-
the CH was subject to CQC enforcement notices, admission bans or relevant moderate or major CQC compliance breaches (e.g. staff training, staff numbers, safeguarding)
-
they were receiving other special support for specific quality concerns, such as being currently subject to, or having pending, any serious safeguarding investigations, or receiving voluntary or compulsory admissions bans, or were in receipt of local commissioning special support as a result of quality concerns
-
they had taken part in any of the earlier REACH studies
-
they were taking part, had recently taken part, or were planning to take part in another trial or initiative that conflicted with the MoveMore intervention or data collection.
Two parallel, standardised processes were used to recruit CHs in West and North Yorkshire. The first, a ‘systematic approach’, was via the publicly available care directory on the CQC website; the second, a ‘targeted approach’ was via the Yorkshire Enabling Research in Care Homes (ENRICH) network, a network of CHs that had already expressed an interested in research. 68 The standardised method used to recruit CHs consisted of screening, researcher contact, visit(s) and a formal letter of agreement. Eligibility was continually assessed from screening through to obtaining consent.
Residents
As the MoveMore intervention is a whole-home intervention designed to assist CH staff to make changes in their approach to working with residents, all residents in the home (regardless of eligibility and consent status) have the potential to be exposed to the intervention. Therefore, residents consented to participate in data collection only.
All residents in the participating CHs were screened for eligibility. Resident eligibility was assessed by the CH manager (or appropriate delegate), with support from the trial researcher once the CH had provided consent.
Residents meeting all of the following criteria and none of the exclusion criteria were considered eligible to participate:
-
Aged ≥ 65 years.
-
Permanent resident in the home, defined as a person residing in the CH and not present for receipt of respite, day care or short-term rehabilitation.
-
Known by the CH manager and/or relevant senior staff member not to be terminally ill or bedbound/cared for in bed.
-
Not taking part in, or planning to take part in, another trial that conflicted with the MoveMore intervention or data collection during the course of their involvement in the trial.
-
Appropriately consented (in accordance with the Mental Capacity Act67 and clinical trials guidance on informed consent). For residents lacking capacity to consent, PCs or NCs were identified to provide consent on their behalf.
To optimise recruitment of participants, and enhance generalisability of the population group, in addition to individual informed consent, we also obtained approval to approach a PC. If the resident had no close family or friend able or willing to act as a PC, another appropriate independent person, usually a member of staff in the CH, who knew the resident well was appointed as a NC.
Randomisation
Once all residents were registered and baseline assessments were completed, CHs were randomised on a one-to-one basis by the Clinical Trials Research Unit statistician using a computer-generated minimisation program incorporating a random element. The minimisation system was stratified on characteristics expected to be correlated with intervention implementation and outcome evaluation, namely the size of the CH (small/medium, ≤ 40 residents; large, > 40 residents) and whether or not the CH had an activity co-ordinator in post.
Care home managers were informed of the outcome of randomisation. Assessors were blind to randomisation and were based separate from the researchers who delivered the intervention. CH staff were asked not to inform the assessment team of randomisation and to remove any material before their visits.
Intervention
MoveMore intervention
The intervention, described previously (see Workstream 4: engaging care home staff and residents in intervention development and refinement of the intervention pack), was supported by regular monthly and additional ad hoc contacts.
Usual care (all care homes)
Usual care, defined as normal care delivered in the setting, continued in both arms. No restrictions were imposed on current practices or on homes undertaking additional development or training as part of UC. The MoveMore intervention was offered to all UC homes at the end of the trial.
Methods for data collection
For a full description of the methods, see Forster et al. 66
Trial data collection
The intention was for the intervention to become embedded in the CH (if randomised to the intervention arm); thus, it was important to assess the impact of the intervention on the CH as a whole. Consequently, data were collected at the level of the CH (including staff), as well as from individual consenting residents. Data were collected by trial researchers blinded to allocation.
For details of data collection, see Forster et al. 66 Briefly, data collection comprised the following.
Care home-level data
-
Care home demographics.
-
Staffing levels.
-
Resident profile.
-
Anonymous data relating to hospital admissions, general practitioner (GP) call-outs, mortality rates and falls in the previous 3 months.
-
At baseline screening process: anonymous PAM-RC (Dr Julie Whitney, personal communication) and BI48,49 scores for all residents.
Staff-level data (for those with face-to-face contact with residents)
-
Basic demographic data.
-
Person-centred care provided in the CH [Person-centred Care Assessment Tool (P-CAT)]. 69
Resident-level data
Via researcher interview
Via staff member
Accelerometry
To allow for the objective measurement of PA, residents were asked at each data collection time point to wear an ActiGraph wGT3X-BT accelerometer (ActiGraph, LLC) on the hip, during waking hours, over the course of 7 days. A detailed protocol, refined through earlier WSs, was followed for administration of the accelerometers, which took place after the data collection defined above to ensure that accelerometer wear did not interfere with residents’ routine PA levels and influence their questionnaire outcome assessments. Researchers assisted with the administration of the accelerometers on the initial visit and instructed care staff in their daily application. Researchers routinely checked compliance by regular telephone calls and visits to the CHs (including a weekend telephone call or visit). Residents and CH staff were also encouraged to complete a purposely designed log to record daily wear time.
Adverse event data
Adverse event data were collected by a researcher via resident-/staff-reported data, via monthly contact with the CHs, and, to explore the best method of collecting service use data, via data routinely recorded by the CH, as well as via receipt of hospital attendance data from NHS Digital and relevant acute hospital trusts.
Intervention data
To inform understanding of the actual implementation and to inform methods for measuring adherence in a definitive trial, data were collected on the workshops (time, place and duration, and number and details of CH attendees present), enhancing implementation and adherence to the intervention. These data are intended to be interpreted alongside the PE study (see Process evaluation).
A record of the monthly and ad hoc contact by the research team with the CHs regarding the implementation of the intervention was maintained (considered as implementation enhancement activities).
Intervention adherence was measured at the 3-, 6- and 9-month data collection points by review of observation and reflection sheets completed by the CHs and kept in the intervention folder in the CH.
Usual care data
Details of UC were recorded at each assessment point via researcher observations (individual residents were not identified during such observations) and via completion of a pro forma developed for the purpose of recording the pattern of movement in all homes for the four discrete dimensions of the intervention (enabling self-care, and movement in daily routines, organised social and leisure activities and tasks around the home) to inform the context in which the study was being conducted.
Data on UC were also captured via the CH booklet in terms of participation in current initiatives relating to enhancing resident care. Researchers also looked for display of materials (posters, leaflets, etc.) related to movement in the CHs.
Statistical methods
For a full description of the statistical methods related to each research question, see Forster et al. 66
Analyses and data summaries were conducted on an intention-to-treat (ITT) population and focused on descripitive statistics and confidence interval (CI) estimation, rather than formal hypothesis testing. All analyses were carried out using SAS® software version 9.4 (SAS Institute Inc., Cary, NC, USA), unless otherwise stated.
Completion and scoring of questionnaires were analysed in line with scoring manuals, including guidance on how to handle missing items. If no direction was given, scores were prorated if ≥ 50% of the items were completed.
Accelerometer
Daily wear time was calculated as the time between the first non-zero and last non-zero reading of the day, minus any periods within that time when there was ≥ 120 minutes of consecutive zero counts (classified as ‘non-wear’). Longer periods of non-wear of 180 minutes and 240 minutes were also examined to reduce misclassification of sedentary activity. Valid wear time for analysis was defined as ≥ 8 hours 25 minutes on ≥ 4 days (which could be non-consecutive days). For residents who provided valid data, the amount of time spent in various PA categories76 and in sedentary behaviour was identified using cut-off points applied to the vertical axis accelerometer counts per minute (cpm) (see Forster et al. 66).
Guidelines for progression to a Phase III trial
Guidelines for progression to a definitive cluster RCT were predefined and based on a traffic-light system of green (proceed to cluster RCT design), amber (review cluster RCT design and/or implementation, then proceed) and red (stop and do not proceed). Definitions for each can be found in Report Supplementary Material 9.
Key findings
The majority of statistical tables can be found in Appendix 7.
Recruitment and follow-up
Estimation of recruitment and follow-up
Overall, 392 CHs were screened between June 2015 and September 2016: 13 (7.6% of those eligible) provided consent and 12 (7.0% of eligible) were randomised (see the CH recruitment paper by Ellwood et al. 77). A range of CHs were recruited in terms of size, location, ownership and provision (see Appendix 7, Table 23). Five CHs were randomised to the MoveMore intervention plus UC and seven were randomised to UC only.
The two strategies used to recruit CHs provided different success rates, as well as time scales to recruitment. A total of 377 CHs in West Yorkshire were screened via the CQC database. Of these, only 164 (43.5%) passed initial eligibility checks and were contacted by a researcher, and 11 (2.9% of those screened) consented. In contrast, 15 CHs in North Yorkshire were screened via the ENRICH network, 12 (80.0%) were contacted by researchers and two (13.3% of those screened) consented to participate. 77
Care home and staff characteristics
Care homes
Care homes in the MoveMore arm were, on average, smaller than the UC CHs, with a smaller number of beds, a smaller number of beds taking part and a smaller number of permanent residents, although there was greater variation in resident numbers across UC homes during the trial. UC homes were, however, less likely to provide rehabilitation or intermediate care and have telemedicine facilities (see Appendix 7, Table 23).
See Appendix 7, Table 24, for follow-up data of CH characteristics.
Care home managers
Information on CH manager demographics is provided in Appendix 7, Table 25.
The CH managers in the MoveMore homes had slightly more experience working in CHs, and more experience as a home or unit manager. However, the managers in the UC homes had been in their current post for, on average, 3 years longer than the managers in the MoveMore homes, although this was skewed by one particular home whose manager had been in the post for 22 years. There was a change in manager at one CH in the UC arm at both the 3- and 9-month follow-ups.
Information on staff demographics (see Appendix 7, Table 26) was obtained via completion of staff booklets, which were distributed to all staff who had face-to-face contact with residents, with the exception of those acting as a NC. Overall return rates were low, ranging between 20 and 39%, with a higher proportion of staff in the UC CHs completing the booklets at each time point. However, as the characteristics of those who completed the booklet at each time point were reasonably similar between the arms, any differences are likely to reflect the profile of the staff at the CHs, rather than any systematic differences in those completing the booklet. Thirteen members of staff across all CHs completed the staff booklet at every time point.
Resident screening and recruitment rates
Three hundred residents in the 12 CHs were screened for participation. Of these, 278 (92.7%) were eligible, 159 consented/had consultee agreement (57.2% of eligible; 53.0% of those screened) and 153 were registered to take part in the study (55.0% of eligible; 96.2% of those consenting/consultee agreement) (Figure 10).
FIGURE 10.
Flow of residents through screening, consent, baseline assessment and registration. a, Reasons not mutually exclusive.
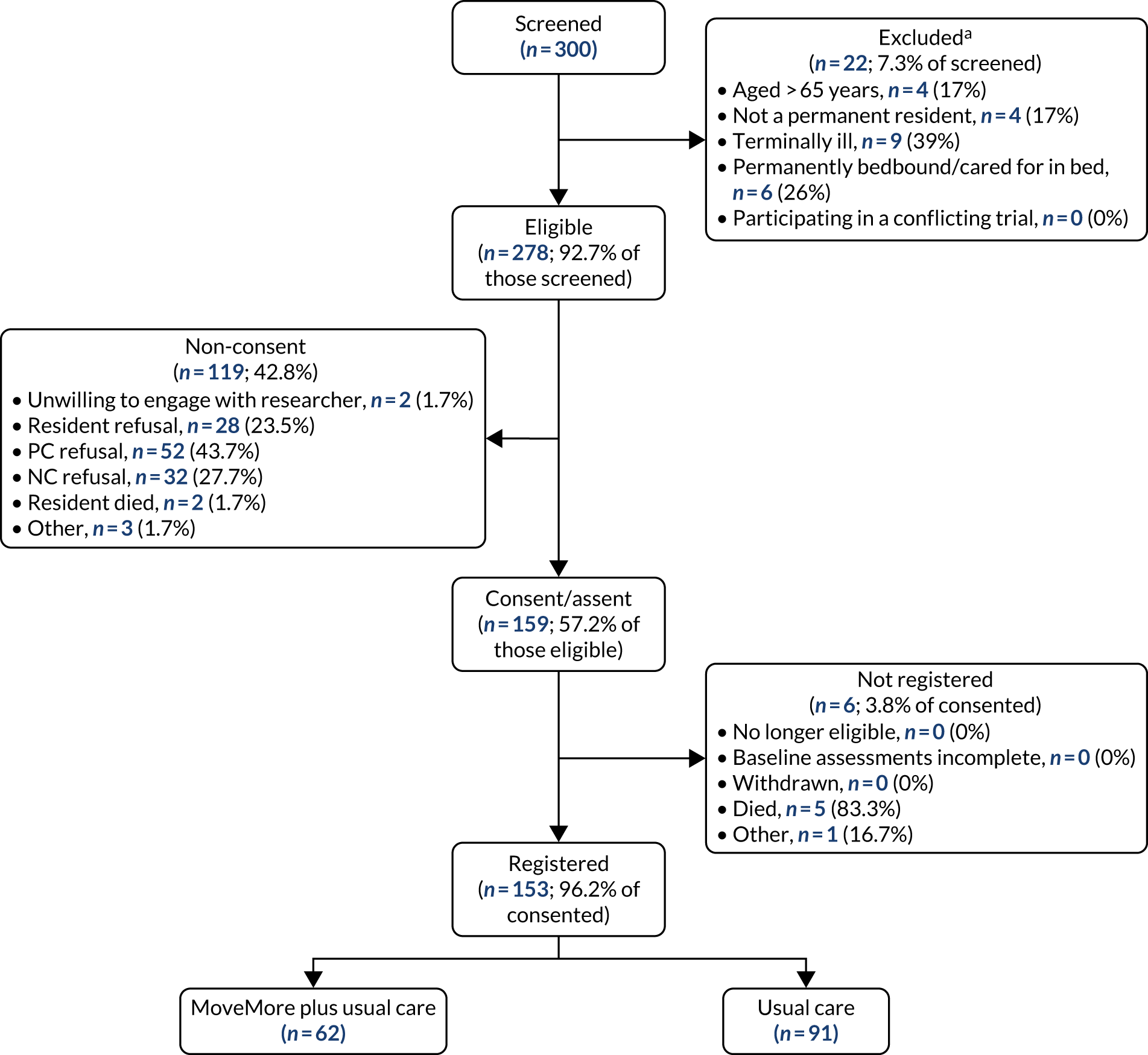
Forty-three (59.7%) of 72 residents with mental capacity were recruited. Of the 203 residents with doubtful or who were lacking mental capacity, 187 had a potential PC; 73 (57.9%) of the 126 PCs who agreed to act agreed for the resident to take part in the study. A NC was used for 76 residents, 43 (56.6%) of whom agreed for the resident to take part in the study.
There was variation across CHs in the proportion of eligible residents who were registered, but the overall proportions were similar between the arms: 62 out of 113 (54.9%) eligible residents were registered in the MoveMore arm, compared with 91 out of 165 (55.2%) in the UC arm (see Appendix 7, Table 27). On average, 12.4 residents per home were registered in the MoveMore arm, and 13 residents per home were registered in the UC arm, although, in one CH, only six residents were registered in each arm (see Appendix 7, Table 27).
The average time for recruitment at the CHs was 64 days; the shortest time was 50 days and the longest was almost twice this (97 days), although these times also included approximately 3 weeks per CH for baseline data collection (depending on the number of participants in each CH).
Follow-up rates
Care home and resident retention during the study period was high, with no CH or resident protocol violations or withdrawals, although one CH in the UC arm temporarily withdrew from researcher visits at 3 months because of renovations in the home (Figure 11).
FIGURE 11.
The CONSORT diagram of the flow of CHs and residents through follow-up by randomised arm.
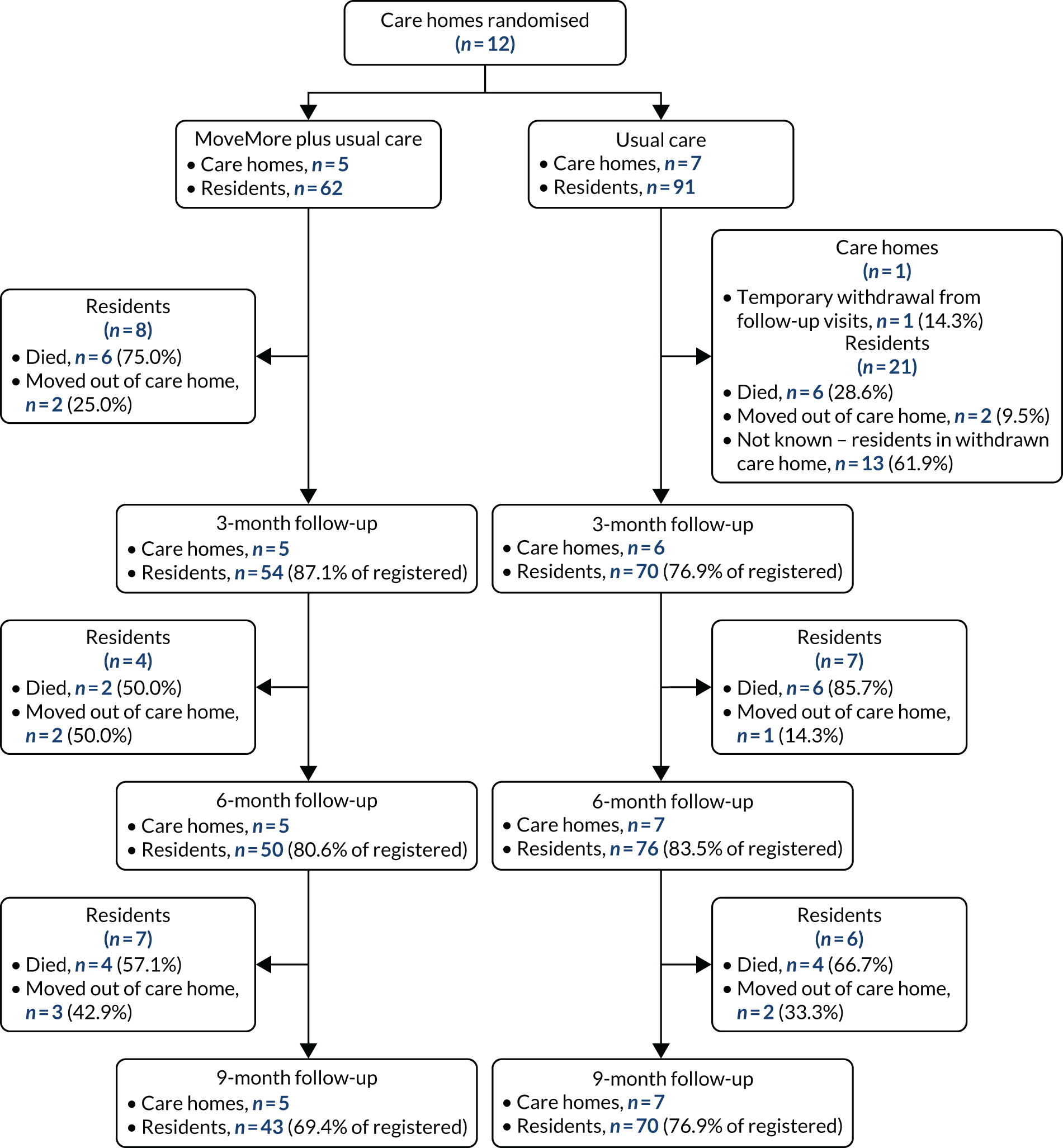
There was some variation in the proportion of residents followed up across the CHs (50.0–90.9% at 9 months) (see Appendix 7, Table 27), with a lower overall proportion in the MoveMore arm (69.4%) than in the UC arm (76.9%) (difference –2.65, 95% CI –17.50 to 12.20) (see Appendix 7, Table 28).
Losses to follow-up were due to deaths and movement of residents out of the CH (see Appendix 7, Table 29). Deaths and resident movement were also similar between arms at the CH level (see Figure 11 and Appendix 7, Table 28).
Screening characteristics
Overall, the consenting residents had similar characteristics to the whole screened population, and therefore can be considered a representative sample (see Appendix 7, Tables 29–31). However, a larger proportion of residents in the MoveMore arm than in the UC arm had had a previous stroke, and residents in the MoveMore arm had lower mean BI and PAM-RC scores (see Appendix 7, Table 30). In the intervention arm, the care of a higher proportion of residents was funded through the local authority and a lower proportion of residents were self-funded (see Appendix 7, Table 30).
There was similarity in screening characteristics between those eligible who consented and those who did not, with the exception of a higher proportion of residents with a diagnosis of dementia consenting (see Appendix 7, Table 31).
Resident baseline characteristics
Baseline characteristics for registered residents reflected the differences between the MoveMore and UC arms in the physical function and history of stroke that was observed at screening (see Appendix 7, Table 32).
In addition, those in the MoveMore arm also had greater cognitive impairment, as measured by the 6-CIT (see Appendix 7, Table 32), than those in the UC arm and a higher proportion had at least one comorbidity (see Appendix 7, Table 33).
A comparison of the baseline characteristics between those who were and those who were not followed up indicated that those not completing follow-up were more likely to be male, have dementia, have no history of stroke, have lower physical function and have greater cognitive impairment (see Appendix 7, Table 34). This is consistent with a higher (although not significant) proportion of residents in the MoveMore arm being lost to follow-up and the residents in this arm having a lower physical function and greater cognitive impairment.
Intervention delivery
Implementation of MoveMore components
A series of three interactive workshops were delivered individually to each of the five intervention CHs, with one CH repeating workshops 1 and 3 to ensure that all those potentially responsible for intervention implementation were included (see Appendix 7, Tables 35–37). Workshops took place at the CHs, with the exception of one CH, for which the workshops took place at its head office.
The implementation of the intervention was designed to be led by a team involving staff, residents (if possible) and their relatives/friends, facilitated by a senior member of CH staff (i.e. the MoveMore lead). The MoveMore lead was present for workshops 1 and 3 at all CHs, and for workshop 2 for four of the five CHs (see Appendix 7, Tables 35–37). The attendees were mainly (permanent) carers (see Appendix 7, Tables 35–37), although staff in other roles attended, particularly in CH5, including administration, ancillary, manager/deputy manager, team leader and specialist non-clinical roles, such as activity co-ordinator. With the exception of one CH, there were at least two staff members from each CH who attended all three workshops. One resident/relative attended workshop 1; in another CH, the executive director attended workshop 2. All workshops were delivered by researchers with key input from an experienced CH physiotherapist and an artist; workshops ranged in duration from 45 minutes to 2 hours 30 minutes, generally decreasing in duration with each workshop (see Appendix 7, Tables 35–37).
Time scales for intervention delivery
There were some challenges delivering the initial workshops for three CHs because of staff sickness, leave and temporary closure. Thus, in practice, the initial workshop was delivered 4–11 weeks after randomisation (Table 4). There were also some delays in subsequent workshops. Only CH5 completed all three workshops within 3 months of randomisation; for three CHs, the workshops spanned > 6 months (see Table 4).
| Outcome measure | Time (weeks) | |||
|---|---|---|---|---|
| Randomisation to workshop 1 | Workshop 1 to workshop 2 | Workshop 2 to workshop 3 | Randomisation to workshop 3 | |
| Planned time | ≤ 2 | 2 | 4–6 | 8–10 |
| CH | ||||
| 1 | 9.3 | 12.0 | 6.0 | 27.3 |
| 2 | 7.3 | 13.0 | 7.7 | 28.0 |
| 3 | 11.7 | 14.9 | 7.3 | 33.9 |
| 4 | 4.6 | 3.3 | 14.9 | 22.7 |
| 5 | 5.4 | 2.0 | 4.0 | 11.4 |
| Mean (SD) | 7.7 (2.90) | 9.0 (5.94) | 8.0 (4.11) | 24.7 (8.3) |
| Median (range) | 7.29 (4.8–11.7) | 12.0 (2.0–14.9) | 7.29 (4.0–14.9) | 27.29 (11.4–33.9) |
The process of organising and scheduling the workshops was refined as the trial progressed and became more efficient.
Enhancing implementation
The amount and type of contact that the researchers had with the CHs varied. An initial meeting was introduced (after randomisation of the first CH) to set the scene for the intervention implementation. Initial contact was focused around administrative details (organising workshops, etc.); thereafter, further support was provided by the research team, with at least one visit to each CH to support intervention delivery (Table 5).
| CH | Method of contact | ||||
|---|---|---|---|---|---|
| Face-to-face | Telephone | Text | Total | ||
| CH, n (%) | |||||
| 1 | 6 (21.4) | 1 (3.6) | 0 (0.0) | 21 (75.0) | 28 (100.0) |
| 2 | 7 (25.9) | 15 (55.6) | 0 (0.0) | 5 (18.5) | 27 (100.0) |
| 3 | 10 (33.3) | 14 (46.7) | 6 (20.0) | 0 (0.0) | 30 (100.0) |
| 4 | 7 (41.2) | 10 (58.8) | 0 (0.0) | 0 (0.0) | 17 (100.0) |
| 5 | 5 (41.7) | 3 (25.0) | 0 (0.0) | 4 (33.3) | 12 (100.0) |
| Number of contacts | |||||
| Mean (SD) | 7.0 (1.87) | 8.6 (6.35) | 1.2 (2.68) | 6.0 (8.69) | 22.8 (7.86) |
| Median (range) | 7 (5.5–8.5) | 10 (2–14.5) | 0 (0–3) | 4 (0–13) | 27 (14.5–29) |
Completeness of MoveMore documentation
The methods used to capture adherence to the intervention paperwork outside the workshops were not successful, as the intervention folders that contained the relevant data were not always available to the researchers in the CHs.
Interestingly, five of the seven UC CHs wished to take up the intervention at the end of the trial. Of these, three went on to have the full series of workshops, one had one workshop before the manager disengaged and one wanted the workshops but was unable to release staff.
The PE (see Process evaluation and Appendix 9) provides further context.
Care home staff
At each time point, almost all CHs experienced staff leaving and joining the home during the preceding 3 months, but there was no suggestion of a difference in staff movement between the arms (see Appendix 7, Table 38).
Usual care
For a description of UC, see Appendix 7, Table 39.
By the end of the trial, both arms had a similar proportion of CHs with an activity co-ordinator in place.
Further details are reported in Process evaluation.
Assessment of outcomes measures
Accelerometer data
For a full description of the accelerometer findings, see Appendix 8.
Accelerometer wear
The proportion of available residents who agreed to wear the accelerometer was similar across arms (88–97%) until the 9-month time point, at which time the proportion agreeing to wear the accelerometer was greater in the MoveMore arm (see Appendix 8, Table 54).
The number of days residents wore the accelerometers was similar between the arms and, within wear days, residents wore the accelerometers for ≈ 10–11 hours (see Appendix 8, Table 54).
The proportion of residents wearing the accelerometer who met the minimum wear criteria for analysis (≥ 8 hours 25 minutes per day for ≥ 4 days) differed between the arms at each time point (see Appendix 8, Table 54). Even so, at each time point, the mean number of days the accelerometer was worn for was > 6 in both arms and mean daily wear time was > 10 hours 18 minutes (see Appendix 8, Table 54).
A preliminary review suggests that the data recorded on the activity logs provided incomplete information on when the accelerometer had been put on and taken off each wear day. Hence, the planned comparison between accelerometer and wear logs was not conducted.
Levels of physical activity and sedentary behaviour
Physical activity
At baseline, residents in the MoveMore arm spent less time engaging in PA of any intensity (mean 1 hour 7 minutes, 8.5% of accelerometer wear time) than residents in the UC arm (mean 1 hour 53 minutes, 13.4% of accelerometer wear time) (see Appendix 8, Tables 60 and 61).
At each follow-up, the mean daily time spent engaging in PA of any intensity increased in both arms. The mean daily time that residents in the MoveMore and UC arms spent engaging in PA of any intensity at 9 months was 1 hour 25 minutes (SD 47 minutes) and 2 hours (SD 2 hours 16 minutes), respectively. This equated to 10.9% (SD 5.5%) of accelerometer wear time in the MoveMore arm and 12.6% (SD 10.8%) in the UC arm. The increase in PA of any intensity from baseline to 9 months was greater in the MoveMore arm than in the UC arm (see Appendix 8, Tables 60 and 61).
However, in both arms, all residents engaged in some level of light and moderate activity, although this was for < 2% of the day (see Appendix 8, Table 61). The increased proportions of time spent in PA were reflected mainly in periods of low intensity (see Appendix 8, Table 61).
In the MoveMore arm, there was a gradual increase in the number of days that residents engaged in low-intensity bouts of 5 minutes’ duration and in the number of 5-minute bouts per day (see Appendix 8, Table 63).
Sedentary behaviour
At baseline, the mean daily time that residents spent sedentary was similar between the arms (MoveMore arm: 11 hours 38 minutes; UC arm: 11 hours 41 minutes) (see Appendix 8, Table 60). This equated to a considerable proportion of accelerometer wear time (MoveMore arm: 91.4%; UC arm: 86.6%) (see Appendix 8, Table 61). As the CIs for these figures did not overlap, there was a suggestion that the proportion of time in sedentary behaviour was greater in the MoveMore arm. This is consistent with residents in the MoveMore arm having lower physical function and more comorbidities than those in the UC arm.
At 9 months, there was no change in the average time residents in the MoveMore arm spent sedentary (11 hours 31 minutes), compared with baseline (see Appendix 8, Table 60); however, this did account for a smaller proportion of accelerometer wear time (89.1%) (see Appendix 8, Table 61). Conversely, in the UC arm, an increase in the time spent sedentary was observed (12 hours 33 minutes) (see Appendix 8, Table 60), such that there was little difference in terms of the proportion of wear time (87.4%) (see Appendix 8, Table 61). Thus, at 9 months, the difference between the arms in terms of percentage of accelerometer wear time spent sedentary narrowed (MoveMore arm: 89.1%; UC arm: 87.4%) (see Appendix 8, Table 61).
Patterns of physical activity and sedentary behaviour
Physical activity bouts
At baseline, residents in the MoveMore arm engaged in bouts of low-intensity PA of at least 5 minutes’ duration on fewer days, with less frequency per day and for shorter duration (see Appendix 8, Table 63) than residents in the UC arm, and they engaged in bouts of low-intensity PA of at least 10 minutes on fewer days and with less frequency per day than residents in the UC arm (see Appendix 8, Table 64). However, the proportion of residents engaging in low-intensity bouts of at least 10 minutes’ duration was lower in the MoveMore arm (19/49; 38.8%) than in the UC arm (49/77; 63.6%); hence, comparisons should be interpreted with caution (see Appendix 8, Table 64).
There were fluctuations during follow-up among residents in the UC arm in low-level intensity bouts of PA of ≥ 5 minutes’ and ≥ 10 minutes’ duration in the number of days they engaged in at least one bout, the number of bouts per day and the average duration of the bouts. However, by 9 months, there was a suggestion that residents engaged in low-intensity bouts of 5 minutes’ duration on fewer days than they did at baseline (see Appendix 8, Table 63). But, on the days they did engage, they had more bouts (see Appendix 8, Table 63), although the average duration of the bouts did not appear to change (see Appendix 8, Table 63).
At 9 months, there was no suggestion of a difference between the arms in the 5-minute low-intensity bout outcomes (see Appendix 8, Table 63), but the difference in the number of days and number of bouts per day for the 10-minute low-intensity bouts that was observed at baseline remained (see Appendix 8, Table 64). There were, however, few residents engaging in low-intensity bouts of 5 minutes’ and 10 minutes’ duration by 9 months; therefore, it is difficult to draw robust conclusions on such small sample sizes (see Appendix 8, Tables 63 and 64).
Breaks in sedentary behaviour
At baseline, the number of breaks in sedentary behaviour that residents had per day were fewer among residents in the MoveMore arm than among residents in the UC arm (see Appendix 8, Table 62).
At each follow-up, the number of breaks in sedentary behaviour increased in both arms, but by a greater amount in the MoveMore arm (see Appendix 8, Table 62), such that, at 9 months, there was no suggestion of any differences in the number of breaks in sedentary behaviour between the arms (see Appendix 8, Table 62).
Sedentary behaviour bouts
At baseline, all residents engaged in sedentary bouts of at least 30 minutes’ duration. On average, residents engaged in at least one 30-minute sedentary bout on 6 of the days that they wore the accelerometer (see Appendix 8, Table 65) [the average number of days’ wear was 6.9; on each of these days residents had, on average, a mean of 6.4 (SD 1.6) sedentary bouts in the MoveMore arm and 5.9 (SD 1.9) sedentary bouts in the UC arm (see Appendix 8, Table 65)]. The duration of the sedentary bouts was similar between arms, lasting, on average, 1.5 hours before the bout was broken by a period of PA, even if this was for only 1 minute.
The number and duration of 60-minute sedentary bouts was also similar between the arms at baseline (see Appendix 8, Table 66), although residents in the MoveMore arm appeared to engage in 60-minute sedentary bouts on more days than residents in the UC arm (see Appendix 8, Table 66). Therefore, although residents in the MoveMore arm appeared to spend a greater percentage of their day sedentary at baseline, there was a suggestion that the difference was in shorter bouts.
Changes in bouts of sedentary behaviour were observed in both arms during follow-up. At 9 months, residents in the MoveMore arm engaged in 30-minute sedentary bouts on the same number of days and had the same number of bouts per day as at baseline, but the duration of these bouts was shorter (see Appendix 8, Table 65). Residents in the UC arm engaged in 30-minute sedentary bouts on fewer days at 9 months than at baseline, but had more bouts per day, although the duration of these bouts was also shorter (see Appendix 8, Table 65). For the 60-minute sedentary bouts, a similar pattern was observed. Residents in the MoveMore arm also engaged in these bouts on fewer days at 9 months than at baseline, and had fewer bouts per day at 9 months than at baseline (see Appendix 8, Table 66).
Variation in outcomes between care homes
The intracluster correlation coefficients (ICCs) (see Appendix 8, Tables 56–59) provide an estimate of the amount of variation in each outcome, explained by the variation between CHs. These data inform sample size calculations for a definitive trial. In this feasibility study, we had a small number of CHs (clusters) with varying cluster size, with a maximum of between three and 20 residents per home, which led to an unbalanced design, for which there is limited research on the performance of ICC estimates.
Individual-level profiles
Displaying the profile of individual residents’ activity in CHs allowed us to examine whether there were any observed changes that may or may not be reflected at the level of the CH. It also allowed us to see the contribution of each resident to analysis at the different time points. We chose sedentary behaviour variables, as these had a larger sample in the population.
There was a large amount of variation between residents in all homes in both arms when examining the percentage of time per day spent sedentary (see Appendix 8, Figures 14 and 15). In particular, in the MoveMore arm there was marked fluctuation in individuals’ sedentary behaviour over the study duration. However, there did appear to be a number of residents in CHs in the MoveMore arm who showed a decrease in the percentage of time spent sedentary, most notably in CH3 and CH4 up to the 6-month follow-up (after which sedentary behaviour increased again) and in CH5 between the 6- and 9-month follow-ups. In the UC CHs, there was a clear increase in the percentage of time spent sedentary per day for all residents in CH7, CH8 and CH11, whereas, in the other CHs, the percentage of time spent sedentary stayed at a similar level or increased slightly. The presence of an activity co-ordinator did not appear to affect residents’ profiles.
The number of breaks in sedentary behaviour per day also showed variation between residents within homes and for individual residents across the study duration (see Appendix 8, Figures 16 and 17). The most notable change in the MoveMore CHs was a general decreasing trend for the majority of residents in CH5 up to 6 months, after which time the number of breaks increased, in line with the observed decrease in the percentage of time spent sedentary.
Completeness of follow-up questionnaire data
Questionnaires completed by the researchers with staff informants (i.e. the FAC, the BI and the PAM-RC) had a high completion rate, and completion levels were similar between arms at all time points (96–100%) (see Appendix 7, Tables 40 and 41). The time taken to complete these questionnaires was constant across arms and time points, with each questionnaire taking, on average, 1–3 minutes.
The EMS was completed by the researchers with staff informants, but also included two physical assessments (timed walk and functional reach). Completion levels for the EMS were variable (see Appendix 7, Tables 40 and 41). At each time point, the two physical assessments had lower completion rates (86–97%) than the other questions in the EMS (95–100%). The most common reasons for non-completion of these two physical assessments were that the resident declined to do them, the resident did not understand what they were being asked to do or was unable to follow instruction, and asking the resident to do these was not suitable because they were very frail, unwell or too tired. Hence, the pattern of completion observed between the arms was consistent with residents in the MoveMore arm having lower cognitive ability at baseline and those with higher cognition being included in the follow-up in both arms.
Among those questionnaires completed by the researcher with the resident (i.e. the GDS, the WHOQOL-OLD, the DEMQOL, the EQ-5D-5L and the 6-CIT), the level of completion was variable, ranging from 33% to 74% (see Appendix 7, Tables 42 and 43). Completion differed between the study arms: for all questionnaires at all time points, completion levels were higher in the MoveMore arm. The most commonly reported reasons for non-completion of the resident-completed questionnaires included staff members and NCs advising that the resident would struggle to understand questions or would be unable to communicate verbally, lack of co-operation or response to the questions, and the resident not being well enough to be approached.
The DEMQOL and the 6-CIT appeared to have slightly poorer completion rates than the GDS, the WHOQOL-OLD and the EQ-5D-5L (completion rates: DEMQOL, 34.1–64.0%; 6-CIT, 32.9–62.0%; GDS, 40.0–66.0%; WHOQOL-OLD, 34.3–69.8%; EQ-5D-5L, 42.9–74.0%).
As would be expected, staff proxy-completed questionnaires had a higher rate of completion than the resident-completed versions (completion rates for resident-completed vs. proxy-completed: DEMQOL, 34.1–64.0% vs. 82.4–100.0%, respectively; EQ-5D-5L, 42.9–74.0% vs. 91.4–100.0%, respectively) (see Appendix 7, Table 44).
The completion of the staff P-CAT was variable in both arms at all time points, with scores available for all but one staff member of those who returned the questionnaire booklets in the MoveMore arm at 3 months (see Appendix 7, Table 45). At baseline, completion levels were similar between the arms, but, at 6 and 9 months, rates of completion were lower in the UC arm. Examination of the item-level completion indicated that the questions on whether or not the ‘environment feels chaotic’ (question 8) and ‘assessment of residents’ needs is undertaken on a daily basis’ (question 11) had lower levels of completion in both arms at all time points (see Appendix 7, Table 45).
Statistical outcomes
Assessment of physical activity outcome
There is limited research available on PA in this population to inform choice of the cut-off points for low-intensity PA or sedentary outcomes. We therefore planned to use the data generated to determine appropriate PA end point(s) for future use in a definitive trial. This decision was to be made following a review of the summary statistics for each of the levels of PA and emerging evidence on physiological effects (e.g. that increasing the number of breaks in sedentary behaviour is more important than reducing the total amount of sedentary behaviour), and would also reference information on (1) numbers of missing data, (2) ceiling and floor effects and (3) sensitivity to change.
Based on the design of the REACH study, the most appropriate analysis and corresponding coefficient to assess sensitivity to change is a correlation of change scores with residents’ retrospective global ratings of change. However, this study was not designed to assess sensitivity to change; therefore, we do not have a global rating of change measure. In addition, although the number of residents wearing the accelerometer was much higher than in other research conducted in this population, the numbers of registered residents wearing an accelerometer and achieving the minimum wear time criteria required for analysis was relatively low for informing a primary outcome. Hence, it was not feasible to investigate this to inform the most appropriate PA end point.
Estimation of effectiveness
Following discussions that it was not appropriate to make a statistical decision on the most appropriate PA end point(s) for future use in a definitive trial, planned analyses on the preliminary estimate of effectiveness were not conducted. Furthermore, it was also inappropriate to conduct any further formal cluster-level analysis on the accelerometer data. At 9 months, the number of residents per cluster ranged from 2 to 14 (mean 7.0) for sedentary outcomes, whereas, for the light-intensity outcomes, there were fewer than four homes per arm; therefore, a formal cluster-level analysis would not produce any meaningful conclusions. Cluster-level analysis is the only recommended approach to analysis with a small number of clusters per arm.
Assessment of questionnaire outcomes (see Appendix 7, Table 46)
There was no evidence of a significant difference in EMS scores between the two groups, although residents in the MoveMore arm had lower EMS scores at baseline, indicating lower mobility. During the study, scores decreased in both arms, with evidence of a difference emerging between the arms from 6 months, with lower scores in the MoveMore arm (difference 3.23, 80% CI 0.25 to 6.22), but caution is required in interpretation given the differing response rates. The BI and PAM-RC scores were significantly lower in the MoveMore arm at baseline, indicating less self-care, physical ability and PA. During the study, scores fluctuated in the MoveMore arm and decreased in the UC arm, such that, by 9 months, there was no evidence of a difference between the arms (BI: 2.55, 80% CI –0.43 to 5.52; PAM-RC: 2.06, 80% CI –0.28 to 4.41).
Sample size estimation
To inform the sample size estimation for a definitive trial, information is required on the average cluster size and coefficient of variation, as well as an estimate of the ICC for the proposed outcomes.
The mean cluster size, as defined by the number of registered residents per CH, was 12.4 (SD 4.51) in the MoveMore arm (62 registered residents; five CHs) and 13 (SD 5.69) in the UC arm (91 registered residents; seven CHs). These correspond to a coefficient of variation in cluster size of 0.36 in the MoveMore arm and 0.44 in the UC arm.
As outlined in Variation in outcomes between care homes, the ICC estimates for the PA outcomes, particularly at 9 months, were not reliable based on such a small number of CHs and residents in CHs. The ICC estimates and 95% CIs for the various resident questionnaires are provided in Appendix 7, Tables 46 and 47. However, as with the PA outcomes, the ICC estimates for the questionnaires completed with the resident were not reliable because of the reduced numbers of residents completing these questionnaires.
Safety reporting
Falls
At baseline, a higher proportion of residents at the CH level in the MoveMore arm than in the UC arm experienced falls in the previous 3 months, and the average number of falls per resident was also higher, although not significantly (see Appendix 7, Table 48). Estimates at the CH level were consistent with the proportions and average fall rate observed among registered residents. The average number of falls per resident was also higher (MoveMore arm mean 2.50, 95% CI 2.00 to 3.00; UC arm mean 1.62, 95% CI 1.10 to 2.13), although not significantly (see Appendix 7, Table 49).
Over the study period, at the CH level, the average number of falls per resident declined in both arms, although not significantly, and there was no difference at 9 months between the arms (see Appendix 7, Table 48).
Among registered residents, over the study follow-up, the proportion of registered residents who fell was similar to that observed at baseline (MoveMore arm, 43.5%; UC arm, 38.5%). In both arms, there was, however, an increase in the average number of falls per resident (MoveMore arm mean 3.37, 95% CI 2.03 to 4.71; UC arm mean 2.00, 95% CI 1.57 to 2.43), although the CIs indicate that these increases were not significant, compared with baseline, and there was no difference in the average fall rate between arms (see Appendix 7, Table 49). In both arms, the reasons for falls among registered residents were largely unknown, as residents were commonly found on the floor. In cases for which the reasons were known, the majority had fallen from their bed.
Hospitalisations
At the CH level, at baseline, the number of registered residents with hospitalisations and the number of hospitalisations per resident over the previous 3 months were similar between arms [number of residents with hospitalisations: MoveMore arm, 8.8% and UC arm, 9.2%; number of hospitalisations per resident: MoveMore arm mean 1.64 (95% CI 1.33 to 1.95) and UC arm mean 1.47 (95% CI 1.34 to 1.61] (see Appendix 7, Table 50). At follow-up, there was an increase in the proportion of residents admitted to hospital in both arms, whereas the number of hospitalisations per resident decreased in the MoveMore arm and increased in the UC arm. Hence, the proportion of residents with hospitalisations and the average number of hospitalisations per resident was lower in the MoveMore arm at follow-up: approximately one-quarter of residents were hospitalised with, on average, 1.60 and 1.27 hospitalisations per resident in the UC and MoveMore arms, respectively (see Appendix 7, Table 51).
When examining the NHS Digital data for hospital admissions among registered residents (see Appendix 7, Table 50), there are marked differences, compared with CH reporting, particularly in the MoveMore arm (see Appendix 7, Table 51). Both the number of hospitalisations and the number of residents with hospitalisations were under-reported via the CH, compared with NHS Digital (proportion of residents with hospitalisations: MoveMore arm, 38.7%; UC arm, 35.2%), although, at the CH level, there were a few homes across both arms for which the number of hospitalisations agreed. In the UC arm, the number of hospitalisations was similar from both sources, but the number of residents with hospitalisation was higher according to NHS Digital. Hence, in contrast to the CH reports, the average number of hospitalisations per resident was higher in the MoveMore arm and in line with the average number of hospitalisations per resident at the CH level. The number of unplanned admissions at the CH level was also under-reported via the CH, compared with NHS Digital. However, this may be because CH-level data from NHS Digital were obtained via the CH postcode, and therefore may include data from those not resident at the CH.
Accident and emergency visits
The mean number of accident and emergency (A&E) visits at the CH level over the study period for each arm was as follows: MoveMore arm, 1.45 (95% CI 1.27 to 1.64); UC arm 1.57 (95% CI 1.40 to 1.74) (see Appendix 7, Table 50). At follow-up, the mean number of visits was 1.22 (95% CI 0.88 to 1.56) for the MoveMore arm and 1.26 (95% CI 0.99 to 1.53) for the UC arm (see Appendix 7, Table 52).
The mean number of A&E visits per registered resident for each arm at baseline was as follows: MoveMore arm: 1; UC arm 1.07 (95% CI 0.92 to 1.23). At follow-up, the mean number of visits was 1.22 (95% CI 0.88 to 1.56) for the MoveMore arm and 1.26 (95% CI 0.99 to 1.53) for the UC arm. The number of residents with an A&E visit appeared to be lower in the MoveMore arm [n = 5 (8.1%)] than in the UC arm [n = 14 (15.4%)] (see Appendix 7, Table 52). The number of A&E visits reported via NHS Digital was much higher than that reported via the CHs. (see Appendix 7, Table 52).
Deaths
The number of deaths was similar between both arms over the study period: MoveMore arm, 29 (6.9%); UC arm, 31 (6.5%) (see Appendix 7, Table 50).
Among registered residents, a similar proportion of deaths occurred in both arms: MoveMore arm, 19.4%; UC arm, 17.6% (see Appendix 7, Table 53).
Further analyses
Researcher unblinding
There were 11 instances of researcher unblinding. One instance occurred between baseline and the 3-month data collection via telephone calls from CH staff requesting to speak to an unblinded researcher, and another at the 9-month data researcher visit. Two instances occurred during the monthly safety calls, during which the researchers were informed of the allocation by CH staff. The remaining instances occurred at the 6-month researcher visit: allocation was revealed during discussions with staff (three instances), by residents (two instances) and via the display of the intervention materials in the CH (two instances).
Process evaluation
For a full description of the PE, see Appendix 9.
Aims and objectives
The purpose of the PE in this feasibility trial was to test and refine the theory of change underpinning the programme, and to explore how and what was delivered over time, the factors that contributed to and/or inhibited change and the programme’s feasibility and acceptability in a CH setting. A short summary is provided in this section, with full details in Appendix 9.
Research design
We adopted a multimethod, comparative case study design78–81 (see Appendix 9, Research design).
Methods
For full details, see Appendix 9, Methods.
All homes
In each home, the PE researcher observed care delivery during baseline to develop a picture of the care environment (≈ 5 hours per home). Completion of a purposely developed pro forma provided a snapshot of movement in both intervention and control homes at each data collection point; interviews were conducted with senior staff following the 9-month data collection period.
Intervention homes
The PE employed multiple methods to examine the process and content of MoveMore implementation as it evolved over time: observation and informant conversations with staff and residents during the preparatory and implementation phases (a total of ≈ 15 hours in each intervention home), analysis of audio recordings of workshop proceedings and documents (completed observations, action plans and reviews), qualitative interviews with implementation team members to explore the process of change over time and the factors constraining or facilitating this change, and conversations with residents.
Analysis
For full details, see Appendix 9, Analysis, Research team roles and relationships, A sensitising framework, and Implementation fidelity.
We employed an interpretive approach to analysis, using grounded theory methods of simultaneous data collection and analysis, constant comparison, searching for negative cases and memo writing. 82
The NPT framework was used as a sensitising lens, with the aim of understanding the degree to which MoveMore may have become embedded in routine practice. Examination of fidelity to the intervention as intended was complicated by the dynamic nature of the CH environment, as well as the intended flexibility of the MoveMore programme. Adherence was thus to be explored across two levels: engagement of the implementation team with the workshops, and the reach of the programme beyond the implementation team to effect change at CH level.
Results
For full details, see Appendix 9, Findings.
Usual care
For full details, see Appendix 9, What is usual care?.
In the majority of homes at baseline (n = 9), staff showed meaningful knowledge of residents, which was reflected in their daily encounters with residents. Six homes adopted a consistently enabling approach in most tasks of daily living; in a further four homes, practice was inconsistent between staff: enabling in some tasks but not in others. In two homes, overall, practice was characterised as not enabling: it was ‘care done to’ individuals, often involving little or no encouraging talk. All homes adopted some flexibility with regard to some aspects of day-to-day practice. For those who were dependent on carer support to wash and dress, the degree of flexibility was constrained by staff availability. Overall, most care managers conveyed a general belief that ‘exercise’ and keeping ‘active’ was a ‘good thing’ to maintain residents’ well-being and to facilitate their engagement in social life. By contrast, the conception of movement as part of everyday life activities was not understood. Homes varied considerably in the opportunities available for engaging in social, leisure, and stimulating or meaningful activities. Not all homes had dedicated activity organisers (AOs) in post, and even those that did (three of five intervention homes and 5/7 control homes) varied in the level of resource available. Of those CHs without AOs, there were spontaneous short-interval activities (music and singalong, games, chair exercises) and organised medium-interval events using a combination of external resources [e.g. Music for Health (www.musicforhealthltd.co.uk/), exercise class] and CH staff (e.g. film nights, reminiscence). In all homes, care staff engaged in one-to-one pampering work (e.g. manicure) and there was access to a hairdresser/barber.
Intervention care homes
For full details, see Appendix 9, MoveMore implementation and Stages of implementation.
Intervention CHs were categorised as full, partial or failed implementers, depending on how far the CH progressed from exploring the programme through installation and initial implementation to full adoption, innovation and sustainability.
Full implementers
Two homes proceeded to full adoption of the programme (CH4 and CH5). Installation of MoveMore was pursued through participation in the workshops, and each step in the change process was taken back and enacted in the CH environment (observation); this was then reflected on in the subsequent workshop (action-planning) and the action plans that had been developed were tried out in the home and then reviewed (review and forward movement). In each case, action plans embraced action relating to individual residents, changes in the care environment and mechanisms to embed changes in care routines (incorporating movement in a review of the content of care plans, introducing systems for communicating action on movement, and training and supervision for all staff). These ‘full implementer’ homes had, during the period of the trial, moved a little beyond the stage of ‘full adoption.’ They had begun to harness the change process in such a way that it was feasible for them to embed aspects of change into their existing systems and procedures. This had the potential to embed movement in routine practice.
Although the process of implementation differed between the two homes and was affected by contextual factors, there were common features. These included strong, committed leadership to provide a steer to take the work forward; use of the observational tool among team members and in the wider staff group to engage staff in building a shared understanding of existing practice and what needed to change to enhance movement and extend the programme’s reach beyond the implementation team; and use of the implementation process to further multiple objectives.
Partial implementers
Two homes were ‘partial implementers’ (CH1 and CH3). Installation of MoveMore was pursued intermittently over a lengthy time span, including extended periods of inaction between participation in the workshops. First steps in the change process were taken back and enacted in the CH environment (observation) and reflected on in the subsequent workshop (action-planning). Some limited work was tried out with action plans in the home and then reviewed. CH1 proceeded in the direction of ‘full adoption’, although it did not quite attain it. In CH3, the focus of implementation was limited to action within the work spheres of the care staff who drove it forward; installation did not proceed beyond trying out one-off initiatives. Action was not pursued over time in either home, nor did action result in practice change at the CH level.
In CH1, contextual factors at the CH level resulted in other priorities taking precedence, and the absence of senior staff for prolonged periods during implementation meant that team members assumed different roles and relationships that negatively affected their capacity to steer the programme. A strategy to engage the newly appointed AO in the work of steering the programme and integrating movement in social and leisure activities was only partially successful: the post-holder was also in the process of developing the role and building relationships with care staff in relation to it. Overall, the intervention was conceived of as not ‘timely’ to implement in the context of what was happening in the home, albeit beliefs and intentions regarding its aims were sustained.
In CH3, at senior level, the conception of MoveMore as an intervention that necessitated joint work with staff to build a shared understanding of the value of movement, and to contribute to the work to make it happen, did not occur. Although individual care staff were enabled to pursue implementation within their own work sphere, active support to engage the wider staff team was not pursued.
Failed implementer
Care home 2 was a ‘failed’ implementer. Although three workshops were provided, what emerged over time was that implementation team members did not share an understanding of existing practice regarding ‘movement’ as a ‘problem’ that needed to be addressed. In particular, the nominal lead of the implementation team, although recognising that more could be done to reduce residents’ sedentary time, considered that existing systems were adequate to achieve this (senior staff mirroring good practice). Although individual care staff in the team held a contrary view, they lacked the legitimacy and power to take it forward. MoveMore was not understood as meaningful to pursue in terms of the knowledge, behaviour and actions required to implement it. In addition, contextual factors operating in this home resulted in a confluence of negative factors affecting care delivery.
Health economic study
Background
The feasibility of collecting cost and outcome data for use in a future evaluation of the cost-effectiveness of the MoveMore intervention was explored. An exploratory cost-effectiveness analysis was undertaken to provide insight into potential cost drivers, to identify where there may be potential differences between MoveMore and UC, and to show how a cost-effectiveness analysis would be feasible as part of a full trial. The exploratory economic evaluation is presented in its entirety in Appendix 10.
Methods
For full description of the methods, see Appendix 10.
Aims
The primary aim was to assess the feasibility of collecting cost and outcome data for use in a future evaluation of the cost-effectiveness of the MoveMore intervention.
Perspective and time frame
The study adopted a health-care and Personal Social Services perspective.
Measurement of outcomes
Residents’ responses to the EQ-5D-5L questionnaire were collected at baseline and at 3, 6 and 9 months post randomisation. Proxy responses to the EQ-5D-5L questionnaire were also obtained at each of these time points.
Measurement of resource use
All health-care resource use was estimated from the perspective of the health-care and personal social service provider and was collected for the trial period of 9 months from randomisation using resident-completed questionnaires and hospital records. This included primary care, such as GP visits and nurse home visits, as well as secondary care, such as outpatient visits and other hospital admissions.
Results
For a full description of the results, see Appendix 10.
Sample
Of the 153 residents recruited to the trial, 126 participants had complete resource use and EQ-5D-5L results for all follow-ups.
Measurement of outcomes
Resident self-reported and proxy-reported EQ-5D-5L scores are presented in Appendix 10, Table 71. In both arms of the trial, the changes in EQ-5D-5L score over the trial period were small. Proxy-reported scores were consistently lower than those reported by residents.
Measurement of resource use
The average health-care resource use of residents in each arm, over the 9 months of the trial, is presented in Appendix 10, Table 67. Unplanned GP and A&E visits were consistently less frequent in the MoveMore arm. However, all differences in resource use between arms were small.
Missing data
Resource use questionnaires were completed for 129 residents for all follow-ups. A total of 43 residents had complete self-reported EQ-5D-5L scores across all time points and 98 residents had complete proxy-reported EQ-5D-5L scores across all time points. Initially, completion of resource use and proxy EQ-5D-5L was very good (baseline: UC arm, 100% proxy EQ-5D-5L completion and 91–100% resource use completion; MoveMore arm, 98% proxy EQ-5D-5L completion and 73–100% resource use completion), but this started to trail off over the trial period (9 months: UC arm, 70% proxy EQ-5D-5L completion and 69–77% resource use completion; MoveMore arm, 66% proxy EQ-5D-5L completion and 61–68% resource use completion). Completion of the self-reported EQ-5D-5L followed a similar trend, but also started from a low baseline rate: at baseline, completion of the EQ-5D-5L was 53% in the UC arm and 68% in the MoveMore arm; at 9 months, it was 36% in the UC arm and 47% in the MoveMore arm.
Considering self-reported and proxy-reported EQ-5D-5L scores together, there was one (< 1%) missing EQ-5D-5L score at baseline. A total of 42 (9%) scores were missing across the remaining follow-ups (months 3–9).
Health economic discussion
Principal findings
Health economic data collection tools were developed and successfully implemented. Of the 153 residents, 129 residents completed health-care resource use questionnaires for all follow-ups, 43 residents had complete self-reported EQ-5D-5L results for all follow-ups and 98 residents had complete proxy-reported EQ-5D-5L scores for all follow-ups. Completion of resource use and proxy-reported EQ-5D-5L was 100% at baseline, but decreased over the course of the trial. Completion of the self-reported EQ-5D-5L followed a similar trend, but also started from a low baseline (53% in the UC arm and 68% in the MoveMore arm). However, considering self-reported and proxy-reported EQ-5D-5L scores together, < 1% of residents were missing EQ-5D-5L scores at baseline, and 9% of scores were missing across the remaining follow-ups.
Strengths and weaknesses of the economic analysis
The analysis conducted for this feasibility trial has shown that collection of cost and outcome data would be feasible as part of a full trial. However, it is noted that for both quality-of-life and resource use data, compliance decreased over the duration of the feasibility trial. Consequently, if a full trial was conducted, ways to maintain compliance should be explored, for example altering the frequency of questionnaires to address questionnaire fatigue.
A further limitation lies in the acceptability of using proxy- and self-reported EQ-5D-5L scores. This was necessary given the frailty of residents in this trial, but is problematic because of potential differences in self-reported and proxy-reported scores. Although self-reported and proxy-reported scores were significantly correlated, scores reported by proxy appeared lower than those that were self-reported. Previous work relating to the impact of the use of proxy-reported quality of life is relatively inconclusive, with some studies arguing that proxies provide an acceptable source of data,83,84 whereas others suggest that there is too much variation between proxy- and self-reported scores. 85 The impact of using proxy- versus self-reported EQ-5D-5L scores was explored in sensitivity analyses, but should be explored further in a full trial analysis, as the relatively small sample size in this feasibility study means that it is not possible to draw firm conclusions.
Workstream 5: discussion and conclusions
Recruitment and follow-up
Care homes
Through our systematic, standardised and inclusive procedures, a range of CHs were recruited in terms of size, location, ownership and provision, so we believe that our cohort is generalisable to CHs across the UK.
However, a significant amount of time and resource was required to recruit CHs to the REACH study. The reasons for this included the following: a poor response by CHs to the first invitation letter; contemporaneous changes to the CQC inspection process and the continual flux of the CH sector required repeated checking of the CQC status of CHs, as CHs that were initially eligible may subsequently have become ineligible in a short space of time; maintaining the interest of CHs required frequent contact from the researchers; obtaining signatures from both the CH manager and owner on a formal letter of agreement (necessary for CH participation) was sometimes problematic and time-consuming; sustaining the interest of CHs in the study in a protracted process involved repeated contacts (face-to-face meetings and telephone calls) between the initial expression of interest and researchers gaining access to the CH to screen residents; and the relatively high burden on CH staff for data collection and the requirements of the intervention were important considerations for CH managers: too great for some, but others saw the requirements of the intervention as ‘free’ training.
Streamlining the recruitment processes (i.e. simplifying the letter of agreement for CH owner/head office approval that was required to access the CH) expedited recruitment.
Residents
We adopted a comprehensive approach to recruitment, including seeking agreement from PCs and NCs, to maximise resident participation. Through this, we successfully achieved the recruitment target.
There were idiosyncrasies in the CH setting. For example, in one CH, residents tended to sit together in a lounge, and appeared to influence each other when considering study participation. Communicating with PCs was time-consuming, resulting in extended periods of recruitment: the average time for recruitment at the CHs was 64 days (range 50–97 days). An additional difficulty was the stability of managers/staff in the CHs: the process of recruiting residents was easier in CHs with staff stability (because of knowledge of the study). Finally, as with trials in other settings, there were seasonal differences, for example Christmas affected processes at CHs 1, 2 and 7, resulting in longer screening durations in these CHs than in other CHs.
All 300 residents in the 12 participating CHs were screened for broad eligibility criteria, commensurate with the CH-wide nature of the intervention. A total of 278 (92.7%) residents met the eligibility criteria; only 22 (7.3%) residents did not. Thus, nearly all residents in the participating CHs had the opportunity to participate. In addition, all eligible residents but one had an assessment of capacity and, therefore, the opportunity to enter the trial.
The recruitment rate of eligible residents to the study was 57%, consistent with rates of 32–84% quoted in other studies,86–92 but varied between the CHs (40–89%). A particular consideration for the residents and PCs approached for the study was the acceptability of the activity monitor (accelerometer). Although residents could still be involved if they declined to wear the device, some residents and PCs still expressed reservations. It is unclear how many may have declined for this reason.
The majority of eligible residents had doubtful or lacked mental capacity [n = 203 (73.0%)], which was higher than the number of residents who had a formal diagnosis of dementia [n = 194 (64.6%)]. This emphasised the importance of the careful recruitment processes, including assessment of mental capacity. More than half (57.1%) of those residents who lacked capacity, or whose capacity was in doubt, were recruited to the study (116/203), compared with 59.7% of residents with capacity (43/71), strengthening the external validity of the study. The recruitment rates via PCs and NCs were similar (57.9% and 56.6%, respectively), justifying both the lengthy procedure involved in asking PCs and the use of NCs, thereby giving residents without mental capacity to consent the opportunity to participate in the study, which is especially important as they form a high proportion of CH residents.
The screening characteristics of eligible residents who consented/had consultee agreement and those who did not consent/have consultee agreement were similar, except that a higher proportion of residents with a diagnosis of dementia consented or had consultee agreement to participate (69.8% vs. 59.3%). This indicates that the recruited residents could be considered a representative sample.
Resident recruitment rates varied between the CHs (40–89%). There was no evidence of bias in the recruitment process: similar proportions of residents gave consent (59.7%), or were recruited via PCs (57.9%) or NCs (56.6%). However, as there were more residents without capacity, a higher proportion of recruited residents did not have capacity [111/159 (69.8%)].
Although we achieved the overall recruitment target, the number of residents recruited in the CHs was small, varying from 6 to 22. The procedures and the context made it difficult to predict how many residents would ultimately be recruited from a CH. Many meetings (which included discussion of the potential number of residents to recruit) and the signing of a collaborative agreement preceded researchers undertaking any recruitment activities. Recruitment activities involved review of capacity, obtaining PC or NC opinion, then undertaking outcome assessment, including wearing of an accelerometer, all prior to finally registering the resident in the trial. (Once this baseline activity was complete, the CH was randomised.) Thus, there were many opportunities for the number of potential participants to diminish, in addition to, unfortunately, in some cases, deaths of residents. The cluster design led to differences in baseline characteristics of the residents, with a higher proportion of residents in the MoveMore arm with a history of stroke and with a lower level of physical function, which reflected differences observed between the arms in the screening populations. In addition, those in the MoveMore arm also had greater cognitive impairment and more comorbidities.
We have demonstrated that it is possible to recruit older CH residents to a cluster RCT, without bias, including those with frailty and cognitive impairment with mental capacity and those with frailty and cognitive impairment without mental capacity. However, this process was time-consuming and resource heavy because of the complexities involved in engaging with residents, PCs and NCs. This has implications for the planning and resourcing of similar future studies.
Randomisation/stratification
Thirteen CHs provided consent and 12 were randomised (one CH was not randomised because the recruitment target was already met). Unfortunately, owing to the small number of clusters randomised, the stratified randomisation process did not achieve balance on sample size per arm. Hence, for a future definitive trial, alternative methods of randomisation should be considered.
Although, overall, the consenting residents had similar characteristics to the whole screened population, and therefore can be considered a representative sample, there were differences in the screened and recruited populations between the two arms in history of previous stroke and physical function. For a future definitive trial, randomisation of CHs stratified by baseline stroke, physical function and cognitive impairment of residents should be considered.
Follow-up
Forty residents (26.1% of registered residents) were lost during the trial (28 residents died and 12 moved out of the CH). For a definitive randomised trial, therefore, it may be worth considering an open cohort study design, particularly if the follow-up duration is longer.
Care home and staff characteristics
Information on staff demographics was obtained via completion of staff booklets, which were distributed to all staff who had face-to-face contact with residents. However, overall return rates for the booklets were low (20–39%), with a higher proportion of staff in the UC CHs completing the booklets at each time point. Hence, despite extensive efforts and the multiple methods used, this would not be a robust method for capturing staff demographics in a definitive trial.
Intervention delivery
Time scales for intervention delivery
In practice, delivering the workshops took far longer than anticipated: only one CH had completed all three workshops within 3 months of randomisation; for three CHs, the workshops spanned > 6 months. We learned over time how to improve the efficiency of delivering the intervention to the CHs. We used a number of strategies to improve this efficiency of implementing the intervention. These strategies included adding an initial meeting between the intervention team and the research lead at the CH to introduce MoveMore and the manual, and to discuss with the CH research lead who in the CH would be appropriate MoveMore team members. In addition, to avoid delays in the implementation of the intervention, we refined the contact processes with the CHs by fixing dates for both the first and second workshops, rather than for the first workshop only, at this initial meeting. This learning should be transferred to a definitive trial, as well as further consideration of the timing and duration of follow-up.
Completeness of MoveMore documentation
The requirements of documentation were considered overly onerous for most participants in this setting. Simplification of the tools and alternative methods for documenting them (e.g. audio-recording), need consideration and testing for a full trial.
Intervention implementation
The detailed PE provides considerable insights into barriers to and facilitators of intervention delivery (see Appendix 9). The workshops provided a forum to create a shared understanding of what needed to change and to generate ideas about goals, priorities and creative solutions from different perspectives to make change happen. This included the innovative work of the artist in capturing and communicating ideas for change in the home environment. Nevertheless, the active role of the implementation team as a vehicle for creating a shared understanding about and goals for action was insufficiently emphasised in presenting the programme. It was notable that, in some homes, rich discussion in the workshops of ideas for action to increase movement did not translate into action plans. This will be addressed in future refinements of the intervention.
Usual care varied across the CHs. At baseline, half the homes adopted an enabling approach to ADL and movement. At the other CHs, this practice was less evident and was variable across staff. Multiple factors affected whether or not CHs were able to promote independence in this way, including resident dependency, environment, care staffing levels and the autonomy senior staff allowed carers in their work.
Assessment of outcome measures
Collection of the anonymised BI and PAM-RC scores at screening (baseline) was successful for all residents and provided important information at the level of the home. Unfortunately, we were refused ethics permission to collect this anonymous data (BI and PAM-RC) at follow-up points. However, following subsequent discussions, this has been agreed for another CH-based study.
Given the difficulties of recruiting all participants to CH studies, gaining this anonymised data does provide important contextual information on the representativeness of the recruited participants and assessment of the impact of the intervention. Questionnaires completed by the researchers with staff informants had a high completion rate, but, perhaps not surprisingly, the level of completion for questionnaires completed by the researcher with the resident was poor and variable, primarily because of levels of capacity. Identifying and optimising completion of appropriate outcome measurements in this population is challenging.
As the intervention focused on increasing PA, our focus was on the carry-over of this increase in PA to enhancing residents’ physical and psychological outcomes. The activity monitor captured levels of PA. The BI and the PAM-RC were appropriate tools for capturing how this translated into meaningful activity. In this population, maintenance of activity may also be considered a positive outcome.
Consideration could be given to a recommended, simplified, core outcome set that would facilitate data collection in this population.
Levels of physical activity
Variations in outcome between care homes
The ICCs, which provide an estimate of the amount of variation in each outcome explained by the variation between CHs, were estimated using mixed-effects models, which assume a normal probability distribution for the cluster means. However, with such a small number of clusters, this assumption does not hold. Ukoumunne93 demonstrated, through simulation studies, marked non-normality in cluster-level random effects, which compromised the performance of the methods used to estimate the ICC and associated CI. In addition, a minimum of four clusters per arm is required to be able to draw any meaningful conclusions about the effect of an intervention. 94 Hence, we are unable to use the ICC estimates and CIs to inform sample size calculations for a definitive trial.
Safety reporting
Delivery of the intervention did not raise any concerns about the safety of the intervention. However, the data collection was resource intensive, as standardisation of routine data collection across homes is limited. For example, staff in CHs use a range of different definitions (e.g. whether or not to class as a ‘fall’ an instance when a resident has been unobserved but found on the floor), and reporting for the monthly safety checks sometimes relied on staff recall. Clarity of definitions would be helpful, but would be difficult across CHs given their different administrative and management structures.
Progression criteria
Recruitment and follow-up
Twelve CHs were recruited, and 53% (159/300) of screened residents consented to take part in the trial. The number of residents recruited per home varied from 6 to 22, with an average of 12.75 residents recruited per home. The green criterion for recruitment was therefore met.
Loss to follow-up was 31% (19/62) in the MoveMore arm and 23% (21/91) in the UC arm, giving an overall loss to follow-up of 26%. Therefore, for follow-up, the amber criterion was met (see Report Supplementary Material 9).
Intervention delivery
All CHs completed the series of three workshops. Three of the five intervention CHs (60%) were recorded as having completed at least one observation review and one action plan via the data collection forms completed at each follow-up by the researcher (see Report Supplementary Material 9). The detailed PE indicated that two homes were ‘full implementers’ of the intervention, two others were ‘partial’ implementers and one was a ‘failed’ implementer. Overall, the criterion is amber.
Data collection and follow-up
In summary, at 9 months, 52.2% of residents available (59/113) provided valid accelerometer data. Sixty-six per cent (59/90) of residents who agreed to wear an accelerometer provided valid data. Based on a non-wear definition of 120 minutes of consecutive zero counts, as predefined in the statistical analysis plan, the proportion of residents providing useable accelerometer data (i.e. that met the minimum wear criteria) was 72.5% in the MoveMore arm and 60% in the UC arm.
At 9 months, > 75% of residents had resident-reported outcome measures for those measures completed with a staff informant or a proxy. However, the outcomes completed by the residents themselves fell into the red criterion. The outcomes this relates to are the GDS, the 6-CIT and the WHOQOL-OLD. Hence, these questionnaires would not be suitable to use in a definitive trial (see Report Supplementary Material 9).
Patient and public involvement
The aim to place resident, CH staff and public involvement at the centre of this programme was chosen to enable us to develop an intervention that was appropriate to the needs of CHs and their residents. The initial idea for the programme was developed and refined with the Bradford Care Home Forum, a group of CH owners and managers who meet to discuss all issues relating to provision of services and support in their homes. The forum was facilitated by officers from Bradford Council, who provided considerable support in the set-up and identification of homes for the early WSs. This enhanced the credibility of the research team with CH colleagues.
We ensured our continued engagement of patient and public involvement (PPI) through a wide range of overarching strategies. These included having lay members on the Programme Management Group (Joan Firth, also a co-applicant) and the Programme Steering Committee (Marylyn Whelan), CH representation on the Programme Management Group (Bev Gallagher, NHS Clinical Quality Manager for CHs) and maintaining our links with the Bradford Care Home Forum. We also undertook a range of activities with the CHs, including attending open days, hosting coffee mornings and speaking at resident and staff meetings to optimise engagement with our work throughout the programme.
We attended the Bradford Older People’s Forum (a group of members of the public) to provide an update of the progress of our research. We also produced regular newsletters and bespoke feedback of WS outputs, which were circulated to CH staff and made available to residents and their relatives/friends.
In addition to these programme-level strategies, residents and CH staff inputs have been integral to each WS. In WS1, interviews and observations in the CH setting were undertaken, and resident feedback on outcome assessment was obtained in WS2 and WS3. The specifically convened intervention development advisory group in WS3 included CH staff, residents and residents’ relatives. The central tenet of our work was the development of a ‘whole-home’ intervention that would be owned and delivered by staff. To this end, staff and residents were engaged in the action groups of WS4 and the implementation teams of WS5.
Our embedded approach to PPI had considerable impact and influence on the programme. Joan Firth, lay applicant, has been committed to this work; throughout, she has seen herself as a representative of the residents and at all times tried to present their perspective in the many Programme Management Group debates over the years, which included review of ethics documents, outcome measures, information materials and research methods. Marylyn Whelan, lay member, also ensured that the ‘resident’s voice’ was heard on the Programme Steering Committee. Bev Gallagher’s very active involvement in the programme ensured that we were aware of the many organisational and care priorities within the sector. The Bradford Older People’s Forum and the Bradford Care Home Forum provided supportive feedback and the latter group also made us aware of other concurrent initiatives in CHs.
The interviews and observations in WS1 provided important context and perspective for the rest of the programme. The feedback from residents in relation to the appropriateness of proposed outcome assessments enabled us to gain a greater understanding of how residents interpreted questions and the meanings attached to their responses.
The input of the advisory group in WS3 was critical in discussing and understanding the findings from previous WSs. The group was heavily involved in generating simple practical ideas and strategies to increase PA in CHs based on our evidence, and providing continuous feedback in relation to the development and prioritisation of these. The engagement with residents and staff in WS3 helped inform the research team as to whether or not our intervention and chosen outcome measures were perceived as appropriate and were not considered an excessive burden by residents and staff.
We believe that we were successful in engaging PPI to underpin our programme. The coffee mornings were successful in raising awareness of our programme for residents, their relatives and staff, and provided an environment for informal queries. During the research process, it was challenging at times to engage with CH staff because of the time constraints they were under. A range of approaches were used to engage with residents, including keeping interactions short and providing short summaries. However, the most successful approach was the interaction with an artist in the resident and CH groups (WS4 and WS5). This prompted wider engagement, especially with ‘harder-to-reach’ residents and staff in the CHs. The feedback we provided to the homes participating in WS4 by creating tailored information sheets for each CH and residents were well received and appreciated by the CHs. Similarly, the tailored feedback provided to participating CHs and residents following the end of WS5 was greatly appreciated by the CHs. A meeting was arranged with each CH manager/research lead to discuss this document. This provided an additional opportunity to gather feedback on their views of the study processes and/or the intervention in a more informal way than the end-of-study interview.
As a programme team, we invested a lot of time and energy (assisted by Joan Firth) to optimise PPI. We believe that we were successful in this regard, and PPI has significantly affected all aspects of the development and implementation of this programme.
Dissemination
We will disseminate our findings through the Bradford Care Home Forum and seek their advice in relation to a preferred method of dissemination that might be used further afield.
Tailored written and verbal feedback was provided to all participating CHs during purposely convened meetings with residents and staff. Presentations have been made at CH conferences [School of Healthcare Education and Debate (SHED) talks, University of Leeds, February 2019]. Colleagues have attended the CH forum and provided feedback, and papers are in preparation.
Discussion
Undertaking research in CHs, although challenging, is extremely important, as CHs remain a key component of the services available to support older people. As in any setting, engagement in research will help enhance the care setting. Improvement in care may result from the research procedures (e.g. improving methods of recording falls in the CH), as well as the research outputs. We have delivered this programme of work according to the plans outlined in the application. Through this work, we have gained considerable insight into the complexities of providing care in this environment, the frailty of the residents, and the challenges of implementing change and undertaking research in this context.
The five WSs all provided useful and informative data.
Workstream 1 unpicked the dynamics of life in a range of different CHs. The study drew on the existing notions of the care environment and organisational culture as sensitising concepts with which to critically consider in-depth qualitative data on routine patterns of residents’ movement in the CH context. Bringing these two concepts together to help inform the analysis is a novel approach. It enabled us to strengthen, through the inductive and deductive cycles of grounded theory analysis, our conceptualisation of the organisational element of the CH environment, allowing us to build an explanation of the organisational structures and mechanisms that shape CH residents’ physical movement. The findings illustrate the importance of translating espoused values of care into tangible and acceptable care practices, systems of management, staff training and development, and the use of care-planning in residents’ routine patterns of movement. 39
Workstream 2 provided rare objective insights into residents’ activity levels. As a group, residents spent the majority of their time sedentary (90.5%) and the little PA they did engage in was predominantly of low intensity (9% of wear time). Accelerometer data also indicated the peaks (around mealtimes) and troughs of residents’ pattern of movement, providing pointers for opportunities to enhance movement. However, it must be noted that data collection was labour intensive for both researchers and CH staff. Researchers need a significant presence in CHs to enable the collection of high-quality data.
Engagement with CHs in WS1 and WS2 highlighted the physical frailty of residents and the high proportion of residents with cognitive impairment who were unable to provide informed consent in the population. To be as inclusive as possible, we adapted our consent procedures to include both PCs and NCs.
In the needs analysis (WS1), CH staff identified needs that were specific to different CH settings (e.g. homes of differing size and/or care provision); this informed the development of a more flexible intervention. We believe that this is likely to make the intervention more suitable for various CH settings, making it more probable that it will affect clinical outcomes if tested in a trial.
Intervention mapping was a useful and informative tool in the development of a provisional intervention in WS3. However, IM is a time-consuming and lengthy process (i.e. identification of outcomes, performance objectives and change objectives). We had a substantive number of qualitative data, which revealed multicomponent barriers to increasing and opportunities to increase movement of residents in CHs, and highlighted again that the needs for each CH are different. Therefore, the list of change objectives and associated strategies needed to be fairly comprehensive and risked becoming unwieldy. It was thus initially difficult to prioritise behavioural determinants that might be suited to varied and dynamic CH environments. We found the advisory group invaluable in the process of selecting the most relevant change objectives, which were indicated to be changeable and could be addressed within the scope of the intervention.
The provisional intervention was further refined and implementation strategies were developed in WS4. Engagement in this WS also emphasised the fragile nature of the setting, with unexpected managerial changes occurring in some of the homes. The heterogeneity of the CH population, as identified by the needs assessment of WS1, was an antecedent for the development of a flexible intervention that would aim to be as inclusive as possible, both across different types of care provision and within each individual CH. The MoveMore intervention was developed with the aim of encouraging a core team of staff to consider both individual- and home-level need, facilitating this through workshops and a cycle of improvement. Although the content and process would be consistent, which included workshops, information from the physiotherapist, engagement of an artist and the ideas bank, implementation by CH staff would be tailored to the unique needs of their home and residents. Providing staff with the appropriate tools and skills to observe, plan and review, while offering ongoing support through workshops, not only ensured that intervention activities suited the needs of the home, but also ensured a sense of ownership over the implementation of MoveMore.
The feasibility cluster randomised trial was successfully completed, with the target number of CHs and residents achieved. We have collected a large data set from the detailed and in-depth PE, accelerometer wear and trial assessments. Together, they provide a comprehensive picture of the environment, residents and staff in CHs.
In the following section, we summarise our reflections on the research process.
Research process
The intent here is to briefly summarise key learning to assist others in the implementation of research in CHs.
Care homes
The fragility of the CH sector became apparent over the course of the research programme. Concern over a possible, imminent, planned or just completed CQC inspection was prevalent in all the homes. Understandably, staff energies were directed towards fulfilling their requirements and, on occasion, addressing the concerns expressed. However, participating in research was seen as a positive thing by some: two CHs asked us to provide a letter for the CQC explaining our involvement in the home and all appreciated the certificates we provided.
Gaining initial engagement with CHs proved to be time-consuming. In early WSs, we worked with our colleagues in the local CH forum to identify homes. However, to increase research rigour, rather than approaching ‘known’ homes for the trial, we purposely sought to be as inclusive and unbiased as possible. Through review of the CQC website, we screened > 300 CHs in our region. However, this iterative process of checking the database, CQC reports, mail-outs, telephone prompts and visits was resource intensive. Recruitment through the ENRICH network required less researcher input and led to a higher recruitment rate; however, these were comparatively small recruitment numbers, and future researchers will have to balance the resource issues of being open and outward-looking against recruiting an atypical and possibly ungeneralisable cohort of CHs.
Engagement of managers and staff
We developed a letter of agreement that required sign-off from the CH manager, owner/provider (individual/chain) and study sponsor. This created huge delays, as the paperwork became bound up in the bureaucracy of the management systems of the CHs. Gaining the approval of larger corporations prior to approaching CHs may reduce recruitment time and expedite access to the homes, but this must be balanced against a potential for sample bias if the head office purposively selects homes.
The concept of the research was not always understood by CH managers, despite discussions. This was partly because of the intervention we sought to introduce, which required whole-home engagement. Some managers still retained the mindset that the researchers would ‘do to’ rather than ‘do with.’
Recruitment of residents
It is interesting to note that the highest number of non-consents were from the PCs, with the highest number of consents coming from residents with capacity. This may reflect the characteristics of those residents for whom PCs did not consent (perceived incapacity due to frailty), but, as the rate of NC agreement was higher, it is likely to reflect relatives’ apprehension about the research process. We tried to address this by making researchers available to consultees and attending relative meetings, but it seems we were only partially successful. The best approach seemed to be when the CH manager had a good relationship with the relatives, engaging with them to give an informed overview of the research. Raising awareness of CH research, similar to campaigns undertaken in the NHS, could reduce an understandable apprehension of research.
Frailty of residents
The average age of the residents involved in our studies was > 80 years. Many had cognitive impairment. We were mindful of this at all times, not only in terms of gaining informed consent, but also in terms of engaging residents in components of the research (e.g. use of accelerometers) and ensuring that the proposed intervention was inclusive in nature. Exclusion of this large section of the CH population would weaken the generalisability of the research.
Data collection
Collection of ethnographic data, observations and interviews were, in the main part, successful, within the limits of this client group. A trial-specific observational tool was also developed to facilitate opportunist observations by trial researchers administering outcome measures, which added to the richness of our data collection.
Quantitative data collection was challenging. We were fortunate to have very skilled and experienced research staff who worked flexibly, going to the CHs at weekends and evenings. This was particularly important in administering the accelerometer. The refinement of procedures over the course of this programme optimised the collection of these data, leading to one of the largest ever data sets for this population (n = 186), to our knowledge. It is of note that more residents provided accelerometer data than provided resident-completed outcome questionnaires.
Outcome assessment
We drew on our previous experience and the literature to identify the most appropriate self-report outcome measures, and undertook additional work with residents exploring their understanding of the questions asked. However, return rates for resident-completed outcomes were low. Although proxy returns were higher, these are not necessarily an accurate reflection of residents’ viewpoints. Further work is required to clarify the most appropriate measures for this group of people.
Whole-home assessment
We sought to implement a whole-home intervention. Ideally, we wished to collect data at the level of the home on all residents. We were successful in achieving this for the numbers of falls, deaths and hospitalisations. When screening residents, we gained anonymous BI and PAM-RC scores on all individuals in a home. This gave us information on the population that enabled us to contextualise our intervention delivery and data collection. Unfortunately, we were refused ethics permission to collect these anonymous data (BI and PAM-RC scores) at follow-up points. We feel that procedures to capture anonymised outcomes on all residents (rather than only those who provide consent) would enable a fuller assessment of ‘whole-home’ intervention effects. Consideration could be given to a recommended, simplified, core outcome set that would facilitate data collection in this population.
Staff
Clearly, staff are a key feature of any CH. Engagement with staff was variable across all WSs. In WS1, we had strong relationships with some staff, who then also participated in the advisory group in WS3. In WS4, it was difficult to sustain staff interest in the action groups. Completion of paperwork was particularly problematic across all WSs. In WS5, recognising challenges with literacy levels, time and personal pressures, we tried many strategies to enhance the return rate of the staff booklets. Despite these, the return rate was low. Ethnographic work provided greater insights.
Implementing change
The premise of the intervention was well received, but some CHs struggled with the concept of self-directed work. Pressures of the care environment contributed to a preference in CHs for external agents (in this case, the research team) to resolve issues regarding reduced mobility and activity, rather than proactively generating solutions themselves. However, the intervention was accepted and implemented, at least in part, in four of the five CHs, demonstrating an appropriate methodology for influencing the care environment. It is also of note that five of the UC CHs requested the intervention, three of which engaged with implementation.
Progression to the full trial
The feasibility trial of the MoveMore intervention achieved green on the traffic-light system for recruitment: 12 CHs were recruited, at least 20% of screened residents were eligible and recruited to the study and, although recruitment varied across homes, an average of at least 10 residents per home participated. Although all CHs randomised to the intervention arm completed the series of workshops, completion of the observation, planning and review cycle was not seen in all homes, thus achieving amber status. Loss to the 9-month follow-up for recruited residents was < 35%, capacity to complete resident-reported outcomes was highly variable and accelerometer data were available at 9 months for 52% of those recruited (red status). There were no safety concerns.
Conclusion
The intensity of the ethnographic work and the range of settings involved enabled us to produce an in-depth picture of life in CHs, which will be helpful for others considering organisational change in this setting. We have produced one of the largest ever accelerometer data sets for residents of CHs, to our knowledge, which provides unique insights into the level of activity undertaken by this group of frail elderly people. We worked productively with a stakeholder group and through action groups in CHs to develop an intervention to enhance movement among CH residents. Although the content and process of the intervention, MoveMore, was consistent, implementation allowed CH staff sufficient flexibility to tailor the intervention to their specific CH. We have demonstrated that it is feasible to undertake a cluster randomised trial in the CH setting, successfully recruiting our target number of CHs and residents. We will consider learning from the CHs identified as ‘full implementers’ to optimise the intervention further. Given the frailty of the population leads to difficulties in following up residents over longer periods of time, alternative methods of evaluation (e.g. an open cohort study) could be considered.
It is clear that, with the increasing frailty of CH residents and an array of contextual factors, including financial, legislative and regulatory considerations, it is challenging to operate CHs successfully. Research may be seen as another burden, but we have demonstrated that it can be successfully implemented in these settings and is much needed.
Recommendations for future research
We have highlighted earlier some of our key messages relating to the implementation of research in CHs. Work in this sector is challenging, enjoyable and productive. We make a number of suggestions:
-
Development of methodology for CH research.
Although RCT is the accepted gold standard, methodology may need to be reconsidered in this frail population for whom longer follow-up is problematic. Other methods, such as open cohort studies, could be evaluated.
-
Co-ordinate the participation of CHs in research.
It would be useful to enhance the mechanisms for identifying and enhancing engagement of CHs. Currently, CHs may be approached and recruited by a number of different research teams. The CH manager may lose track of the studies they are participating in; this could result in a CH participating in two very similar or conflicting studies, thereby confounding the research process and invalidating the results.
Local networks of CHs with regular meetings to develop research priorities and data collection methods could be developed. Engagement in research projects could then be evaluated, for example by collecting data on the number of CHs participating in projects, the number of residents recruited and fidelity with the intervention.
-
Develop and evaluate mechanisms for robust PPI engagement.
Establishing a robust and ‘living’ PPI network, including residents, relatives and CH staff, locally to advise on active trials, as well as to feed into new grant applications, would ensure greater relevance of research to its participants. Different mechanisms to develop and provide such a network (e.g. remotely or face-to face meetings) needs evaluation.
-
Data collection
Robust, relevant data collection is key to all research. This is an area for which further research is required, some examples are as follows –
-
Routine data: CHs are tasked with collection of data for many auditing purposes (for their own management, to inform the CQC, for the NHS). However, standardisation is limited. For example, collection of falls data is problematic when CHs use a range of definitions (i.e. whether or not an instance when a fall has not been observed but a resident is found on the floor should be classed as a ‘fall’). Consensus group methodology could be used to develop methods and terminology to standardise routine data collection in CHs.
-
Core outcome set: outcome assessment remains problematic with frail, cognitively impaired individuals. Research is needed to develop a core outcome set for CH research. This would facilitate data collection in this population, allow the synthesis of research results and reduce research waste.
-
Advances in technology: technology (e.g. smart clothing) may produce less intrusive sensors to measure the PA of residents, but their accuracy would need evaluation and ethics aspects would need to be carefully considered.
-
Implications for practice
We have produced one of the largest ever accelerometer data sets for residents of CHs, to our knowledge, which provides unique insights into the level of PA and sedentary behaviour in this population. This has demonstrated the low levels of PA and high levels of sedentary behaviour undertaken by residents in CHs. CH staff and residents found that the feedback provided following participation in WS4 prompted discussions around how to change features in the CH to enhance PA. The use of commercially available technology (e.g. Fitbit; Fitbit, Inc., San Francisco, CA, USA) may prompt similar discussion. Simple observation tools could also be used to encourage staff to take a step back and observe the level of sedentary behaviour/PA being undertaken by residents.
It emerged through this research that it might be helpful for the role and function of the activity co-ordinator to be considered in the CHs. Although having an important role to play in some CHs, sometimes care staff felt that enhancing residents’ PA was the responsibility of the activity co-ordinator and not part of their (caring) role. This led to an overemphasis on occasional organised activities, rather than on trying to improve the PA of residents in everyday activities.
During the programme, we changed our terminology to emphasise ‘movement’. This change was to emphasise the whole-home approach we sought to implement. In the CHs, the phrase ‘physical activity’, and associated terminology, was more commonly linked with exercise classes. This slight change of language might emphasise that the aims of the programme were to enhance day-to-day activity levels.
Care homes could be encouraged to adopt an approach to care that enables their residents: this is a key component of ‘movement’ in our intervention, MoveMore.
Engagement with an artist was a particularly successful feature of this programme of research. The artist was able to interact not only with CH staff, but also with residents with a range of cognitive abilities, and to elicit views about the CH environment and explore ideas about ways to enhance movement. The materials produced proved helpful as posters to prompt increased activity in the CH.
There is opportunity to enhance the PA levels of residents of CHs, but this research programme suggests that it requires a whole-home initiative involving all staff.
Acknowledgements
We would like to thank the owners, managers, staff, residents and relatives of residents of the following CHs for participating in the research programme:
-
The Borrins, Baildon, Shipley
-
Brookfield, Shipley (staff and residents from Brookfield also participated in the advisory group meetings in WS3)
-
Broxbourne House, Wakefield
-
Cookridge Court, Leeds
-
Croft House, Keighley
-
The Gables, Silsden (staff and residents from The Gables participated in the advisory group meetings in WS3)
-
The Hawthornes, Birkenshaw
-
Heath Lodge, Harrogate
-
Howgate House, Idle
-
Manor House, Old Farnley, Leeds
-
Priestley, Batley
-
Riccall House, Riccall, York
-
Sal Royd Villa, Bradford
-
Sandholme Fold, Hipperholme, Halifax
-
Simon Marks Court, Lower Wortley, Leeds
-
Stamford Bridge Beaumont, Stamford Bridge
-
Woodfield Grange, Greetland, Halifax.
The input from artist Tom Bailey was transformational.
We would like to thank physiotherapist Heather Parsons, who assisted in shaping our thinking, gaining buy-in from CHs for WS1 and contributed to all workstreams.
We also thank all members of the WS3 group.
We are pleased to acknowledge the help provided by our research colleagues Gill Procter, Sarah Smith, Rukhsana Rashid and Michelle Platton, and members of the Yorkshire and the Humber National Institute for Health Research Clinical Research Network.
We are extremely grateful to the members of the Programme Steering Committee, who have supported this work throughout implementation of this programme. Their input has been invaluable. The Programme Steering Committee comprised Professor JRF Gladman (chairperson), Marylyn Whelan, Professor Alisoun J Milne, Professor Ngaire Kerse and Rhiannon Whitaker.
We much appreciated the support provided by the Bradford Care Home Forum, particularly colleagues from Bradford Council, Paul Marshall and Matthew Hintze, who helped to develop and establish this research.
We would like to thank colleagues in the Academic Unit for Ageing and Stroke Research and the Clinical Trials Research Unit (University of Leeds) who have provided support and advice over the last few years.
This report is dedicated to the memory of Mary Godfrey whose professional career was spent researching and improving the lives of older people, and who was a co-applicant and lead researcher on this research programme grant.
Contributions of authors
Anne Forster (https://orcid.org/0000-0001-7466-4414) (Professor of Stroke Rehabilitation) was the lead grant holder and chief investigator for the programme, oversaw the design and running of the feasibility trial and was a member of the Programme Management Group.
Mary Godfrey (https://orcid.org/0000-0002-2408-534X) (Reader in Health and Social Care) was a co-applicant on the research programme grant, and led and contributed to the set-up, design and analysis of data in WSs 1 and 4. She also took on a lead role in intervention development, led the intervention training and implementation, and was responsible for the implementation and analysis of the PE of the feasibility trial. Furthermore, she was a member of the Programme Management Group.
John Green (https://orcid.org/0000-0003-1434-9345) (Research Programme Manager, Academic Unit for Ageing and Stroke Research) was the programme manager from November 2015. He oversaw the operational delivery of the feasibility trial at the Academic Unit for Ageing and Stroke Research and was a member of the Programme Management Group.
Nicola McMaster (https://orcid.org/0000-0002-4224-894X) (Research Programme Manager, Academic Unit for Ageing and Stroke Research) was the programme manager from April 2013 to November 2015, oversaw the operational delivery of WSs 1–4. and was a member of the Programme Management Group.
Jennifer Airlie (https://orcid.org/0000-0002-7505-3049) (Research Fellow, Academic Unit for Ageing and Stroke Research and PhD student) took a lead role in accelerometer data acquisition and analysis during WSs 2 and 4 and the feasibility trial. She also contributed to the development of the intervention, and was involved with CH recruitment, participant recruitment and data collection in WSs 2 and 4 and the feasibility trial. Furthermore, she was a member of the Programme Management Group.
Bonnie Cundill (https://orcid.org/0000-0002-3648-820X) (Principal Statistician, Clinical Trials Research Unit) wrote the statistical analysis plan, was responsible for the statistical analysis and reporting of the feasibility trial, and was a member of the Programme Management Group.
Rebecca Lawton (https://orcid.org/0000-0002-5832-402X) (Professor in Psychology of Healthcare) was a co-applicant on the research programme grant and led WS3, taking a lead role in intervention development. She was also a member of the Programme Management Group.
Rebecca Hawkins (https://orcid.org/0000-0003-1811-1369) (Senior Research Fellow, Academic Unit for Ageing and Stroke Research) contributed to the design, set-up, and acquisition and analysis of data in WS1.
Claire Hulme (https://orcid.org/0000-0003-2077-0419) (Professor of Health Economics) was a co-applicant on the research programme grant, led the design of the health economic components of the feasibility trial, was responsible for the health economic analysis, including reporting, and was a member of the Programme Management Group.
Karen Birch (https://orcid.org/0000-0001-7796-8640) (Professor of Exercise Science) was a co-applicant on the research programme grant, led WS2, was involved in the accelerometer data analysis over the course of the programme and was a member of the Programme Management Group.
Lesley Brown (https://orcid.org/0000-0001-5499-9145) (Senior Research Fellow, Academic Unit for Ageing and Stroke Research) contributed to the design and set-up of WS1.
Robert Cicero (https://orcid.org/0000-0002-3713-2934) (Statistician, Clinical Trials Research Unit) was responsible for the statistical analysis and reporting of the feasibility trial, and was a member of the Programme Management Group.
Thomas Frederick Crocker (https://orcid.org/0000-0001-7450-3143) (Senior Research Fellow, Academic Unit for Ageing and Stroke Research) was the administrative contact for the programme grant application, lead author of the Cochrane review, had input in WS3 and contributed to the selection of outcome measures for the feasibility trial.
Bryony Dawkins (https://orcid.org/0000-0002-7038-1975) (Research Fellow) was responsible for the health economic analysis of the feasibility trial, including write-up.
David R Ellard (https://orcid.org/0000-0002-2992-048X) (Principal Research Fellow) was a co-applicant on the research programme grant, contributed to the design of WS1, had input throughout the programme and was a member of the Programme Management Group.
Alison Ellwood (https://orcid.org/0000-0001-8632-1830) (Research Assistant, Academic Unit for Ageing and Stroke Research) led intervention training and implementation, and was responsible for CH and participant recruitment in the feasibility trial.
Joan Firth (lay member) was a co-applicant on the research programme grant, had input throughout the programme and was a member of the Programme Management Group.
Bev Gallagher (https://orcid.org/0000-0003-1005-7804) (NHS Senior Clinical Quality Manager for Independent Providers, Bradford and Craven CCGs) had input throughout the programme and was a member of the Programme Management Group.
Liz Graham (https://orcid.org/0000-0003-4276-1257) (Senior Trial Manager, Clinical Trials Research Unit) was a co-applicant on the research programme grant, was responsible for the operational delivery of the feasibility trial at the Clinical Trials Research Unit and was a member of the Programme Management Group.
Louise Johnson (https://orcid.org/0000-0002-9052-5032) (formerly a lecturer in physiotherapy at the University of Bradford) was a co-applicant on the research programme grant and contributed to the design of WS2.
Adelaide Lusambili (https://orcid.org/0000-0002-3633-6978) (Research Fellow, Academic Unit for Ageing and Stroke Research) contributed to data acquisition and analysis in WS1. She was also involved in the data collection in WS4.
Joachim Marti (https://orcid.org/0000-0001-5763-3704) (formerly a lecturer at the University of Leeds) contributed to the design of the health economic components of the feasibility trial.
Carolyn McCrorie (https://orcid.org/0000-0002-2673-6839) (Research Fellow, Academic Unit for Ageing and Stroke Research) was involved in participant recruitment and data collection in WS4. She also undertook the PE of the feasibility trial.
Vicki McLellan (https://orcid.org/0000-0003-1630-9355) (Senior Trial Co-ordinator, Clinical Trials Research Unit) was responsible for the operational delivery of the feasibility trial at the Clinical Trials Research Unit and was a member of the Programme Management Group.
Ismail Patel (https://orcid.org/0000-0001-8550-4678) (Elderly Care Researcher, Academic Unit for Ageing and Stroke Research) took a lead role in participant recruitment and data collection for the feasibility trial.
Arvin Prashar (https://orcid.org/0000-0003-3349-4353) (Research Fellow, Academic Unit for Ageing and Stroke Research) contributed to the design and set-up of WSs 1 and 4. He also took a lead role in data acquisition and analysis in these WSs.
Najma Siddiqi (https://orcid.org/0000-0003-1794-2152) (Clinical Senior Lecturer, and honorary consultant psychiatrist at Bradford District Care NHS Foundation Trust) was a co-applicant on the research programme grant, had input throughout the programme and was a member of the Programme Management Group.
Dominic Trépel (https://orcid.org/0000-0002-1421-2966) (formerly a Senior Research Fellow at the University of Leeds) was responsible for the design and write-up of the health economic model in the feasibility trial.
Ian Wheeler (https://orcid.org/0000-0003-0955-8556) (Trial Co-ordinator, Clinical Trials Research Unit) supported delivery of the feasibility trial at the Clinical Trials Research Unit.
Alan Wright (https://orcid.org/0000-0002-5787-293X) (Research Fellow, Academic Unit for Ageing and Stroke Research) took a lead role in participant recruitment and data collection in WS4 and the feasibility trial. He also contributed to development of the intervention.
John Young (https://orcid.org/0000-0003-4085-9306) (Professor of Elderly Care) was a co-applicant on the research programme grant, shared clinical expertise throughout the programme and was a member of the Programme Management Group.
Amanda Farrin (https://orcid.org/0000-0002-2876-0584) (Professor of Clinical Trials and Evaluation of Complex Interventions) was a co-applicant on the research programme grant, was the programme methodologist, was responsible for the main statistical analysis and reporting of the feasibility trial, and was a member of the Programme Management Group.
Publications
Forster A, Airlie J, Birch K, Cicero R, Cundill B, Ellwood A, et al. Research Exploring Physical Activity in Care Homes (REACH): study protocol for a randomised controlled trial. Trials 2017;18:182. https://doi.org/10.1186/s13063-017-1921-8
Ellwood A, Airlie J, Cicero R, Cundill B, Ellard DR, Farrin A, et al. Recruiting care homes to a randomised controlled trial. Trials 2018;19:535. https://doi.org/10.1186/s13063-018-2915-x
Hawkins RJ, Prashar A, Lusambili A, Ellard DR, Godfrey M. ‘If they don't use it, they lose it’: how organisational structures and practices shape residents’ physical movement in care home settings. Ageing Soc 2018;38:1817–42. https://doi.org/10.1017/S0144686X17000290
Forster A, Airlie J, Ellwood A, Godfrey M, Green J, Cundill B, et al. An intervention to increase physical activity in care home residents: results of a cluster-randomised, controlled feasibility trial (the REACH trial) [Published online ahead of print July 23 2021]. Age Ageing 2021. https://doi.org/10.1093/ageing/afab130
Data-sharing statement
Workstreams in this programme grant involved qualitative methodologies; therefore, the data generated are not suitable for sharing beyond that contained in this report. Further information can be obtained from the corresponding author.
As WS5 was a feasibility trial to inform a definitive trial, sharing of the trial data set is not anticipated; however, any data requests should be sent to the corresponding author and will be subject to review by a subgroup of the trial team, which will include the data guarantor, Amanda Farrin. All data-sharing activities would require a data-sharing agreement.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, CCF, NETSCC, PGfAR or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PGfAR programme or the Department of Health and Social Care.
References
- Forster A, Airlie J, Ellwood A, Godfrey M, Green J, Cundill B, et al. An intervention to increase physical activity in care home residents: results of a cluster-randomised, controlled feasibility trial (the REACH trial). Age Ageing 2021. https://doi.org/10.1093/ageing/afab130.
- World Health Organization . Global Health and Aging 2011. www.who.int/ageing/publications/global_health.pdf (accessed July 2018).
- Age UK . Improving Later Life. Understanding the Oldest Old 2013. www.ageuk.org.uk/Documents/EN-GB/For-professionals/Research/Improving%20Later%20Life%202%20WEB.pdf?dtrk=true%20 (accessed November 2013).
- Office for National Statistics . National Population Projections, 2014-Based Statistical Bulletin 2011. www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationprojections/bulletins/nationalpopulationprojections/2015-10-29#changing-age-structure (accessed July 2018).
- Prince MJ, Wu F, Guo Y, Gutierrez Robledo LM, O’Donnell M, Sullivan R, et al. The burden of disease in older people and implications for health policy and practice. Lancet 2015;385:549-62. https://doi.org/10.1016/S0140-6736(14)61347-7.
- Kirchberger I, Meisinger C, Heier M, Zimmermann AK, Thorand B, Autenrieth CS, et al. Patterns of multimorbidity in the aged population. Results from the KORA-Age study. PLOS ONE 2012;7. https://doi.org/10.1371/journal.pone.0030556.
- Caughey GE, Ramsay EN, Vitry AI, Gilbert AL, Luszcz MA, Ryan P, et al. Comorbid chronic diseases, discordant impact on mortality in older people: a 14-year longitudinal population study. J Epidemiol Community Health 2010;64:1036-42. https://doi.org/10.1136/jech.2009.088260.
- Rodrigues R, Huber M, Lamura G. Facts and Figures on Healthy Ageing and Long-term Care. Vienna: European Centre for Social Welfare Policy and Research; 2012.
- Forder J, Fernandez JL. Length of Stay in Care Homes. Canterbury: PSSRU, University of Kent; 2011.
- Harwood RH. Do we still need care homes?. Age Ageing 2004;33:529-30. https://doi.org/10.1093/ageing/afh191.
- Gordon AL, Franklin M, Bradshaw L, Logan P, Elliott R, Gladman JR. Health status of UK care home residents: a cohort study. Age Ageing 2014;43:97-103. https://doi.org/10.1093/ageing/aft077.
- National Institute for Health and Care Excellence (NICE) . Mental Wellbeing in Over 65s: Occupational Therapy and Physical Activity Interventions 2008.
- Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet 2013;381:752-62. https://doi.org/10.1016/S0140-6736(12)62167-9.
- Myint PK, Welch AA. Healthier ageing. BMJ 2012;344. https://doi.org/10.1136/bmj.e1214.
- Pettee Gabriel KK, Morrow JR, Woolsey AL. Framework for physical activity as a complex and multidimensional behavior. J Phys Act Health 2012;9:11-8. https://doi.org/10.1123/jpah.9.s1.s11.
- Barber SE, Clegg AP, Young JB. Is there a role for physical activity in preventing cognitive decline in people with mild cognitive impairment?. Age Ageing 2012;41:5-8. https://doi.org/10.1093/ageing/afr138.
- Blake H, Mo P, Malik S, Thomas S. How effective are physical activity interventions for alleviating depressive symptoms in older people? A systematic review. Clin Rehabil 2009;23:873-87. https://doi.org/10.1177/0269215509337449.
- Binder EF, Schechtman KB, Ehsani AA, Steger-May K, Brown M, Sinacore DR, et al. Effects of exercise training on frailty in community-dwelling older adults: results of a randomized, controlled trial. J Am Geriatr Soc 2002;50:1921-8. https://doi.org/10.1046/j.1532-5415.2002.50601.x.
- Potter R, Ellard D, Rees K, Thorogood M. A systematic review of the effects of physical activity on physical functioning, quality of life and depression in older people with dementia. Int J Geriatr Psychiatry 2011;26:1000-11. https://doi.org/10.1002/gps.2641.
- Weening-Dijksterhuis E, de Greef MH, Scherder EJ, Slaets JP, van der Schans CP. Frail institutionalized older persons: a comprehensive review on physical exercise, physical fitness, activities of daily living, and quality-of-life. Am J Phys Med Rehabil 2011;90:156-68. https://doi.org/10.1097/PHM.0b013e3181f703ef.
- Chin A, Paw MJ, van Uffelen JG, Riphagen I, van Mechelen W. The functional effects of physical exercise training in frail older people: a systematic review. Sports Med 2008;38:781-93. https://doi.org/10.2165/00007256-200838090-00006.
- Mendes de Leon CF. Social engagement and successful aging. Eur J Ageing 2005;2:64-6. https://doi.org/10.1007/s10433-005-0020-y.
- Marmeleira J, Ferreira S, Raimundo A. Physical activity and physical fitness of nursing home residents with cognitive impairment: a pilot study. Exp Gerontol 2017;100:63-9. https://doi.org/10.1016/j.exger.2017.10.025.
- Barber SE, Forster A, Birch KM. Levels and patterns of daily physical activity and sedentary behavior measured objectively in older care home residents in the United Kingdom. J Aging Phys Act 2015;23:133-43. https://doi.org/10.1123/japa.2013-0091.
- Sackley CM, Hoppitt T, Levin S, Cardoso K. Observations of activity levels and social interaction in a residential care setting. Int J Ther Rehabil 2006;13:370-3. https://doi.org/10.12968/ijtr.2006.13.8.370.
- de Rezende LF, Rey-López JP, Matsudo VK, do Carmo Luiz O. Sedentary behavior and health outcomes among older adults: a systematic review. BMC Public Health 2014;14. https://doi.org/10.1186/1471-2458-14-333.
- Same RV, Feldman DI, Shah N, Martin SS, Al Rifai M, Blaha MJ, et al. Relationship between sedentary behavior and cardiovascular risk. Curr Cardiol Reps 2016;18. https://doi.org/10.1007/s11886-015-0678-5.
- Sardinha LB, Santos DA, Silva AM, Baptista F, Owen N. Breaking-up sedentary time is associated with physical function in older adults. J Gerontol A Biol Sci Med Sci 2015;70:119-24. https://doi.org/10.1093/gerona/glu193.
- Gennuso KP, Gangnon RE, Matthews CE, Thraen-Borowski KM, Colbert LH. Sedentary behavior, physical activity, and markers of health in older adults. Med Sci Sports Exerc 2013;45:1493-500. https://doi.org/10.1249/MSS.0b013e318288a1e5.
- O’Neill C, Dogra S. Different types of sedentary activities and their association with perceived health and wellness among middle-aged and older adults: a cross-sectional analysis. Am J Health Promot 2016;30:314-22. https://doi.org/10.1177/0890117116646334.
- Meneguci J, Sasaki JE, da Silva Santos Á, Scatena LM, Damião R. Socio-demographic, clinical and health behavior correlates of sitting time in older adults. BMC Public Health 2015;15. https://doi.org/10.1186/s12889-015-1426-x.
- Butler RN, Davis R, Lewis CB, Nelson ME, Strauss E. Physical fitness: benefits of exercise for the older patient. 2. Geriatrics 1998;53.
- British Heart Foundation National Centre . Interpreting the UK Physical Activity Guidelines for Older Adults (65+). Guidance for Those Who Work With Frailer, Older People 2012.
- Crocker T, Forster A, Young J, Brown L, Ozer S, Smith J, et al. Physical rehabilitation for older people in long-term care. Cochrane Database Syst Rev 2013;2. https://doi.org/10.1002/14651858.CD004294.pub3.
- National Institute for Health Research . Research Award. Development and Testing of Strategies to Enhance Physical Activity in Care Homes: A Feasibility Study n.d. https://fundingawards.nihr.ac.uk/award/RP-DG-0709-10141 (accessed 26 October 2020).
- Ball MM, Lepore ML, Perkins MM, Hollingsworth C, Sweatman M. ‘They are the reason I come to work’: the meaning of resident–staff relationships in assisted living. J Aging Stud 2009;23:37-4. https://doi.org/10.1016/j.jaging.2007.09.006.
- Godfrey M, Keen J, Townsend J, Moore J, Ware P, Hardy B, et al. An Evaluation of Intermediate Care for Older People: Final Report 2005.
- Dey I. Grounding Grounded Theory: Guidelines for Qualitative Inquiry. San Diego, CA: Academic Press; 1999.
- Hawkins RJ, Prashar A, Lusambili A, Ellard DR, Godrey M. ‘If they don’t use it, they lose it’: how organisational structures and practices shape residents’ physical movement in care home settings. Ageing Soc 2018;38:1817-42. https://doi.org/10.1017/S0144686X17000290.
- Emerson RM, Fretz RI, Shaw LL, Atkinson P, Coffey A, Delamont S, et al. Handbook of Ethnography. London: SAGE Publications Ltd; 2002.
- Spradley J. Participant Observation. New York, NY: Holt, Rinehart, and Winston; 1980.
- McCormack B. Negotiating Partnerships with Older People: A Person Centred Approach. Aldershot: Ashgate; 2001.
- Hawkins R, Redley M, Holland AJ. Duty of care and autonomy: how support workers managed the tension between protecting service users from risk and promoting their independence in a specialist group home. J Intellect Disabil Res 2011;55:873-84. https://doi.org/10.1111/j.1365-2788.2011.01445.x.
- Kirkley C, Bamford C, Poole M, Arksey H, Hughes J, Bond J. The impact of organisational culture on the delivery of person-centred care in services providing respite care and short breaks for people with dementia. Health Soc Care Community 2011;19:438-48. https://doi.org/10.1111/j.1365-2524.2011.00998.x.
- Killett A, Burns D, Kelly F, Brooker D, Bowes A, La Fontaine J, et al. Digging deep: how organisational culture affects care home residents’ experiences. Ageing Soc 2016;36:160-88. https://doi.org/10.1017/S0144686X14001111.
- Hauer K, Lord SR, Lindemann U, Lamb SE, Aminian K, Schwenk M. Assessment of physical activity in older people with and without cognitive impairment. J Aging Phys Act 2011;19:347-72. https://doi.org/10.1123/japa.19.4.347.
- Brooke P, Bullock R. Validation of a 6 item cognitive impairment test with a view to primary care usage. Int J Geriatr Psychiatry 1999;14:936-40.
- Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J 1965;14:61-5.
- Collin C, Wade DT, Davies S, Horne V. The Barthel ADL Index: a reliability study. Int Disabil Stud 1988;10:61-3. https://doi.org/10.3109/09638288809164103.
- Holden MK, Gill KM, Magliozzi MR, Nathan J, Piehl-Baker L. Clinical gait assessment in the neurologically impaired. Reliability and meaningfulness. Phys Ther 1984;64:35-40. https://doi.org/10.1093/ptj/64.1.35.
- Gupta A. Measurement Scales Used in Elderly Care. Oxford: Radcliffe Publishing Ltd; 2008.
- Gerdhem P, Dencker M, Ringsberg K, Akesson K. Accelerometer-measured daily physical activity among octogenerians: results and associations to other indices of physical performance and bone density. Eur J Appl Physiol 2008;102:173-80. https://doi.org/10.1007/s00421-007-0571-z.
- Orme M, Wijndaele K, Sharp SJ, Westgate K, Ekelund U, Brage S. Combined influence of epoch length, cut-point and bout duration on accelerometry-derived physical activity. Int J Behav Nutr Phys Act 2014;11. https://doi.org/10.1186/1479-5868-11-34.
- Jørstad-Stein EC, Hauer K, Becker C, Bonnefoy M, Nakash RA, Skelton DA, et al. Suitability of physical activity questionnaires for older adults in fall-prevention trials: a systematic review. J Aging Phys Act 2005;13:461-81. https://doi.org/10.1123/japa.13.4.461.
- Stewart AL, Mills KM, King AC, Haskell WL, Gillis D, Ritter PL. CHAMPS physical activity questionnaire for older adults: outcomes for interventions. Med Sci Sports Exerc 2001;33:1126-41. https://doi.org/10.1097/00005768-200107000-00010.
- Quinn TJ, Langhorne P, Stott DJ. Barthel index for stroke trials: development, properties, and application. Stroke 2011;42:1146-51. https://doi.org/10.1161/STROKEAHA.110.598540.
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159-74. https://doi.org/10.2307/2529310.
- Leung PM, Ejupi A, van Schooten KS, Aziz O, Feldman F, Mackey DC, et al. Association between sedentary behaviour and physical, cognitive, and psychosocial status among older adults in assisted living. Biomed Res Int 2017;2017. https://doi.org/10.1155/2017/9160504.
- Corcoran MP, Chui KK, White DK, Reid KF, Kirn D, Nelson ME, et al. Accelerometer assessment of physical activity and its association with physical function in older adults residing at assisted care facilities. J Nutr Health Aging 2016;20:752-8. https://doi.org/10.1007/s12603-015-0640-7.
- Schrack JA, Cooper R, Koster A, Shiroma EJ, Murabito JM, Rejeski WJ, et al. Assessing daily physical activity in older adults: unravelling the complexity of monitors, measures, and methods. J Gerontol A Biol Sci Med Sci 2016;71:1039-48. https://doi.org/10.1093/gerona/glw026.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and Evaluating Complex Interventions: New Guidance. London: Medical Research Council; 2008.
- Bartholomew L, Parcel G, Kok G, Gottlieb N, Fernandez M. Planning Health Promotion Program. San Francisco, CA: Joffey-Ball; 2011.
- Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A. ‘Psychological Theory’ Group . Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care 2005;14:26-33. https://doi.org/10.1136/qshc.2004.011155.
- Royal College of Occupational Therapists . Living Well Through Activity in Care Homes: The Toolkit n.d. www.rcot.co.uk/sites/default/files/Unit4-Care-home-Inspectors-2015.pdf (accessed 26 October 2020).
- Kemmis S, McTaggart R, Nixon R. The Action Research Planner: Doing Critical Participatory Action Research. Singapore: Springer; 2013.
- Forster A, Airlie J, Birch K, Cicero R, Cundill B, Ellwood A, et al. Research Exploring Physical Activity in Care Homes (REACH): study protocol for a randomised controlled trial. Trials 2017;18. https://doi.org/10.1186/s13063-017-1921-8.
- Great Britain . Mental Capacity Act 2005 2005.
- Davies SL, Goodman C, Manthorpe J, Smith A, Carrick N, Iliffe S. Enabling research in care homes: an evaluation of a national network of research ready care homes. BMC Med Res Methodol 2014;14. https://doi.org/10.1186/1471-2288-14-47.
- Edvardsson D, Fetherstonhaugh D, Nay R, Gibson S. Development and initial testing of the Person-centred Care Assessment Tool (P-CAT). Int Psychogeriatr 2010;22:101-8. https://doi.org/10.1017/S1041610209990688.
- Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 1983;17:37-49. https://doi.org/10.1016/0022-3956(82)90033-4.
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36. https://doi.org/10.1007/s11136-011-9903-x.
- Smith SC, Lamping DL, Banerjee S, Harwood RH, Foley B, Smith P, et al. Development of a new measure of health-related quality of life for people with dementia: DEMQOL. Psychol Med 2007;37:737-46. https://doi.org/10.1017/S0033291706009469.
- Power M, Quinn K, Schmidt S. WHOQOL-OLD Group . Development of the WHOQOL-old module. Qual Life Res 2005;14:2197-214. https://doi.org/10.1007/s11136-005-7380-9.
- Smith R. Validation and reliability of the Elderly Mobility Scale. Physiother 1994;80:744-7. https://doi.org/10.1016/S0031-9406(10)60612-8.
- Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol 1994;47:1245-51. https://doi.org/10.1016/0895-4356(94)90129-5.
- Hansen BH, Kolle E, Dyrstad SM, Holme I, Anderssen SA. Accelerometer-determined physical activity in adults and older people. Med Sci Sports Exerc 2012;44:266-72. https://doi.org/10.1249/MSS.0b013e31822cb354.
- Ellwood A, Airlie J, Cicero R, Cundill B, Ellard DR, Farrin A, et al. Recruiting care homes to a randomised controlled trial. Trials 2018;19. https://doi.org/10.1186/s13063-018-2915-x.
- Ragin C, Becker H, Ragin C, Becker H. What is a Case? Exploring the Foundations of Social Inquiry. Cambridge: Cambridge University Press; 1992.
- Stake R. The Art of Case Study Research. London: SAGE Publications Ltd; 1995.
- Yin R. Case Study Research: Design and Methods. London: SAGE Publications Ltd; 2009.
- Byrne D, Byrne D, Ragin C. The Sage Handbook of Case-based Methods. London: SAGE Publications Ltd; 2013.
- Charmaz K. Constructing Grounded Theory. Thousand Oaks CA: SAGE Publications Ltd; 2014.
- Devine A, Taylor SJ, Spencer A, Diaz-Ordaz K, Eldridge S, Underwood M. The agreement between proxy and self-completed EQ-5D for care home residents was better for index scores than individual domains. J Clin Epidemiol 2014;67:1035-43. https://doi.org/10.1016/j.jclinepi.2014.04.005.
- McPhail S, Beller E, Haines T. Two perspectives of proxy reporting of health-related quality of life using the Euroqol-5D, an investigation of agreement. Med Care 2008;46:1140-8. https://doi.org/10.1097/MLR.0b013e31817d69a6.
- Tamim H, McCusker J, Dendukuri N. Proxy reporting of quality of life using the EQ-5D. Med Care 2002;40:1186-95. https://doi.org/10.1097/00005650-200212000-00006.
- Kalinowski S, Budnick A, Kuhnert R, Könner F, Kissel-Kröll A, Kreutz R, et al. Nonpharmacologic pain management interventions in German Nursing Homes: a cluster randomized trial. Pain Manag Nurs 2015;16:464-74. https://doi.org/10.1016/j.pmn.2014.09.002.
- Zermansky AG, Alldred DP, Petty DR, Raynor DK, Freemantle N, Eastaugh J, et al. Clinical medication review by a pharmacist of elderly people living in care homes – randomised controlled trial. Age Ageing 2006;35:586-91. https://doi.org/10.1093/ageing/afl075.
- Underwood M, Lamb SE, Eldridge S, Sheehan B, Slowther AM, Spencer A, et al. Exercise for depression in elderly residents of care homes: a cluster-randomised controlled trial. Lancet 2013;382:41-9. https://doi.org/10.1016/S0140-6736(13)60649-2.
- Siddiqi N, Cheater F, Collinson M, Farrin A, Forster A, George D, et al. The PiTSTOP study: a feasibility cluster randomized trial of delirium prevention in care homes for older people. Age Ageing 2016;45:652-61. https://doi.org/10.1093/ageing/afw091.
- Flicker L, MacInnis RJ, Stein MS, Scherer SC, Mead KE, Nowson CA, et al. Should older people in residential care receive vitamin D to prevent falls? Results of a randomized trial. J Am Geriatr Soc 2005;53:1881-8. https://doi.org/10.1111/j.1532-5415.2005.00468.x.
- Sackley CM, Walker MF, Burton CR, Watkins CL, Mant J, Roalfe AK, et al. An occupational therapy intervention for residents with stroke related disabilities in UK care homes (OTCH): cluster randomised controlled trial. BMJ 2015;350. https://doi.org/10.1136/bmj.h468.
- Sandvik RK, Selbaek G, Seifert R, Aarsland D, Ballard C, Corbett A, et al. Impact of a stepwise protocol for treating pain on pain intensity in nursing home patients with dementia: a cluster randomized trial. Eur J Pain 2014;18:1490-500. https://doi.org/10.1002/ejp.523.
- Ukoumunne OC. A comparison of confidence interval methods for the intraclass correlation coefficient in cluster randomized trials. Stat Med 2002;21:3757-74. https://doi.org/10.1002/sim.1330.
- Hayes RJ, Moulton LH. Cluster Randomised Trials. Boca Raton, FL: CRC Press; 2017.
- Office for National Statistics (ONS) . National Population Projections, 2008-Based 2009.
- Szczepura A, Nelson S, Wild D. In-reach specialist nursing teams for residential care homes: uptake of services, impact on care provision and cost-effectiveness. BMC Health Serv Res 2008;8. https://doi.org/10.1186/1472-6963-8-269.
- Continuing Care Conference . Care at the Crossroads: CCC Care Census Points the Way Forward 2006. www.ccc-ltc.org.uk/pr/2006-07-03.pdf (accessed 2010).
- Mokdad AH, Giles WH, Bowman BA, Mensah GA, Ford ES, Smith SM, et al. Changes in health behaviors among older Americans, 1990 to 2000. Public Health Rep 2004;119:356-61. https://doi.org/10.1016/j.phr.2004.04.015.
- Lee IM, Skerrett PJ. Physical activity and all-cause mortality: what is the dose–response relation?. Med Sci Sports Exerc 2001;33:S459-471. https://doi.org/10.1097/00005768-200106001-00016.
- Department of Health and Social Care (DHSC) . Securing Better Mental Health As Part of Active Ageing 2005.
- Department of Health and Social Care (DHSC) . Choosing Activity: A Physical Activity Action Plan 2005.
- Windle G, Hughes D, Linck P, Russell I, Woods B. Is exercise effective in promoting mental well-being in older age? A systematic review. Aging Ment Health 2010;14:652-69. https://doi.org/10.1080/13607861003713232.
- Baum EE, Jarjoura D, Polen AE, Faur D, Rutecki G. Effectiveness of a group exercise program in a long-term care facility: a randomized pilot trial. J Am Med Dir Assoc 2003;4:74-80. https://doi.org/10.1097/01.JAM.0000053513.24044.6C.
- Bruunsgaard H, Bjerregaard E, Schroll M, Pedersen BK. Muscle strength after resistance training is inversely correlated with baseline levels of soluble tumor necrosis factor receptors in the oldest old. J Am Geriatr Soc 2004;52:237-41.
- Smalbrugge M, Pot AM, Jongenelis L, Gundy CM, Beekman AT, Eefsting JA. The impact of depression and anxiety on well being, disability and use of health care services in nursing home patients. Int J Geriatr Psychiatry 2006;21:325-32. https://doi.org/10.1002/gps.1466.
- Barodawala S, Kesavan S, Young J. A survey of physiotherapy and occupational therapy provision in UK nursing homes. Clin Rehabil 2001;15:607-10. https://doi.org/10.1191/0269215501cr454oa.
- Kerse N, Peri K, Robinson E, Wilkinson T, von Randow M, Kiata L, et al. Does a functional activity programme improve function, quality of life, and falls for residents in long term care? Cluster randomised controlled trial. BMJ 2008;337. https://doi.org/10.1136/bmj.a1445.
- Whitaker A. Family involvement in the institutional eldercare context. Towards a new understanding. J Aging Stud 2009;23:158-67. https://doi.org/10.1016/j.jaging.2008.12.006.
- Bauer M, Nay R. Family and staff partnerships in long-term care. A review of the literature. J Gerontol Nurs 2003;29:46-53. https://doi.org/10.3928/0098-9134-20031001-09.
- Sinoff G, Ore L. The Barthel activities of daily living index: self-reporting versus actual performance in the old-old (> or = 75 years). J Am Geriatr Soc 1997;45:832-6. https://doi.org/10.1111/j.1532-5415.1997.tb01510.x.
- Podsiadlo D, Richardson S. The timed ‘Up & Go’: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 1991;39:142-8. https://doi.org/10.1111/j.1532-5415.1991.tb01616.x.
- Blessed G, Tomlinson BE, Roth M. The association between quantitative measures of dementia and of senile change in the cerebral grey matter of elderly subjects. Br J Psychiatry 1968;114:797-811.
- Folstein MF, Folstein SE, McHugh PR. ‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189-98. https://doi.org/10.1016/0022-3956(75)90026-6.
- LaPorte RE, Montoye HJ, Caspersen CJ. Assessment of physical activity in epidemiologic research: problems and prospects. Public Health Rep 1985;100:131-46.
- Yang CC, Hsu YL. A review of accelerometry-based wearable motion detectors for physical activity monitoring. Sensors 2010;10:7772-88. https://doi.org/10.3390/s100807772.
- Chen KY, Bassett DR. The technology of accelerometry-based activity monitors: current and future. Med Sci Sports Exerc 2005;37:490-50. https://doi.org/10.1249/01.mss.0000185571.49104.82.
- Welk GJ. Principles of design and analyses for the calibration of accelerometry-based activity monitors. Med Sci Sports Exerc 2005;37:501-11. https://doi.org/10.1249/01.mss.0000185660.38335.de.
- Bassett DR. Device-based monitoring in physical activity and public health research. Physiol Meas 2012;33:1769-83. https://doi.org/10.1088/0967-3334/33/11/1769.
- LaMunion SR, Bassett DR, Toth LP, Crouter SE. The effect of body placement site on ActiGraph wGT3X-BT activity counts. Biomed Phys Eng Express 2017;3. https://doi.org/10.1088/2057-1976/aa777c.
- Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc 2008;40:181-8. https://doi.org/10.1249/mss.0b013e31815a51b3.
- Mâsse LC, Fuemmeler BF, Anderson CB, Matthews CE, Trost SG, Catellier DJ, et al. Accelerometer data reduction: a comparison of four reduction algorithms on select outcome variables. Med Sci Sports Exerc 2005;37:544-54. https://doi.org/10.1249/01.mss.0000185674.09066.8a.
- Ridgers ND, Fairclough S. Assessing free-living physical activity using accelerometry: practical issues for researchers and practitioners. Eur J Sport Sci 2011;11:205-13. https://doi.org/10.1080/17461391.2010.501116.
- ActiGraph . What Does the ‘Worn on Wrist’ Option Do in the Scoring Tab? n.d. https://actigraphcorp.force.com/support/s/article/What-does-the-Worn-on-Wrist-option-do-in-the-Scoring-tab (accessed 17 November 2020).
- Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR, Tudor-Locke C, et al. 2011 Compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc 2011;43:1575-81. https://doi.org/10.1249/MSS.0b013e31821ece12.
- Aguilar-Farías N, Brown WJ, Peeters GM. ActiGraph GT3X+ cut-points for identifying sedentary behaviour in older adults in free-living environments. J Sci Med Sport 2014;17:293-9. https://doi.org/10.1016/j.jsams.2013.07.002.
- Hutto B, Howard VJ, Blair SN, Colabianchi N, Vena JE, Rhodes D, et al. Identifying accelerometer nonwear and wear time in older adults. Int J Behav Nutr Phys Act 2013;10. https://doi.org/10.1186/1479-5868-10-120.
- Copeland JL, Esliger DW. Accelerometer assessment of physical activity in active, healthy older adults. J Aging Phys Act 2009;17:17-30. https://doi.org/10.1123/japa.17.1.17.
- Matthews CE. Calibration of accelerometer output for adults. Med Sci Sports Exerc 2005;37:S512-22. https://doi.org/10.1249/01.mss.0000185659.11982.3d.
- Hinkley T, O’Connell E, Okely AD, Crawford D, Hesketh K, Salmon J. Assessing volume of accelerometry data for reliability in preschool children. Med Sci Sports Exerc 2012;44:2436-41. https://doi.org/10.1249/MSS.0b013e3182661478.
- Hoppitt T, Sackley C, Wright C. Finding the right outcome measures for care home research. Age Ageing 2010;39:119-22. https://doi.org/10.1093/ageing/afp189.
- Moore G, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process Evaluations of Complex Interventions: UK Medical Research Council (MRC) Guidance. London: Medical Research Council; 2011.
- Oakley A, Strange V, Bonell C, Allen E, Stephenson J. Process evaluations in randomised controlled trials of complex interventions. BMJ 2006;332:413-16. https://doi.org/10.1136/bmj.332.7538.413.
- Clarke D, Godfrey M, Hawkins R, Sadler E, Harding G, Forster A, et al. Implementing a training intervention to support caregivers after stroke: a process valuation examining the initiation and embedding of programme change. Implement Sci 2013;8. https://doi.org/10.1186/1748-5908-8-96.
- Godfrey M, Young J, Shannon R, Skingley A, Woolley R, Arrojo F, et al. The Person, Interactions and Environment Programme to improve care of people with dementia in hospital: a multisite study. Health Serv Deliv Res 2018;6. https://doi.org/10.3310/hsdr06230.
- Stame N. Theory-based evaluation and types of complexity. Evaluation 2006;10:58-76. https://doi.org/10.1177/1356389004043135.
- Fixsen DL, Naoom SF, Blase KA, Friedman RM, Wallace F. Implementation Research: A Synthesis of the Literature. Tampa, FL: University of South Florida, Louis de la Parte Florida Mental Health Institute, National Implementation Research Network (FMHI Publication #231); 2005.
- Rogers PJ. Using programme theory to evaluate complicated and complex aspects of interventions. Evaluation 2008;14:29-48. https://doi.org/10.1177/1356389007084674.
- Sabatier PA. Top-down and bottom-up approaches to implementation research: a critical analysis and suggested synthesis. J Pub Pol 1986;6:21-48. https://doi.org/10.1017/S0143814X00003846.
- Powell A, Rushmer R, Davies H. A Systematic Narrative Review of Quality Improvement Models in Health Care. Edinburgh: NHS Quality Improvement Scotland; 2009.
- Lukas CV, Holmes SK, Cohen AB, Restuccia J, Cramer IE, Schwartz M, et al. Transformational change in healthcare systems: an organizational model. Health Care Manage Rev 2007;32:309-20. https://doi.org/10.1097/01.HMR.0000296785.29718.5d.
- Bate P, Mendel P, Robert G. Organising for Quality: The Improvement Journeys of Leading Hospitals in Europe and the United States. London: The Nuffield Trust; 2008.
- Hawe P, Shiell A, Riley T. Complex interventions: how ‘out of control’ can a randomised controlled trial be?. BMJ 2004;328:1561-3. https://doi.org/10.1136/bmj.328.7455.1561.
- Hawe P, Shiell A, Riley T. Theorising interventions as events in systems. Am J Community Psychol 2009;43:267-76. https://doi.org/10.1007/s10464-009-9229-9.
- Atkinson P. For Ethnography. London: SAGE Publications Ltd; 2015.
- Lofland J, Snow D, Anderson L, Lofland LH. Analysing Social Settings: A Guide to Qualitative Observations and Analysis. Belmont CA: Wadsworth; 2006.
- Mishler EG. Research Interviewing: Context and Narrative. Cambridge, MA: Harvard University Press; 1986.
- Rubin H, Rubin I. Qualitative Interviewing: The Art of Hearing Data. Thousand Oaks, CA: SAGE Publications, Ltd; 2012.
- Century J, Cassata A, Rudnick M, Freeman C. Measuring enactment of innovations and the factors that affect implementation and sustainability: moving toward common language and shared conceptual understanding. J Behav Health Serv Res 2012;39:343-61. https://doi.org/10.1007/s11414-012-9287-x.
- Emerson RM, Fretz RI, Shaw LL. Writing Ethnographic Fieldnotes. Chicago, IL: University of Chicago Press; 1995.
- Maxwell JA. Qualitative Research Design: An Interactive Approach. London: SAGE Publications Ltd; 2012.
- May C, Finch T. Implementing, embedding and integrating practices: an outline of normalization process theory. Sociology 2009;43:535-54. https://doi.org/10.1177/0038038509103208.
- May C. Agency and implementation: understanding the embedding of healthcare innovations in practice. Soc Sci Med 2013;78:26-33. https://doi.org/10.1016/j.socscimed.2012.11.021.
- May C. Towards a general theory of implementation. Implement Sci 2013;8. https://doi.org/10.1186/1748-5908-8-18.
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009;4. https://doi.org/10.1186/1748-5908-4-50.
- Dopson S, Fitzgerald L, Ferlie E. Understanding change and innovation in healthcare settings: reconceptualizing the active role of context. J Change Man 2008;8:213-31. https://doi.org/10.1080/14697010802133577.
- Carroll C, Patterson M, Wood S, Booth A, Rick J, Balain S. A conceptual framework for implementation fidelity. Implement Sci 2007;2. https://doi.org/10.1186/1748-5908-2-40.
- Hulscher ME, Laurant MG, Grol RP. Process evaluation on quality improvement interventions. Qual Saf Health Care 2003;12:40-6. https://doi.org/10.1136/qhc.12.1.40.
- Dusenbury L, Brannigan R, Hansen WB, Walsh J, Falco M. Quality of implementation: developing measures crucial to understanding the diffusion of preventive interventions. Health Educ Res 2005;20:308-13. https://doi.org/10.1093/her/cyg134.
- Becker DR, Smith J, Tanzman B, Drake RE, Tremblay T. Fidelity of supported employment programs and employment outcomes. Psychiatr Serv 2001;52:834-6. https://doi.org/10.1176/appi.ps.52.6.834.
- Sanetti LMH, Kratochwill TR. Toward developing a science of treatment integrity: introduction to the special series. School Psychol Rev 2009;38:445-59.
- McGrew JH, Griss ME. Concurrent and predictive validity of two scales to assess the fidelity of implementation of supported employment. Psychiatr Rehabil J 2005;29:41-7. https://doi.org/10.2975/29.2005.41.47.
- Kogan AC, Wilber K, Mosqueda L. Person-centered care for older adults with chronic conditions and functional impairment: a systematic literature review. J Am Geriatr Soc 2016;64:e1-7. https://doi.org/10.1111/jgs.13873.
- Sharma T, Bamford M, Dodman D. Person-centred care: an overview of reviews. Contemp Nurse 2015;51:107-20. https://doi.org/10.1080/10376178.2016.1150192.
- The Health Foundation . Person-Centred Care Made Simple 2014.
- Øvretveit J. Understanding the conditions for improvement: research to discover which context influences affect improvement success. BMJ Qual Saf 2011;20:i18-23. https://doi.org/10.1136/bmjqs.2010.045955.
- Twigg J. Carework as a form of bodywork. Ageing Soc 2000;20:389-411. https://doi.org/10.1017/S0144686X99007801.
- National Institute for Health and Care Excellence (NICE) . Guide to the Methods of Technology Appraisal 2013 2013.
- Glick HA, Doshi JA, Sonnad SS. Economic Evaluation in Clinical Trials. Oxford: Oxford University Press; 2014.
- EuroQol Group . EuroQol – a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208. https://doi.org/10.1016/0168-8510(90)90421-9.
- Devlin NJ, Shah KK, Feng Y, Mulhern B, van Hout B. Valuing health-related quality of life: an EQ-5D-5L value set for England. Health Econ 2018;27:7-22. https://doi.org/10.1002/hec.3564.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2016. Canterbury: Personal Social Services Research Unit, University of Kent; 2016.
- Department of Health and Social Care . NHS Reference Costs 2015 to 2016 n.d. www.gov.uk/government/publications/nhs-reference-costs-2015-to-2016 (accessed October 2018).
- National Minimum Data Set for Social Care . Workforce Hourly Pay Rates n.d. www.nmds-sc-online.org.uk/reportengine/GuestDashboard.aspx?type=Medianhourlypay (accessed 16 January 2018).
- Hunter RM, Baio G, Butt T, Morris S, Round J, Freemantle N. An educational review of the statistical issues in analysing utility data for cost-utility analysis. PharmacoEconomics 2015;33:355-66. https://doi.org/10.1007/s40273-014-0247-6.
- Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ 2005;14:487-96. https://doi.org/10.1002/hec.944.
- Faria R, Gomes M, Epstein D, White IR. A guide to handling missing data in cost-effectiveness analysis conducted within randomised controlled trials. PharmacoEconomics 2014;32:1157-70. https://doi.org/10.1007/s40273-014-0193-3.
- Ramsey SD, Willke RJ, Glick H, Reed SD, Augustovski F, Jonsson B, et al. Cost-effectiveness analysis alongside clinical trials II – an ISPOR Good Research Practices Task Force report. Value Health 2015;18:161-72. https://doi.org/10.1016/j.jval.2015.02.001.
- White IR, Thompson SG. Adjusting for partially missing baseline measurements in randomized trials. Stat Med 2005;24:993-1007. https://doi.org/10.1002/sim.1981.
- Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2015.
- Leontjevas R, Teerenstra S, Smalbrugge M, Koopmans RT, Gerritsen DL. Quality of life assessments in nursing homes revealed a tendency of proxies to moderate patients’ self-reports. J Clin Epidemiol 2016;80:123-33. https://doi.org/10.1016/j.jclinepi.2016.07.009.
- Crespo M, Bernaldo de Quirós M, Gómez MM, Hornillos C. Quality of life of nursing home residents with dementia: a comparison of perspectives of residents, family, and staff. Gerontologist 2012;52:56-65. https://doi.org/10.1093/geront/gnr080.
- Hounsome N, Orrell M, Edwards RT. EQ-5D as a quality of life measure in people with dementia and their carers: evidence and key issues. Value Health 2011;14:390-9. https://doi.org/10.1016/j.jval.2010.08.002.
- Kunz S. Psychometric properties of the EQ-5D in a study of people with mild to moderate dementia. Qual Life Res 2010;19:425-34. https://doi.org/10.1007/s11136-010-9600-1.
- Moyle W, Murfield JE, Griffiths SG, Venturato L. Assessing quality of life of older people with dementia: a comparison of quantitative self-report and proxy accounts. J Adv Nurs 2012;68:2237-46. https://doi.org/10.1111/j.1365-2648.2011.05912.x.
- Orgeta V, Edwards RT, Hounsome B, Orrell M, Woods B. The use of the EQ-5D as a measure of health-related quality of life in people with dementia and their carers. Qual Life Res 2015;24:315-24. https://doi.org/10.1007/s11136-014-0770-0.
- Sheehan BD, Lall R, Stinton C, Mitchell K, Gage H, Holland C, et al. Patient and proxy measurement of quality of life among general hospital in-patients with dementia. Aging Ment Health 2012;16:603-7. https://doi.org/10.1080/13607863.2011.653955.
- National Institute for Health and Care Excellence (NICE) . Position Statement on Use of the EQ-5D-5L Valuation Set for England (Updated October 2019) n.d. www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/technology-appraisal-guidance/eq-5d-5l (accessed 10 December 2020).
- van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health 2012;15:708-15. https://doi.org/10.1016/j.jval.2012.02.008.
- O’Brien BJ, Briggs AH. Analysis of uncertainty in health care cost-effectiveness studies: an introduction to statistical issues and methods. Stat Methods Med Res 2002;11:455-68. https://doi.org/10.1191/0962280202sm304ra.
- Briggs AH, O’Brien BJ, Blackhouse G. Thinking outside the box: recent advances in the analysis and presentation of uncertainty in cost-effectiveness studies. Annu Rev Public Health 2002;23:377-401. https://doi.org/10.1146/annurev.publhealth.23.100901.140534.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2015. Canterbury: Personal Social Services Research Unit, University of Kent; 2015.
- Lamb SE, Bruce J, Hossain A, Ji C, Longo R, Lall R, et al. Screening and intervention to prevent falls and fractures in older people. N Engl J Med 2020;383:1848-59. https://doi.org/10.1056/NEJMoa2001500.
Appendix 1 Workstream 1: ethnographic observations of daily life in four care homes – final report
Introduction
Life expectancy has increased dramatically over the past century, with an expansion in the number of older people, in particular the oldest old (i.e. those aged ≥ 85 years). In England and Wales, it is estimated that there are 1.3 million people in this age group. 95 One consequence of this is an increase in the demand for long-term care. 10 There are currently approximately 19,000 residential and nursing homes for older adults in England, with a total capacity of 441,000 places. 96
Increasing age is associated with increasing disability. A UK survey reported that 89% of residents of CHs required care because of disability from long-term conditions, 72% had mobility problems and 62% were confused. 97 Mobility problems and reduced physical activity compound health difficulties by directly affecting physical and psychological health and by reducing opportunities to participate in social activities. 97 Observational research has reported that CH residents spend the majority of their time inactive,25 with low levels of interaction with staff. Sedentary behaviour is one of the leading preventable causes of death,98 and an inverse linear relationship exists between physical activity and all-cause mortality. 99 Encouraging residents to be more active could deliver benefits in terms of physical and psychological health, and quality of life. 12,100,101 There is evidence to suggest that, for older people, interventions focused on physical function can improve a range of outcomes, including depression and mood,17,102 balance,103 muscle strength and endurance. 104 Additional benefits may be secured through increasing social engagement,105 which has been linked with more successful ageing. 22
As part of framing this study, we had completed and updated a Cochrane review34 that focused on physical rehabilitation in elderly long-term care residents. Although the review identified the wealth of research in this area (67 studies), most of the studies had small sample sizes (median n = 56 participants) and most were conducted outside Western Europe. Nevertheless, it demonstrated the feasibility of implementing strategies to increase physical activity in CHs, and consistent statistical benefits were observed in relation to mobility and, less frequently, daily living activities. However, this and other reviews21 highlighted the need for further, more robust, studies, with clinically relevant outcomes. Several issues in particular were identified that indicated a need for further research. First, the existing research employed a wide variety of interventions and implementation approaches, with no clarity as to what might work best for residents with different characteristics and needs. Second, many of the interventions were short term and excluded the more disabled residents, without evidence that the intervention was ineffective or unsafe for these residents. Third, many interventions were resource intensive, provided by staff external to the home, and the gains were not sustained, suggesting that long-term, perhaps indefinite, programmes are required to maintain benefit. Yet surveys of CHs have reported limited involvement of NHS services. 106 Although therapy input should be available for individual clients with specific needs, it is unrealistic to expect a CH activity programme to be delivered by already overstretched services. Kerse et al. 107 reinforced the need for greater engagement of CH staff in developing and delivering practice change. We believe that it is necessary to create and ultimately deliver viable and sustainable interventions that can enhance routine physical activity in CHs.
The intent of our 5-year programme of research (funded by the National Institute for Health Research) was to develop and evaluate a complex intervention to enhance PA among CH residents that can be delivered as part of routine care, thereby improving physical and psychological outcomes. First, in WS 1, we aimed to explore, through ethnographic work, the potential for developing and delivering a PA-enhancing intervention within the daily life routines of CH residents, with the objective of assessing needs and clarifying opportunities and barriers for enhancing PA.
Methods
Sampling strategy
We purposively selected four CHs (nursing homes and residential CHs) in the Bradford area: Rowntree, Eden Park, Bournville and Hebble (care home names are pseudonyms). All of the CHs expressed willingness to participate in the research study based on summary information circulated within the Bradford Care Home Forum. The selected homes were different from each other in terms of size, setting and ownership, with one of the homes selected having a dementia unit, which enhanced our knowledge and understanding of residents with dementia. We selected homes that reported success in encouraging engagement with activities, and others that achieved more limited success in this regard. A combination of urban and rurally situated homes was also selecteded to secure, potentially, a more diverse ethnic mix of participants. Access to selected homes was informed by our experience in the PDG work. Following provisional agreement with CH managers, further visits were undertaken to explain the study to residents, staff and relatives and to respond to any queries. Information was provided to homes in the form of posters outlining the purpose of the research and providing contact details for further information.
Ethnographic work (observations)
An ethnographic approach was adopted to develop an understanding of how daily life is organised in relation to the resident profile, and the physical and social environment within which care is delivered. This combines observation and informant interviewing in a naturalistic setting. The purpose was to develop a systematic account of life as it is lived within the homes; the activities, behaviours and interactions that comprise the routine and taken-for-granted world of staff and residents; the contexts in which these occur; and the meaning of what was observed from the perspective of those involved. Ethnographic work will enable us to further our understanding of potential linkages between CH culture, staff practices and residents’ engagement with different kinds of social and physical activities. It will also allow us to better comprehend residents’ involvement with activities in the context of the spatial characteristics of different homes.
Sites were visited prior to study commencement to familiarise the researchers with the spatial environment, daily routines and regular events of the CH to develop an initial observational strategy: where to start observations, during what time points, who are the key actors involved and what should be the focus of the observation. This also provided an opportunity for staff and residents to become familiar with the researcher and to allow the researcher to explain and answer any questions about the research. Our interest was in observing what residents and staff do. This included action and interaction between residents, between staff and residents, and between residents and visitors. Given our focus, we were not interested in what particular named individuals did, although we were observing the pattern of activities and interactions of residents with different levels of disability.
In the course of observation, the researcher engaged in informal interviewing/conversation with both residents and staff, which allowed us to investigate the meanings of behaviour and action from the perspective of those involved. In our previous work, this more informal discussion proved particularly informative with residents. For those with a cognitive impairment, for example, conversation in the context of concrete experience of activities, or reminiscences of what they enjoyed in the past, triggered through conversations amongst residents, produced richer and more meaningful information than the formal interview. We looked to combine these informant interviews with formal interviews, discussed in Qualitative interviews with residents and relatives.
Observations were recorded in contemporaneous fieldnotes focused on events, activities, interactions and conversations with residents, staff and relatives. A chronological fieldwork journal combined descriptive materials with reflective accounts of the meaning of what was observed, as well as hunches and working hypotheses. These included the researcher’s impressions and reactions to the observations.
Observations undertaken during our previous work identified several emerging categories or preliminary hypotheses, and these were explored further through more focused observation:
-
The particular kinds of activities (e.g. music) that not only engage residents in PA, but also stimulate social interaction between residents, with an apparent impact on collective engagement.
-
The extent to which organised activities in the home are (or are not) based on residents’ interests and abilities.
-
Discrete focus on the potential to increase PA in respect of personal and instrumental ADL.
-
Individual and collective activity in the leisure spaces within and outside the home.
-
Resources available (room space, Wi-Fi, activity co-ordinators) to stimulate PA.
Particular emphasis will be placed on what is typical, as well as what is idiosyncratic, within and between homes, and what is distinguishable between homes that are more resident-centred in their culture and care practices that will be relevant to introducing an implementation process and homes that are less so.
The ethnographic work will enable an understanding of the physical movement undertaken by CH residents within the context of daily routine life. It will also allow for an understanding of ways in which greater physical movement may be facilitated and provide an indication of the kinds of culturally specific changes that would be required to bring about such developments, given the characteristics of residents’ physical and mental health, as well as the processes by which health and social care services are delivered.
Qualitative interviews with residents and relatives
The aims of the interviews were to clarify our findings from the ethnographic work; to examine options, preferences and choice of activities; and to examine opportunities for and barriers to their introduction. The significance of families’/friends’ continued involvement with residents in homes has been identified. 108 There are benefits to including relatives in decision-making processes109 and they have a potential role in stimulating residents’ participation in self-care. The individual interviews, which were conducted (when practical and feasible) in a quiet private area, were, with their permission, recorded and transcribed verbatim for analysis.
Informed consent was obtained from those participating in the qualitative interviews who had the capacity to consent. Advice was taken from either a PC or a NC in relation to the potential participation of CH residents who lacked capacity. Interviews with residents and/or relatives focused on their perspectives, and drew on the expressed views and experiences of residents/families. Interview schedules were devised during the process of undertaking our PDG work and were based on ethnographic interpretations of barriers to and opportunities for physical activity. These were further refined based on the ethnographic work undertaken and any site-specific issues. We discussed with participants their views on new technology, based on Global Positioning System devices, which track movement (such devices are being developed as falls detection devices). These devices may have uses, but residents’ views and perceptions are important considerations. Drawing on the observational work and synthesis of the literature, we discussed the feasibility of exemplar interventions to inform discussions, for example undertaking additional exercise during daily activities.
Qualitative interviews with staff
Purposive samples of staff from each home were selected for interview. We drew on the observational data to identify individuals who played a significant role in the life of the home, including those who may have had experience/knowledge of potential barriers to increasing PA and those who potentially may be drivers of or barriers to change. Regular visitors to the home, for example physiotherapists or community matrons, were also approached. The interviews encompassed knowledge, perspectives and attitudes towards enhancing activities, exploring opportunities for and barriers to active interventions, including perceived benefits and risks, and the contexts in which they might work for residents with different abilities and preferences. In interviews with managers from each home, we additionally explored current provision of social and exercise opportunities (e.g. activity co-ordinators, access to physiotherapy), facilities and resources available. We also examined and discussed their routine data collection and recording systems. As for residents, the interviews, which were conducted in a private area, were, with participants’ permission, recorded and transcribed verbatim for analysis. Informed consent was obtained from all staff members who participated in research interviews.
Permission was granted by an NHS ethics committee, CH managers and, if required, key personnel within the wider CH organisation to undertake the research. Informed consent or consultee opinion was sought for focused observations (i.e. shadowing particular staff members or spending time with particular residents) and interviews. Pseudonyms (including the names of the CHs) are used throughout, and efforts have been made to remove identifiable information.
Data analysis
All of the qualitative data (observations and transcribed interviews) were entered into NVivo to facilitate management of a large data set. Thus, we used grounded theory analytic techniques: concurrent data collection and analysis, constant comparison, search for disconfirming cases and memo writing. 38 But we also employed, as a sensitising lens, the framework developed in the PDG work. This conceptualised how the relationship between resident characteristics, the physical and care environment of homes, and the organisation of daily life shaped the work of staff in accomplishing daily life routines and the actions, interactions and activities of residents. The focus was on exploring these relationships empirically alongside iterative engagement with the research literature. The observations were analysed to identify actual and potential opportunities for enhancing activities, and possible opportunities for change.
Themes were identified and coded, and categories were developed. We examined within- and across-group similarities and differences, with the focus on exploring what shapes perceptions and behaviour and opportunities for and barriers to PA. The findings from all research participants shed light on those mechanisms or triggers in different care contexts that might facilitate a shift in care practices and resident motivation to optimise opportunities for increasing activity/reducing sedentary behaviour, both in ADL and in leisure spaces.
Results
Observations
Ethnographic observations40,41 were conducted in the communal spaces, as planned, on approximately 2 days per week over a period of approximately 4 months in each home by researchers (RH, AP and AL). Each session of observation took approximately 4 hours (there was some flexibility at the discretion of the researcher, however, to enable them to sufficiently capture a variety of activities taking place in the CHs). Each researcher was allocated a particular CH (or CHs) in which to conduct their observations, as is standard practice in ethnographic work. To ensure the quality and consistency of the data across the CHs, researchers visited the participating CHs (and so were familiar with the different CHs and how they were structured and organised). Observations encompassed the day, evenings and weekends to include different types of activities at different time points, as well as to facilitate contact with families and friends. 36,37 An observation guide was produced, drawing on the conceptual framework developed during the PDG and initial observations to support ongoing focusing of the observations and to ensure consistency across the CHs. The guide included prompts to observe domains such as care practices, daily routines, what work is prioritised, the organisation and delivery of care, space and use of space, interactions between staff, and interactions between staff and residents. Researchers engaged residents, staff members and visitors in ethnographic conversations41 to explore the meanings people gave to the events taking place. These conversations were particularly helpful for involving those residents with dementia and busy staff who did not have time to participate in formal qualitative interviews. Detailed fieldnotes were produced to capture the observations. The researchers shared their field notes and met regularly to discuss them.
More than 100 observations were carried out across the four homes.
Interviews
A purposive sample of staff occupying varied roles was approached from each home to take part in interviews, including care assistants, activity co-ordinators, domestic staff, senior care staff and managers. Staff differed in the nature of their involvement in the organisation and delivery of care and routine activities. Residents were sampled for interview based on diversity of their physical and cognitive capabilities, daily routines and level of physical movement. Their relatives were also approached for interview.
Fifty-five interviews were undertaken in the four CHs (Table 6).
| CH | Staff | Resident (n) | Family members (n) | Total (n) | |
|---|---|---|---|---|---|
| n | Role | ||||
| Rowntree | 10 | Activities co-ordinator/senior care assistant | 4 | 5 | 19 |
| Joint owner/manager | |||||
| Nurse (× 2) | |||||
| Senior care assistant (× 2) | |||||
| Complementary therapist (freelance) | |||||
| Care assistant | |||||
| Cleaner/laundry worker | |||||
| Physiotherapist | |||||
| Eden Park | 4 | Senior care assistant (× 2) | 6 | 4 | 14 |
| Training officer/senior care assistant | |||||
| Assistant manager | |||||
| Bournville | 4 | CH manager | 4 | 6 | 14 |
| Senior care assistant | |||||
| Care assistant (× 2) | |||||
| Hebble | 4 | Manager | 2a | 2 | 8 |
| Assistant manager | |||||
| Senior care assistant | |||||
| Care assistant | |||||
| Total | 22 | 16 | 17 | 55 | |
Rich description of daily life in participating care homes
Rowntree Nursing Home
Setting
Rowntree Nursing Home is a fairly modern two-storey nursing home situated on the outskirts of a small, rural village. Local resources are very near the nursing home. Village shopping areas are diverse in character, and include cafes, pubs and other amenities, such as the local library; these were perhaps one-quarter of a mile from the CH. A green space, incorporating a field with seating areas, was roughly 100 m from the nursing home. The CH is owned, managed and run by a family who had set it up as a limited company. There were approximately 44 residents in total, roughly eight of whom were male. Rowntree Nursing Home provided mainly permanent care; however, on occasions, respite care was offered if a bed was available. Approximately half of the residents were self-funded, with the remaining half funded by the council. In addition, four beds were available that were funded by the NHS.
The routine of the organisation is concerned with carrying out the tasks of providing meals and dispensing medicines, as well as meeting residents’ needs in terms of general care. In addition to assisting residents with moving to different areas of the CH, such as the dining areas, encouraging them to finish their meals and assisting them with toileting, a more holistic approach to satisfying residents’ social and emotional needs allowed for the provision of regular daily activities, which usually took place in the afternoons.
Organisation, management and delivery of care
The managerial hierarchy in Rowntree Nursing Home centred on the family. Key responsibilities for overall management and administration were held by the general manager and his stepson; the general manager’s wife was the nurse manager.
Hands-on care was provided by a group of experienced care workers, most of whom had been employed in Rowntree Nursing Home for a number of years; this created an atmosphere of stability and regularity around procedures and engagement with residents. Most of the care workers were female and generally aged in their 40s, with a few others aged in their 20s or 30s. Some of the care workers displayed particularly strong empathetic skills in emotionally engaging with residents and were able to spend time talking to residents, holding their hands and listening to residents for longer periods than other careworkers, who undertook care in a more perfunctory manner (Table 7 presents further details of the staff body).
| Role | Number |
|---|---|
| Director | 2 |
| Assistant manager | 1 |
| Nurse manager | 1 |
| Nurses (non-agency) | 13 |
| Senior carer (non-agency) | 9 |
| Care assistants (non-agency) | 18 |
| Activity co-ordinator | 1 |
| Domestic | 5 |
| Catering | 6 |
| Maintenance | 1 |
In general terms, routine procedures around mealtimes, dispensing medicines, and assisting residents with toileting and other aspects of personal care reflected a more holistic ethos to caring for residents. This approach involved socially interacting with residents in ways that were mindful of residents’ personal characteristics and likes/dislikes; this often produced richer, higher-quality social interactions, which seemed to support a strong sense of well-being among residents. This holistic ethos of care was in marked contrast to the more managerial approach to delivering care in other homes, driven by the need to perform specific tasks, such as gathering residents to the dining table at mealtimes, within a limited time frame, in which the quality of social interactions seemed poorer.
Care staff worked varying shift patterns according to the number of hours they worked each week. Irrespective of the shift patterns, there was always a combination of 10 care and nursing staff to cover the morning periods, nine to cover the afternoons, eight to cover the evenings and four to cover the night-time.
An experienced, creative and motivated activities co-ordinator planned and delivered various social activities and PAs, such as arts and crafts, musical performance, bingo, outdoor trips and quizzes. A physiotherapist assisted the activities co-ordinator in delivering armchair exercises on a fortnightly basis. Unusually for a CH, a complementary therapist provided various therapies, such as reiki, homeopathy and Indian head massage. In addition, a reminiscence therapist worked on a one-to-one basis with residents. Additional support was provided by speech and language therapists, nutritionists, district nurses, mental health nurses and medical consultants through the local NHS.
Some relatives took a fairly active role at the nursing home, occasionally accompanying residents and staff on day trips to provide additional support. During times when they visited the CHs, there was considerable banter between relatives and other residents, as well as with members of staff when in the communal spaces, and this conveyed a sense of warmth in the environment.
Physical environment
The approach to Rowntree Nursing Home comprised a large garden space with a lawn, flower beds and raised beds, as well as window boxes beneath residents’ windows on both upper and lower floors; the overall impact during the spring and summer period was the production of a vivid and colourful floral display.
Rowntree Nursing Home is a two-storey building. It used to be a former mill owner’s home and has been adapted and expanded in various ways that have allowed for additional rooms to become available for residents, and has enabled the conservatory space to be built. The top floor houses residents’ rooms, a dining area, the kitchen and the conservatory, which was used for delivering activities and was also a lounge space. The lower floor houses more residents’ rooms, a lounge/dining area and an administration office. Most of the residents’ rooms have en suite facilities.
In general terms, the home is decorated in warm bright colours, has modern decor and there are various pictures adorning the walls. The ground-floor lounge space is smaller than the upper lounge space and can seat approximately 10 residents. Residents would generally prefer to sit in the same seats rather than move from lounge to lounge, and so lower-floor residents would tend to remain there rather than venture to the upper floor, even to participate in activities. Seating on the ground floor was arranged around the perimeter of the lounge, with residents facing inward, and a television set was positioned in the corner of the room. A collapsible dining table rested against a wall and could seat about eight residents.
The upper-floor lounge space was much larger and there were a number of small dining tables that could each accommodate four residents. An open doorway linked the upper lounge to the conservatory space, which also acted as a lounge space. Comfortable seating was available in both the upper lounge and the conservatory space and residents tended to sit in corner spaces in both areas, which facilitated some communication.
In the lounge spaces on both floors, residents tended to do very little beyond the mid-afternoon period, usually 14.00–15.00, during which activities were provided for residents in the conservatory or lounge space on the upper floor. Residents were generally lethargic, spending time napping in their chairs, reading newspapers or else asleep. There was some conversation between residents, although this varied considerably. Sedentary behaviour was prevalent, with most residents seated for the majority of the time and shuffling infrequently between lounge space, bathroom and dining areas. However, three or four residents were extremely physically active, wandering about the CH for much of the time in a fairly aimless fashion.
Individual environment
Roughly 25 of the 40 residents were observed over the course of the fieldwork, as a large proportion spent most of their time in their rooms. Some of these residents were in exceptionally poor health.
The majority of the residents observed were aged between 80 and 100 years. Physical mobility was generally poor. Although 10 of the residents were fully able to self-mobilise, eight required a walking frame and two required the use of a wheelchair. Conversations and observations with both residents and staff indicated that most of the residents had lived for a number of years in the vicinity of Rowntree, and a number had known each other during earlier parts of their lives.
Based on the observations of the researcher, residents’ cognitive abilities were also limited, with approximately 12 residents deemed to have severe cognitive impairment and five deemed to have a mild cognitive impairment. Some of those with severe cognitive impairment were unable to speak or make themselves understood. Residents with mild cognitive impairment were able to hold conversations for short periods and to volunteer thoughts and opinions on various subjects.
The pen portraits in Box 1 summarise the key characteristics for three residents living at Rowntree Nursing Home. The first pen portrait presented describes a resident who is relatively able and active, the second is someone who is fairly average in terms of physical and cognitive ability, and the third is someone who is physically and cognitively frailer than average.
Anita could be described as being relatively more active and able than her peers. A tall woman aged in her early 90s, Anita was one of a handful of residents who took part in most activities and seemed to enjoy them all, particularly arts and crafts and musical events, during which she would sing. Unusual in being able to walk independent of any mobility aid, Anita often walked from upper to lower lounge spaces, generally in the company of her close companion, Lucy. They were generally inseparable. During conversations with Lucy, Anita reflected on her earlier enjoyment of dancing and swimming, and so being active seemed to be an important part of her background, which perhaps encouraged her to remain active. Most residents tended to occupy either the upper or the lower lounge spaces, but Anita was equally comfortable in either environment. She had a generally positive outlook, indicated by her willingness to take part in activities, and socially interacted well with peers, staff members and visitors who attended the CH. Akin to her peers, Anita seemed bored at various times during observations, but, unlike most of them, she voluntarily took part in physical actions of her own volition, such as closing the curtains or carrying cups to the kitchen. Sometimes she was observed being visited by members of her family. Anita was also prone to bouts of tearful grieving for her parents, and these occurred intermittently and seemingly without warning. During these moments of extreme distress, the holistic nature of the care environment would become apparent, as staff would respond to Anita’s grief by taking her to one side, removed from the other residents, and consoling her.
MonicaMonica could be described as being fairly typical of her peers. Monica spent most of her time either in the downstairs lounge, where she ate her meals, or in her room. Like most residents, she displayed no real interest in any communal activities provided for residents, and spent much of her time shuffling from lounge to room with the use of her walking frame. Monica was more outspoken than most of her peers, and this was partially a consequence of the difficult relationship that existed between herself and another resident, Albert, which often led to heated spats in the lounge. Monica could also be quite cantankerous at times towards other residents and staff members. Monica did not enjoy real friendships within Rowntree Nursing Home, beyond a sense of familiarity with the other residents at mealtimes, and this reflected the general experience of residents. Her cognitive skills wavered from being fairly strong to sudden episodes of confusion, when she would forget the whereabouts of her room and required assistance to return there. Like most residents, she was also strongly affected by feelings of boredom, particularly during the period prior to the evening meal, during which times she would become agitated and confused. She was visited by her daughter quite frequently. During these episodes of confusion, when Monica would sometimes lose sense of where her room was situated or how she might return to it, the personalised nature of care was such that staff would step in to assist her to her room and spend a little time talking to her, so that she became secure in her surroundings.
MadeleineA small, bespectacled woman aged about 90 years who had lived in Rowntree for 1 year or so, Madeleine’s family had migrated to West Yorkshire from Ireland when she was a young child; she could be described as being relatively frailer than her peers. She had lived with one of her daughters before the onset of Parkinson’s disease meant that she was unable to climb the stairs; this had brought about her move into nursing care. Madeleine was also affected by vascular dementia and the combination of ailments, particularly Parkinson’s, caused her to shake uncontrollably at times. Madeleine spent most of her day confined to a large sofa chair that rested on wheels in the conservatory space on the upper floor. Her physical disabilities meant that she had very limited movement and needed to be spoon-fed. Although unable to participate in activities, she enjoyed being in the lounge space and being part of what was happening around her, even if she could not participate herself. Yet, for most of the time, there was no activity or conversation, other than at mealtimes. Hence, although Madeleine had eight children and some of them visited frequently, for long periods of the day she sat alone, gazing into space, and presented a powerful sense of being socially isolated. Yet she relished the opportunity to have conversations with staff, who sometimes engaged in humorous banter with her. The holistic nature of care provided meant that, despite her profound disabilities, efforts were made to encourage Madeleine’s inclusion in organised activities. Therefore, during an observed game of bingo, despite being unable to hold a pen and strike numbers from a board, the activities co-ordinator, Alison, interacted with her and struck the numbers from her board so that Madeleine would feel included in the activity. Despite having reasonable mental capacity, however, there were some occasions when Madeleine became confused, asking when she could go ‘home’, presumably to her daughter’s home.
Care home names are pseudonyms.
Daily routine
Morning routines centred on getting residents ready for breakfast, and helping them with washing and toileting. Most residents had breakfast in the communal spaces, either on the upper or the lower floor. There was some flexibility regarding the timing of breakfast, and in the time prior to lunch residents mostly sat about idle in the lounges. Yet this was the time of the day when they seemed most alert and energised, and it seemed to represent a good opportunity for delivering PA.
Generally, residents were extremely sedentary, spending most of their time in a seated position. In terms of routine life, getting ready for mealtimes, toileting and moving into the conservatory space to take part in activities were the peak times for physical movement (beyond actual participation in the few PA-orientated sessions provided).
Lunchtimes followed a similar pattern, with residents being served at their tables, and the activities that took place in the afternoons were a highlight for residents, giving them something to do.
The activities co-ordinator organised and facilitated a range of physical and social activities on a daily basis that mainly took place during the week. Activities took place mainly in the post-lunch period from 14.00 to 15.00, although occasionally there were late-morning activities. Although the activities co-ordinator worked from 10.00 to 15.00, most of her time in the morning was occupied with providing care support to residents, such as serving lunchtime meals, and comparatively little time was spent on activities.
Most activities were social rather than physical, and were usually orientated around music. A male guitarist and singer visited once or twice a week during the post-lunch period, performing songs from the 1940s and 1950s. This person also delivered painting, as well as arts and craft sessions on a fortnightly basis. Another male guitarist and singer also performed once per month. During Saturday afternoons, female singers as well as a male saxophonist also entertained residents. Musical activities also stimulated some physical movement through foot-tapping and hand-clapping.
Other social activities included bingo sessions, quizzes on topical issues, dominoes, board games and film showings on Sunday afternoons. Occasional visits to the CH included a children’s Christmas choir, and an organisation facilitating engagement with small farm animals. Pampering sessions involving hand massage and foot spa took place on a monthly basis. Various outdoor trips to local places of interest were also planned, but most were abandoned because of inclement weather.
A reminiscence therapist also visited the CH twice weekly. This support involved one-to-one therapy in residents’ rooms and so was not subject to observation. Similarly, a complementary therapist visited twice weekly and offered reiki, head massage and reflexology, but these sessions also largely took place in residents’ rooms.
Physical activities were supported by the activities co-ordinator as well as a physiotherapist. Chair exercises were organised on a fortnightly basis for 1 hour after lunch, and involved mainly stretching movements and playing with balloons, all of which was demonstrated and participation encouraged by the activities co-ordinator and physiotherapist. Occasionally, specific PA sessions were organised, such as hoopla, bread-making and parachute games. On a monthly basis, Music for Health sessions took place. These involved residents listening to pieces of music and performing directed physical actions, as well as music-based quiz questions. They were immensely popular, as were all music-related events, with residents enjoying the singing and social interaction.
At the conclusion of the set activity period, there was often a return to boredom and physical inertia, which were regular features of the CH routine, with residents in communal spaces spending long periods of the day doing very little at all. During the lead-up to teatime, the prevailing boredom combined with residents having to share communal spaces with others who were quite confined, and this created ongoing antagonism among some residents, which sometimes caused heated disputes that seemed partially a consequence of boredom and spatial confinement. Residents generally returned to their rooms by 19.00.
Changes at Rowntree Nursing Home over the course of the fieldwork
The process of conducting interviews with residents, relatives and staff involved spending further time at Rowntree Nursing Home, which allowed for a general sense of change as the observations were concluded. The rapid physical and mental decline of some of the residents was particularly striking, with some residents who had been in relatively robust health becoming very poorly. Some decorative changes were also evident in the ground-floor lounge, which was redecorated in brighter colours with new wooden flooring fitted together, with new doors leading to the garden area at the front of the building. A flat-screen television set had also been fitted, and these changes created the visual impression of being in a large space.
Eden Park Care Home
Eden Park CH was observed approximately 2 days per week from May 2013 to mid-October 2013. During this period, the researcher spent time with residents, relatives and staff in public spaces, both the lounges and garden. Further ‘focused’ observations were made during the subsequent 6 weeks, a period when the researcher conducted interviews with residents, staff and relatives.
Setting
Owned by a small local company, Eden Park is part of a larger complex in the north of England that includes a nursing home and a development of houses and apartments for those aged > 55 years, all of whom have available to them a range of leisure facilities.
The home’s core objectives are to provide accommodation, meals, personal care and medications for older people who are no longer able to manage in their own homes. Occasionally, the home offers respite care whenever a bed is available. The home has two twin rooms and the rest are single rooms: all but one of the rooms have en suite facilities. Over the course of the fieldwork, a lounge was converted into two en suite rooms.
Organisation, management and delivery of care
Eden Park has 35 staff members. At the top of the ladder, the senior manager reports to the owner of the CH, and the assistant manager reports to the manager. During this study, Eden Park’s manager (Sandra) was rarely on the premises. The assistant manager (Chloe) took care of most managerial responsibilities and also sometimes worked on the floor as a senior-in-charge. The senior-in-charge, senior care assistants and kitchen and domestic staff all reported to the assistant manager, and the care assistants reported to the senior care assistants (Table 8 presents further information about the staff profile).
| Role | Full-time staff (n) | Part-time staff (n) |
|---|---|---|
| Manager | 1 | |
| Assistant manager | 1 | |
| Administrative assistant | 1 | |
| Senior-in-charge | 5 | 1 |
| Senior care assistant | 3 | 1 |
| Care assistant | 8 | 5 |
| Kitchen staff | 2 | 2 |
| Domestic staff | 3 | 2 |
| Total | 24 | 11 |
Interviews with residents and senior staff revealed that there was a high turnover among the care assistants, as opposed to the senior staff who had all worked at Eden Park for > 3 years. Because different ranks wore different uniforms, the organisational hierarchy was always clear.
The senior-in-charge was required to have National Vocational Qualification (NVQ) Level 3 certification, plus additional training in the administration of medications. Their role was to deputise for the assistant manager; allocate staff duties; oversee medication delivery; and handle communications with GPs, hospital admissions and ambulances. The senior care assistant was required to have NVQ Level 2 certification. Senior care assistants allocated the care assistants’ duties. Care assistants, who took care of residents’ essential daily needs (bathing, toileting, dressing, wheeling, etc.) were mostly trained in-house by the CH, on which they received NVQ Level 2 qualifications. Kitchen staff prepared residents’ food, keeping in mind their various dietary restrictions and needs. During main meals, kitchen staff also frequently helped to serve the food. Over the course of the study, a few residents were visited privately by different therapists. These visits were arranged by both staff and relatives.
Each day was divided into three shifts: morning (07.00–14.30), afternoon (14.30–21.00) night (21.00–07.00). A total of eight staff members were on hand during morning and afternoon shifts (one senior-in-charge, two senior care assistants, four care assistants and the assistant manager, who was on site and stepped in to help with delivering care if required). Care staff spent a lot of time attending to the needs of those residents who stayed in their bedrooms; therefore, staff were absent from the communal areas for long periods of time during the day. Five staff members were on duty during the night shift (one senior-in-charge, one senior care assistant and three care assistants). Domestic staff worked from 07.00 to 13.00, and kitchen staff worked from 07.00 to 16.00. After the end of the shift, their workload was shared among care staff, who often complained about the effect this additional work had on their caring roles. In addition to taking care of residents, the night shift was required to do all the domestic work, which increased their workload.
The care assistants at Eden Park adopted a task-orientated approach to care delivery, meaning that the focus was on having the caring job done within a specific time frame. Amplified by the high turnover among this group, there was minimal interaction with residents, which may have been due to inadequate knowledge about various residents. The senior staff, all of whom had worked in the CH for several years, possessed greater knowledge of the residents, and sometimes took a more resident-focused approach to delivering care. The assistant manager talked about the importance of staff ensuring that all residents got out of bed and had at least three meals per day. Senior staff also noted the importance of informing residents about the day, date, menus and activities of the day during breakfast. Overall, at Eden Park, meeting the essential care needs of residents, reinforcing routines and ensuring that residents’ safety was maintained was crucial.
Physical environment
Eden Park is housed in a two-story Victorian house that retains many original features, plus two car parks and two beautiful and spacious gardens outside.
Eden Park has eight public spaces that are located both on the upper and lower level of the building. Of the eight public spaces, six were routinely used by specific residents throughout the time of the study.
On the lower level are a staff office, two dining rooms, a kitchen, two lounges, a conservatory with a patio door (opening out onto the garden) and two communal toilets. The lower-level small office is used by all the staff for administrative purposes and to store personal items. The first dining room is used by residents who are physically frail and require help with feeding. It has two large windows, a good view of the garden and sufficient natural light throughout the day. Its furnishings include a stereo for playing music during mealtimes, two cabinets for storing residents’ medicines, three tables and a few dining chairs. Space is left around tables for residents in wheelchairs. This dining room has an exit that opens into the corridor leading to the lift, which is used to take residents to bedrooms on the upper and lower levels. A second dining room is used by residents who do not require help with feeding. With four tables, 16 chairs and a wall unit, it is a bit crowded. Because it faces north and does not get enough natural light, lights are switched on during daily meals. Both dining rooms have wooden floors and walls painted in different pastel colours.
The first lounge on the lower level seats four and has seven doors that exit to the upper-level stairwell, the toilet, the kitchen, the dining rooms, the second lounge and the main entrance. On the wall, there is the menu of the day and a notice board for planned activities. Given its central location, staff, residents, visitors, trolleys and deliveries compete in this space.
The second lounge on the lower level, which seats five, is furnished with a television, a clock, a coffee table and five heavy armchairs arranged to face the television. All residents who use these public spaces prefer to sit in this lounge, and there is considerable competition for the five chairs. This lounge opens onto a small conservatory and also has an exit to the hall with residents’ bedrooms.
The conservatory has small windows and is furnished with four heavy, closely arranged armchairs. The proximity of the chairs allows residents to form new friendships and to converse with friends, but can also lead to tensions between residents.
Reached by a lift or a steep flight of stairs, the upper level contains three communal lounges, a toilet and a manager’s office. Each communal lounge is furnished with a television, a clock, a coffee table and heavy-to-move armchairs. One lounge and one dining room (devoted to the physically frail and least able residents) also contain a stereo system for playing music. Staff post notices of the daily menu and planned activities and events on a centrally located notice board.
The upper level contains three communal lounges, a toilet, a lift and a manager’s office. The first communal lounge on the upper level is devoted to physically frail residents. It is furnished with five armchairs arranged with enough space for a hoist machine to transfer residents from their wheelchairs to the armchairs. This lounge also has a music stereo, a television and an (unused) residents’ computer and desk.
The second upstairs lounge, which seats eight people, is used for organised activities. It contains eight chairs and a television; unless there are activities, it is empty most of the time.
The third upstairs lounge contains two armchairs, two cabinets and a table, and is used by staff. All three lounges exit into the hall with residents’ bedrooms. A manager’s office is on the upper level, used mainly for administrative purposes. All lounges have attractive blue and cream carpeting that is well maintained.
Residents’ private rooms are divided into five zones which are distributed on both floors. Doors to lounges, painted brown, are heavy enough to be difficult for some residents to open. Doors to toilets are painted the same colour as the adjoining walls, making them difficult to see.
At Eden Park, rather unusually, residents and staff frequently use the home’s public spaces together. Both staff and residents with mobility roamed freely through offices, lounges, dining rooms, the garden and the stairwells. During staff’s short breaks, for instance, a few staff members generally congregated together in communal areas rooms, where they were sometimes joined by residents.
The way members of staff used the CH space was, in part, shaped by their role. The seniors-in-charge were frequently in public spaces giving medications, answering telephone calls and meeting with relatives and visitors who had enquiries. The senior care assistants and care assistants who helped residents with ADL spent most of their time in residents’ private rooms and were most evident in the CH’s public spaces during routine hours, such as mealtimes. Ten to 15 residents described by the manager as ‘poorly’ remained in their rooms and were dependent on the care assistants to help with ADL.
Individual environment
Based on the observations of the researcher, the residents of Eden Park varied in terms of their cognitive ability: some residents were very cognitively able, whereas others were in the later stages of dementia. In terms of mobility, there was a broad range: some residents were independently mobile, whereas others required a hoist. Most residents, however, experienced problems with their short-term memory and many were also physically weak. Residents frequently came to Eden Park following a crisis, such as a fall or bereavement. Many of the residents at Eden Park had either lived in the retirement flats owned by the owner of the CH or came from the neighbourhood, with the exception of approximately five residents who had come from a different town. Senior staff told the researcher that many residents come to Eden Park when they can no longer manage at home and their intent is to stay there until they die. According to the assistant manager, unusually, the proportion of privately funded residents at Eden Park CH is larger than the proportion funded by the local authority. Over the course of the fieldwork, a number of residents suffered an abrupt decline in their physical abilities and there were several deaths.
The pen portraits in Box 2 summarise key characteristics for three residents living at Eden Park CH. The first pen portrait describes a resident who was relatively able and active, the second is someone who is fairly average in terms of physical and cognitive ability, and the third is someone who is physically and cognitively frailer than average.
Myra was relatively more able and active than her fellow residents at Eden Park CH. She is 97 years of age and has been living at Eden Park CH for 1 year. From her interview, she describes her coming to the CH as unplanned:
I was just coming here just for Christmas week because most of the family were going to go away, and the majority of people in my block were going to be away, and so my son decided he didn’t want that . . . so, Sandra [the CH manager] came and persuaded me to come here for a week.
While staying at Eden Park CH, Myra’s flat flooded:
[A]pparently the place was flooded . . . there was water pouring everywhere. So they [the family] just said, ‘well you can’t go back’ . . . I walked into my flat, yes, gave one look at it, my daughter-in-law and granddaughter were there mopping up and cleaning up, I thought, ‘I can’t cope with this, it is no use.’ I must have had some kind of breakdown.
Myra is cognitively able, physically strong and walks independently without the use of a mobility aid. Although she has impaired vision and hearing, Myra managed to live independently with the support of her family, ‘I managed my life and did everything myself’. Before coming to Eden Park, Myra was a hard-working homemaker who cherished her family. She has always been active with swimming, gardening and helping take care of young children.
At Eden Park CH, Myra is very busy. In the summer, her typical day entailed going for a walk, visiting friends in the neighbourhood and going out for a meal. Myra grew up with many of the residents who now live at the CH. On a warm day, she sat in the garden and talked with other residents. She hardly ever sat in the public lounges and is very critical of other residents who sit in the lounges and watch television. She is always well dressed and boasts of being in control of her life:
I choose my clothes . . . I don’t let staff leave a dirty bin in my room . . . I don’t let dry-cleaning staff mix up my clothes, I label my laundry and count how many pieces they have taken to wash, because I don’t want to lose anything.
During autumn and winter season, she spent much of her time in her bedroom and complained of boredom:
I get very bored just sitting with nothing to do. I do have talking books, unfortunately, everything is iPod now, well I don’t understand that . . . Nobody realises that I can’t see things unfortunately . . . I expected to have everything that came to be read to me, that people would be able to spend half an hour . . .
Clarice
Clarice, 82 years of age, is originally from Trinidad and Tobago. She came to the UK when she was young. She came to Eden Park CH after dementia made it a struggle to carry on her daily life. Clarice can be thought of as fairly typical of the residents living at Eden Park CH in terms of her physical and cognitive abilities.
Clarice has good days when she walks about the lounges without assistance, sings gospel hymns, goes to the toilet on her own, walks to the dining room and reads newspapers. On her bad days, she stays in her room or is put in a wheelchair and brought to the public lounges. There, she spends most of the time sleeping and is, at times, confused. She likes to engage in short conversations with other residents and staff. In the evenings, in particular, she can become agitated and goes around closing windows and doors and switching off lights. She has children and family living close by the CH and they visit her twice a week.
LindaLinda is 98 years of age. She has been living at Eden Park CH for 6 years. She came to Eden Park CH after her family got worried about her deteriorating health. During the interview, her daughter explained that:
She started to fall and my brother and I were too frightened to leave her in her own home any longer. Dementia was just beginning . . . she couldn’t remember how to do the washing machine and things like that . . . that was it really, were desperate, it was an immediate . . . we needed help . . . when she fell and she was alone it was traumatic, I couldn’t bear it anymore.
Linda was born, raised and lived near the CH. According to her daughter, Linda did a variety of things:
She was into amateur dramatics and that is where her singing came from . . . she worked in a dress shop, she drove a van for her business, she drove an ambulance during the war, and she went out a lot.
At the CH, Linda sits in a wheelchair and is dependent on staff for washing, dressing, feeding and hoisting. Her daughter observed that her mother has changed tremendously from the time she joined the CH:
[S]he can’t speak, she says naughty words, and she is immobile now. Her teeth went, then she still managed to eat, but now, after the latest, she has a choking incident . . . and they are now liquidising all her food.
Linda spends time singing and vocalising. Because of her frailty, she is put in a separate room with other very frail residents.
Care home names are pseudonyms.
Daily routine
Residents’ daily routines revolved around the three main meals of the day: breakfast (07.30–09.30), lunch (11.30–13.00) and dinner (16.00–17.30). Because breakfast extends over 2 hours, there are periods when the dining room is empty and periods when it is full. Observations and interviews with staff showed that many residents prefer to have their breakfast in their private rooms. Those who choose to have breakfast in the public spaces are not obliged to use the dining room, and so most residents prefer to have breakfast in the public lounges as they watch television.
Observation data, further supported by staff interviews, showed that, after main meals, some residents are taken to specific lounges and sit on the same seat daily, a social seating pattern that is reinforced by the CH staff:
Hmm, if we’re trying to place them always on the same chair because it’s easier for us as well and it’s, I mean for them it’s easier because they remember where they’re sitting and they know, we always, for us it’s like we’ll go to the dining room and we’ll look so we know who’s missing, if they’ll be sitting at every day different seat we’ll be twice longer for us to count them, who’s there and who’s not, yeah.
Laurie, senior care
According to the assistant manager, this routine seating patterns suit most residents fairly well and facilitates staff efforts to meet residents’ many and varied needs:
It is knowing your residents . . . Linda doesn’t like lots of noise, lots of business, she likes to be just in the quiet. The same to Alyssa and so they have a separate lounge. Constance, Millicent and Emma read a lot and that is why you will find them in the conservatory.
Chloe, assistant manager
During mid-morning, residents are served tea, coffee, juices, water and biscuits. Staff, who are extremely busy at this time of day, do not assist physically frail residents with eating as they do at main meals. As a result, many residents either spill their drinks or end up not drinking them at all.
On Tuesdays and Fridays, staff reminded some selected residents to attend the Music for Health class that runs from 10.30–11.30. Staff also encouraged female residents to take advantage of the hairdresser who visits Eden Park on Wednesdays from 09.00 to 16.00. Most residents made use of this facility and seemed to enjoy it. On the last Friday of the month, there was a music class in the afternoon, which many residents delightfully attended.
During lunchtime, care assistants would begin to seat those who required help with eating at 11.30 in a specific dining room. At around 11.45, staff walked through the lounges fetching, supporting and encouraging other residents to come in to lunch. During this period, some residents were assisted to the toilet and into the dining rooms. A few independently mobile residents walked to the dining room just before the food was served. Just as in the lounges, the seating patterns in the dining rooms were reinforced by the care staff.
After lunch, residents spend their time in the lounges, where they rest, watch television or read newspapers. Some of those who were able to walk independently tended to wander in and out of the lounges. During warm weather, a few able residents arranged trips to local shops, theatres and museums. On warm days, two residents, Ashby and Eda, spent much of the day outside gardening. Care staff sometimes brought other residents to sit outdoors.
Afternoon tea was served at 14.45. Beginning at around 15.30, staff followed the same routine as at lunch. In the period following dinner, when most residents had returned (or were returned) to their private rooms, there were long periods of time when staff members were absent from the lounge spaces. This often meant that the few residents who remained in the lower-level lounges were left entirely on their own, sometimes for > 1 hour. During the evening was often when tensions arose between residents.
Changes at Eden Park Care Home over the course of the fieldwork
Several changes have been noted at Eden Park CH over the course of the fieldwork, including: residents’ changing use of outdoor space, care staff making an increased effort to involve those residents who were very physically and cognitively frail in activities, the dramatically declining health of several residents and the increasing dissatisfaction of some residents with the service offered by Eden Park CH.
Fieldwork commenced in May 2013; during this time, many residents spent ample time in the garden area. During the cooler weather, in October and November, residents spent increasing amounts of time in their bedrooms. Even those who had spent time in the lounges typically returned to their own rooms as soon as it got dark. With the garden no longer appealing and most lounges empty for some of the time, Eden Park took on a lonely and forlorn air.
When fieldwork began, only residents who were regulars in the communal lounges took part in music classes or other organised activities. The number of residents participating in the PA class slowly declined over the summer. In winter, just before the study was concluded, staff brought physically frail residents, many of whom had remained in their rooms, to activity classes, not to participate, but rather to listen to music and meet others. Senior staff reported that they felt that it was important for residents to come out of their rooms whenever possible to meet others. Staff were also observed to encourage residents sitting in the lounges to take part, and Irene (senior care assistant) said that, after attending training on how to help people with dementia, she now encourages other staff members to help residents participate in activities. This is a change from the earlier institutional policy of leaving such decisions to residents as a matter of free choice.
Over summer and autumn, seven Eden Park residents died. In all cases, these deaths were unpreventable and sudden. Staff report that, with older residents, these sudden fatal events are not uncommon. In addition to deaths, a number of residents suffered an abrupt decline in their physical abilities, and even a minor illness was seen to affect even the most active residents adversely. When 94-year-old Beatrix came to Eden Park in July 2013, for instance, she was active and well connected with the CH community. Her days were filled with things to do and people to meet. By the end of the study, Beatrix suffered continual bouts of diarrhoea, could no longer walk and was virtually bedridden.
Over the course of the study, the researcher observed a shift in some residents’ feelings about Eden Park CH. By the end of the study, a group of long-term residents who are physically mobile and who had good cognitive abilities complained to the researcher about boredom and the lack of an activities co-ordinator, the need for a new manager who could be present throughout the week and the lack of staff response to buzzers.
Towards the completion of this study, residents also noted that the way junior staff interacted with them had changed:
The staff changed a lot, honestly. They are not friendly as they used to be. The good ones [mostly care assistants] have left.
Ashby, CH resident
These changes were noticed by other residents, who felt that it was due to high turnover among this group:
They don’t stay [care assistants]. Only bad ones are still here . . . I don’t know their names as they are always hurrying and when you know them, they are gone . . . so we have to put up with unfriendly new faces everyday . . . you don’t know who is coming to your room next.
Myra, CH resident
Most emphatically of all, these residents complained about their desire to be allowed out without being accompanied by care staff. As one disgruntled interviewee commented:
It is crazy, absolutely crazy. The law states you’ve got to have three members of staff on here. Weekend is worse, it [Eden Park] has gone downhill a lot. I don’t think Beatrix, Eda, Evie have a good word either. This place wants a very good old shake-up, I tell you.
Ashby, CH resident
These residents had spoken well of Eden Park at the beginning of this study.
In addition, there were four residents with good mobility and short-term memory loss who joined the CH when this study had already began. These residents complained that management had misled them into coming to the home by promising activities that are not in fact offered in the recruitment package.
Bourneville Care Home
Observations took place 2 days per week from early June 2013 to mid-October 2013 in communal spaces: the front and rear lounges, and the large outdoor garden space.
Setting
Bourneville CH is a three-storey residential home that is owned, run and managed by a large international corporate provider of health and social care to older adults in the UK. It is home to roughly 25 residents, virtually all of whom are female. It is located in a town in a semirural district, with ready access to moorland, on the outskirts of a large city in the north of England. It has ready access to shops and local amenities. It offers a combination of mainly permanent care, as well as more limited respite and rehabilitative care.
Organisation, management and delivery of care
The CH has a defined managerial hierarchy, with a general manager overseeing a deputy manager and a senior care assistant, who were responsible for medicine management. These senior staff members dictate the daily care procedures to more junior care assistants, although care is, in some ways, governed by residents’ requests for assistance or as a consequence of crises, such as falls (Table 9).
| Role | Number |
|---|---|
| Manager | 1 |
| Nurse manager | 1 |
| Non-agency senior carers | 5 |
| Non-agency carers | 16 |
| Non-agency activity co-ordinators | 1 |
| Non-agency domestic staff | 4 |
| Non-agency catering staff | 4 |
| Non-agency maintenance staff | 1 |
Care staff worked varying shift patterns according to the number of hours they worked each week.
Shift patterns meant that there were four care assistants in the morning, three in the afternoon and three on the night shift. There is always a senior care assistant on duty. Some staff work 6-hour shifts (i.e. 08.00–14.00 or 14.00–20.00), but others work 12-hour shifts (i.e. 08.00–20.00 or 20.00–08.00). The breakdown of staff that cover these shift patterns is given in Table 10.
| Shift patterns | Staffing |
|---|---|
| 08.00–20.00; 20.00–08.00 | One senior carer; two carers |
| 14.00–20.00 | One senior carer; two carers |
| 08.00–14.00 | One senior carer; two carers |
In addition, district nurses and physiotherapists provided additional health care, based on identified residents’ needs.
An activity co-ordinator was in post who was much less experienced than the one employed at Rowntree CH, and did not offer the same variety of activities for residents.
Most hands-on care is undertaken by care assistants, comprising mainly women aged over 40 years, with one or two younger women aged in their 20s. In addition, there is a chef, a gardener, an office-based administrative worker and a part-time activities co-ordinator, who was responsible for delivering activities for residents. Some musical entertainers came in to perform for residents, but not as frequently as at Rowntree Nursing Home. As a residential CH, there were no nursing staff on site, although there were regular visits by district nurses as well as by GPs.
Both senior care assistants were highly experienced, although the CH manager had been appointed more recently. The care assistants presented a more mixed group; some of them had worked at Bourneville CH for a number of years, or else seemed very experienced.
Care assistants attend to a variety of daily tasks: responding to the sound of buzzers in residents’ rooms; helping them with toileting; feeding, when necessary; and maintaining daily records in the personalised care plan documents, which was a source of irritation for them, as it was seen to represent a laborious process. Tensions between the general manager and junior staff were evident through the conduct of team meetings and staff demeanour in the lounges. There was a general sense of low morale among staff, who seemed harassed for the most part and overwhelmed by their workload.
Although there is relative stability within the staff group, there was a sense of disquiet between the manager and care staff. During the period of observation, one member of care staff had left. After the study, it came to light that the CH manager had departed the CH, and had apparently taken up a managerial post at another site in the same organisation.
The ethos of care provided at Bourneville CH might best be described as managerial, in that the primary focus was on the performance of set tasks, such as undertaking paperwork or assisting residents to and from the dining area, within a highly restricted time frame. Hence, care staff would scuttle briskly from resident to resident in the lounge space, and back and forth to residents’ rooms, constantly mindful of the urgent needs of other residents. This produced a sense of anxiety, such that social interactions with residents became characterised by brief, rushed verbal exchanges centred on the task at hand, rather than meaningful engagement. The quality of these exchanges were limited in scope and depth, and did not support the development of relationship-based interactions that were representative of a more holistic ethos, as observed in Rowntree Nursing Home.
Relatives and friends played a fairly neutral role at Bourneville, spending time with the residents, but there was not the same sense of conviviality with other residents or with members of staff. Relatives spent their time mainly with their loved ones, and not really interacting with others in communal spaces.
Physical environment
Bourneville CH is a three-storey building set in its own grounds that has been converted from being a private home. The internal decor of Bourneville CH seemed quite old-fashioned, with the hallway area marked by dark wooden panelling, which gave it a gloomy appearance, as no natural light could penetrate this area of the building.
The top floor contains office space and a small care workers’ rest room. The ground and first floors house residents’ rooms interspersed with some communal bathrooms, although most rooms are en suite. The communal spaces are all on the ground floor, where two lounges are provided.
The front lounge, which more residents tend to use, could be entered from the main doorway. On the left side of this lounge were a number of chairs positioned along a wall facing inward towards a television set. On the right side were two small dining tables that could each seat about six residents. A doorway linked to a second rear lounge. On the right side of this rear lounge was a large dining table that could seat about a dozen residents. This table also acted as a resource for care staff to complete resident care-related documentation. Seating in this lounge was arranged along the same plane as the main lounge. During the day, residents were generally evenly spaced between both of the ground floor lounges, although some residents very rarely, if ever, frequented communal areas. Staff seemed to oscillate fairly evenly across both areas, as well as the dining areas, although they would often leave these areas to attend to residents who had requested assistance by pressing their buzzers.
The CH is surrounded by copious garden space, with raised beds for planting, ample seating, tables and secure pathways all around. Yet residents were generally reluctant to venture outdoors, although a few were more than happy to do so, and to stroll around the outdoor space. The exit from the rear lounge to the garden had a sloping ramp that was a barrier to those using a walking frame, as the width of the ramp was narrower than the walking frame.
Over the course of the fieldwork, significant structural changes in the front lounge involved the creation of a care workers’ office for general administration. This meant that the dining space in the front lounge, incorporating some small tables, was removed so that all residents were now dining in the rear lounge. This seemed to allow for greater social interaction among residents through having greater numbers of residents in a small space.
Individual environment
Seventeen residents were observed. Their ages ranged from roughly 85 to 100 years. Generally, physical mobility was poor, with two residents requiring a hoist to transfer them from armchair to wheelchair, three wheelchair users, six requiring a walking frame and five requiring either a walking stick or a walking frame. One resident could walk without assistance. There was a strong sense that most of the residents had spent a number of years living in the local environment prior to moving to the CH, based on the kinds of conversations that ensued between residents. The residents’ lengths of stay varied from a few months to several years. The CH manager was unable to provide the research team with information regarding the number of residents who were funded by the local authority or self-funded, owing to matters of confidentiality.
There are a total of 26 beds at Bourneville CH, with one of the residents currently in hospital. Based on the researcher’s observations, four residents had full capacity, eight had mild cognitive impairment, two had greater impairment and three had severe impairment. Some of those with a severe impairment were unable to verbally communicate and required assistance with eating. The majority, however, could maintain a simple conversation.
Over the course of the study, the rapid physical and mental decline of some of the residents was particularly striking, with some residents who had been in relatively robust health becoming very poorly, or dying.
The pen portraits in Box 3 summarise key characteristics for three residents living at Bourneville CH. The first pen portrait presented describes a resident who was relatively able and active, the second is someone who is fairly average in terms of physical and cognitive ability, and the third is someone who is physically and cognitively frailer than average.
Flora, a resident aged about 90 years, could be described as being relatively more active and able than her peers. She came into Bourneville after she had fallen on some ice near her home, and was initially due to stay there for 1 week or so. A keen hiker in different parts of the UK since her youth, Flora’s energy and enthusiasm for being outdoors was in stark contrast to her peers, who were generally reluctant to venture into the garden space. Flora walked with two walking sticks, which she did not lean on but which acted as more of a guide, and had an appreciation of the need to remain physically active. Yet the more mechanistic approach to care meant that Flora was not always encouraged to take walks, partly, it seemed, as this would mean that a care worker would need to accompany her, but also because of the lesser importance attached to enhancing physical movement in comparison with achieving time-bound targets. She further differed from most of her peers in having an array of friends visiting her regularly, which seemed to help in connecting her with mainstream life external to Bourneville CH. Flora also struck up conversations with residents in the rear lounge, all of whom seemed to have come from the local community. Over the period of observation, it became clear that Flora would need to take up permanent residence. The process of adjustment was difficult for her, particularly the prospect of selling her home, yet was tempered by a realisation that she would be safer in a residential care setting. Flora maintained strong mental capacity throughout the period of observation.
PoppyPoppy, a resident approximately 92 years of age, could be described as being fairly typical of her peers. Poppy entered Bourneville CH about 2 years ago, having lived alone at home independently for many years, with some support from her family. However, she had become confused, and then suffered a fall. After a short spell in hospital, followed by some time in a rehabilitation centre, it was decided that she could no longer live independently. She had been very active in her local community before coming into residential care, but now spent most of the time oscillating from her room to the lounges, and, when in communal spaces, would sit quietly by herself. Her dementia meant that her capacity to communicate clearly was limited, as the focus of her concentration would shift rapidly, so she spoke in a fairly slow and deliberate fashion. She infrequently spoke to the other residents, other than at mealtimes, and the conversations often seemed quite short and stilted. Her family would visit her each week, but the conversations were often fairly limited, as Poppy’s declining mental capacity meant that she had begun to forget the names of family members. Poppy used a walking frame to move from space to space, and she would usually sit adjacent to the television set, although she did not watch television. Despite the physical effort involved in moving about, Poppy maintained the determination to do so, and this sense of managing to look after herself as best she could extended to toileting and dressing herself. She did not participate in any activities, although few were provided during the period of observation. The managerial ethos of Bourneville CH meant that, on those occasions when Poppy became confused, she did not receive the kind of supportive social interaction from care staff that may have provided valuable reassurance.
GeraldineGeraldine could be described as being relatively frailer than her peers. Aged ≈ 99 years, Geraldine’s social and cultural background had been centred on the Methodist church and her working life focused on a series of clerical jobs. Prior to moving into Bourneville, Geraldine had lived in a sheltered accommodation facility that was adjacent to it. Following a hip replacement, Geraldine became less willing to walk independently and became reliant on using a walking frame. A further stay in hospital was followed by a 2-year stay in a rehabilitation centre, and then her inability to manage on her own meant that she moved into Bourneville, where she had lived for approximately 2 years. During the period of observation, Geraldine, a small, frail woman, had declined, so she no longer used a walking frame and spent her time seated in a chair in the lounge space. Here she would sit hunched forward facing the television set, which she watched without really following the programmes, and this seemed to be a way of alleviating boredom. She required a hoist to be transferred to a wheelchair to go to the toilet or to the dining table for her meals, although she often ate alone in her chair. Since moving into the CH, Geraldine had taken part in a few activities, but this had declined so that she was observed participating in a game of quoits on a single occasion, although few opportunities were provided. She did not communicate with other residents, despite having strong verbal skills; she occasionally communicated with care staff, although there was an air of frustration about these interactions, as she was often irked by having to wait for two members of staff to be able to operate the hoist. Geraldine was also quite confused at times, partly as a consequence of an infection that caused her to have a short stay in hospital, and generally unhappy with her quality of life at Bourneville CH. Staff interaction with Geraldine was limited, partially a consequence of Geraldine’s low mood, and generally involved placing meals and drinks on low tables beside her and assisting her with toileting or getting to the dining table. During the performance of these actions, the quality of conversation between Geraldine and care staff seemed generally poor, and did not convey a sense of familiarity with Geraldine’s life and interests. Interactions were mainly stilted in nature, reflecting an ethos centred on task performance rather than meaningful, sustained interactions with residents, as observed at Rowntree Nursing Home.
Care home names are pseudonyms.
Daily routine
The routines of daily living are centred on delivering medicines and organising mealtimes. The morning routine involves care workers spending time in residents’ rooms preparing them for breakfast. Residents gather at the dining tables from the lounge spaces, if they have been awake for a while, or use the lift to reach the dining room from the second floor. The general sense is that this can take some time, depending on residents’ health and well-being, given that some residents have their breakfast when most of the others have finished. Medicines management is carried out by the senior care assistants, who are responsible for handing out medicines and maintaining paper records. This process is carried out in the mornings, afternoons and evenings.
During the morning period between breakfast and lunchtime (about 12.30), and then between lunchtime and teatime (about 17.00), the residents spend most of their time sitting idle and bored, and some of them are frustrated by the absence of things to do. Despite there being an activities co-ordinator, and a weekly programme of activities that are supposed to occur, in practice, very few formal, organised activities were provided, other than a single singing session and two quiz sessions. One outdoor canal trip has been arranged. The programme of weekly activities includes two armchair exercises, a quiz, bingo, a craft session and board games. Hence, there is a complete disconnect between what is supposed to occur and what actually happens.
Informal activities have involved some residents going for short walks outdoors during fine weather, or sitting outside on benches, but these are infrequent. Sometimes the activity co-ordinator engages with some residents on a one-to-one basis in their rooms, but the nature of this engagement is not known. The mood of lethargy culminates in residents snoozing for most of the day.
Changes at Bourneville Care Home over the course of the fieldwork
Over the course of the fieldwork, there was an increase in PA through the delivery of armchair exercises three times per week; the participation of some residents, who seemed uninterested in PA during the period of observation, was notable.
Hebble House Care Home
Fieldwork was conducted at Hebble House between July 2013 and December 2013.
Setting
Hebble House is a local authority-run CH that specialises in caring for older adults with a diagnosis of dementia. It is situated in a large, post-war social housing estate on the outskirts of a large city in Yorkshire. The area surrounding the CH is one of the most deprived in the region, and, according to information obtained from the local council, has a poor reputation, with poor housing stock, low levels of economic activity and high rates of crime. Talking to people who live locally, however, there is a strong sense of community; this is echoed by the presence of the community garden that runs down one side of the CH. The CH is approximately 5 minutes’ walking distance from local amenities, including a chemist, local shops, a church and transport links to the city centre. Other amenities, such as pubs, cafes, restaurants and supermarkets are a short (10- to 15-minute) bus ride away in the city centre.
The home is registered to provide residential care for 35 adults, aged ≥ 65 years, and also acts as a day centre for those living in the local community. In discussions with staff members, some referred to the CH as an elderly mentally infirm (EMI) unit. Although an outdated term, EMI refers to the fact that people throughout all stages of dementia (including those in the later stages of dementia) and those who experience other mental health problems associated with their diagnosis are cared for in this unit. The CQC carried out a routine inspection of the CH during the period of fieldwork, and produced a positive report, with the CH meeting all of the standards against which it was assessed.
At the beginning of the fieldwork, Hebble House accepted both permanent and short-stay residents, with a specific wing of the CH allocated for those who were short-stay residents. Over the course of the fieldwork, however, the number of short-stay residents placed at Hebble House to undergo assessment increased significantly, as they stopped accepting new permanent residents. This resulted in short-stay residents residing in all four wings of the CH.
Organisation, management and delivery of care
The staff body consists of 65 members and is well established, with a low turnover. The CH manager, Laura, has worked in management roles for the previous 12 years. She moved to work at Hebble House 7 years ago, and has been the CH manager for 5 years. She is trained to NVQ level four in dementia studies and dementia care. In conversations with Laura, she communicates a desire to create an ethos of enabling residents at Hebble House, but acknowledges the challenges of achieving this, which included the busyness of staff and their fear of putting residents at risk.
The CH manager worked weekdays and had overall responsibility for running the CH; she had to ensure that care was delivered to a high standard, that care plans were accurate and implemented, that issues with her staff were quickly and appropriately resolved, and that any bad practice was identified and addressed. She conducted staff supervisions and appraisals and oversaw the recruitment of new staff members. She also dealt with complex cases. Laura was also involved with overseeing ‘disciplinaries’ at other local authority-run CHs. She reported to the divisional manager.
Laura was initially supported by a full-time deputy manager, a full-time assistant unit manager and an administrator. During the day (including at weekends), the deputy manager or the assistant unit manager was usually present. Although the staff body was fairly static, a significant loss was the deputy manager, who left her post mid-way through the fieldwork. This post remains vacant.
The assistant unit manager, Karen, assisted the CH manager with staff supervisions and appraisals, oversaw the staff rota and booked in the medications (with the support of the administrator). She also helped with the running of the staff office, which involved liaising with external health and social care professionals and responding to any issues that arose during the day. A significant amount of her time, however, was spent on carrying out residents’ assessments (short stay):
So I just prioritise what needs doing. So if I need to do me flexi-bed assessments, depending on how many I’ve got in, you see, I could have six to do in a week, because if all six have come in at once (. . .). So it’s very varied, like I say, very different, and I prioritise through, like I say, the flexi-beds and things like that because I have to be on a timeline with them, because the social work, they only have 4 weeks in a flexi-bed (. . .).
What about when you’re working on the office, what kind of, is your priorities then, is that . . .?
It’s all about the service users. Making sure the environment’s clean, tidy, making sure that everybody’s doing what they should be doing, making sure the doctors are called if they’re needed, any of our service users as are end-of-life care, ‘cause we’ve got a couple, I like to be involved in that, in their care, at least once a day, I like to be able to go in and assist with changing or checking pressure points and things like that, making sure that the skin’s not breaking down, and just making sure generally that they’re OK (. . .). So, I prioritise, my first thing when I come on duty, I do the handover, and then anybody that’s an end-of-life care, I like to make sure I go and see ‘em (. . .) before the office gets too busy, because that office gets absolutely manic.
The home employed four, and then later five, senior carers and 23 care assistants (who do the majority of the face-to-face care). The hours worked by members of the care team ranged from 37 hours per week (full time) to 22 hours per week. In addition to their NVQ care qualifications, the majority of care staff have undergone dementia training. The senior carers and care assistants work in shift patterns. There are three shifts to cover the care throughout each 24-hour period, and each shift overlaps by at least 15 minutes to allow for transfer of information. The morning shift runs from 07.15 to 14:45, the afternoon shift runs from 14:15 to 21:45 and the night shift runs from 21:30 to 07:30. The morning and afternoon shifts have a senior carer and four care assistants (one care assistant will be allocated to each of the four wings of the CH; the remaining two will ‘float’ between wings to assist with jobs that need more than one person, e.g. using the hoist). The night shift has one senior carer and two care assistants.
Senior carers were responsible for the running of their allocated shift and overseeing the work of the care assistants. This comprised tasks such as allocating the care assistants to particular areas of the CH, conducting the handover, arranging visits from health-care professionals, distributing medications (although some care assistants had also been trained to do this), keeping the diary and communication book up to date, helping out the care assistants and working with those residents who were distressed:
Could you take me through a typical day, what a typical shift would look like for you, from when you get in to when you finish?
Well, me, I’m always in half an hour before me shift. Normally, we do the allocation where people are going, where the staff are going on a morning, get the handover from night staff or if we’re in on lates, then it’s often the morning staff. If we’re on a mornings, we get the handover then we give the handover to the staff; they need to get a full handover before they go onto floor. They go onto the floor, we start looking in the diary, communication book to see what needs doing for that day, so 8 o’clock we start getting in touch with the doctors or the district nurses or community matron, social workers if we need to and deal with the stuff that we need to deal with. Then we go into medication, which that can take you quite a while and after you’ve done the medication, normally, it’s just seeing the running of the floor or whichever floor or the building if it comes to where you’re working on your own and just to make sure that everybody’s doing what they’re supposed to be doing. We have a lot of service users that are demanding, I won’t say demanding, that they need more your help than anybody else (. . .) on an afternoon, washing up, setting the tables, you know, seeing to laundry, so if you can take a little bit of that off ‘em [the care assistants], you know, then the shift runs a lot smoothly.
Care assistants were responsible for face-to-face care: their role comprised bath and body work (such as washing, dressing and toileting residents), serving meals and assisting residents to eat and drink, ensuring residents were well hydrated and filling out the necessary paperwork. They tended to prioritise residents’ health needs and were also attentive to whether or not residents were distressed. If they had time, care assistants would sit and talk with residents, sometimes engaging them in activities. Care assistants would often sit and talk with residents while completing their paperwork:
I’ll start at half past 7, I’ll come up [upstairs], try and give personal care and then I have to break off at 9 o’clock from personal care in order to start dispensing the medications so they’re getting it at the allotted times. So I have to do medication and then, once that’s done, it’s go back to my service users and then it’s any toileting or if there’s anything that they need to try and get that in; then I break off at 11 o’clock again to get the files out to write down what’s happened in the morning, and at that time it’s toileting, you know, taking them, assisting with toileting and then back into the dining room for lunch. Once they’ve had their lunch, you start your transfers and then I’m broken off again ‘cause I have to go back again and start the paperwork to write down what diet input they’ve had and how they’ve been, so it’s constantly breaking away from your service users to make sure the paperwork is done.
Maya, care assistant, Hebble House
There was a sense of collaborative working at the CH and staff members commented that they felt supported by others, including those in more senior and managerial positions. One complaint noted by the researcher over the period of fieldwork related to the increased workload created by the intake of more short-stay residents, who were there to be assessed; therefore, their care needs were unknown. Depending on the particular resident, such placements could result in care assistants spending a considerable amount of time helping the resident to settle in, and learning about the new resident’s needs, behaviours and preferences. This often meant that care assistants had less time for permanent residents. Care staff also sometimes mentioned that it would be beneficial to have more care staff on duty, but also acknowledged that this was always going to be the case in such settings.
Domestics, a chef, kitchen assistants and a handyman were also employed at Hebble House. Over the course of the research, the activity co-ordinator post was vacant (due to maternity leave). However, towards the end of the fieldwork, they had recruited a new activities co-ordinator who was due to start in the new year. There was also an exercise professional who visited the home once a fortnight to lead a seated exercise session. External people were also brought in from time to time to provide activities for residents, including ‘pat the dog’.
In addition to the paid staff, there was a volunteer who came to the home twice per week to provide one-to-one support to a particular resident. Over the course of the fieldwork, the activity co-ordinator, who was on maternity leave, arranged for a group of volunteers from a local business to come to the CH and decorate a sensory room and tidy one of the gardens. There was also a small, but active, group of relatives who organised special events, including a Halloween party and fundraising events, and tried to arrange trips out for the residents. Over the course of the fieldwork, this group of relatives were successful at arranging a range of events. However, they struggled to arrange a trip out for the residents because of a lack of volunteers and transport.
The staff at Hebble House had access to a wide range of external professionals from whom they regularly sought input and advice. Health-care professionals were called on regularly, including doctors, the district nurse and the community matron. They also liaised with social workers. In addition, the staff at Hebble House worked closely with the community psychiatric nurses and, if a particular resident was causing concern in terms of their behaviour, they worked together with this team and with the resident’s family members to produce a plan of how they could best manage the situation. External experts were brought in to assess the mobility of residents if staff members noted a change in residents’ mobility.
Physical environment
Hebble House is a fairly modern, T-shaped building with two floors. Inside, the CH is divided into four wings (two downstairs and two upstairs), as well as a large, open-plan day centre space on the ground floor. Each of the four wings comprises a lounge area, a kitchen/dining room area, bathrooms and toilets, and the residents’ bedrooms. Residents’ bedrooms were small, with just enough room for a single bed, a wardrobe, a chair and a few personal belongings. Residents rarely spent time in their rooms, unless they were unwell or receiving palliative care. Residents tended to spend time in the lounge on their wing, moving a short distance to the kitchen/dining area for meals.
Each floor of the CH also had a brightly coloured ‘sensory room’, which was rarely used by residents or staff, and an ‘activity room’ which, for the duration of the fieldwork, was used as storage space. The upper floor also had a small additional lounge, which was sometimes used by residents. Care assistants would also very occasionally sit Grace (see Box 4) in this room with another resident or, if she was on her own, they would sit with her. Grace was unable to speak, but she vocalised, sometimes loudly, which resulted in other residents shouting at her. The ground floor also had a ‘smoking room’, a room used by the hairdresser, the laundry room and the staff locker rooms. The seated exercise class and other formally organised activities took place in the day centre area.
Although each of the four wings of the CH were, in fact, long corridors, attempts had been made to make them more accessible for residents. For instance, the toilet doors were painted red and images were hung on all the doors to communicate the purpose of the room, such as a picture of a plate, knife and fork on the doors to the kitchen/dining rooms. Personal photographs had been placed on residents’ bedroom doors, to help them identify their room. There was also a ‘pit-stop’ chair on the lower level, so that residents could pause and have a rest if they tired when walking along the corridor. This chair was located outside the main staff office, and so Joy (see Box 4), who liked to be kept informed of goings-on, used to spend a lot of time sat in the pit-stop chair.
Despite attempts to make Hebble House a more accessible and homely environment for residents, some residents were unable to orientate themselves in the setting. Those residents with moderate and later-stage dementia (the majority) became disorientated if they left the lounge areas, and many were unable to locate the toilet or their bedrooms. Many residents were unaware that they were living in the CH. Staff frequently responded to a wandering resident by asking them where they were going and, if the resident replied that they did not know, they were routinely encouraged to return to their chair in the lounge. Some residents, who were physically able and happy to venture beyond the lounge area, were allowed to wander the corridors.
The floors were linked by two staircases, both of which were out of bounds for residents, and a lift. Although residents were allowed to use the lift, there was only one resident, James, who regularly did so to access the smoking room on the lower level. Mabel occasionally used the lift if she wished to speak with a senior member of staff, which usually occurred when she had become distressed or disgruntled with the care assistants or her fellow residents as a result of a perceived misdemeanour. The vast majority of residents, therefore, rarely ventured beyond the floor where their rooms were located. Residents from the upper floor were taken to the lower floor by care assistants so that they could visit the hairdresser, and, occasionally, so that they could sit in the day centre, participate in the seated exercise class or go for a walk in the garden. Care assistants reported that residents liked routine and the familiar space of their lounge area, and so often disliked it if taken to another area of the CH.
Although there were distinctive areas of the CH that were intended for staff use, boundaries between staff spaces and resident spaces were somewhat blurred. On both floors, there is office space for staff, including the CH manager’s office, assistant unit manager’s and administrator’s office, and general staff office on the ground floor, and a small office space for those working on the top floor. With the exception of the assistant unit manager’s and administrator’s office, the offices all had large glass windows that looked out onto lounge areas. The CH manager, Laura, regularly spent time in all three offices on the lower level, and also with residents in the communal areas of the CH. Over the course of the study, she began inviting a recently arrived resident, Julie (see Box 4), into her office while she was working. She encouraged Julie to occupy herself by organising piles of paper, which Laura felt Julie enjoyed. The door to the general staff office, where the majority of the day-to-day running of the CH took place, was often propped open. Some residents, in particular Joy and Polly, would sit outside this office interacting with staff members. Occasionally, one or two residents would sit in this office with staff members. The office on the upper floor was a thoroughfare between a lounge and kitchen/dining room and the residents’ bedrooms; therefore, residents passed through this office. Care assistants rarely spent much time in the office spaces. If they had time, they would also sit with residents in the lounge areas and engage them in conversation, reminiscence or other ad hoc activities such as singing, throwing a ball or playing a game. They would also complete their paperwork in the lounge areas or kitchen/dining rooms.
The CH is surrounded by three small gardens and a car park. One of the gardens had been developed into a community space, where local residents and school children grow vegetables. There was, however, little interaction observed between those who use the community garden and the CH residents. During the warm weather, some day-centre participants and CH residents sat outside in the gardens. It tended to be the case that those residents who lived on the lower level were those who were able (or were assisted) to access the garden spaces, with the exception of a male resident, James, who, despite living on the upper level, regularly used the lift, unaccompanied, to access the lower level.
The external doors of the CH were locked and residents rarely left the CH setting. Occasionally, one resident, Julie, would go along for a ride in the minibus with the day-centre participants when they were driven home. Residents were occasionally taken for a short walk and a cigarette. Towards the end of the fieldwork, a small group of residents were taken for a pub lunch. This had been requested by a particular resident, Caroline, and facilitated by several committed care assistants and the CH manager, Laura. A small group of relatives tried to organise a day trip for residents; however, this was indefinitely postponed. Relatives and visitors rarely took residents out of the CH. In her interview, the CH manager bemoaned the fact that relatives rarely took residents out:
. . . I feel sad that the families as well think that, once their loved one comes here, that that’s it.
Do you think that’s quite common?
I think that if the families came in and continued doing what they used to do with their loved one in their home environment, I think that person would be maintained at a steadier level for a longer period of time. So if they still continued to take them out to the pub of an evening or if they still continued to say ‘I’m, mum I’m popping to Morrison’s, do you want to come with me?’ But it’s like, as soon as they come through the door, that’s it, the family don’t want, think that’s it, there’s nothing more that they can do. (. . .) But they should just carry on the way that they used to do, if you know what I mean? Because that would help. It’s like none of them go out for Christmas but why wouldn’t you want to take them out and have them over at your house for Christmas? I don’t understand it. That, isn’t that what families do? (. . .) I know some of them, like Edith, couldn’t at the moment but Julie could, Joy could. There’s still quite a few upstairs that could, but it’s just like, that’s it, no they don’t. They don’t want to do it. And, see, that would keep them going, wouldn’t it? Stimulate their mind, you know, it’s a change of scenery going out for the day. It’s sad, I think.
Interviews with residents’ relatives, however, highlighted some of the difficulties of taking residents out of the CH, including that residents sometimes became distressed and disorientated by an unfamiliar environment.
Individual environment
The majority of residents are female and have moderate, or are in the later stages of, dementia. Many therefore have impaired memory. Some also experience visual disturbances, mobility problems, communication impairments, and/or impaired eating and appetite. In terms of mobility and physical abilities, there is great variation among the residents. The majority of residents require some form of support from a staff member (i.e. they usually require a staff member to physically support or encourage and instruct them when moving). Several are independently mobile and several residents require a hoist.
The pen portraits in Box 4 summarise key characteristics for three residents living at Hebble House. The first pen portrait describes a resident who was relatively able and active, the second is someone who is fairly average in terms of physical and cognitive ability and the third is someone who is physically and cognitively frailer than average.
Julie was relatively physically able and active, compared with her fellow residents. She moved to Hebble House around the time fieldwork commenced, in July 2013. She has not mentioned a partner or husband, but she has two children who visit her regularly (at least once a week).
Julie is a tall, slender woman who has a friendly and bubbly character. She often plays the comedian and attempts to make staff, residents and myself laugh at her comic asides. Julie can walk independently with no mobility aids and often spends her days alternating between sitting in one of the downstairs lounges and walking around the lower level of the CH. If music is playing in a lounge area, Julie will often start to dance and care staff will encourage her to move to the music. For the first few weeks she was living in the CH, she became close to James and they would sometimes dance together. More recently, however, James has remained on the upper level of the CH and they no longer spend time together.
Julie and the researcher had short conversations, but did not manage to converse for any length of time or in any great depth. On her good days, Julie is aware that she is living at the CH. On her bad days, Julie seems to be aware that she is in an institution of some sort, but she does not know why and often thinks she has only been there for a few hours. Adapting to life in the CH has been difficult for Julie, and she regularly talks about going home. On occasions, she collects some of her belongings to sit in the front lounge waiting to go home. The CH manager and care assistants created roles for Julie, to help her settle in to the CH and to give her a purpose to her day. These roles included helping in the laundry and doing paperwork in the manager’s office.
JoyJoy is in her mid-70s. She grew up in the local area, but lived abroad for almost 20 years. She talks fondly about her past and her husband. Joy’s husband unfortunately passed away, but her daughter visits her fortnightly. Joy has had several strokes, which have had an impact on both her physical and cognitive abilities. She also has vascular dementia. Joy could be described as being fairly typical of the residents of Hebble House in terms of her physical abilities. However, she is relatively able in terms of her cognitive abilities and is one of the few residents who recognises the researcher.
Joy was very active when she was in her 20s and 30s, and regularly went walking and potholing. When she met her husband and moved abroad, her levels of physical activity reduced, as she prioritised her education and career. Joy experienced a long and gradual decline in her physical abilities, which was exacerbated by the stroke she had in her 50s. She returned to the UK with her family as her physical abilities declined.
Joy’s transition to Hebble House occurred during a traumatic period in her life. Joy and her husband lived in supported accommodation in their 60s, where Joy lived a socially active life. Even following her diagnosis of dementia in her mid-60s, her daughter commented that she managed to retain her independence. Following her husband’s death, however, her daughter explained that her mum was increasingly struggling to live at home. Following a fall and subsequent admission to hospital, Joy was assessed and admitted to a CH. Her daughter had concerns about the care that she received at this CH, and, following a further admission to hospital, her family collected her belongings and insisted that she be moved elsewhere. Joy was given a place at Hebble House and has been living here for 4 years.
Joy is a friendly and generally jovial character; she is often heard laughing. Joy is accepting of other residents and will initiate and engage in the odd bit of conversation when she is sat in a lounge area. At certain points in the day, however, she becomes frustrated by aspects of life in the CH and states that she needs to ‘get out’. Although Joy has short-term memory problems, she and the researcher had long conversations and she tends to be aware of what is going on around her. Joy regularly sits outside the main staff office downstairs. She has very good hearing and will often comment on what she has overheard staff discussing.
Joy walks very slowly and with great effort, using a walking frame. She smokes and spends quite a large part of her day requesting staff to take her for a cigarette and then walking to and from a smoking area. It can take her between 20 and 30 minutes to walk the length of the corridor to the smoking room. In order to keep Joy as mobile as possible, and to encourage her efforts, care assistants often negotiate with her by offering to wheel her back from the smoking room in her wheelchair, if she walks there using her walking frame.
GraceGrace is one of the residents at Hebble House who is in the later stages of dementia and who has very limited physical and cognitive abilities. She has been living in the CH for several years. Over the course of the observations, no-one was seen visiting Grace and the researcher was unsure whether or not she has any family.
Grace is generally quite bubbly and regularly smiles at care staff members and the researcher. However, she has very little engagement with other residents. Grace’s physical abilities have declined since the fieldwork commenced. At the start of the observations, she walked, with great effort, using a walking frame. However, now Grace is transferred by two staff members into her wheelchair and wheeled about the CH. Care assistants have been observed discussing Grace’s declining mobility and how best to support her.
Grace spends most of her time sat in a comfortable chair in the lounge, from which she is now unable to move unless assisted. She spends her time watching care staff as they move in and out of the lounge. Grace requires significant support in terms of ADL; however, she is still able to feed herself if food is placed in her hand and she is encouraged. Grace has very little speech and regularly vocalises (repetitive, high-pitched sounds that increase in volume over time). Grace will often stop vocalising if a care staff member talks to her. Sometimes, care assistants will spend significant amounts of time sitting and talking to Grace. Other residents, however, get very frustrated with Grace’s vocalising and several will shout at her to stop. Staff often try to calm these situations by talking with Grace.
Care home names are pseudonyms.
Daily routine
Residents’ typical daily routine was structured around mealtimes. Breakfast was served at 09.00, lunch (the main meal of the day) was eaten at 13.00 and the evening meal between 16.30 and 17.00. During mealtimes, groups of four residents sat around small round tables while care assistants served the meals and assisted some to eat. There was usually some conversation between residents and also between residents and staff during mealtimes. Kitchen/dining room areas were used by residents primarily during mealtimes, although Mavis would sometimes help care assistants wash and put away dishes at the end of the meal.
With the exception of a small number of residents who walked around the CH (i.e. Julie, Evie and Emily) or occupied themselves by tidying the CH (Mavis), residents tended to spend the time between meals sitting quietly, watching television or sleeping in the lounge areas. The arrival of the tea trolley broke up the morning and afternoon. Those residents who smoked also occupied themselves by going outside or to the smoking room for a cigarette.
Generally, there was little conversation between residents. A small number of residents, however, regularly conversed with others. Ann, Joy and Mavis regularly struck up conversations with each other and with other residents, and Caroline and Jane happily engaged in lengthy conversations from time to time, although there was little shared understanding. Some of the more able residents, including Mabel, Ann and Joy, often demonstrated patience and thoughtfulness in their interactions with other residents. Residents sometimes helped others, for instance Mabel regularly fetched Evie’s forgotten walking stick. A few residents vocalised or talked to themselves, which sometimes prompted reactions from others including concern (‘are you OK?’) or disparaging comments (‘shut up’). There were times when tensions were high between residents; staff tried to manage these situations. Care assistants would also strike up conversations with residents when they were in the lounge areas. Residents enjoyed conversations with members of the care staff, which tended to be light-hearted and jovial. Care staff demonstrated good knowledge of individual residents’ histories, likes, dislikes and abilities. Many were extremely enabling in the approach they took to their interactions with residents, often encouraging them to do as much for themselves as they could.
Some residents had regular visits from relatives and friends, which were often welcomed, with some residents visibly delighted by the arrival of their visitors. Visits tended to consist of residents and visitors sitting together and talking in the lounge areas. Some visitors (who are familiar with the home) spent time talking with other residents and staff. For some residents, these visits formed a topic of conversation and they enjoyed telling others about their visitors. For others, however, they were soon forgotten.
Although activity timetables were displayed on the walls of the wings, very few of these formal activities actually took place over the course of the fieldwork. The organisation and delivery of such activities were considered to be the role of the activity co-ordinator, who was on maternity leave. When the care staff had spare time, however, they organised spontaneous activities. One member of the care staff, who used to work in a kitchen teaching adults with learning disabilities, organised baking sessions with small groups of residents during which she encouraged them to do as much as possible.
Changes at Hebble House over the course of the fieldwork
In addition to the changes detailed throughout the previous sections, over the course of the fieldwork, the physical and cognitive decline of several residents, including Ann, Mabel, Grace and Bella, was particularly apparent and difficult to witness. Other residents, such as Joy, James, Jane and Evie, however, experienced a much more gradual decline.
The routinisation of movement and physical activity in care homes
Understanding the rhythm and routine of residents’ daily life in the participating care homes: factors that sustained the pattern of daily life
This section details the interacting factors and social processes that shaped and sustained the pattern of residents’ daily life and the routinisation of movement in the CH settings. Furthermore, the opportunities for changing the routine to increase residents’ movement and physical activity are highlighted.
The ethos of care
There were different philosophies of care at the four participating CHs. These philosophies were shaped, in part, by the wider political economy of care, by the policies of the care company and by the managerial team. At Rowntree Nursing Home, Bourneville CH and Hebble House, the CH manager had a very strong influence over the ethos of care and how it was operationalised.
At Rowntree Nursing Home, the philosophy of care centred around the notion of the family and the provision of care was holistic and personally meaningful in its delivery. Rowntree Nursing Home invested significant resources in employing a broad range of professionals to support an array of activities and therapies for residents, thereby providing residents with more opportunities to participate in organised activities than the other CHs.
At Eden Park, the CH manager was largely absent over the course of the study, and the assistant manager was acting up to fill the gap left by the manager. The ethos of care was paternalistic in nature, in that the emphasis was on ‘caring for’ (doing for) residents. Although there were discussions of resident choice, residents were not often enabled to make choices or take action. They were, therefore, often constructed as passive recipients of care.
At Bourneville CH, the philosophy of care was closely aligned with the managerial and audit culture, in that the emphasis was on procedures, documentation and a task-focused approach to care delivery. There were tensions between the manager at Bourneville CH and the care staff, which was, in part, shaped by the manager’s focus on procedures and documentation.
At Hebble House, the ethos of care was constructed around enabling ‘service users’ through the provision of personally meaningful and enabling support. The CH manager, Laura, wished to foster an atmosphere of interdependency in which residents were supported to do certain everyday activities, rather than the care assistants doing such activities to or for them.
The ethos of care at each of the four CHs had implications for the care environment in relation to how care was managed, organised and delivered. Thus, it was one factor that had shaped and helped to (re)produce residents’ pattern of daily life.
Organisation, management and delivery of care
Enabling residents, managing risk or avoiding risks
The holistic and enabling philosophies of care at Rowntree Nursing Home and Hebble House fostered an atmosphere in which residents were given more opportunities to engage in certain occupations or were supported in doing certain things for themselves. These visions of care, however, raised particular challenges relating to risk and promoting residents’ abilities and autonomy. Andrew, the manager of Rowntree Nursing Home, drew attention to the difficult balance that CHs need to strike between facilitating greater personal independence among residents and maintaining their safety:
The problem is . . . if, say, residents are doing more for themselves, we say ‘Well, we’ll put a kettle in your room and you make yourself a cup of tea’, then you’ve got to think ‘well, do we need a fridge for the milk?, what if they spill the hot, boiling water on themselves?’, it’s all, sort of, that risk assessment-type sort of culture . . . ‘Oh Monica, go and make yourself a cup of tea’ and then she’s got the steps and then there’s the tea and the water and you think ‘oh, it’s not really . . .’, I don’t think there’s that many people here, some could do it physically, but not mentally, and some could do it mentally and not physically, you wouldn’t trust Edith to make a cup of tea really, would you? And she would probably have forgotten what she was doing between going from standing up and getting to the kitchen . . . It’s all the supervision, you see; so I suppose if you said to Monica ‘Right, do you fancy going and making a cup of tea together’ then she probably would do that, but you need that one-to-one attention, don’t you?
Andrew, CH Manager, Rowntree Nursing Home
The tension between enabling residents to do things for themselves and managing risk was brought to the fore in the context of these two philosophies of care. This had implications for care assistants in how they delivered care. At Hebble House, the CH manager, Laura, emphasised her desire to create an ethos of enabling residents to have greater autonomy. She attempted to encourage care assistants to enable residents when they could by highlighting examples of good practice. In her interview, however, she highlighted that the care assistants’ fear that they would be exposing residents to potential risk sometimes prevented them from allowing residents to do things for themselves:
For example, with regard to medication, there are some people when they come into Hebble House that could still administer their medication, but that’s a fear factor with the staff. They think that they can’t. But you, it’s like a simple thing, like putting a teapot on the table, but the staff won’t let them, the service user, pour the tea, ‘but they’ll burn themselves’. But they, it’s not, that’s not about a speed thing, that’s about them thinking they’re going to hurt themselves, but you’ve got to give them the chance to try. We took the service users out on Sunday for dinner and they all poured their own tea from teapots, and the staff, I said ‘see, don’t do it for them, they can do it themselves’, you know what I mean? And it, that, I think they forget in this environment, if you know what I mean?
Laura, CH Manager, Hebble House
Such tensions were less evident at Eden Park and Bourneville CHs, as the care philosophies aligned themselves with a more paternalistic and risk-averse approach to delivering care.
Surveillance, monitoring and enabling: the example of mobility
In all of the participating CHs, it was evident that care assistants monitored the movement of residents, often breaking away from undertaking other tasks to intervene in a situation if they felt it was warranted. In terms of residents moving around the homes, staff engaged in different forms of monitoring for residents with different levels of mobility and behaviours in different situations.
Those residents who were mobile, but for whom walking was effortful, and who were vulnerable to falls, were conceptualised as being ‘risky’ and their movement was closely monitored by care staff. In all four CHs, there was the very real possibility that residents would fall, injure themselves and be admitted to hospital. At Eden Park, such residents were often sat in a particular lounge where care assistants and other staff members could closely observe them while they were going about their routine tasks, to ensure that they remained seated and safe:
That lounge close to the dining room is, we’ve been told, it’s like, for people who need more attention, like, people who wander or let’s say they might have some feet, some, you know, and they are prone to some falls. They’re supposed to sit in that lounge so it’s close to, it’s in the middle so every time somebody’s passing from the laundry, the cleaners, . . . like, we can observe them all the time.
Senior carer, Eden Park CH
The following extract from Rowntree Nursing Home records an instance of a resident sustaining a fall, and an implied assumption from a care worker that the resident ought to notify staff, or ask permission, when going for a walk:
Suddenly there is a cry that someone has fallen over. I walk into the lounge and see Alison, the activity co-ordinator, talking to a prostrate resident who moans in discomfort. A care worker cradles her head in her hands, and she is gradually helped to her feet. I hear a fellow care worker say under her breath, ‘they will walk off without letting us know!’. It seems like she will be OK. I reflect upon the conflict between encouraging residents to move about their living space and remain active, and the need to remain vigilant to prevent falls.
Extract from fieldwork notes, Rowntree CH
To protect ‘risky’ residents from falls, care assistants sometimes curtailed their non-purposeful movement, by emphasising the risks involved in walking and encouraging them to remain seated:
Vaile is taking small steps toward the conservatory. He has bandages on his forehead and arms. His left eye is swollen, and fresh blood is on his ears. He sits in a chair, but after 5 minutes stands up and starts to walk toward the main lounge. He takes about 10 steps, when one of the chefs sees him and quickly comes to help him back to his chair. ‘I don’t want to see you walking’, the chef tells him, ‘It is not safe for you.’. Immediately after this, the chef leaves. Vaile stands up, walks and manages to get to the stairs. Natalie (care assistant), passing by with a trolley of files, abandons the trolley, runs to take hold of Vaile’s hand, and takes him back to his seat. Four minutes after Natalie leaves, Vaile again stands up and begins walking toward the main entrance. Ryan (senior-in-charge), coming in with a frail female resident in a wheelchair, meets Vaile en route. Unlike the other staff, he encourages Vaile to walk, but warns him to be careful. As Vaile takes a few shaky steps toward the stairs, however, Ursula (care assistant) comes running to support him, takes his hands and begins walking slowly with him. Ursula reminds Vaile he is not supposed to walk alone because he may fall again and hurt himself further.
Extract from fieldwork notes, Eden Park CH
As these extracts demonstrate, it is often the more junior staff members, who are more regularly involved in the face-to-face care work, who are risk averse with regard to the movement of residents.
Similarly, at Hebble House, several residents who struggled with their mobility were closely monitored by care assistants. When these residents stood or started to walk around the CH, care assistants enquired where they were going; if they did not have a particular purpose, care assistants would often gently, but repeatedly, suggest that they take a seat in the lounge. The following extract is from Hebble House:
Judith was wheeled in to the day centre lounge in a wheelchair. The care assistant supported Judith to stand and transfer to her comfy chair (this was done with patience and they enabled Judith to do what she could by herself). Judith and I spoke for a few minutes, she told me that she had fallen and banged her head once, which meant she had to spend time in hospital. The care assistant (who was nearby) overheard Judith and commented that she had to be careful when she was walking. (. . .) Judith appears frail and sits slightly hunched. When she walks it takes a lot of effort – she uses a [walking] frame, which – in her hands – looks very heavy. Every time she lifts the frame, she groans a little. Her feet turn inwards slightly and this means that it takes both time and effort to shuffle forward. It became apparent that care assistants keep a particular eye on Judith. Throughout the morning, Judith regularly stood up and tried to walk. When she did so, care assistants would either stay close by and offer support if necessary, or would enquire where she was going and, if she replied that she did not know (which was often the case), they would encourage her to sit back down.
At one point during the morning Judith got up and walked towards the toilet. She slowly made her way out of the lounge area and in to the corridor, but there were no care assistants around. Her walking was effortful and she seemed a little unsteady (I was a bit concerned about her falling). Once she crossed the corridor (heading towards the toilets), Judith got stuck, part of the frame was trapped against the wall and she needed to shift a little to the right in order to continue towards the toilet. She seemed unable to manoeuvre her frame to allow her to do this. A care assistant was walking down the corridor and came over to Judith; she asked her if she wanted the toilet and Judith replied that she did. The care assistant then helped Judith manoeuvre her frame and went to assist her in the toilet. I returned to the lounge. Judith and the care assistant were in the toilet for a while, during which time another care assistant enquired where Judith was. When she was informed that she was in the toilet, she anxiously asked if someone was in there assisting. When this was confirmed, she seemed relieved.
Extract from fieldwork notes, Hebble House
These extracts demonstrate how care assistants monitor, and may even attempt to curtail, the movement of residents whom they consider to be at risk of falling by requesting that residents sit down. However, the previous extract also demonstrates that care assistants at Hebble House would enable and support residents to move around the home, in particular if they were moving for a particular purpose (e.g. to go to the bathroom, to walk to the smoking room, to move between the dining room and lounge area).
Similar monitoring of residents’ movement was identified in Bourneville CH. Here, a resident, Scarlet, spent most of her time in the front lounge, usually in the same kind of approximate position. Although she used a walking stick to get about, there were many occasions when she did not use any kind of assistance, and she would move quite swiftly. During the course of observations, Scarlet had at least a couple of falls in the communal areas, one in the hallway and also in the dining area, where she somehow fell from her seat.
Scarlet’s determination and keenness to walk independently presented a difficulty for the CH regime in wishing to prevent her from falling. In the following extract, Scarlet suddenly gets up and starts walking, the deputy manager quickly comes over to monitor Scarlet, allowing her to walk, but ready to intervene if necessary:
Suddenly Scarlet lurches to her feet while I have been chatting to Beryl (a fellow resident) in the front lounge. Fearful of another fall, I follow her, ask her where she’s going and she tells me she needs the toilet, and then mistakenly enters the rear lounge, saying ‘they must have moved it since I was last here’, does an about-turn and walks through the front lounge to where the toilets are situated. Deborah (Deputy Manager) follows her, saying ‘I’m right behind you, Scarlet’, who stops to listen as Deborah continues ‘you know that voice, don’t you?’. Deborah says to me ‘it’s OK, I’ll watch her’ and accompanies Scarlet to the toilet.
Fieldwork notes from Bourneville CH
This sense of low-level monitoring was apparent to Scarlet’s husband, Norman, who, during the course of an interview, remarked on being cajoled by staff to discourage Scarlet’s movement, something that he felt deeply uncomfortable with and refused to endorse:
Scarlet is Scarlet, she is very mentally determined, I couldn’t stop her, someone in the home said would I speak to her, and, some months ago this was, said would I speak to her and say not to walk, I said ‘no, it’s not, I can’t stop her walking’, you know, she will walk, if she wants to walk, she will walk.
Norman, Scarlet’s husband, Bourneville CH
At several of the homes, it was noted that, when staff were busy, they took less time to enable residents and occasionally they would shepherd residents to and from where they were going. The sometimes very different reactions from care assistants when ‘risky’ residents moved were also noted, with some care assistants being supportive whereas others were concerned. Belinda spent much of her time seated in a wheelchair that she was incapable of steering in the communal spaces of Bourneville CH. The following extract from the observational study reflects on the response of care staff as Belinda moves from a wheelchair to a sofa chair:
A resident seated in a wheelchair (Belinda) keeps trying to stand up, and a young man who works part time in the catering department tells her to remain seated as her ‘legs can’t stand it’. A care worker wheels her to a comfy chair and tells her she’ll be more comfortable sitting there, but Belinda seems unconvinced. The care worker leaves her . . . during which time Belinda manages to stand up, turn around and be seated in the comfy chair. It is interesting to observe the response of two care workers to this incident: one of them says positively ‘see Belinda, you can do it’, which seems to be an approbation of her physical independence, whereas the other care worker, who had intended to help Belinda into the comfy chair, looks slightly aghast, perhaps fearful that Belinda may have fallen and injured herself.
Extract from fieldwork notes, Bourneville CH
At Hebble House, in particular, the care assistants took great effort to enable residents to do as much as they could with regard to mobilising for a particular purpose. On several occasions, the care assistants at Hebble House engaged in discussions about particular residents’ mobility if they noted a change (both in terms of an improvement or decline in mobility):
Shortly afterwards, Denise (care assistant) and Molly (care assistant) brought Grace (a resident) into the lounge area in her wheelchair. Both of them supported Grace to stand and transfer into her usual comfy seat; while they did so, they verbally guided and encouraged her. Afterwards, they commented on Grace’s changing mobility. They noted that she now takes very little of her own weight when she was being transferred. Grace has needed support with her mobility since I commenced my fieldwork, but, in July, she was able to walk a short distance using a [walking] frame with support and encouragement. Over the past 4 months or so, however, Grace’s mobility has declined and she appears unable to support her own weight for more than a few seconds. The care assistants have continued to encourage and support her.
Extract from fieldwork notes, Hebble House
Such changes in mobility would be reported and an expert would be brought in to assess residents’ mobility needs. This meant that the residents at this CH had aids and support that were appropriate for their level of mobility. Care assistants implemented the recommendations, but would also seek a re-assessment if they felt that there had been further changes or if they felt that the recommendation was not appropriate.
In addition to the ‘risky’ residents, who were vulnerable because of their fragile mobility and the risk of falls, there was a group of residents at Hebble House who would resist mobilising and who would prefer to remain sedentary. These ‘sedentary’ residents often had mobility problems and found walking so difficult, wearisome or even frightening that they were reluctant to walk. Their lack of movement caused care assistants concern with regard to maintaining the little mobility they had. Care assistants would, therefore, encourage, negotiate and sometimes physically support these residents to mobilise. For instance, Joy struggled with her knee joints and found it painful and exhausting to walk. She had both a walking frame and a wheelchair. Joy smoked and would go to the smoking room, which was situated at the end of a long corridor, several times during the day. Care assistants were keen to maintain the muscle and mobility Joy had, so they would negotiate that, if she walked to the smoking room, they would wheel her back in the wheelchair. It would take Joy 20–30 minutes to walk to the end of the corridor; to support Joy, the manager had placed a ‘pit-stop’ chair along the way so that she could pause and rest. Staff members would verbally encourage Joy as she walked along.
Frank was particularly reticent to walk. He used a walking frame, but his walking was laboured and slow. He preferred to sit in the lounge, rather than walk any distance:
While I was sat in the front lounge, Frank emerged from the toilets adjacent to the lounge. Over the course of 10 to 15 minutes, I observed three different care assistants encouraging Frank to walk back from the bathroom to his chair in the lounge (a distance of approximately 3 m). Frank struggles with his mobility – he walks using a [walking] frame, extremely slowly. He often seems reluctant to walk and care assistants can often be heard negotiating with him to get him to walk. Today, between them, they invested quite a bit of time (verbally encouraging, pointing out directions, showing him to his chair, ensuring that his path was clear of other people, etc.) to encourage and enable him to walk to his chair. When he arrived, one care assistant praised him for walking.
Fieldwork notes from Hebble House
Not all residents, however, were monitored so closely. Across all the CHs, those who were deemed physically able to walk (i.e. they were thought to be stable on their feet and at lower risk of falls) were not monitored in the same way. At Eden Park CH, a group of seven residents were relatively able and some were allowed to leave the CH independently. This group of residents would also spend time in the garden and move about the CH as they wished.
At Hebble House, residents did not leave the CH setting unsupported. However, those who were more mobile were allowed to walk around the CH, sometimes for long periods of time. For instance, Evie (a resident who walks with a stick and is independently mobile) can often be found walking along the long corridor on the upper floor of the home. Care assistants allow Evie to walk along the corridors and only tend to suggest that she sits down in a lounge when she becomes out of breath and mentions that she is tired.
However, there were exceptions: some residents who were able to mobilise independently were monitored closely by care staff and even, on occasions, their movements were curtailed. At Hebble House, all residents had a diagnosis of dementia, the staff were well trained and had a good understanding of the complex behaviours that are associated with the middle and later stages of dementia. Generally, these complex behaviours were appropriately and sensitively handled by care staff. There were some residents who were physically mobile, but who, because of their memory problems, would quickly become disorientated and distressed if they left the familiar space of their lounge areas. If these residents left the lounge area, care assistants would enquire where they were going; if they replied that they did not know, care assistants would often encourage them to sit down in the lounge areas. For instance, Lesley is independently mobile, but she has impaired vision as well as memory problems. Although she is able to navigate from the lounge to the dining room with verbal guidance, if she left the lounge without support, she would become disorientated very quickly and could become distressed. Care assistants would, therefore, encourage her and guide her back to the lounge, where she would usually settle.
At Eden Park CH, there were several residents who were closely monitored with regard to behaviours that staff considered challenging. Kaylee and Nora were both physically able, but would regularly try to leave the CH to return home. They were often seated in a particular lounge to allow care assistants to keep a particular eye on them and monitor their movements to ensure that they did not leave the CH:
The lounge between the dining room is for the residents who are likely to fall or get lost in the building. Kaylee and Nora are always looking for a chance to leave the building. If they are seated in that lounge, then we know that they are safe and everybody can see them.
Assistant manager, Eden Park CH
Russell was also often seated in this lounge area and closely monitored by care assistants. He would sometimes become aggressive towards other residents and cause them distress. Over the course of the fieldwork, care staff took measures to monitor and even curtail his movement around the home to ensure that he did not cause himself or other residents harm. At times, care staff placed a specially designed wooden trolley in front of him to restrict his movement while he was seated in the lounge, and served his meals in his bedroom rather than the dining room. This restriction of the movement of a particular resident, however, was extremely unusual.
Although the majority of residents had a largely sedentary lifestyle, even those who struggled to mobilise were supported and enabled to move, especially if they had a purpose for their movement. At all homes, those who were unable to mobilise and who were dependent on care assistants to hoist them would often spend the time between meals sat without being mobilised. Although sometimes enabled to participate in ad hoc activities at Hebble House and engaged in conversation, the physical movement of this group of residents was extremely limited and not consistently enabled in any of the CHs.
Organisational need for routine
Across all of the CHs, the organisation of the day-to-day running of the home was largely structured around bed and body work, mealtimes and medications. As is the case in many organisations, there is a requirement for some kind of routine to ensure that the institution functions and achieves its purpose. Within this organisational routine, however, care could be delivered in a flexible, resident-focused manner or in a task-focused manner.
In an interview with Laura, the CH manager of Hebble House, she articulated the tension between running the organisation, allowing the provision of necessary care, and the desire to be flexible to ensure that residents have some choice over their routine:
[Residents] their daily routine and, kind of, the activities they kind of do? Could you just tell me a little bit about that?
Daily routine. You try not, it’s hard within a residential unit because there has to be some kind of routine because the cook’s here for only various times. The care staff have certain things to do at certain times as well, so although you try not to make it establishment orientated, there is a routine because you can’t go through all day having breakfast or a cook cooking all day, it’s impossible, you can’t, you know. So really basically the service users get up when they want, that’s their choice. (. . .). We try to end breakfast about 10 o’clock because otherwise they won’t, there has to be a period where they’re not eating, otherwise they’re not going to eat their lunch. Also there’s the problem with tablets as well. We can only give out tablets within a time frame that’s quite tight on the way it’s prescribed, so we have to think right, if somebody’s having breakfast, then breakfast is between 8 and 10, lunch is between 1 and 2, tea’s between half 4 and normally runs to about 6 o’clock. (. . .). It’s their home so it’s not rigid as in ‘you’ve got to be up, you’ve got to go to bed’, but there are time frames when certain things do happen, yeah.
The different care philosophies of the CHs certainly influenced whether, and in what circumstances, care was delivered in a flexible, resident-focused or task-focused manner. Other factors, however, including the prioritisation of tasks, care staff’s knowledge of residents as individuals, and how care assistants perceived their role, had implications for the manner in which care was delivered. There were examples of both resident-focused and task-focused instances of care delivery at all CHs.
The following extract from ethnographic notes centres on the interaction between Geraldine, a wheelchair-using resident who required the use of a hoist, and care assistants immediately prior to lunchtime and highlights the prioritisation of the routine above the requests of a resident:
Geraldine asks if she can go to the toilet, pointing out that ‘they usually fit me in’ before lunchtime. The carer asks if she can hang on (it’s now 12 p.m.), but she says that she needs to go. Two care workers are fetched, and she is hoisted from her armchair into a wheelchair. ‘Oh it’s busy in there’ she says, gesturing to the carers preparing for lunch, as she lands in the wheelchair, and they agree. She is wheeled to the toilet. Here, the routine preparation for lunchtime seems to supersede the need to attend to someone’s toileting needs, and the attempt to ensure the toileting process fits in with mealtime routines. There is no sense of reassurance that Geraldine can go to the toilet whenever she wishes, and she is clearly aware of and acknowledges this, and understands that her behaviour needs to fit in with the prevailing routines.
Extract from fieldwork notes, Bourneville CH
An approach that prioritises the routine over the resident(s) was, on occasions, reinforced and (re)produced by senior care staff:
Sheba’s son has come to visit his mother, who is sitting with Mandy and Mariel. They are reading the newspapers and discussing the queen’s speech and recent changes in pensions. Emma and Ascon, who have just woken up from a long nap, see a bird on the windowsill. Emma enthusiastically exclaims, ‘It must be summer, right? Look at the window. Those are the birds of Africa. They have come to build their nests. That is how we know it is summer. When I was growing up, we knew it was summer when we saw the birds of Africa. They cross the Atlantic to come and built their nests here and go back to Africa in the winter.’. This topic is well received by the five other residents nearby, who eagerly join in the discussion. Many tell about their own experiences when they were young, and how they, too, couldn’t wait until they saw the birds of Africa arrive as harbingers of summer.
As the discussion of the arrival of the birds from Africa is going on, a care assistant comes to get residents ready to go to the dining room. But, unusually, this discussion about the birds of Africa has evoked such memories that the residents don’t want to leave. After listening to their discussion, the care assistant joins in. Shortly after, Dylan (senior-in-charge) comes into the lounge and asks the residents to go to the dining room. He is not happy with the care assistant for failing to get them there. ‘They should be seated by now’, he says, clearly annoyed. His impatience breaks the mood. Sheba’s son hugs her, says goodbye to her and the other residents, and leaves.
Extract from fieldwork notes, Eden Park CH
On this occasion, Dylan, a senior care assistant, who often demonstrated a resident-focused approach in his interactions with residents, prioritised the routine of the CH when certain tasks, in this case feeding residents, needed to be accomplished. This may have had implications for how the care assistant conducted her role in future.
Knowing individual residents, including their likes, dislikes, abilities and impairments, as well as having knowledge of their past and social connections, often facilitated care staff in delivering care in a more resident-focused manner.
The following extract details a mealtime at Rowntree Nursing Home. In this example, the care assistants demonstrate little knowledge about or interest in the residents and they feed the residents in a perfunctory manner. Their focus is on getting the job done:
Dora (resident) raises her hand and tells me that she needs a nurse, and so I find a care worker with whom she can speak. It appears that her main need is for pain relief. The care worker says she will be put to bed after lunch. She then spoon-feeds Judie her meal, and delivers a meal to Dora, who can feed herself. Another care assistant feeds Ada. Violet becomes a bit anxious for her meal, slapping her hand against the table in front of her, and then striking her cup against it. ‘Don’t do that please’ says the care worker. The feeding that takes place is done in a perfunctory manner, and I reflect upon the lack of communication here between resident and carer.
Extract from fieldwork notes, Rowntree Nursing Home
The following extract also details a mealtime at Rowntree Nursing Home. Tracey, a care assistant, demonstrates in-depth knowledge about Albert, a resident whom she is feeding, which enables her to accomplish the job of feeding Albert. She also takes the opportunity to learn more about Albert and another resident, Monica:
There is some verbal jousting between Albert and a care worker, Tracey, who feeds him. She says ‘that cricket could be (substituted for) knitting you know, with all the carrots’ and Albert laughs, picking up on his known dislike of carrots and knitting and his enjoyment of cricket. Tracey asks Albert various questions, mainly about the cricket (on television), such as ‘who’s playing? I thought it was India versus Pakistan? Did you play cricket as a lad? Were you a bowler?’ and Albert replies as best he can, usually with a short answer. ‘Did you like sport?’ she asks Monica, who replies ‘no, I hate it, I was never any good at it.’. A carer asks Tracey if she likes darts, and she replies ‘yes I do, I whack it at the board and see what happens’, and she and Albert laugh. She adds ‘I tend to play better after a few wines’, and the residents are amused.
Tracey asks Monica how she relaxes, and she says she doesn’t know, before adding that she likes reading newspapers. Tracey suggests that she might read the paper for half an hour or so if she needs to relax, and Monica says that’s a good idea. The atmosphere has become very convivial now. Tracey asks Albert if he has any brothers and sisters, and he says he hasn’t and she replies ‘good job, isn’t it, one Albert is enough’ and they both laugh.
Extract from fieldwork notes, Rowntree Nursing Home
In the above extract, Tracey utilised her knowledge of Albert’s hobbies, his likes and his dislikes to deliver resident-focused care. Staff-inspired banter often focused on residents’ personal idiosyncrasies, likes and dislikes to telling effect, and on these occasions residents seemed to enjoy a sense of their identities being recognised and valued.
In the following extract, Rosa, a care assistant at Hebble House, also draws on her knowledge of Elizabeth. In this case, however, Elizabeth is able to eat and drink with support. Rosa uses her knowledge of Elizabeth’s abilities and vulnerabilities to enable her to drink her cup of tea. This is done with patience and encouragement:
At approximately 2.30 p.m., Rosa, a care assistant, pushed the tea trolley into the lounge. She paused, took the lids off each of the plastic teapots to figure out which was tea and which was coffee. She served tea or coffee to each resident, asking them what they wanted to drink and chatting. When Rosa gave Elizabeth a cup of tea, she paused and quietly waited, observing, as Elizabeth attempted to drink. Elizabeth, very slowly and carefully, but slightly jerkily, lifted the cup towards her lips. As she lifted the cup, she began to tip the cup slightly to one side, so the tea was in danger of spilling. Rosa gently prompted Elizabeth to be careful, and then when Elizabeth did not manage to steady the cup, she intercepted before Elizabeth spilt the tea. Instead of taking the cup from Elizabeth, however, she placed her hands over Elizabeth’s, steadied the cup, and then gently guided the teacup to Elizabeth’s lips. Once Elisabeth had taken a mouthful or two, Rosa helped her to place the teacup on the table beside Elizabeth’s chair. Rosa then suggested to Elizabeth that may want to leave it to cool for a while, as it was quite hot. Rosa then distributed the biscuits and, as she did so, she chatted with the residents about the biscuit selection.
Extract from fieldwork notes, Hebble House CH
Perceptions of the role of the care assistant: engaging residents in activities, interaction and occupation
Across all four CHs, care assistants were kept busy attending to the physical needs of residents, including those who were nearing the end of life, and keeping up to date with their paperwork. Thus, conversing with and engaging residents in activities was seen by many care assistants as an aspect of their role that they were able to deliver only if they were on top of their ‘jobs’. Although some care assistants viewed such work as an important part of their role and attempted to undertake such activities when they could, there were also care assistants who indicated that such activities were not part of their remit at all.
In general, it was considered to be the role of the activity co-ordinator to occupy residents’ time. This led to situations in both Rowntree Nursing Home and Bourneville CH, both of which employed an activity co-ordinator, when, in the absence of the activity co-ordinators, regular care staff displayed indifference to delivering such activities for the benefit of residents.
The following extract is taken from Rowntree Nursing Home on an occasion when a game of skittles was to be delivered for residents on a day when Alison, the activities co-ordinator, was absent:
Anita leans toward Susanna, a fellow resident, and says ‘we’ll be playing skittles soon, that’ll cheer you up’ and smiles broadly. Eleanor, the nurse, walks in wheeling a trolley and says to me ‘it looks like we won’t be playing skittles after all’. Kim, a female Filipino care worker enters the room from a separate entrance and Eleanor has a quiet word with her . . .. Kim is adamant that there will be no skittles today, as she shakes her head determinedly, clutching a box of biscuits.
Eleanor, the nurse, says in a loud voice to Kim that Alison, the activities co-ordinator, will be asking if we played skittles whilst she was away. It appears as if she is applying subtle pressure upon Kim to organise a game of skittles, particularly given her greater seniority of position within the CH. However, within an instant, she backs down and mumbles something about the playing of skittles not being part of the carer’s cultural background, and with that the game is abandoned.
Fieldwork extract from Rowntree Nursing Home
Similarly, during the course of an interview, the activity co-ordinator at Bourneville CH, Vanessa, lamented the fact that carers were generally not more supportive of her work, and recalled an occasion when an entertainer performed for residents on a weekend afternoon. Vanessa visited Bourneville CH during the afternoon to see the performance, and was disappointed to find that none of the care staff had joined in with singing and physical movements to ‘chivvy them along’ in waving their arms and offering encouragement. She further recalled the entertainer expressing dismay, and commenting to Vanessa that ‘it’s a good job you arrived (to join in), as otherwise nobody would have joined in’. Expressing exasperation, Vanessa commented that ‘they don’t see that that’s part of their role, even though they’ve been told that it is’.
There were some care assistants, however, who incorporated activities with residents into their daily routine. At Hebble House, in particular, several care assistants would engage residents in spontaneous, ad hoc activities, such as singing, quizzes and encouraging residents to dance and move to music. One care assistant, who used to work in a kitchen supporting adults with learning disabilities, occasionally organised baking sessions with a small group of residents, during which she encouraged them to do as much as possible. Intermittently, these ad hoc activities were initiated by the residents themselves, in particular singing and dancing, and care assistants would join in. Regularly, care assistants would sit in the lounge areas writing up their notes while talking to residents. Unfortunately, care assistants were often pulled away from interacting with residents to undertake specific tasks.
Towards the end of fieldwork, care assistants working in one of the wings at Hebble House held a meeting with residents to discuss what activities they wished to do. Those who were able to engage in the conversation did identify some activities, for instance Caroline discussed making jewellery and going out for a pub meal with one of the care assistants, while Mabel talked about craft activities and painting. The CH manager had given the wing a small budget and the care assistants were planning to use this to buy the necessary equipment. Shortly before Christmas, the CH manager and some other care assistants took Caroline and several other residents out for a pub meal. This discussion of activities was enabled by a supportive CH manager and a particularly committed group of care assistants, one of whom knew the residents well and felt that her ‘ladies’ were not particularly interested in taking part in the organised exercise class.
Barriers to and opportunities for enhancing movement
-
The ethos of care shaped opportunities for occupation, activity and movement. If the CH adopted a more enabling or holistic care philosophy, this often resulted in greater opportunities for residents to move.
-
The tension between risk management and the promotion of independence, and how this was managed at an organisational level and at the point of care delivery, had implications for residents’ daily routine.
-
Whether a resident-focused or task-focused approach to the delivery of care was facilitated and encouraged. In particular, how care assistants went about monitoring, curtailing and enabling residents’ movement.
-
Whether or not care staff perceived their role to include spending time engaging with residents socially and in activities.
Individual environment
Resident profile
The physical and cognitive abilities of the residents were very varied (within and between the four homes), but most required significant support with ADL. This section explores various factors relating to residents’ subjective experiences that shaped the rhythm and routine of daily living in the CHs, including residents’ transition to the CH and adjustment to daily life, and the subjective meaning of the CH for residents.
Transition to the care home
Residents’ trajectories to the homes differed, but generally fitted one of two patterns. The first trajectory was typified by older people experiencing a slow and gradual decline in their physical and cognitive abilities over time, which meant that they required increasing support that eventually led to their admission to residential care. Such a transition often involved moving from their home, or some other form of supported accommodation, where they tended to live alone. The second trajectory involved older people suddenly experiencing a decline in their physical and/or cognitive abilities, often due to a crisis event and admission to hospital, followed by a move to residential care.
Admission to a CH setting was generally unsettling and sometimes traumatic for older people. This was particularly the case if their transition seemed sudden to them, and if they had a strong attachment, which many did, to their home.
For some residents, however, the move into the CH was considered, in general, to be a positive move. This was usually the case if they had had time to accept that they required increased levels of support, and if they felt a connection with staff and/or fellow residents. For Katie’s daughter, Cerys, moving into Rowntree Nursing Home represented a realisation for her mother that living without constant care and support was no longer feasible, given worsening health and well-being, brought about by arthritis, chronic asthma and a spinal injury resulting from a fall:
At home, she had carers at home for quite a while but that didn’t really work out . . ., they did their best but didn’t really help her so we used to go every day, but she got to the point where she just . . . she always said ‘I never ever want to go into a nursing home’ and we said ‘well, we’d never, we’ll never do that’, but she decided, she says ‘I realise that I can’t manage so I’m going to have to go into a nursing home’ and she came up here and chose this one and never looked back really, she loves it.
Cerys, Katie’s daughter, Rowntree Nursing Home
A key element in helping her mother’s adjustment to living in Rowntree Nursing Home was the encouraging attitude of care staff, and the humour that arose from Katie’s interaction with them. The personal nature of these interactions, rooted in Katie’s personal idiosyncrasies and habits/dislikes seems of vital importance here:
She came for a week respite and when she came out of hospital, obviously she’d seen what it was like and she decided this was where she wanted to be . . . I mean she’s actually said to us ‘I love it here’, which is nice for us, you know . . . she likes the staff and she’s got a bit of . . . rapport with the staff, you know, where she can have a laugh with them.
Cerys, Katie’s daughter, Rowntree Nursing Home
A few residents, such as Frances at Rowntree Nursing Home, relished the change in environment. According to Frances’ daughters, their mother had become isolated at her previous accommodation and they noticed a positive change in her behaviour when she moved to Rowntree Nursing Home:
I think, where she had been living, she was feeling increasingly isolated, it was retirement apartments, so they were all elderly-ish people but fairly well-to-do and . . . in the main, not with dementia, and I think they didn’t really like her being there when she started to show signs of her dementia and . . . she felt sort of rejected by them and was uncomfortable mixing with them. We . . . told her she was coming for a break, we had to, we couldn’t say, you know, we’re going to put you in a home (. . .).
Jody, Frances’ daughters Rowntree Nursing Home
I mean, she spent the first few days saying, ‘When am I going home?’ . . . And that was very difficult for us, but she stopped very quickly and one of the first things I noticed was her finding her way around so quickly, she couldn’t find her way anywhere at home, could she? She just sat in that chair and we’d found she’d got to the point where she wasn’t going to bed at night ‘cause she couldn’t get dressed or undressed, she was just sitting in her chair. Terrible, but when she was here, she started whizzing about [laughs] and she didn’t get lost, she knew her way back to her room, it was, the difference was massive . . . I think she’d lost all confidence where she lived before.
Glenda, Frances’ daughters Rowntree Nursing Home
Over time, even those residents who found the transition to the CH traumatic adapted to the CH setting and settled into the daily routine. There was a sense of realisation that being at home and looking after oneself was not really feasible. Hermione, a resident at Bourneville CH, was visually impaired and had impaired hearing. Having sustained a broken hip and spent time in hospital, the decision to enter residential care was taken by her son, Matthew, and wider family based on her inability to undertake tasks of daily living. An interview with Matthew shed light on these issues:
So what was it like for your mum then, moving in here?
Like I say, initially, it was something new for her, and she still mentioned about, you know, ‘my little flat’ and things like that, but once she’d sort of got into it, and on one occasion we had again to take her to [hospital] for a few days, I think she’d got a chest infection . . . and the first thing she said when we got there was, ‘I want to go back home to the Bourneville CH’, and she was like that again the other night . . . when I told you she’d been in hospital while 7 o’clock, ‘I want to go back to the Bourneville CH’.
At Hebble House, however, a number of residents had little awareness that they were living in a CH setting or did not understand the reasons for their residency:
I headed back towards the front upstairs lounge. Lesley had almost made it to her seat in the front lounge, but she looked a little hesitant. She asked ‘where am I?’ and explained that she keeps forgetting. She sat down in the lounge. Lesley repeated her question, and I enquired further to decipher what she meant. She asked me if she was in a CH. I explained she was at Hebble House CH and we chatted briefly about it. She thanked me for letting her know (. . .). A few minutes later, Molly, a care assistant, came into the room, and Lesley asked again where she was. Molly sat with Lesley and they talked. Molly explained where Lesley was. She then went on to add that she had worked here for 5 years and that Lesley had lived there when she started. The conversation was warm and friendly, and Lesley appeared to be comforted by Molly’s conversation and reassurance. Molly settled Lesley and then leaned over and gave her a peck on the forehead. Lesley sat back in her seat, seemingly reassured by her interaction with Molly. Molly left to continue to support residents from the dining area to the lounge.
Extract from fieldwork notes, Hebble House
Several continued to talk of going ‘home’. For several, their inability to go home was a source of deep distress. Staff members were often extremely empathetic and would spend time explaining where they were and why they were living in a CH. The topic of home was especially important for those who had recently moved to the CH; for instance, Julie often spent her days walking between lounges and regularly spoke of going home. The following extract illustrates a regular occurrence, when Julie would gather her belonging and wait to go home:
Julie was walking from the wing where her bedroom is located towards the front lounge – she had her long, brown woollen coat on and her hands were full of belongings (including her bag, her pink dressing gown, her slippers and a box of what looked like medical gloves). I greeted Julie, and she told me she was going home. She went to stand by the front door of the CH, which is locked by a keypad. I stood next to her at the door and we chatted. She told me that she was going home, that she had had enough, that she was waiting for the bus. She asked me when the bus would come, and I replied that I did not know. She repeatedly told me that she was going home, waiting for the bus, that she had had enough here. (. . .) After a while, we went to sit in the front lounge. Julie was still waiting for the bus, so we sat together. Paula (care assistant) came into the lounge pushing a hoist. She saw Julie, with her coat and belongings, and asked her if she was going to take her coat off. Julie replied that she was going home. Paula quite sternly told her that she was staying here for now, so she can take her belongings back to her room. Julie pulled a face and Paula repeated her request. Julie stood up, glanced at me and went down the corridor towards her room.
Extract from fieldwork notes, Hebble House
A few long-term residents of Hebble House also spoke of home. Victoria would regularly say that she needed to leave to go home as her parents would be wondering where she was. Ann, who on her good days was aware that she lived in a CH, also spoke about her home and joked about possible ways she could escape. Talk of home and going home increased in intensity with the growth in the number of short-stay residents.
By contrast, a small number of residents at Eden Park CH had chosen to move into the CH from the nearby flats; this decision had been based on a range of factors, including the CH’s promotional brochure. Despite their choice, however, many of these residents felt disappointed by the realities of CH life.
Meanings given to the care home setting
To understand daily life in the CH settings, it is important to understand the meanings residents attribute to the setting and how this shapes their routine and movement around the CH.
As noted previously, across all of the homes, residents spent a lot of time in the lounge areas of the home. For some, the lounge areas were important, familiar places that were an integral part of their daily routine. Residents routinely sat in the same lounge and often in the same chair. This familiarity and ability to actively create their own space in the CH was important for many residents. At Eden Park CH, five chairs were available in one particular lounge, which led to tension between residents, as demonstrated in the following extract:
On one occasion, Mandy — a female resident with a defined seat — went to the toilet leaving her bag, sweater and makeup on the seat to make sure nobody else took it. Nora, another female resident who had been wandering around, quickly came over, put Mandy’s belongings on the coffee table, and sat down. At that, Mariel, Mandy’s close friend who generally sat next to her, stood up and adamantly demanded that Nora move. But while they were arguing, another female resident, Kaylee, who happened to be wandering by, came over and claimed Mariel’s seat. Not realising that Kaylee had sat on her seat, Mariel sat down without looking and ended up sitting on Kaylee. By then Mandy had returned and an argument ensued, which was only resolved when the chef, manager and care assistant emerged to settle the differences. Such episodes occur on a daily basis, since, as one care assistant observed: ‘They all want to sit in this lounge . . . but there is no space for extra chairs.’.
Extract from fieldwork notes, Eden Park CH
Some residents struggled to establish such a sense of belonging in the CH setting, which was often exacerbated by memory problems. This was particularly apparent at Hebble House, as several residents were unaware that they were living in a CH and were often unable to orientate themselves within the setting.
Residents attributed different meanings to the CH settings, which shaped how they occupy themselves and move around the home. For instance, at Hebble House, those with moderate and later-stage dementia may not recognise that they are living in a CH. The meanings ascribed to the CH space vary and shift. For instance, Polly considers it to be her own, private home; Jane sometimes views the lounge as the waiting room at the doctors’ surgery; and Mavis often considers the CH to be her work place and, at other times, her own home.
Barriers to and opportunities for enhancing movement
-
The transition of residents to the CH setting, their expectations of the CH and how they were supported to adapt to living in the CH setting shaped their routine.
-
The subjective meanings residents attributed to the setting shaped how they occupied themselves and moved around the CH.
Physical environment
Built environment
All four CHs comprised buildings with multiple floors and an outside space. They all had a similar combination of spaces tailored for the use of residents, including bedrooms, lounges and kitchen/dining areas. At Rowntree Nursing Home and Hebble House, the built environment was organised in such a way that each floor of the homes had a combination of residents’ bedrooms, lounges and kitchen/dining areas. This meant that residents who were able, but struggled, to walk were more likely to be able to access the different spaces on their own or with limited support from staff. They were unlikely, however, to be encouraged or enabled to routinely move between floors. Conversely, at Eden Park CH, the kitchen/dining rooms were located on the ground floor and, at Bourneville CH, the lounge spaces were located on the ground floor. This meant that those residents who had a bedroom located on the upper levels routinely moved between floors. The degree to which residents who struggled to walk were enabled to mobilise with support from staff or were wheeled in a wheelchair varied.
Physical barriers to accessing areas of the care home settings
Across the CHs, there were various physical barriers that restricted residents’ movement around the homes, including heavy fire doors; locked doors; insufficient lighting; and small spaces, within which residents found it difficult to manoeuvre. Bourneville CH seemed particularly problematic in terms of barriers. Bourneville CH is an old building that had been adapted for use as a CH. The physical structure, with its darker hall spaces, fire doors and narrower corridors, did not encourage physical movement and created hazards for residents. The following extract is taken from a conversation with Scarlet, a resident who walked around the CH using a walking stick:
I sit beside Scarlet again. She tells me that she suffered a fall soon before I had arrived this morning. She is still shaken, and I commiserate with her. When I ask her how it occurred, she tells me that she was walking from her room, on the ground floor, to the lounge. The route she took meant having to walk across a hall and then open a couple of fire doors. As we talk, it becomes clear that the difficulty of opening a fire door, which has heavy leverage that pulls the door shut after it has been pulled open, combined with having to use a stick while walking, created an additional falls hazard. She also draws attention to the darkness of the lounge, and I reflect upon the way in which this reduces the confidence of residents to move about their living space.
Extract from fieldwork notes, Bourneville CH
All of the CHs had external gardens, which residents sometimes spent time in during periods of warmer weather. Mostly, residents sat and chatted while in the gardens. However, at Eden Park CH, two of the residents enjoyed gardening. Accessing the outside areas could be difficult, however, and often required assistance and encouragement. During the summer fete at Bourneville CH, one resident, Beryl, who often sat beside another, Cordelia, struggled to pass through a doorway, and would later refer to this incident, so it had a lasting impact on entrenching her reluctance to go outdoors:
Beryl sits in her usual seat next to Cordelia, whose daughter encourages her to go outdoors. We then encourage Beryl to do the same, but she is reluctant to do so, making a joke of it and saying ‘I’m lazy’. We continue to ask her, and eventually she agrees, getting to her feet and using her [walking] frame to get to the rear of the building, where there is a ramp that leads down to a wooden table with chairs. To have reached the ramp, Beryl would have travelled a distance of approximately 12 m. She walks relatively briskly and not hesitating, as I might have imagined. As we reach the ramp, Cordelia’s daughter and I on either side of her, it becomes clear that [the] width of the ramp is narrower than the width of the [walking] frame. This is quite surprising, as the nature of this kind of structural impediment to exiting the building has not been apparent in Bourneville CH. Beryl is loath to proceed, but eventually Cordelia’s daughter and I manage to coax her over the threshold, so that she is eventually seated beside Cordelia.
Extract from fieldwork notes, Bourneville CH
Use of space
Residents conducted the majority of their lives in semipublic spaces. In the CHs, the most used spaces (from the resident perspective) were the lounge areas, where the majority of residents would spend the majority of their days, often sitting quietly, resting, reading or watching television. Lounges were familiar to residents and were where staff usually encouraged them to settle between mealtimes. Dining room/kitchen areas were used by residents during mealtimes, but very rarely in between meals. Although lounges and dining areas were familiar spaces, they were also communal spaces, and so were subject to shared expectations of behaviour. Care assistants had expectations of how residents would conduct themselves in a semipublic lounge area. Furthermore, across all the CHs, we observed tensions between residents using these semipublic spaces, which was often associated with a perceived transgression of these social rules:
I entered the front, upstairs lounge. There were six residents sat in this lounge today (Frank, William, Evie, Jessica, James and Lesley). Grace, who often sits in this lounge, was sat in the smaller, adjacent lounge. Grace is no longer able to speak, but she sometimes vocalises. Today she was sat and vocalising quite loudly. This was clearly audible in the front lounge. (. . .). Lesley loudly shouted at Grace to shut up (. . .). Lesley requested a cup of coffee (there were no care assistants around). Lesley, who has poor eyesight, suddenly stood up and felt her way to the entrance of the lounge. She started banging, loudly on the door, she did this several times. Lesley often bangs on the door if she wants to attract the attention of the care assistants. She comments that they should have tea and biscuits, that they get nothing, and that they pay for tea and biscuits. Grace’s vocalisations are audible and this time both Lesley and Evie shout at her, telling her to shut up. Evie then looks at me, sheepishly, and giggles. Lesley looks cross. Lesley bangs the door again and James shouts at her, ‘we’ve heard you’. Sarita (a care assistant) who was heading towards the lounge speaks to Lesley, she reassures her that someone will be bringing her a cuppa in a few minutes. When she leaves Lesley bangs the door again, and this time Evie tells her to shut up. Just then, Rosa appeared with the tea trolley.
Extract from fieldwork notes, Hebble House
In the preceding extract, both Grace and Lesley are reprimanded by others for transgressing what is considered to be acceptable behaviour in these semipublic spaces. The other residents who regularly sat in this lounge with Grace often chastised her when she vocalised. On such occasions, care assistants who overheard would try to ease the tension by explaining to residents that Grace could not help vocalising and they would also spend time speaking to Grace, which often stopped her from loudly vocalising.
At Hebble House, only a small number of residents spent time in their rooms, as this was generally discouraged by staff, unless residents were feeling poorly or are very ill. At Rowntree Nursing Home, Eden Park CH and Bourneville CH, a significant number of residents spent time in their own bedroom, including some residents who were relatively able.
Although the bedroom areas could be considered private spaces, care staff also had access to bedrooms and, on occasions, residents also accessed other people’s bedrooms. For some residents, however, the relative privacy of their bedroom and the fact that they were able to make it ‘their’ space encouraged them to spend time in their own room.
The following example details an occasion when Rose, a resident at Eden Park CH who usually stayed in her bedroom, was brought into a communal space. Irene, the senior-in-charge, explained to the researcher that Rose preferred to stay in her room. When Rose became distressed, saying she wanted to go home, Irene took Rose back to her room. On this occasion, therefore, Irene interprets Rose’s distress as a sign that she wanted to be taken back to her bedroom, which perhaps reinforced Rose’s desire to spend time in her room:
Rose is seated and eating alone in the conservatory. Irene (senior-in-charge) tells me that this resident has been at the CH for 2 years. I have not seen her in the public lounges since this study began. Irene tells me that her name is Rose and she hardly uses public lounges because she is scared to look at people. Rose is in a wheelchair, and well dressed. She is slowly eating her food when suddenly she stops and starts calling for help ‘I need to go home. I want my cat’. Irene explains to me that she thinks Rose wants to go back to her room as she does not want to mix with other residents. As she is shouting, Nora and Kaylee walk from their lounge and stand directly in front of her trying to console her. This seems to aggravate her as she struggled to get out of the chair. Irene transfers her in the wheelchair and wheels her to her room.
Shortly, Irene comes back and explains to me that Rose prefers her room because she has a computer with a collection of all the photos of the places she visited, her children, grandchildren and friends, all that come in a form of a documentary. So she replays it over and over again and she never gets bored.
Extract from fieldwork notes, Eden Park CH
It is important to note that we have limited information about those residents who chose to stay in their bedrooms, as our observations were conducted in the communal areas of the CHs.
Care staff, therefore, do shape and influence residents’ use of space. Sometimes care assistants control residents’ use of space. This is particularly the case for those residents who are dependent on staff to move around the CH and in those CHs where the emphasis is placed on a task-focused approach to care delivery:
Nicola and Linda are mostly upstairs. But I think they are here because it’s, they are fed and they are hoisted and it’s better if they are here because it’s easier to hoist them and while downstairs is a bit crowded. And, as well, they need, only two of them, they need to be fed and even if you give them drinks, they have drinks with Thick & Easy [Thick & Easy®; Hormel Foods Corporation, Austin, MN, USA] and if they are downstairs some people they, or they cause, like, some extra, mm, attention but not in a good way. Because people are looking at them and they say ‘oh that’s disgusting, I can’t imagine it’. So some people they just don’t want to look at people who need to be fed like those in that lounge. Yeah, so that’s why they are here because they’re hoisted.
Laurie, senior-in-charge, Eden Park CH
In the preceding extract, in addition to the task-focused approach to care being cited as a reason for these residents being seated in a separate lounge upstairs, the senior-in-charge also discusses her perception that other residents would respond negatively to Nicola and Linda if they sat with them.
With the exception of a small group of relatively able residents living in Eden Park CH, the majority of residents spent most of their time within the confines of the care facility. All of the CHs had gardens, however, and during the warmer weather residents would spend time sat outside. There were some barriers to accessing the outside spaces, particularly for those on the upper levels. Yet when residents did go outdoors, being in a different environment seemed to promote conversation. The following extract is taken from Bourneville CH:
I ask Cordelia if she’d be interested in going outdoors, and she agrees. Beryl declines. So I inform a senior care assistant (Leanne) who takes her arm and leads her out of the front door towards a quiet area of the garden that is partially in shade. From the lounge it is perhaps a distance of 20 m or so. We sit together and have a varied conversation, touching upon the time she spent in Sussex, her husband’s career that took her to India, South Africa and to Manchester, as well as gardening. Norman and Scarlet are seated on an adjacent bench, and are in conversation with a mutual friend. After a time they converse with Cordelia, and at one point, Leanne reappears with hot drinks and biscuits. Cordelia seems to enjoy the conversation, and thanks me for the company. After 30 minutes or so, Cordelia says that she has had enough, and so we return to the lounge space, where there is no movement or conversation, and everyone is either asleep or falling asleep.
Extract from fieldwork notes, Bourneville CH
Owing to routine patterns of how space was used in the CHs, residents were familiar with certain spaces and unfamiliar with others. For many residents, this unfamiliarity meant that they were less likely or less comfortable with accessing areas of the CH where they did not routinely spend time.
The following description of a weekly Music for Health class at Eden Park CH illustrates how Kaylee reacted to an unfamiliar space when she was also separated from her usual circle of friends:
Kaylee, who usually sits in a particular lounge or walks around that area with Nora, was brought to exercise class. (. . .) The exercise class starts, but then stops abruptly when Kaylee suddenly stands up and proclaims: ‘I don’t know where I am’. ‘Sweetheart’, the instructor answers kindly, ‘this is the exercise class’. Kaylee then walks over and repeats her statement to Beatrix. (. . .). Myra observes sharply, ‘Well, they shouldn’t have been brought here without their friends’, stands up, and calls out to Katie (care assistant). Katie walks in, tells the instructor, ‘Their friends won’t come to exercise class’, and helps the residents walk back to the lower lounge where there friends are.
Extract from fieldwork notes, Eden Park CH
Being uncomfortable in unfamiliar spaces was particularly apparent at Hebble House, where some residents became very distressed if they were away from a familiar space. This was noted by members of the care staff:
But they get set in their own routines, and they don’t like to be moved [laughs]. I know they say to us, ‘Oh we want to go out, we want to do this, we’re bored’, and you do try and stimulate them, you do try and do something and they’re like, ‘Where are you taking me?, I want to go back upstairs, I want to go back to my room, I want to go back to my area’; they don’t want to participate.
Oh really?
Yeah, but it is good.
Are they all, kind of, quite like to be in their routine then, not . . .
Yeah, because we have tried, we’ve got these sensory groups that we’ve got for them and we do try and take the service users off, take them into the sensory room so they could use it, you could go down the corridor [laughs], take them to a sensory room, start something off with them and they’re off like a whippet, they’ve gone back, ‘Don’t you want to join us?’. ‘No, I want to go back home’, and they get set in their ways, don’t they? They don’t like the change. I know they want the change, they want to do something, they’re bored, they need that stimulation, but in the same time [laughs] they don’t want to do anything, they just want to stay where they are, they want to be left alone.
Any timetabled activities that did occur in the CHs often occurred away from the lounge areas (or in a particular lounge) and, therefore, away from the spaces that some residents routinely occupied and were familiar with. This had implications for residents’ abilities to participate in activities. Residents may not even be aware of activities occurring in other areas of the CH, as there is little information concerning what is taking place elsewhere in the home.
There were ways that care assistants could enable residents to access unfamiliar spaces in the CH setting so that they could participate in certain events and activities. In her interview, Maya went on to outline various factors, including reassurance and providing occupations that residents find meaningful and engaging, that enabled residents to spend time in unfamiliar spaces of the CH:
Yeah, so how do you manage that then, what kind of things do you . . .
Just give them loads of reassurance and try and prompt them and say, help them, you know, and the day will pass by quicker, and sometimes, if they’re in a good mood, they usually stop and they’ll do stuff with you, and if they don’t want to and they’re adamant, there is no way you’re going to make them do what they don’t want to do, they will not do it [both laugh], they will sit there and they will not budge for love nor money [laughs]. We try all sorts, we have like little tea parties, we’ll say, ‘We’ll go a tea room’, you know, sit there, we’ll have little talks and go through reminiscence, knitting and stuff that they used to do and sometimes it will coax them and they will come ‘cause they remember something. And other times they don’t, but if, like we had Pat the dog here yesterday and they all love that, they don’t come down, and we say, ‘Pat the dog’s here’, they’re all downstairs in 2 minutes flat [laughs], and they love the cats, we’ve got Arthur [cat] walking around, we’ve got Shrek [cat] and they love them, absolutely love them.
For a very small number of residents, however, a lack of familiarity fostered a sense of adventure and the desire to explore. At Hebble House, Evie would sometimes be found walking up and down the corridor on the top floor of the CH. Evie sometimes became bored of sitting in the lounge areas and she quickly forgot the layout of the space. Walking up and down the unfamiliar corridor, therefore, enabled her to explore the space and observe the goings on of the CH:
Evie was sat quietly in the front, upstairs lounge. When I entered and sat next to her, she smiled. We had a brief chat and I commented that she does not usually sit here; she explained that she fancied a change. I asked if she was watching what was on the TV and she replied that she wasn’t (. . .). A little while later, Evie stands and announces that she is going to go for a walk to see what there is. She heads to the door and out into the corridor. Once she leaves, I notice that she has left her walking stick. Evie can walk quite well unaided, but I think the stick is there to help with her balance if necessary. I pick up the stick and begin to follow her down the corridor. I quickly catch up with her and return her walking stick, she is pleased and thanks me by giving me a kiss on my cheek. I ask if I can walk with her and she replies that I can, if I like. We walk together down the corridor, which is too narrow to walk side by side, so I walk slightly awkwardly just behind her. She gets to the end of the corridor, where there is the entrance to a small lounge to the right. She peers around the door into the lounge. She then looks back at me, points her stick to the people sat in this lounge, and exclaims, ‘oh, there’s some more!’ This is the lounge closest to her bedroom and where she usually sits, but the space and the residents within it seem to be unfamiliar to her. We return to the front lounge and sit down. We walk up and down the same corridor again a little later on and this time she is curious as to what is behind a red door at the end of the corridor, she opens the door, peers inside and discovers the toilet.
Extract from fieldwork notes, Hebble House
Barriers to and opportunities for enhancing movement
-
Routine use of space:
-
Organisation of physical space.
-
If there was a task-based or resident-focused approach to how residents use spaces/where they spent time.
-
If residents were enabled to move around a space.
-
How residents expected each other to behave in semipublic spaces shaped their conduct in such settings.
-
-
Familiarity and comfort with the CH space. Moving around the house and/or participating in activities is facilitated by:
-
Familiarity of the space.
-
Familiar faces and companionship.
-
Engaging occupation and activities.
-
Encouragement, reassurance and support of care staff.
-
Daily routine: residents’ daily life in the participating care homes
The pattern of residents’ daily life was largely structured around regenerative activities and discretionary/leisure activities.
Regenerative activities
Regenerative activities are those activities that are carried out to maintain residents’ physical existence, and include eating, drinking, taking medications, personal hygiene, sleeping and resting. Residents required support with such activities, with the most vulnerable at each of the four CHs almost entirely dependent on staff to undertake regenerative tasks, including eating and drinking. Supporting regenerative activities was the core business of all of the CHs because of the needs of the residents.
Such activities were often delivered at key points of the day: getting up and breakfast, lunchtime, the evening meal and going to bed. The manner in which such support was delivered, however, was shaped by the care environment (as discussed previously in Organisation, management and delivery of care). Between such bursts of activity, many residents spent time either in the lounge areas (or their bedrooms) sitting quietly, resting or engaging in discretionary activities.
Resting
Between the bursts of bed and body work, residents often spent a significant amount of time resting. Researchers noted how quickly residents would tire from both physical movement and social interaction. Resting was one regenerative activity that residents did not usually need the support of care assistants to achieve.
At all of the CHs, it was commonplace to observe residents sat in the lounge areas sleeping in their chairs. There were some residents who were alert some days and extremely tired on other days, and there were some residents who spent considerable amounts of time each day resting and sleeping. For instance, at Hebble House, Mabel would be alert and chatty on some days, but, on other days, she would spend much of the day curled up in her chair, cuddling a soft toy and sleeping deeply. On such occasions, she sometimes commented that she was too tired to eat or drink. Lesley, on the other hand, would catnap throughout the day and would often request to be taken to bed in the middle of the afternoon, as she felt tired:
As I approached the front, upstairs lounge I saw that James was snoozing in his chair. Lesley was stood up by her chair by the entrance to the lounge. I greeted her and she grabbed my hand, telling me that she wanted to go to bed. We talked briefly about her feeling sleepy. She asked me the time and I told her that it was 3.20 in the afternoon, she was surprised it was that early as she thought it was much later as she felt so tired. We chatted a little more about feeling tired and then she returned to sitting in her chair.
Extract from fieldwork notes, Hebble House
Resting formed a significant and important part of the day for many residents.
Mealtimes were significant events for residents, in that they provided an opportunity for movement between different spaces, as well as banter between staff and residents, which was facilitated by the close physical proximity that the delivery of food and drink entailed. The following extract from ethnographic notes relates to a mealtime session at Rowntree Nursing Home, and the interaction between Alison (the activity co-ordinator) and two residents, Madeleine and Nicholas:
Simone, the care worker, leaves the room and Alison feeds Madeleine. ‘What time are you going home?’ asks Madeleine of Alison, who replies ‘3 o’clock. Can’t get rid of me, I’m like a bad penny’, and adds ‘you look like you’ve had a hot flush, have you been running up a hill?’. As Madeleine tucks into her pudding, Alison comments ‘got a bit of a sweet tooth, Madeleine? Nowt wrong with that, you’re a good little eater’. Nicholas is wheeled into the communal space from having had his hair cut by the hairdresser, who comments favourably upon what seems to be renewed hair growth on the top of Nicholas’s head. Alison asks wryly ‘what have you been putting on your head?’, and Nicholas smiles and replies ‘nothing’ to which Alison says ‘maybe it’s watching all that Jeremy Kyle’ and he grins broadly.
Extract from fieldwork notes, Rowntree Nursing Home
Discretionary and leisure activities
The pattern of residents’ daily life was also structured, albeit often to a lesser extent, around discretionary and leisure activities. These activities can be thought of as consumptive or productive in nature. Consumptive activities are those activities that are carried out for their own sake, for instance watching television, listening to music, reading and creative activities. Productive activities are those that are carried out for their outcomes, such as domestic tasks, and are often delegated to staff in CH settings. The nature of such activities, and whether or not such activities were supported and/or enabled, was shaped by the CH environment and, therefore, the ethos of care.
Consumptive discretionary and leisure activities
The degree to which such activities were organised and/or enabled by the care environment varied across the CHs. Many of the activities organised by the CH were communal. Rowntree Nursing Home, which aimed to foster a holistic approach to care, allocated a significant amount of resource to organising and delivering a range of leisure activities. This was done by employing numerous professionals, including an experienced activities co-ordinator, a physiotherapist, a complementary therapist, a reminiscence therapist, someone who supported arts and crafts, and so on.
Care assistants would occasionally engage residents in conversations and/or ad hoc activities. It is important to note that the ability of care assistants to engage residents in occupation in a meaningful and personalised manner varied both between and within the participating CHs. This ability was shaped by several inter-related factors, including the ethos of care, the care environment (the way care was organised and delivered), the degree to which such engagement was supported and encouraged by the CH manager and senior staff, and whether or not the care assistants perceived this to be an important part of their role.
Certain care assistants at Hebble House viewed engaging residents in activity as part of their role (especially in the absence of an activity co-ordinator). Despite being very busy and often being pulled away from engaging with residents to attend to the needs of others, these care assistants were particularly adept at engaging residents in activities that, although communal in nature, were tailored to individual needs. The following edited extract illustrates one occasion when Sarita, a care assistant, worked to enable residents to engage in an ad hoc game of catch:
From approximately 2.30 p.m., I sat in the front, downstairs lounge. There were eight residents sat around the perimeter of the room (Julie, Amy, Polly, Mary, Philip, Judi, Ann and, initially, Mavis) and one care assistant, Sarita, who was attending to them. Music was playing on the CD player. Everyone was sat around quietly, Sarita left for a few moments, and when she returned, she picked up a beach ball that was lying in the corner of the lounge and tried to encourage people to engage in a game of catch with her. First, she addressed Julie, who was sat in a seat next to me. Julie is the most physically able of the residents who were sat in the lounge this afternoon. Sarita stood in front of Julie, who remained seated, and threw the ball to her. Julie smiled. Julie and Sarita then threw the ball to each other and Sarita counted the number of throws. Julie, who is physically very able, managed this with ease. Sarita then moved from one resident to another throwing the ball.
Mary, Phillip and Judi (who were all sat next to one another) are very physically and cognitively frail. They are hoisted into their comfy chairs in between meals and move very little. Mary and Phillip are no longer able to speak. Sarita tried to involve these residents in the game of catch. She gently placed the beach ball on Mary’s lap and encouraged her to try and hold the ball. Mary briefly looked at Sarita, but then continued to stare straight ahead. She seemed unaware that the ball was there, despite Sarita attempting to draw her attention to it. After a few minutes of trying to engaging Mary in the activity, Sarita moved on. Phillip was fast asleep and Sarita did not try to wake him. She moved to stand in front of Judi instead. She asked Judi if she wanted to play; Judi smiled. Sarita gently threw the ball to Judi, but she did not manage to catch it. So, Sarita placed the ball on her lap and encouraged her to try to grasp the ball in her hands. Judi replied that she could not do it, so Sarita gently placed Judi’s hands on the ball. Judi held the ball. Sarita encouraged her to throw it. Judi said she was unable to. Sarita then suggested she just tried to push the ball forward. Judi replied that she is unable to use her left hand. Sarita continued to encourage her, explaining that she uses her hand to hold her cup to drink. She encouraged Judi to pick up her cup of juice by her side and take a drink to demonstrate that she is able to grasp with her left hand. Once Judi had done this, Sarita encouraged her to hold the ball once more. Judi did so and managed to push the ball forward a couple of times. She was smiling throughout this activity and seemed to enjoy the interaction with Sarita. Sarita then turned to Ann. Ann, who is usually quite jovial and generally in a good mood, seemed down today. She refused to join in and gave the impression that she thought it was a silly game. Sarita then threw the ball to Julie, Amy and Polly once more, before finishing the ball game.
Extract from fieldwork notes, Hebble House
Throughout this episode, however, Sarita’s attention and focus was repeatedly dragged away from the game. Sarita was drawn away from the ball game to ensure that residents were drinking, to check on Phillip (he was very ill the previous week), to comfort residents (Amy and Ann) and to support Amy, who is unsteady on her feet and repeatedly tried to stand and walk.
At Hebble House, the ability of some care assistants to engage even the most vulnerable residents to participate in ad hoc activities was evident. This was due, in part, to their knowledge of the residents as individuals, both in terms of their individual needs and abilities, and their identity as persons. It was also encouraged and reinforced by the organisational emphasis on enabling residents, as the CH manager praised the actions of these care assistants. The skills of some care assistants at engaging some of the most vulnerable residents often surpassed those of external professionals brought into the home to provide activities.
Many of the leisure activities provided by the CH or delivered by care assistants were communal in nature as a result of the organisation and delivery of care (it was unusual for residents to receive one-to-one input). Some communal activities, however, seemed to engage residents much more readily than others. Of importance was whether or not the activity was familiar or was connected to residents’ life history in some way.
Music and musical performances were extremely successful at engaging residents, as the music performed was associated with their past, but was also something that could be enjoyed communally, in the present, as a shared experience. Residents also knew how they were able to join in, for instance by tapping their feet, singing along or even dancing, and would often do so unprompted. Verbal encouragement, as observed in Rowntree Nursing Home, was also helpful in engaging residents in the activity:
Reginald starts to play a Scottish tune. I am seated next to Veronica, and without prompting from anyone, she moves her feet and gently claps her hands to a Scottish jig. Three other women start to clap their hands. I notice that Stephen is clapping now and it seems to encourage others to follow suit. I notice a lady seated at the back of the room tapping her feet, and one or two other ladies are mouthing the words. There is warm applause at the end. The residents seem quite engrossed now, with many of them mouthing the words. He sings ‘That’s The Story of My Life’ and I notice Hilda, who is generally still, moves her head from side to side. I reflect again on the power of music to help residents to reconnect with an earlier part of their lives. There is some warm laughter towards the end, and I reflect upon Reginald’s warm friendly rapport with residents and the importance of this in eliciting their engagement with the music.
Extract from fieldwork notes, Rowntree Nursing Home
At Hebble House, music was often played in the day-centre lounge and residents would occasionally engage in an impromptu singalong or dance. Care assistants often encouraged those who they knew enjoyed singing or dancing, and their participation would often encourage others to engage in the activity.
Knowing the abilities of individual residents was important to engage them in activity. One of the residents at Rowntree Nursing Home, Edith, had a keen interest in playing the violin. Being encouraged to do so was immensely satisfying for her, at least in part as representing an important aspect of her identity. The following extract from ethnographic notes summarised her engagement with playing the violin:
Alison (activities co-ordinator) asks ‘can I get your violin?’ to Edith, who frowns a little, saying ‘you’re a nuisance aren’t you?’ and then signals her assent. Alison disappears to fetch it (and) reappears with a battered old brown leather violin case, which she opens up. Edith takes hold of the violin and bow and starts to play in her seated position, firstly a Scottish dance piece, and Harriet, Madeleine (residents) and the care workers applaud. She then plays Noel, followed by a few patriotic tunes, Rule Britannia, God Save The Queen, There’ll Always Be An England, Land of Hope and Glory. I am struck by the high quality of her performance, and the ease with which she manoeuvres the bow . . . Edith asks us to suggest additional tunes for her to play, and performs Ba Ba Black Sheep, followed by When The Saints Go Marching In, and then In The Bleak Midwinter. She finishes by playing When Irish Eyes Are Smiling.
Extract from fieldwork notes, Rowntree Nursing Home
Alison, the activity co-ordinator at Rowntree Nursing Home, recognised the connection between activities that engaged residents through their past interests during a conversation with the ethnographer:
Alison (activities co-ordinator) then speaks generally about the way in which different kinds of events and activities spark interest among different residents. She refers to a visit before Christmas by a woman who gave a talk to residents about Yorkshire dialect, which some residents, who had knowledge of Yorkshire dialect, could join in with. She also mentions a talk given around Christmas time on Christmas dinners from the past. She felt that this was of particular interest to Alan H, who used to work as a butcher within the area, as well as another female resident who taught domestic science within schools. Apparently, both residents, who do not ordinarily participate in activities, were engrossed in these talks, which resonated with their working lives and their involvement with food.
Extract from fieldwork notes, Rowntree Nursing Home
At Rowntree Nursing Home and Hebble House, baking was another activity that evoked keen interest and engagement among those who participated. A combination of evoked memories from their past, communal directed involvement and the physicality of the process seemed most pertinent here. The following extract from ethnographic notes summarises the involvement of residents in a bread-making session at Rowntree Nursing Home:
Veronica, Anita, Lucy and Edith are seated at a table in the conservatory space. There are two bowls of flour and Alison pours a tablespoon of oil into them, and Anita stirs the flour and oil with a knife. The bowl is then handed to Lucy who takes over. More water is added to the bowl by Alison and it’s handed over to Veronica, who says ‘I’m finding it very difficult’, and wants to use her hands, but is told to use the knife. Alison explains that it needs to be ‘proved’ so that it can rise.
The dough mixture is then taken out of the bowl and given to Anita and Lucy on one side of the table, and then Veronica and Edith on the other. Each resident then takes turns to knead the bread with their hands. ‘Really knead it, Anita, pretend it’s someone you don’t like’ says Alison, and she kneads it well, her long fingers pressing into it with gusto. The dough mixture is then passed to Lucy, who continues to do it well and is told to use her knuckles, which she does to quite good effect. Edith then takes over. It’s then passed to Veronica, who struggles to exert much force on the dough, her small, delicate fingers seemingly lost in the dough rather than in control of it.
As they work, the group tell me that they used to make bread at home, with the exception of Veronica, who watched her mother do this (. . .) it is the sharing of the activity in a collective environment, the constant encouragement from Alison and the sense of companionship within the group, even without a welter of verbal communication, which seems to produce most impact.
Extract from fieldwork notes, Rowntree Nursing Home
Similarly, engaging residents in humorous banter facilitated their participation in activities. Mark, an arts and crafts co-ordinator at Rowntree Nursing Home, often used humour to interact with residents. The following extract from ethnographic notes concerns the commencement of a painting session:
Mark takes a roll of white paper and unravels it along the length of a dining table, about four feet by three feet, and uses Sellotape to affix it to the underside of the table. Edith comes into the dining area to join us and is accompanied by Marika, the Dutch resident. Immediately Mark begins to engage in banter with them. He takes a cylindrical item, looks through it as if it were a telescope, and says ‘I see no ships, only hardships’ and the residents giggle. He then says, ‘I went to a good school mind, it was approved’, and they laugh. He engages in banter with them about the plurals of nouns. There follows a comical discussion between Mark, Marika and Edith as to whether sheep have tails, and the difference between male sheep (rams) and female sheep (ewes). Mark hands out some leaves of a chrysanthemum plant from a raised bed at the side of the dining room and hands it to the group, asking them to smell the aroma of the plant. Mark asks them to think of something they might like to paint that is associated with spring. The groups are struggling for ideas, and Mark takes a pencil and draws a crocus, a daffodil and a sheep to give them an impetus. Mark puts a plastic tray with different coloured paints, including orange, yellow, green and blue. He dips a paintbrush into orange paint, passes it to Marika and asks her to paint the head of the daffodil, and he is encouraging of their efforts, commenting to Marika ‘you’re like Vincent van Gogh’, and she smiles at the connection with her Dutch heritage.
Extract from fieldwork notes, Rowntree Nursing Home
Interactions involving banter were much less frequent in Bourneville CH, partly, it seemed, because of the enhanced time pressures on staff, hurtling from resident to resident to offer assistance, and the organisational emphasis on task-focused interaction and the completion of paperwork.
Activities that permeated the boundary of the CH facilities also seemed to engage residents, including activities that involved animals. At Hebble House, various activities were arranged that involved bringing animals into the CH, including ‘pat the dog’ and, on another occasion, bringing a donkey into the day centre. Although these activities were not observed by the researcher, care staff spoke of how much residents enjoyed such activities. Similarly, a visit to Rowntree Nursing Home by West Riding Farm enabled residents to interact with small animals, and evoked strong engagement. The following extract from ethnographic notes explores this visit and the impact that it had on resident well-being:
Marika, the Dutch resident, tells me of her love of animals and of her dog, which she felt intuitively understood whether she was feeling happy or sad. Alison and Tina, the physiotherapist, bring residents into the conservatory space: Nancy, Alan H, Albert, Betty, Hilda, Edith, Anita and Lucy. Madeleine, seated in a chair, is wheeled into the room. A woman from West Riding Farm arrives with a cat, guinea pig, rabbit and a lizard. Edith cradles (the cat), and smiles. I reflect upon the number of times she has told me she needs to go ‘home’ to look after her cats. She interacts with it warmly, stroking it and gazing at it admiringly. Meanwhile, the lizard rests on Ruby’s lap. The grey guinea pig is passed to Alan H who strokes it, smiling. Tracey, a care worker, strokes the rabbit, which rests in the lap of Trevor, a resident with an amputated leg, who recently moved into the CH. Meanwhile, the guinea pig defecates on Alan T’s lap, and he laughs as the rounded balls of excrement are removed, and the guinea pig is then put onto a towel that rests upon Colin’s lap. Colin strokes it tenderly, and I reflect upon the impact that this activity is having in terms of relaxing residents, provoking humour and perhaps reminding them of a time when they may have kept domestic animals or else engaged with them during their working lives. ‘Oh Albert, you don’t look impressed’ says Alison as the cat tramples uninvited onto Albert’s lap, and he grins broadly, his sole tooth glinting in his open mouth. Alison takes hold of the cat and it is placed onto Alan H’s lap, and Alison encourages him to tickle it under its chin, which he does.
Extract from fieldwork notes, Rowntree Nursing Home
Communal activities that engaged residents were often those that had some connection with their past, but could be enjoyed communally and residents knew how they could participate.
Some activities did not really engage residents, and it seemed that these were not meaningful for residents. Often, such activities appeared to be more attuned to the interests of the CH regimes, in terms of the relative ease of provision, rather than a realistic appraisal of the extent to which a diverse range of residents, with the broad range of interests that they represented, would wish to become involved with them.
At Rowntree Nursing Home, an exercise in reminiscence therapy involving the use of plastic toy animals did not seem to evoke much interest, given the response from residents. An extract from the ethnographic notes is illustrative of this:
Annie (reminiscence therapist) informs me she is doing an activity which requires residents to name furry animals that she is carrying with her. There are five residents, including Veronica and Monica, the German lady. Annie goes from resident to resident with her plastic tiger, monkey and lion, asking residents to name each of them in turn, and records their responses on a sheet of paper. I say hello to Veronica, who is not enthused by this activity. She says ‘this is what we’re doing now, it’s supposed to be entertaining’ with more than a hint of irony. It’s certainly not entertaining for her. I reflect upon the need to develop activities that are of interest to everyone. It seems that this kind of activity is much too easy for Veronica. Whilst there are certain activities in which everybody can be encouraged to participate, such as musical events, it seems that there are others, such as these naming activities, which are entirely meaningless for some residents.
Extract from fieldwork notes, Rowntree Nursing Home
A lack of knowledge of residents’ abilities, likes and dislikes, also affected the ability of residents to engage in activities, as the following extract demonstrates, which details an exercise class at Eden Park CH:
The exercise class is about to begin. The instructor is a young woman who works for a private company. In the absence of staff, who are probably busy in residents’ private rooms, the instructor finds it difficult to persuade residents to walk to the upper-level lounge, which is cold and unfamiliar to residents. The instructor appears displeased as she has been waiting for 20 minutes to have residents settled in the room. Today there are eight participants for the class.
The instructor introduces the first activity, ‘moving’. She explains that it involves all round movement to help improve circulation and co-ordination. The residents are told to move their feet up and down, then to turn at the neck, shoulders and waist. The instructor encourages them to participate, but tells those who find this activity too difficult to refrain. Kaylee and Nora do not seem to have followed the instructions. Myra, who has swollen feet, also does not do the activity. Serena and Constance are in wheelchairs and are unable to move their feet. Only three of the eight participants are able to do the movements (. . .). Later the instructor introduces a complex set of instructions about an unfamiliar activity using a hoop, which residents also struggle to engage with. While this activity is in progress, however, Kaylee’s daughter walks in, joins the circle, and begins doing the hoop exercise following the instructions. Kaylee, who is pleased to see her daughter, immediately begins to imitate her daughter.
Extract from fieldwork notes, Eden Park CH
On some occasions, staff members did not ask residents if they wished to take part in a particular activity or they did not try to actively engage them in anyway. At Bourneville CH, Vanessa, the activity co-ordinator, would occasionally play a digital versatile disc (DVD) for residents. This seemed more to do with Vanessa meeting her remit regarding activities provision, rather than representing a genuine attempt at providing something with a resident-centred focus. The following extract from ethnographic notes details one such occasion:
In the lounge, I am seated with Scarlet and her husband, Norman, and Beryl and some other residents are seated to our right. Vanessa (the activity co-ordinator) walks into the lounge, bends in front of the television, tinkers with it and then leaves, and it’s only then that I realise she has put on a DVD. It is the film The King’s Speech. There has been no consultation with residents about this. I don’t think that anybody has requested to watch any film, or this particular film. It has just been put on. Scarlet and Norman start to watch it, although they have seen it before. The other residents are drowsy or asleep. Nobody is really watching the film.
Extract from fieldwork notes, Bourneville CH
It was common to find residents in the lounge spaces resting or sitting quietly. The following is an edited extract from fieldwork notes that summarises an entire morning (09.30–12.00) of observations in the day-centre lounge at Hebble House:
The day centre was largely quiet and peaceful for much of the morning. The lounge gradually filled up with residents from 9.30 a.m. onwards (over the morning, the number changed slightly, but stayed around eight – including Harry, Joy, Ann, Seth, Thomas, Bella, Caroline and Megan). Most sat quietly – occasionally the volunteer, the staff member and I talked with residents. Music was playing in the background.
When the day-centre bus arrived at about 10.45 a.m., the three day-centre participants – Jacob, Olivia and Esther – quickly settled in amongst the other residents. It was a lovely sunny day, so Olivia, Joy and Ann sat outside on the benches. Once people attending the day centre had arrived, Morag (care assistant) began preparing and distributing cups of tea and coffee and biscuits. People sat quietly sipping their cups of tea. Morag asked those sat in the lounge area if they wanted to do a jigsaw or puzzle – but no one responded. The rest of the morning was spent quietly, some slept in their chairs and others sat in silence.
In between smoking her cigarettes outside, Joy would walk back inside to sit in the lounge using her [walking] frame. Joy and the volunteer had a short conversation about horse racing. Besides Joy occasionally moving in and out of the lounge and talking to the volunteer, there was very little movement or interaction.
A little later, Seth asked a care assistant who he was sat next to. She replied that he was sat next to Thomas. Seth called Thomas a ‘pillock’. The staff member gently reprimanded Seth for being rude to Thomas. Seth spoke to the staff member for a while, and eventually settled down and fell asleep. The lounge fell quiet again.
Music was quietly playing in the background. Thomas spontaneously stood up and swayed to the music, occasionally clapping his hand. The volunteer noted that Thomas enjoys dancing. At this time, Ann and Joy were sat outside smoking, occasionally chatting and laughing. The other residents, sat inside, rarely spoke or interacted with one another. This was the case until lunchtime approached and the volunteer started to set the tables in the dining area of the day centre, with the help of Mavis (a resident).
Extract from fieldwork notes, Hebble House
The preceding extract demonstrates a typical period between mealtimes when some residents engaged in activities such as resting, sleeping, conversing, smoking and dancing.
In addition to those activities organised by the CH or supported by care assistants, residents also occupied themselves with activities such as talking with one another, reading and watching television.
In general, there was little conversation between residents. However, reading and watching television sometimes provided points for discussion or triggered a conversation. The following extract demonstrates how reading and discussing what they have read gave some of the residents of Eden Park CH the opportunity to interact with others:
Five residents (Serena, Laney, Constance, Eda and Ashby) sit quietly reading. Serena is reading a book and the rest are reading newspapers. ‘The murder of the soldier in London was horrendous. Nobody is safe really!’ notes Eda. ‘What do you mean?’ asks Serena. ‘There was this . . .’ Eda begins to explain, but Ashby interrupts, telling her that Serena does not want to hear negative stories. Laney looks up and says, ‘There was a ravaging storm in Oklahoma. Did you see that dog that survived in the rubble?’. A visiting male resident at the next table chimes in, ‘My son saw it and got worried about his dog’. Ashby takes a new tack with, ‘Well I am happy I lived the time I did. The world now is upside down. I have to tell you this. I always worried that one day we would be wiped by the sea. You know how UK is surrounded by the sea. I don’t worry now, because I am old.’. Serena replies, ‘That is why I read books. My favourite book is The Book of Books.’. Interested, another resident responds that he has heard about The Book of Books but cannot remember its content. Ashby responds, ‘Um, it led to many changes; talked of civil rights movements, equality, and women’s rights. I can’t remember everything. I have the book in my room.’. Eda, also trying to remember, adds, ‘Was it not the King James Bible?’. ‘I am not a religious person,’ says Ashby, ‘but I think the King James Bible had to do with the Protestantism and the Church of England, and all that stuff about breaking away from the Roman church.’. ‘Well, we have a King James Bible, don’t we?’ Constance observes.
Extract from fieldwork notes, Eden Park CH
Few residents at Hebble House read or actively watched the television. Occasionally, however, something on the television was meaningful to a particular resident and could prompt a train of thought and conversation:
There were five residents sat in the comfy chairs in one of the upstairs lounges (Jane, Caroline, Mabel, Evelyn and Elizabeth). The room was quiet. As I entered the room, I said, ‘hello Caroline’, as she was sat in the chair next to the door. On hearing her name, she reached for my hand. She said that I had been the first person to use her name today. She clung onto my hand, tightly, and she chatted. (. . .). She started to talk about the storm that hit the UK yesterday, and she mentioned that a teenage lass had died, and how terrible it all was. She told me that she likes watching the news, but that she was a panicky mum and she started to talk about her children. (. . .). As we were chatting, Jane leaned forward to listen. Caroline said that she [Jane] wanted to join in our conversation. Jane then stood up and gradually shuffled towards us. Jane told me that she and Caroline chat and that they go for walks. Caroline agreed, saying that she and Jane take each other’s hand and walk. (. . .). We chatted for a few moments longer, then Jane said that she must be off and she pushed her [walking] frame forward and took shuffling steps towards the door and out down the corridor.
Extract from fieldwork notes, Hebble House
Across all four CHs, residents spent long periods of time sitting quietly, often resting. Often, what looked to outsiders like a lack of activity was acceptable or tolerated by residents. In the context of the ambiguous CH setting, residents had limited resources with which to initiate activity themselves. Residents had physical and cognitive impairments, which restricted their ability to move and engage in activities. There were also limited facilities available for residents to engage in occupation. The lounge areas, where residents spent considerable amounts of time, were dominated by comfortable chairs and televisions, and little else. Sometimes residents would verbalise their frustration at this lack of opportunity for occupation. This frustration was particularly acute when residents wished to interact with others but conversation was not forthcoming.
The following is an extract from ethnographic fieldnotes at Rowntree Nursing Home:
I return to the lounge where four residents are sitting quietly. I notice a member of staff enter the downstairs lounge – this is the sole care worker, and as she leaves a female resident (Veronica) calls out ‘I don’t want you to waltz out and just leave us, what do we do, just sit here and wait?’ The other residents in this lounge are resting. She continues ‘will somebody please come back now?’, ‘Is there nobody here who will help me?’ she calls. The care worker responds, ‘I’m doing the medicines, I’ll be back in half an hour’ and the woman replies ‘Can you see me waiting for half an hour?’.
Extract from fieldwork notes, Rowntree Nursing Home
Similarly, at Bourneville CH:
Scarlet is in the front lounge with other residents, but there is silence. She says something, but there is no response, and in frustration she says loudly ‘that’s right, ignore me, that way I don’t need to talk to anybody’. I reflect again upon the absence of social interaction and the anxiety/irritation that this can cause as Scarlet gazes into the distance, one hand in the shape of a fist pressed against her forehead and the other hand resting upon her lap.
Extract from fieldwork notes, Bournville CH
Across all the CHs, however, a small number of residents were able to occupy themselves when they wished: for instance by reading, walking around the CH or adopting a particular role. These residents were either able to initiate and engage in such activities unsupported, or enabled to do so by care staff.
Productive discretionary and leisure activities: finding a role in the care home setting
A few residents were able to adopt an active and productive role in the CH setting. Some residents engaged in productive discretionary and leisure activities, such as helping others or doing domestic tasks.
At Eden Park CH, the small group of seven relatively able residents established an active social group with an interest in the running of the home. They participated in resident meetings and occasionally helped other residents by advocating on their behalf. This kind of critical engagement with the CH and the service it provided was unusual (and only found among this small group). This group of residents had managed to establish a distinct and purposeful role within the CH setting.
The following extract describes an incident when Eda, a resident, spoke to staff members about dehydration:
Eda is holding a newspaper, the headline of which reads: ‘More deaths are caused by dehydration in the CHs . . .’ Slowly, she stands up and walks into the dining room, where staff on break are having a cup of tea. The seated staff group includes Dylan, Natalie, Chloe (assistant manager), a domestic staff member and Peter (chef). ‘I wanted to draw your attention to this’, Eda says, pointing to the newspaper headline. ‘If we can have at least one staff [member] to check on the frail[est] residents and help them have at least a sip of water, [it] would be good. You know they can’t help themselves.’ Chloe, the assistant manager, looks at the headline and draws it to the attention of the other staff members. ‘Thank you,’ she says to Eda, in an appreciative tone.
Extract from fieldwork notes, Eden Park CH
It was not unusual at Eden Park CH for this group of residents to point out to staff instances when, in their opinion, the delivery of care was falling short.
Across all the CHs, there were examples of residents helping others; for instance, at Hebble House, Mabel would often find Evie’s walking stick and return it to her. At Eden Park CH, one of the most able residents, Ashby, would help with the delivery of care if he felt that residents’ needs were not being met. For instance, he regularly reassured residents if they were distressed, made them cups of tea and even helped some residents to drink:
Ashby and Eda walk into the lounge. Linda is making high-pitched sound. They stop and walk to where Linda is sitting in a wheelchair; holding Linda’s sippy cup, Ashby says, ‘take at least a sip’, as he tries to feed Linda. Linda is helped by Ashby to take two sips, after which Ashby kisses her, and Linda kisses him; Linda smiles.
Extract from fieldwork notes, Eden Park CH
The degree to which the care environment enabled residents to adopt such a role varied. During his interview, Ashby noted that, in recent times, he has been reprimanded for helping other residents:
I get told off a hell of a lot now, because, at one time, you used to help people, and now they say, ‘It’s against health and safety. You’re not allowed to do this’ and ‘You’re not allowed to do that’. You know, I mean, we used to help, me and Eda used to help a lot of people, you know. But [now], if they’re gonna fall, you have to stand out of the way and let them fall. But I don’t like the idea of that.
Ashby, resident, Eden Park CH
At all four CHs, some residents volunteered to do certain jobs, often domestic tasks, around the CH. These activities were often familiar or meaningful for the individual because they were activities that they had routinely undertaken at home (tidying, washing up, setting the table), or they were associated with hobbies (gardening) or their job (sorting out paperwork). For instance, at Rowntree Nursing Home, Anita was observed undertaking everyday tasks:
I see Anita appear from behind Christina (a relative) and pull the curtains so that they are closed. Behind me I am aware of Lucy pulling the curtains from the other side of the bay windows. When these are closed, I then see Anita and Lucy walk over to the other side of the room and close the other curtains – there are about eight pairs of curtains (. . .).
Extract from fieldwork notes, Rowntree Nursing Home
At Hebble House, in particular, the meaning that residents attributed to the CH also led them to adopt a particular role in the setting. For instance, Polly often perceived the CH to be her own private home and so she would occasionally tidy the lounge area or work with care assistants to tidy the kitchen area.
It is important to note that care staff played a central role in whether such activities were recognised, curtailed or supported in the CH setting. This had implications for the extent to which residents maintained such activities over time.
For instance, Darren had lived at Bourneville CH for several years, during which time he tended to the garden. His daughter, Delia, felt that, in recent times, the staff’s lack of appreciation and support of his gardening, combined with his declining health, meant that he felt deterred from continuing to garden and subsequent loss of interest:
What caused the change, what precipitated the change [Darren’s participation in gardening]?
Well, (a) he’s not as fit and able as he was, he can’t walk very far without being extremely breathless, and the other reason was that he didn’t feel as though he was being supported, nobody would help him to turn over the soil, they’d always be promising that they’d do it but it never happened, you know; in the raised beds, he’d struggle with the hosepipe and then he’d get annoyed and frustrated and say, ‘Well, it isn’t my job’, you know, the hosepipe goes all around the back of the building, in order to water the baskets that they have under the windows on the conservatory thing, and he used to do all that; it would just have been nice if now and again somebody would have wandered around with him and said, ‘Well I’ll help you’, but they didn’t. And because they’re too busy doing the day-to-day things that they have to do. (. . .). Like, at one time he grew some herbs for the kitchen, and his carrots [laughs] and things like that, and he’d pick them and his lettuce, and he’d take them in and they never used them, so he got around to thinking ‘well they must just bin them, what’s the point, why should I bother?’.
At Bourneville CH, the organisation and delivery of care, including the perceived role of the care assistants, had implications for the lack of support and encouragement Darren received.
At both Rowntree Nursing Home and Hebble House, however, there were instances when members of the staff team would actively encourage, facilitate and support residents to undertake certain tasks around the house. This was facilitated by knowledge of the individual.
The researcher had observed Stacey, a member of the domestic staff at Rowntree Nursing Home, facilitating residents’ involvement in domestic tasks. In her interview, Stacey reflected on her experiences of engaging Orla in activities that were meaningful for her:
Orla only retired a couple of years before she came here, and she was a nurse as well, so she’ll know all the roles of this place, and yes, I’d take her into the laundry and we’d fold tea towels and stand and have a chat, ask her what she did at work and what she liked doing best and, I always get a good response from Orla, I always get a cuddle, she’ll always come to me, and she will start folding and she can do it but then she might start overfolding, unfolding again, which isn’t a problem because she’s just happy chatting really and she feels as if she’s doing something and is part of something.
Stacey, domestic at Rowntree Nursing Home
Enabling residents to engage in purposeful activities around the CH was also facilitated by several members of staff at Hebble House. Mavis, who sometimes believed that the CH was either her private home or her workplace, could regularly be found tidying the CH. The following extract, taken from observations at Hebble House, demonstrates how Mavis was enabled by care staff and the volunteer to take an active role in the CH setting:
As lunchtime approached, the volunteer started to set the tables in the dining area of the day centre. Mavis appeared in the dining room and started to help the volunteer set the table. She took cups from the tea trolley and placed them on the tables. The volunteer allowed her to continue, but discretely began to collect the cups as he continued to set the tables. He quietly explained to me that these cups had already been used that morning, so needed to be washed. Mavis continued to help setting the tables by putting the cups out. A staff member came into the dining room and praised Mavis for helping to set the tables. She explained that she was pleased, as she had suggested to Mavis she may like to help set the tables.
Extract from fieldwork notes, Hebble House
Stacey, a member of the domestic staff at Rowntree Nursing Home, pointed out that when residents first moved to Rowntree Nursing Home, they continued to do some of the activities that they used to do in their own homes. She highlights the potential for enabling and supporting new residents to continue undertaking such activities:
A lot of them, when they first come in, they’ll get their cup and saucer and they’ll come to the kitchen and they want to wash it up and I think that would be nice if they could because, there is another sink downstairs and I think if they wanted to go and wash those pots up in the sink, they do it in their own sinks in their room, you know, and then we’ll find the cups and saucers.
Stacey, domestic at Rowntree Nursing Home
At Hebble House, care staff actively created a role for Julie, a relatively new permanent resident. Julie is physically very able and likes to keep busy; she is often found walking around the CH, sitting looking at magazines, talking with others, or, if music is playing, dancing. She regularly becomes quite down, however, and wishes to leave the CH and go home. Sometimes she will sit, with some of her belongings, waiting to be taken home. The care manager, Laura, began to invite Julie into her office and gave her small tasks to do, including stacking papers. According to Laura, Julie enjoys such small jobs and she is convinced it has given Julie a sense of purpose. Laura works late 2 days per week to catch up with paperwork and now regularly invites Julie to help her in the office. Some care assistants, taking the lead from Laura, have also allowed Julie into the office to sort paperwork. Julie has also begun to help out in the laundry room.
Even at Rowntree Nursing Home and Hebble House, however, there were challenges to enabling residents to adopt a purposeful role within the CH settings. An awareness of the potential risks involved in residents undertaking such tasks meant that care assistants were sometimes keen to step in and take over, rather than enabling the residents to do things for themselves. The following extract from Rowntree Nursing Home illustrates such an occurrence:
I see Anita walk into the downstairs lounge carrying four drinking mugs and put them down onto a small table. Seeing her do this, a male care worker says to her ‘let us take those into the kitchen’ and as Anita then sits down, the care worker picks up the mugs and takes them away. I am surprised to see a resident carry such items in this unsolicited way, as it is something I have not witnessed before. I ask Anita if she has carried and/or washed these mugs before and she says ‘oh yes, I often do . . . do you want me to show you the kitchen?’. I agree to this, so she gets to her feet and gently shuffles her way down the corridor toward the staircase and then turns left toward the main kitchen, but then opens an adjacent door which houses a small washbasin.
Extract from fieldwork notes, Rowntree Nursing Home
At Hebble House, the CH manager, who aligned herself with an ethos of care centred around the enablement of residents, discussed how she was working to encourage care assistants to routinely enable residents to have a more active role within the CH setting. One way she felt that this could be done would be to enable residents to serve themselves teas and coffees, rather than the care assistants serving residents, which was usual practice. She firmly believed that many residents would be both capable and willing to do this and she illustrated this point by giving the example of taking a group of residents out for a pub meal, when they all poured themselves tea from a pot, as that is what they expected to do in that context. She had had little success in persuading care assistants to enable residents to do this in the CH setting, however, because of the perceived risks in allowing residents to pour boiling hot water. She also felt that, although some residents would happily adopt a more active role if the care assistants allowed them to, there were others who she felt would resist, as they preferred to be looked after and this was their expectation of life in the CH.
Barriers to and opportunities for enhancing movement
-
The relative importance given to regenerative and leisure activities.
-
Whether residents’ participation in occupation and activity is encouraged in a manner that demonstrates knowledge of residents’ abilities, likes or dislikes.
-
If activities are personally meaningful, familiar or have some connection with the life history of the group of residents.
-
The role that residents are enabled and supported to adopt in the CH setting (and whether that is an active or passive role), in particular, opportunities for increasing residents’ involvement in domestic-type tasks.
Appendix 2 Report on workstream 2: development and preliminary testing of strategies to enhance routine physical activity in care homes
Aims and objectives
The primary aims and objectives of WS2 were to:
-
review methods of data collection at the level of the residents and CHs
-
evaluate methods and tools to measure PA in this population to inform outcome assessment in a future RCT.
A secondary aim was to review and assess the method of recruiting CH residents to the research study to inform the processes for the feasibility trial in WS5.
Methods/design
The study was divided into two phases:
-
Phase 1 was designed to explore the methods of routinely collecting data in CHs and the content of such data, and to explore the appropriateness of different assessments of physical function and mobility in a CH population.
-
Phase 2 was designed to explore different methods of measuring PA and sedentary behaviour in older CH residents. The methods considered were identified in the development work as having potential among the CH population. Phase 2 comprised two parts. In part one, the criterion validity (compared with direct observation) of estimates of PA and sedentary time in CH residents derived from the ActiGraph accelerometer worn on the hip and wrist was assessed by undertaking an observational study in the CH setting. Part two then examined the feasibility of assessing the PA and sedentary behaviour of CH residents over an extended period using the ActiGraph accelerometer. The APAFOP questionnaire was also evaluated.
Recruitment of care homes
Care homes run by independent providers (private, voluntary or non-profit) in the Bradford area that had expressed an interest in participating were purposively selected for both WS1 and WS2 to reflect differences in size, setting and ownership.
Recruitment of residents
All residents in the participating homes who did not meet the exclusion criteria were eligible.
Residents were excluded if they were acutely unwell, bedbound or near to death (in receipt of palliative care). In addition, residents who, in the opinion of the CH manager, may have found the research distressing were not approached.
The researcher initially liaised with the CH manager to establish which, if any, residents met the exclusion criteria. All eligible residents were then approached for study participation by the researcher following an introduction from a member of the CH staff. The researcher talked informally with the residents to put them at ease and get a feel for whether or not the presence of a member of the CH staff or a familiar face would aid communication. Although the majority of individuals residing in CHs are likely to have some kind of age-related cognitive impairment, it was presumed that, as directed by the Mental Capacity Act 2005,67 residents had the capacity to consent unless it was established that they lacked capacity. If appropriate, the researcher provided the resident with an information leaflet detailing the study and briefly explained what study participation would involve. The researcher assessed capacity to consent by considering whether or not they felt that the resident understood the information they provided about the study, whether or not the resident was able to retain the information and whether or not the resident was capable of making a decision of their own free will.
Potential participants with capacity to consent were given verbal information and a written information sheet about the study. They were given as much time as they required to consider participation and the opportunity to discuss the study with their family and ask questions of the researcher. Residents wishing to participate were asked to sign and date the consent form. When this was not possible, for example because of a physical difficulty, participants were asked to give verbal consent in the presence of a witness (a relative, close friend or staff member from the CH) and this was detailed on the consent form.
Potential participants without capacity to consent were asked if they could identify a PC (i.e. a family member or friend) with whom they were happy for the researcher to discuss their participation in the study. If the resident was unable to identify someone to assist, the CH manager was asked to identify a PC. The researcher also checked with the CH manger whether or not any residents had an advance directive relevant to identifying a PC regarding participation in research in place.
Personal consultees were contacted in writing via the CH. A covering letter outlined the role of a PC. The PC was also provided with the participant information leaflet, along with a consultee declaration form and objection slip (with pre-chosen reasons for declining). PCs were requested to respond within 2 weeks using the pre-paid envelope provided.
According to the original protocol, if there was no response from the potential PC or they were unwilling to take on the role, an individual, independent of the research team, in the CHs was to be asked to act as the NC and advise on the likely views of the resident. However, the CH manager of the first home where recruitment was undertaken was uncomfortable with this procedure. We did not, therefore, further pursue the use of NCs in this phase of the research in any of the CHs.
Data collection
Phase 1: methods of routinely collecting data
The research team collected personal health data for residents participating in the study, including sex, age, date of admission to CH, height, weight, date of birth, primary diagnosis and any secondary comorbidities, critical incidents (including number of falls and soft-tissue injuries in the previous 6 months), hospital admissions (including length of inpatient stay) and number of health professional call-outs/consultations.
The feasibility of using a range of tools, identified as a result of the PDG work and a review of the literature, designed to assess mobility and other outcomes was explored. Specifically, physical function was assessed using the BI, the PAM-RC, functional walking ability (based on the FAC) and the Timed Up and Go Test (TUGT). Cognitive impairment was assessed using the 6-CIT.
Physical function assessments
The Barthel Index of Activities of Daily Living
The BI48,49 assesses functional status on a 21-point scale (scored 0–20) by recording the ability to complete 10 ADL: bathing, bladder function, bowel function, dressing, feeding, grooming, mobility, stairs, toilet use and transfers. Higher scores on the BI indicate greater independence; scores of ≤ 11 indicate dependence on a carer for ADL. 51,110 The BI was completed by the activities co-ordinator or senior care assistant, together with the researcher.
The Physical Activity and Mobility in Residential Care Scale
The recently developed PAM-RC (Dr Julie Whitney, personal communication) is intended to be a simple, valid and reliable scale for assessing mobility and activity levels in aged residential-care residents. It is designed to be completed by residents’ key carers, based on activity levels over the previous week. It involves rating five domains, with a total score range of 0–21: mobility (0–6), balance (0–4), walking frequency (0–4), wandering (0–3) and outdoor mobility (0–4). Higher scores indicate greater independence/engagement in more activity (Table 11). The PAM-RC was generally completed by either the activities co-ordinator or the senior care assistant, together with the researcher.
| Based on usual activities in the previous week . . . | Score |
|---|---|
| Ability | |
| Mobility | |
| Bedbound | 0 |
| Wheelchair bound (transfers with hoist) | 1 |
| Wheelchair bound (standing transfers with assistance) | 2 |
| Wheelchair bound (standing transfers without assistance) | 3 |
| Able to walk short distances within room (< 3 m with/without aids/assistance) | 4 |
| Walks longer distances (> 3 m) using walking aid/assistance/supervision | 5 |
| Walks longer distances (> 3 m) independently | 6 |
| Balance | |
| Immobile | 0 |
| Needs assistance of one or two people to maintain balance | 1 |
| Needs to use walking aid (stick/frame) to maintain balance | 2 |
| Uses no walking aid but unsteady | 3 |
| Uses no walking aid but gait is steady | 4 |
| Activity | |
| Walking frequency | |
| Does not walk at all | 0 |
| Walks in room to help with personal care (i.e. to the toilet or commode) | 1 |
| Walks in the room and around the home when necessary only (toilet/dining area) | 2 |
| Walks around the home more often than for necessary functions, but spends majority of time sitting | 3 |
| Walks around the home more often than for necessary functions, spending only short periods sitting | 4 |
| Wandering | |
| Wandering not exhibited in last 7 days | 0 |
| Wandering occurred 1–3 days out of last 7 | 1 |
| Wandering occurred 4–6 days out of last 7 | 2 |
| Wandering occurred daily | 3 |
| Outdoor mobility | |
| Does not go out (except for hospital appointments) | 0 |
| Only goes out in wheelchair | 1 |
| Goes for short walks (< 50 m) with assistance of carer (i.e. around the garden) | 2 |
| Goes for longer walks (> 50 m) with assistance of carer (i.e. to local shops) | 3 |
| Goes out longer distances (> 50 m) without carers (includes absconding) | 4 |
As the PAM-RC is designed to be completed by carers, it offers an advantage over resident-reported measures because some residential CH residents have difficulties writing or reliably recalling recent activities. However, to date, the PAM-RC has been piloted on only a small sample of older people in residential care; a larger validation study is required. The sensitivity of the scale (to detect changes as a result of an intervention) has not been investigated. Nevertheless, it has been reported to have excellent test–retest reliability, internal consistency and good construct validity (Dr Julie Whitney, personal communication).
In Dr Whitney’s research, the PAM-RC scale was found to be highly correlated with PA measured using activity monitors and to other measures of physical performance, including strength, gait and balance.
Functional walking ability
Functional walking ability was based on the FAC,50 which categorises individuals according to basic motor skills necessary for functional ambulation. Each level of the FAC (0–5) relates to a graded ambulation description, with 0 being ‘unable to ambulate’ and 5 being ‘independent in ambulation’.
In consultation with the CH staff (usually the activities co-ordinator or senior care assistant), each resident’s level of functional walking ability was categorised into four groups: 0, non-ambulatory (unable to walk) (FAC score of 0), 1, low ability (unable to walk without assistance of two people) (FAC score of 0), 2, medium ability (walks with assistance/supervision of one person) (FAC scores of 1–3) and 3, high ability (able to walk fully independently) (FAC scores of 4 or 5).
Timed Up and Go Test
The TUGT111 is a general physical performance test to assess mobility, balance and locomotor performance. It is a short, timed task specifically designed for elderly people; it involves an individual standing up from a chair, walking 3 m, turning around, walking back to the chair and sitting down. Participants are instructed to perform the complete procedure as quickly and as safely as possible, and the time taken to perform the task is recorded from being instructed to perform the manoeuvre until returning to a safely seated position.
Cognitive assessment
The Six-item Cognitive Impairment Test
The 6-CIT47 was developed by regression analysis of the Blessed Information–Memory–Concentration Test. 112 The 6-CIT correlates well with the Mini Mental State Examination,113 which is often considered the ‘gold-standard’ cognitive impairment test. It therefore can be considered a valid measure of cognitive impairment. 47 The 6-CIT comprises six questions that are weighted to produce a total score out of 28. An inverse scoring system is used, with scores of 0–7 considered normal and scores of ≥ 8 considered indicative of cognitive impairment. This 7/8 cut-off point has produced sensitivity and specificity scores of 90% and 100%, respectively. 47 A researcher verbally administered the 6-CIT to each resident.
Phase 2: assessment of physical activity
The aim of this phase of the WS was to explore different methods of measuring PA and sedentary behaviour in older CH residents. The feasibility of data collection and validity of the data collected using accelerometers and the APAFOP questionnaire was considered. Further details on each of these measures are provided in the following sections.
ActiGraph accelerometer
Accelerometers are electronic sensors that measure the acceleration of an object along reference axes. 114 Acceleration is proportional to external force; thus, the accelerometer reflects the intensity and frequency of human movement. 115
The outputs generated from the ActiGraph accelerometer are referred to as ‘activity counts’. Activity counts are proprietary units that reflect raw accelerations that have undergone some data processing and have been summed over a user-defined discrete time period (epoch). 116 The sum of the activity counts in a given epoch is related to activity intensity and may be categorised based on validated activity count cut-off points. 117,118 Using ActiLife software, it is then possible to apply algorithms to classify how long individuals spend sedentary and engaging in PA of different intensities, and to calculate energy expenditure estimates.
Accelerometers were worn on the wrist (attached by a strap) or on an elasticated belt around the waist (positioned above the hip). We used the ActiGraph GT3X+ model accelerometer for the study.
Assessment of Physical Activity in Frail Older People
The APAFOP is a PA questionnaire that has been purposely developed for and tested for reliability with older people with and without cognitive impairment. 46 It is administered verbally by a researcher with the interviewee, who is asked to recall activities undertaken in the previous 24 hours, with a focus on ADL.
Observational study: exploration of the criterion validity of estimates of physical activity and sedentary time derived from hip- and wrist-worn accelerometers
Accelerometer wear location is an important methodological consideration when using these devices, as the activity counts recorded are likely to differ markedly dependent on where the accelerometer is worn on the body. 119 Yet guidance on how to interpret activity counts recorded by an accelerometer worn on a location other than the hip in a meaningful way is limited. Nonetheless, wrist-worn accelerometers are increasingly being used in large-scale epidemiological studies in the light of reports of improved compliance, compared with a hip-worn monitor. 120 Furthermore, there is some evidence to suggest that an accelerometer worn on the wrist rather than the hip may be better suited to measuring the PA of frail older adults, as it can capture upper body movements typical of non-ambulatory activities (e.g. ADL, such as dressing) and the influence of atypical gait patterns is likely to be minimised. 60 However, to date, there is a paucity of studies comparing the outputs derived from hip- and wrist-worn accelerometers among older adults. Furthermore, no studies have assessed agreement with a criterion measure. Therefore, it is not possible to make inferences about which wear location results in the most valid measure of PA in this population.
The aims of this observational study were to:
-
use observations of residents’ activities as a reference to compare with data captured by accelerometers to assess the validity of using accelerometers in a frail, elderly and largely inactive population
-
identify whether an accelerometer worn on the hip or an accelerometer worn on the wrist was the most accurate in recording the types of activities in which frail, older adult residents in CHs typically engage.
Residents who had been recruited to WS2 were approached in the communal areas of the CHs and asked whether or not they would be prepared to participate in the observational study. Residents were invited to wear a hip-worn and/or wrist-worn accelerometer over a 2-hour ‘free-living’ period while being observed by the researcher.
The researcher used a predetermined list of activities to record systematically every 15 seconds what they observed participants doing over the monitoring period. The list of activities included both sedentary behaviours and PAs that were thought to be typical of CH residents. Any additional details that would facilitate the accurate classification of activities during analysis were also noted. For example, if a participant was observed walking, a note was made regarding walking speed. The time the 2-hour monitoring period started was documented to ensure appropriate data comparisons could be made across the two recording methods.
Feasibility study: use of accelerometers to assess physical activity over extended periods
Participants in habitual PA studies are typically asked to wear an accelerometer during all waking hours over a 7-day period. 121 However, compliance with this requirement is variable. Consequently, studies typically require participants to have met a prespecified wear-time criterion in an effort to ensure that estimates of PA and sedentary behaviour are reliable. While numerous wear-time criteria are reported in the literature, these are typically derived from studies among younger adults and empirical evidence supporting the superiority of a specific criterion is absent. 122 Nevertheless, in studies involving community-dwelling older adults, a wear-time criterion of at least 8 hours per day on at least 4 days is often required for inclusion in analysis. 52,53
In addition, given that the use of questionnaires remains an attractive method to measure PA, recent efforts have also been directed at developing questionnaires appropriate to old-old CH residents (i.e. those aged ≥ 85 years).
Thus, the aims of this feasibility study were to:
-
investigate both the practical feasibility of using accelerometers and the appropriateness of the aforementioned wear criteria in older CH residents
-
describe the levels of PA and sedentary behaviour
-
explore the use of a PA questionnaire (APAFOP).
All recruited residents in the participating CHs were invited to wear an accelerometer around the hip for a period of up to 10 days, while they continued with their usual routine.
During the wear period, it was requested that a daily log of wear time (i.e. the time the monitor was put on and removed) was kept. The ‘activity log’ also included a column for recording the reason(s) the monitor was removed (e.g. for showering). Residents capable of completing the log and putting the accelerometer on themselves were encouraged to do so, although the process of completing the activity log was also explained to staff and they were asked to offer support with this, when appropriate. The arrangements for completing the activity logs were discussed with the CH managers in each home prior to the monitors being administered.
Following the collection of the accelerometers, the APAFOP questionnaire was trialled.
Data analysis
All data were assessed for normality of distribution visually (using histograms) and using the Shapiro–Wilk test. When data were non-normally distributed, data were log-transformed to permit the use of parametric statistics. Alternatively, if log transformation was not appropriate or did not result in a normal distribution of data, non-parametric statistics were utilised. Data are presented as mean ± SD, unless otherwise specified, and alpha was accepted as p < 0.05.
Phase 1: methods of routinely collecting data
Descriptive statistics [medians, interquartile ranges (IQRs) and ranges] were utilised to describe the outcomes. Participants were grouped according to age (< 85 years or ≥ 85 years), sex (male or female), functional walking ability (score of 0–1 or 2–3), physical function [BI score of ≤ 11 (dependent) or > 11 (independent)] and level of cognitive impairment (6-CIT score of < 8 or ≥ 8). Differences between groups were assessed using a series of one-way analyses of variance (ANOVAs) or Kruskal–Wallis tests, as appropriate.
Phase 2: assessment of physical activity and sedentary behaviour
Observational study: exploration of the criterion validity of estimates of physical activity and sedentary time derived from hip- and wrist-worn accelerometers in older care home residents
To enable direct comparison between counts recorded by the hip and wrist accelerometers, all four counts recorded by the wrist accelerometer were adjusted according to the recommendations of the manufacturer (Table 12). These adjusted wrist counts were used in all analyses.
| Wrist count | Equivalent counts |
|---|---|
| 0 | 0 |
| 0–644 | 0.5341614 × wrist count |
| 645–1272 | (1.7133758 × wrist count) – 759.414013 |
| 1273–3806 | (0.3997632 × wrist count) + 911.501184 |
| ≥ 3807 | (0.0128995 × wrist count) + 2383.904505 |
To align with the observational data, each of the accelerometer data sets was reviewed alongside the observational tool. Equivalent epochs for which participants were unavailable for observation (either because the participant was out of a communal area or because the observer was unavailable) were manually removed.
On the predetermined list of activities used systematically to record what participants were doing, activities were categorised as either sedentary behaviour or PA, based on metabolic equivalent of task (MET) values assigned to the same (or similar) activity in the Compendium of Physical Activities124 (Table 13). Thus, each observation was coded as either sedentary behaviour or PA.
| Sedentary behaviour | PA |
|---|---|
| Active social interaction (e.g. talking with others) | Low-intensity PA (e.g. craft activities) |
| Passive social interaction (e.g. listening or watching others) | Light-intensity PA (e.g. moving to music, clapping) |
| Eating and/or drinking | Moderate to vigorous PA (e.g. performing exercises) |
| Sedentary activities (e.g. reading, watching television) | Walking (with or without aid) |
| Wheelchair transference | Sit-to-stand transfer |
| Receiving care | Stand-to-sit transfer |
| Socially or recreationally inactive (i.e. no engagement in any activity) | Standing still |
| Sleeping/dozing |
Next, to enable direct comparison with observational data, accelerometer counts were coded as either sedentary behaviour (i.e. < 10 counts) or PA (≥ 10 counts). These cut-off points were developed in a sample of 37 community-dwelling older adults aged ≥ 65 years. 125
The agreement between the categorisation of sedentary behaviour and PA derived from the observational data and the accelerometer data was evaluated. Specifically, sensitivity, PV, overall agreement (Equations 1–3) and the kappa statistic were calculated:
With regard to sensitivity, PV and overall agreement, values close to 100% were deemed indicative of good agreement between the observational and accelerometer data, whereas a value close to zero suggested that the estimated time spent engaging in PA and sedentary behaviour, as categorised by the accelerometer data, was very different from that derived from the observational data. In line with recommendations from Landis and Koch,57 the kappa statistic was interpreted as follows: a value of between 0 and 0.2 was indicative of slight agreement, between 0.2 and 0.4 indicated fair agreement, between 0.4 and 0.6 indicated moderate agreement, between 0.6 and 0.8 indicated substantial agreement and between 0.8 and 1.0 indicated almost perfect agreement.
Feasibility study: use of accelerometers to assess physical activity over extended periods
Raw activity count data collected by the accelerometers were downloaded, processed with the normal filter and aggregated over 60-second epochs using the ActiLife software (version 6.8.0). Activity counts recorded in the vertical axis were used for analysis.
To reduce the risk of distorting data provided by the least active residents,126 all data were manually screened alongside the activity logs, and periods of non-wear time were removed. Daily wear time was determined by subtracting non-wear time from total possible minutes in a day (1440 minutes). Valid accelerometer wear time for this sample was identified as ≥ 8 hours on ≥ 4 days of the week.
Next, cut-off points, which had previously been applied to data collected in a sample of CH residents,24 were applied to the vertical axis accelerometer cpm to identify time spent engaging in sedentary behaviour (< 100 cpm),76,127 low-intensity PA (100–759 cpm), light-intensity PA (760–2019 cpm) and moderate to vigorous intensity PA (≥ 2020 cpm). 76,128 The data for each of these separate PA outcomes were also converted into a percentage of daily wear time to account for intraindividual and interindividual differences in daily wear time. 129
To facilitate discussion around the patterns of sedentary behaviour and PA, the number and length of ‘bouts’ of sedentary behaviour and PA were calculated. Specifically, a bout of sedentary behaviour was defined as a period of at least 30 minutes up to 59 minutes, or at least 60 consecutive minutes, and a bout of PA was defined as a period of at least 10 consecutive minutes of activity. The total amount of sedentary and PA time accumulated in bouts was also calculated.
Differences in the demographic characteristics and physical function of the following groups of participants were compared using a series of one-way ANOVAs or Kruskal–Wallis tests, as appropriate. First, those residents who agreed to wear a hip-worn accelerometer were compared with those who did not. Second, those participants wearing a hip-worn accelerometer and who provided valid data were compared with those participants wearing a hip-worn accelerometer who did not provide valid data.
Descriptive statistics (medians, IQRs and ranges) were used to describe the levels of sedentary behaviour and PA. Next, to explore the effect of personal characteristics on levels of PA and sedentary behaviour, participants were grouped according to age (< 85 years or ≥ 85 years), sex (male or female), functional walking ability (score of 0–1 or 2–3), physical function [BI score of ≤ 11 (dependent) or > 11 (independent)] and level of cognitive impairment (6-CIT score of < 8 or ≥ 8). Differences between the groups were assessed using a series of one-way ANOVAs or Kruskal–Wallis tests, as appropriate.
Results
Recruitment of care homes
Four CHs were selected and recruited over 4 months, from June 2013 to September 2013, to participate in both WS1 and WS2. An additional two CHs were recruited in November 2013 for WS2, to assess the appropriateness of PA measures, as resident recruitment was lower than anticipated in the originally recruited four CHs.
Four CHs offered residential care (one specialised in dementia care) and two offered CHs with nursing. One was run by the local authority, three by private or family companies, one by a national company and one by a large international company. Sizes ranged from 20 to 55 beds. One CH was situated in an inner city; the others were in semiurban, semirural or rural locations.
Table 14 summarises the characteristics of participating CHs.
| Characteristic | Description |
|---|---|
| CH1 | |
| Pseudonym (WS1) | Rowntree |
| Organisational context |
|
| Environment | Two-storey facility (occupied by residents on two floors); communal lounge located on each floor |
| People | Approximately 25 residents were observed. Physical mobility was generally poor, with only eight of the residents observed able to fully self-mobilise (the rest required use of wheelchairs, walking frames or some other assistance). Cognitive capacity was poor, with only a dozen or so residents having strong mental capacity |
| Daily routine | Residents generally extremely sedentary (spending most of their time in a seated position). |
| PA | Formal activities took place in the post-lunch period from 14.00–15.00, with occasional late-morning activities. Most activities were social rather than physical, and usually orientated around music. Chair exercises were organised on a fortnightly basis |
| CH2 | |
| Pseudonym (WS1) | Eden Park |
| Organisational context |
|
| Environment | Two-storey facility; two communal lounges located on the lower level and three located on the upper level. Residents’ bedrooms located on both levels |
| People |
|
| Daily routine | Movement revolved around the three main meals, before which, residents are assisted to the toilet. Staff helped residents who were moderately impaired to walk to the dining rooms, while able-bodied and mobile residents walked on their own. After each daytime meal, frail and otherwise immobile residents were transferred to an upstairs lounge; after the evening meal, they were taken straight to bed. Most residents were in their rooms by 18.30. Residents who were not bedridden/wheelchair bound/frail generally sat sedentarily in the lower-level lounges. Those who were more mobile wandered in and out of the lounges and garden. A few residents arranged trips to local shops, theatres and museums. On warm days, a few residents gardened and spent much of the day outside. Care assistants often assisted residents to walk around |
| PA | The post of activity co-ordinator was vacant. A ‘Music for Health and Well-being’ class was offered twice a week (only 8–10 residents with good cognitive capacity attended this class). Light exercises were provided one Friday evening a month |
| CH3 | |
| Pseudonym (WS1) | Bournville |
| Organisational context |
|
| Environment | Three-storey facility (occupied by residents on two floors); residents’ rooms interspersed with some communal bathrooms (although most rooms are en suite). Two communal lounges located on the ground floor |
| People | Most residents had very poor physical capacity. The majority of residents had stronger levels of cognitive function, and could maintain simple conversation; a small number of residents had very poor mental capacity |
| Daily routine | Between breakfast and lunchtime at 12.30, and then until teatime (about 17.00), residents spent most of their time sitting idle and bored |
| PA | An activities co-ordinator was in post; however, few activities were provided. Informal activities involved residents going for short walks outside during fine weather (but this was infrequent) |
| CH4 | |
| Pseudonym (WS1) | Hebble House |
| Organisational context |
|
| Environment | Two-storey facility dived into four wings (two downstairs and two upstairs), with a lounge area in each wing |
| People | Housing both permanent and short-stay residents, the majority of whom had moderate dementia, or were in the later stages of dementia. Great variation in physical capacity; several residents independently mobile |
| Daily routine | Generally, residents were very sedentary and spent much of the day sitting. In between meals, residents were encouraged to sit in the lounge areas. A small number of residents who were independently mobile walked around the CH and sat for short periods of time in different lounges (approximately five residents routinely moved about the home). Residents who smoked spent some of their day walking to/from the outside smoking area. One resident occasionally helped out with the running of the home by washing dishes and setting the table (which was encouraged and facilitated by staff). A few residents spent time in their rooms; however, this was discouraged by staff (except if residents were ill). Some residents went outside in warm weather. The majority of staff encouraged and supported residents to mobilise as much as possible when moving around the CH |
| PA | The activity co-ordinator was on maternity leave. An organised class ran once a fortnight, which consisted of mainly seated activities. When staff had time, they engaged residents in spontaneous activities, which included encouraging residents to move/dance to music |
| CH5 | |
| Pseudonym (WS1) | Not applicable |
| Organisational context |
|
| Environment |
|
| People |
|
| Daily routine |
|
| PA | The home employs a full-time activities co-ordinator, who organises quizzes, bingo, gardening, sewing, reminiscence work, musical events involving physical movement and other similar activities throughout the week. There are also other activities at certain times, such as a party for the Queen’s Jubilee, in which all residents come together. Generally, activities are delivered to residents on one floor during the morning, and then to the second group of residents in the afternoon |
| CH6 (taken from website) | |
| Pseudonym (WS1) | Not applicable |
| Organisational context |
|
| Environment |
|
| People | |
| Daily routine | Communal areas are spacious and light; it is here that residents often spend time together, with a choice of bustling or quiet lounges, ideal for personal gatherings with family or friends |
| PA | The activity co-ordinator supports the individual interests and hobbies of the residents, providing a full calendar of events and plans that residents can get involved in and look forward to |
Recruitment of participants
There were 220 residents in the six participating CHs (mean number of residents per CH 37, range 23–55). Forty-three (19.5%) residents who did not have mental capacity in one of the CHs were not put forward for the study by the CH manager. Twenty-six (11.8%) residents were ineligible. Reasons for ineligibility were as follows: acutely unwell (n = 14), permanently bedbound/cared for in bed (n = 3), having had a recent fall or operation (n = 2), not a permanent resident (n = 1), in hospital during the period of recruitment (n = 3) and other (n = 3). Thus, a total of 151 (68.6%) of the 220 residents were eligible to participate. Figure 12 shows the flow of participants through the recruitment process.
FIGURE 12.
Flow of participants through the recruitment process.
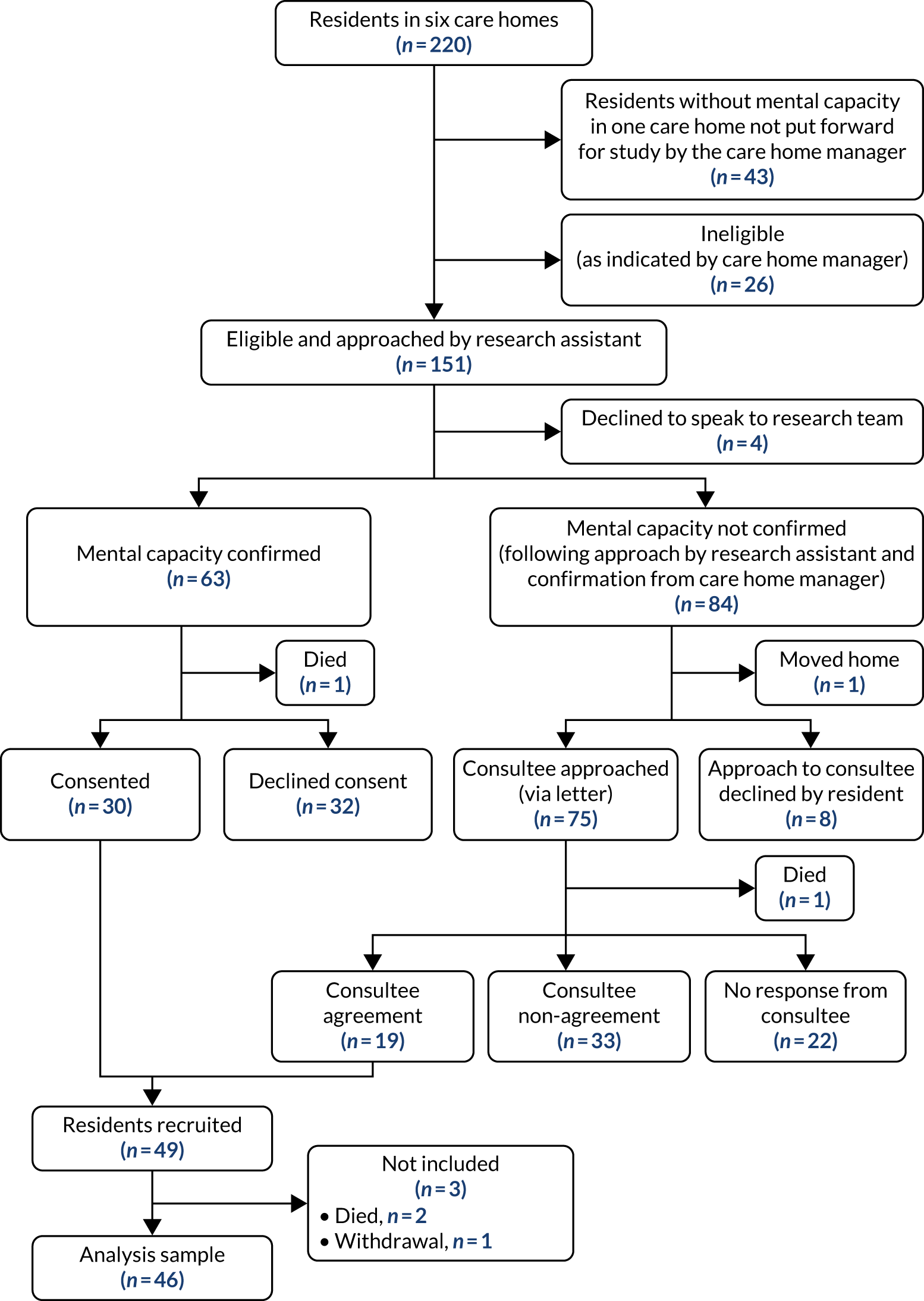
Sixty-three (41.7%) of the 151 eligible residents had capacity to consent, 84 (55.6%) did not have capacity to consent and four (2.6%) refused to speak to the researcher. Thirty (47.6%) of the 63 residents with capacity consented and 32 (50.8%) refused [one (1.6%) resident died]. The most common reason given by residents for not wanting to participate was that they did not want to be involved in research [n = 14 (43.8%)]. Other reasons residents gave were as follows: they did not think that they could be useful [n = 3 (9.4%)], a recent fall [n = 2 (6.3%)], depression [n = 1 (3.1%)], they felt that it would be too burdensome for staff [n = 1 (3.1%)] and they felt that they had ‘too much going on’ [n = 1 (3.1%)]. The remaining 10 (31.3%) residents did not give a reason for not wishing to participate.
Seventy-five PCs of the 84 eligible residents who did not have capacity to consent were sent a letter requesting their agreement for their relative/friend to participate in the study. Eight (9.5%) residents refused permission for researchers to approach a PC (see Figure 12), with two residents stating that this was because they would not like to wear an activity monitor and one resident having moved to another CH. Nineteen (25.3%) PCs agreed to participation, 33 (44.0%) declined and there was no response from 22 (29.3%) PCs. Reasons for declining agreement are shown in Table 15.
| Reason | n | % |
|---|---|---|
| Relative/friend would not choose to participate | 16 | 32.7 |
| Resident not well enough | 15 | 30.6 |
| Resident’s lack of comprehension/resident unable to converse (dementia) | 6 | 12.2 |
| Resident’s anxiety/worry/agitation/confusion | 5 | 10.2 |
| Resident not mobile/inactive | 4 | 8.2 |
| Resident unable to converse (deaf/suffered stroke) | 1 | 2.0 |
| Unable to comply with protocol/participate in previous research | 1 | 2.0 |
| No reason given | 1 | 2.0 |
| Total | 49a | 100 |
In total, therefore, 49 residents were recruited: 30 consented and the PCs of a further 19 residents agreed to participation. Of these 49 participating residents, two died and one withdrew before data collection. Thus, 46 residents contributed to data collection in phase 1. Unfortunately, a further participant died during data collection. In phase 2, nine residents took part in the observational study and 41 took part in the feasibility study.
Participant characteristics
Sixty-seven per cent of participants were female and 55% were aged ≥ 85 years. Participant characteristics are shown in Table 16.
| Participant characteristics | N | n (%), mean ± SD or median (IQR) |
|---|---|---|
| Sex (female) | 46 | 31 (67) |
| Age (years) | 44 | 85 ± 8 |
| Age group (years) | 44 | |
| < 85 | 20 (45) | |
| ≥ 85 | 24 (55) | |
| Length of residence in CH (months) | 45 | 15 (8–29) |
| Height (cm) | 35 | 164.8 ± 9.7 |
| Weight (kg) | 45 | 67.9 ± 12.8 |
| BMI (kg/m2) | 35 | 25.2 ± 4.4 |
| Capacity to consent | 46 | 29 (63) |
| Primary diagnosisa | 37 | |
| Dementia | 16 (43.2) | |
| Stroke/TIA | 11 (29.7) | |
| Heart conditions | 4 (10.8) | |
| Respiratory conditions | 4 (10.8) | |
| Urinary tract infections | 4 (10.8) | |
| Otherb | 20 (54.1) | |
| In the previous 6 months | ||
| Fall | 37 | 14 (37.8) |
| Soft-tissue injury | 35 | 9 (25.7) |
| Routine GP consultations | 37 | 31 (83.8) |
| Unplanned GP consultations | 37 | 23 (62.6) |
| Nurse visits | 37 | 16 (43.2) |
| Unplanned hospital admissions | 37 | 5 (13.5) |
Phase 1: outcome measures
Barthel Index
The BI was completed by researchers in collaboration with the CH staff for all 46 residents participating in phase 1. The mean score was 12 (SD 5) points and the median score was 12 points (IQR 7–16; range 2–20 points). Nineteen (41%) of the residents had a score of ≤ 11, indicating dependence in ADL.
The Physical Activity and Mobility in Residential Care Scale
The PAM-RC was completed by a member of the CH staff for all 46 participants. PAM-RC scores are shown in Table 17.
| PAM-RC | Score | |
|---|---|---|
| Median | IQR | |
| Ability | ||
| Mobility (≥ 4: ambulatory) | 4 | 1–6 |
| Balance (≥ 3: walks without aid) | 2 | 0–4 |
| Activity | ||
| Walking frequency (≥ 3: walks more than necessary) | 2 | 0–4 |
| Wandering (≥ 1: wanders) | 0 | 0–3 |
| Outdoor mobility (≥ 2: goes out and walks) | 1 | 0–4 |
| Total score | 9 | 1–19 |
There were only small differences between mobility assessment scores according to age and sex, as shown in Table 18.
| Mobility assessment | Age (years) (N = 44) | Sex (N = 46) | ||
|---|---|---|---|---|
| < 85 (n = 20) | ≥ 85 (n = 24) | Male (n = 15) | Female (n = 31) | |
| BI score (n = 46) | 12 ± 6 | 12 ± 5 | 12 ± 6 | 11 ± 5 |
| PAM-RC score (n = 46) | 11 ± 6 | 9 ± 6 | 12 ± 6 | 10 ± 6 |
Functional walking ability
Functional walking ability was completed by CH staff for all 46 residents. Twelve (26.1%) residents were categorised as non-ambulatory; three (6.5%) were categorised as being of low ability; 12 (26.1%) as of medium ability; and 19 (41.3%) as of high ability.
The Timed Up and Go test
The TUGT was not implemented in the CHs as more than one-quarter of participants were immobile, and were thus unable to undertake the test. In addition, there were concerns expressed by CH managers about the safety of frail residents with limited or poor mobility being able to undertake the test safely, and there were worries about the risks and consequences of falls.
The Six-item Cognitive Impairment Test
The 6-CIT was attempted by 36 (78.3%) of the 46 participating residents. Thirty-one residents completed and five partly completed the test. The five residents who did not complete the test expressed difficulties maintaining concentration, fatigue or a lack of desire to participate, hence the lower completion rate.
Twenty-two (71.0%) of the 31 residents who completed the test had a score of ≥ 8, indicating significant cognitive impairment.
Phase 2: assessment of physical activity
Observational study: exploration of the criterion validity of estimates of physical activity and sedentary time derived from hip- and wrist-worn accelerometers in older care home residents
Nine residents previously recruited to WS2 agreed to participate in the observational study. Twelve separate observations were undertaken on these nine residents: seven observations were undertaken on residents wearing an accelerometer on the hip; a further two observations were undertaken with two of those seven residents while they wore an accelerometer on the wrist; two observations were undertaken on residents wearing an accelerometer on the wrist; and one further observation was also undertaken on one of these two residents while they wore an accelerometer on both the hip and the wrist. Therefore, the total number of observations of accelerometers were as follows: hip, n = 8; and wrist, n = 5. Unfortunately, two of the wrist accelerometers malfunctioned, meaning that data were available to analyse for eight hip-placed accelerometers and three wrist-placed accelerometers. A total of 19 hours and 43 minutes of activity were available for analysis, with a mean of 1 hour 48 minutes per participant.
Sensitivity, PV, overall agreement and kappa statistics are presented in Table 1. The sensitivity for sedentary time and PV for PA was higher for the hip counts than for the wrist counts. Conversely, the sensitivity for PA time and PV for sedentary behaviour was higher for the wrist than for the hip counts. Overall agreement was better for the hip data than for those collected by the wrist-worn accelerometer. The kappa statistic indicated that the agreement for hip counts was moderate, whereas the agreement for the wrist counts was slight. However, these results must be treated with some caution because of the limited sample size.
Feasibility study: use of accelerometers to assess physical activity over extended periods
The feasibility study was conducted in only five CHs, as it included residents who wore a hip-worn accelerometer only. No residents from CH1 wore a hip monitor for an extended period.
Practical feasibility of using accelerometers
Forty-one (89.1%) of the 46 recruited residents available for the phase 2 study undertook extended wear of an accelerometer. Four residents were deemed too unwell to participate and one resident refused to wear the accelerometer.
A hip-worn accelerometer was administered to 30 (73.2%) participants and, at the request of the research leads in two of the CHs, a wrist-worn accelerometer was administered to 10 (24.4%) participants. The reason for requesting residents to wear wrist-worn accelerometers rather than hip-worn accelerometers was that the CH managers felt that wrist-worn accelerometers would be more appropriate for their frail residents. In addition, one resident was asked to wear a commercially available device so that we could explore the data collected by this device.
There were no significant differences in the personal characteristics of those participants who were fitted with a hip-worn accelerometer and those who were fitted with a wrist-worn accelerometer (p > 0.05). However, those participants who wore a hip-worn accelerometer had higher BI scores than those participants who wore a wrist-worn accelerometer [mean BI scores: 13 (SD 5) and 9 (SD 6) respectively; p < 0.05].
Although wrist-worn accelerometers are increasingly being used in large-scale studies as a result of reports of improved compliance of wrist-worn accelerometers, compared with hip-worn accelerometers, there is a paucity of studies comparing the outputs derived from hip- and wrist-worn accelerometers among older adults. The results of the observation study outlined above suggested that data collected from a hip-worn accelerometer had better validity than wrist data in this population. Furthermore, there is limited guidance available on how best to interpret data collected from a wrist-worn accelerometer. Consequently, the decision was taken not to further analyse the wrist data collected in this study.
Twenty-two of the 30 participants who wore an accelerometer on the hip met the criteria for valid accelerometer data: two monitors were lost and six residents did not meet the criteria for valid wear time (≥ 8 hours on ≥ 4 days of the week). All of these six residents wore the monitor for < 4 days. Participant distress and/or confusion and the accelerometer interfering with the provision of care were the most common reasons provided to explain the removal of accelerometers over the monitoring period. There were no differences in the personal characteristics (sex, age, length of residence, height, weight, mental capacity, total BI score) of the 22 participants who met the criteria for valid accelerometer data and the eight who did not (p > 0.05).
Completion of the activity logs
Eight (19.5%) of the 41 activity logs distributed with the accelerometers were fully completed for the period of time the activity monitors were in the residents’ possession (range 3–9 days); 20 (48.8%) were partially completed and 13 (31.7%) were not completed at all.
A designated individual in most of the homes, usually the activity co-ordinator, was asked by the CH manager to assist in the completion of the activity logs. However, in practice, the researcher completed 25 (89.3%) of the logs, either alone [n = 13 (46.4%)] or with the assistance of CH staff [n = 12 (42.9%)]. Only three (10.7%) of the logs were completed by the residents (Table 19).
| Individual(s) | n (%) |
|---|---|
| Researcher | 13 (46.4) |
| Staff and researcher | 12 (42.9) |
| Resident | 3 (10.7) |
| Staff | 0 (0.0) |
| Total | 28 (100.0) |
Accelerometer wear
Of the 22 participants with valid accelerometer data, accelerometers were worn for a mean of 6 days. Eight (36%) residents had 7 valid days, two (9%) residents had 6 valid days, three (14%) residents had 5 valid days and nine (41%) residents had 4 valid days. Mean daily wear time was 12 hours 24 minutes (SD 2 hours 36 minutes). Details regarding the daily wear time at each of the five CHs is displayed in Table 2.
Levels of sedentary behaviour and physical activity
Sedentary behaviour
The mean daily time spent sedentary was 11 hours 11 minutes (SD 2 hours 21 minutes) (see Table 3). This equates to 90.5% (SD 8.3%) of accelerometer wear time (see Figure 3). Except for the single resident in CH3 who spent 82% of their time sedentary, there were only small variations in the percentage of time spent in different activity levels across participating CHs (88–93%).
A considerable proportion of the time spent engaging in sedentary behaviour was accumulated in bouts of 30–59 minutes (19.3%) and ≥ 60 minutes (19.0%). All residents engaged in at least one 30- to 59-minute bout of sedentary behaviour daily over the course of the measurement period. The mean number of daily sedentary bouts of 30–59 minutes’ duration was 3 (SD 2) and each bout lasted, on average, 42 minutes (SD 9 minutes). Twenty (91%) of participating residents engaged in at least one bout of sedentary behaviour of ≥ 60 minutes over the course of the measurement period, with seven (32%) residents engaging in at least one sedentary bout of ≥ 60 minutes daily. The mean number of daily sedentary bouts of ≥ 60 minutes was 1 (SD 1) and each bout lasted, on average, 1 hour 40 minutes.
Physical activity
The mean daily time spent engaging in PA was 1 hour 13 minutes (SD 1 hour 8 minutes) (see Table 3), which equated to 9.5% (SD 8.3%) of accelerometer wear time (see Figure 3). The majority of time engaging in PA was spent in low-intensity PA [8.7% (SD 7.7%) of wear time], with mean daily time in low-intensity PA being 1 hour 7 minutes (SD 1 hour 4 minutes).
Eight residents (36%) did engage in at least 30 minutes of low-intensity PA daily. Only one resident accumulated this time in bouts of at least 10 minutes, although 15 (68%) residents did perform at least one bout (i.e. ≥ 10 minutes) of low-intensity PA over the course of the measurement period, with three (14%) residents performing at least one bout daily.
Overall, residents spent only 5 minutes (SD 7 minutes) engaging in light PA and 1 minute (SD 1 minute) engaging in moderate to vigorous PA [equivalent to 0.7% (SD 0.9%) and 0.1% (SD 0.2%) of wear time, respectively] (see Table 3).
Residents in CHs 2, 3 and 6 spent a greater proportion of their time engaging in PA than residents in the other two homes. Still, the greatest difference was observed between the time spent engaging in low-intensity PA and the very little time being spent engaging in higher-intensity PA.
None of the residents engaged in any bouts of ≥ 10 minutes of either light or moderate to vigorous PA over the measurement period. Nonetheless, just over half [n = 12 (55%)] of the residents did manage to engage in some (i.e. at least 1 minute) light PA daily and three (14%) residents accumulated at least 5 minutes of light-intensity PA daily over the course of the measurement period. Furthermore, eight residents (36%) performed at least one light-intensity PA bout of at least 5 minutes’ duration, and one resident did perform a single moderate to vigorous PA bout of at least 5 minutes over the course of the measurement period.
Table 20 shows the percentage of wear time for sedentary behaviour and PA behaviour across the days of the week. Although the proportion of wear time spent sedentary was a little higher on Saturday and Sunday (91.7% and 93.6%, respectively) than on weekdays (88.5–90.4%), this trend did not reach statistical significance (p > 0.05).
| Day | Wear time (%) | |
|---|---|---|
| Sedentary behaviour | Combined total PA categories | |
| Monday | 88.5 | 11.5 |
| Tuesday | 88.5 | 11.5 |
| Wednesday | 90.1 | 9.9 |
| Thursday | 90.4 | 9.6 |
| Friday | 90.3 | 9.7 |
| Saturday | 91.7 | 8.3 |
| Sunday | 93.6 | 6.4 |
Patterns of sedentary behaviour and physical activity
As discussed previously, residents spent the majority of their time engaging in sedentary behaviours and the little PA they did engage in was predominantly of low intensity. Figures 5 and 6 provide further information on the patterns of sedentary behaviour and PA across a ‘typical day’. Although Figures 5 and 6 represent the patterns of movement of two residents from a single CH (CH5), these two patterns of activity were ‘typical’ of the residents wearing the accelerometers across all of the CHs.
As can be seen in Figure 5, this resident spent the majority of his time sedentary, and the little PA that he did engage in was associated with self-care activities (getting out of bed and dressed in the morning and getting ready for bed in the evening). Conversely, the resident in Figure 6 engaged in more PA throughout the day and actually managed to accumulate continuous ‘bouts’ of at least 10 minutes of low-intensity PA. Based on observational data, the main form of regular movement observed in all the CHs generally involved accessing the toilet or moving to a different location for meals/organised activities.
Relationships between sedentary behaviour and physical activity and age, sex, physical function and cognitive ability
The differences between groups (e.g. age, sex) in the time and percentage of time spent in sedentary behaviour and PA are shown in Table 21. As can be seen from the table, there were no significant differences in the time spent engaging in sedentary behaviour or PA of any intensity between those aged < 85 and those aged ≥ 85 years, or between males and females (p > 0.05). Similarly, no differences in sedentary behaviour or PA were observed between those participants categorised as having a significant score on the 6-CIT (≥ 8) (i.e. higher level of cognitive impairment) and those who did not (6-CIT score of < 8).
| Group and PA category | Time | Percentage of time | ||||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Age (years) | < 85 (n = 11) | ≥ 85 (n = 11) | < 85 (n = 11) | ≥ 85 (n = 11) | ||||
| Sedentary | 11 h 2 min | 1 h 40 min | 11 h 5 min | 1 h 41 min | 91.4 | 4.5 | 90.9 | 6.4 |
| Low-intensity PA | 0 h 54 min | 0 h 47 min | 1 h 10 min | 1 h 3 min | 7.7 | 7.0 | 8.6 | 6.2 |
| Light-intensity PA | 0 h 6 min | 0 h 5 min | 0 h 4 min | 0 h 3 min | 0.8 | 0.9 | 0.6 | 0.5 |
| Moderate to vigorous PA | 0 h 1 min | 0 h 1 min | 0 h 1 min | 0 h 1 min | Negligible | Negligible | Negligible | Negligible |
| Sex | Male (n = 8) | Female (n = 14) | Male (n = 8) | Female (n = 14) | ||||
| Sedentary | 10 h 38 min | 1 h 39 min | 11 h 18 min | 1 h 38 min | 90.6 | 9.5 | 91.4 | 5.1 |
| Low-intensity PA | 1 h 7 min | 1 h 16 min | 0 h 59 min | 0 h 41 min | 9.0 | 9.2 | 7.7 | 4.6 |
| Light-intensity PA | 0 h 3 min | 0 h 3 min | 0 h 6 min | 0 h 4 min | 0.5 | 0.8 | 0.8 | 0.7 |
| Moderate to vigorous PA | 0 h 0 min | 0 h 0 min | 0 h 1 min | 0 h 1 min | Negligible | Negligible | Negligible | Negligible |
| Functional walking ability score | 0–1 (n = 5) | 2–3 (n = 17) | 0–1 (n = 5) | 2–3 (n = 17) | ||||
| Sedentary | 10 h 41 min | 1 h 34 min | 11 h 10 min | 1 h 41 min | 96.4** | 1.5 | 89.6** | 7.0 |
| Low-intensity PA | 0 h 20 min** | 0 h 10 min | 1 h 14 min** | 0 h 57 min | 3.0** | 1.0 | 9.7** | 6.6 |
| Light-intensity PA | 0 h 4 min | 0 h 2 min | 0 h 5 min | 0 h 4 min | 0.6 | 0.5 | 0.7 | 0.8 |
| Moderate to vigorous PA | 0 h 1 min | 0 h 1 min | 0 h 1 min | 0 h 1 min | Negligible | Negligible | Negligible | Negligible |
| BI score | ≤ 11 (n = 8) | > 11 (n = 14) | ≤ 11 (n = 8) | > 11 (n = 14) | ||||
| Sedentary | 11 h 25 min | 1 h 35 min | 10 h 51 min | 1 h 41 min | 95.4** | 2.5 | 88.7** | 7.4 |
| Low-intensity PA | 0 h 28 min** | 0 h 19 min | 1 h 21 min** | 1 h 0 min | 4.0** | 2.4 | 10.6** | 6.9 |
| Light-intensity PA | 0 h 4 min | 0 h 3 min | 0 h 6 min | 0 h 5 min | 0.5 | 0.5 | 0.8 | 0.8 |
| Moderate to vigorous PA | 0 h 1 min | 0 h 1 min | 0 h 1 min | 0 h 1 min | Negligible | Negligible | Negligible | Negligible |
| 6-CIT | < 8 (n = 8) | ≥ 8 (n = 11) | < 8 (n = 8) | ≥ 8 (n = 11) | ||||
| Sedentary | 11 h 6 min | 1 h 31 min | 10 h 44 min | 1 h 57 min | 91.3 | 7.8 | 93.2 | 4.8 |
| Low-intensity PA | 0 h 48 min | 0 h 43 min | 0 h 56 min | 0 h 50 min | 8.3 | 7.7 | 6.3 | 4.4 |
| Light-intensity PA | 0 h 5 min | 0 h 4 min | 0 h 4 min | 0 h 3 min | 0.6 | 0.7 | 0.6 | 0.7 |
| Moderate to vigorous PA | 0 h 1 min | 0 h 1 min | 0 h 0 min | 0 h 0 min | Negligible | Negligible | Negligible | Negligible |
However, those residents with better functional walking ability and better physical function, as assessed by the BI, spent a smaller proportion of accelerometer wear time engaging in sedentary behaviours than those with poorer walking ability and poorer physical function (p < 0.01). In addition, those residents with better functional walking ability and physical function also spent more time, and a greater percentage of accelerometer wear time, engaging in low-intensity PA than those with poorer walking ability and physical function (p < 0.01) (see Table 21).
Assessment of Physical Activity in Frail Older People questionnaire
The APAFOP46 was trialled with two purposively selected residents with relatively strong cognitive ability in CH1 (Table 22).
| Characteristic | Resident 1 | Resident 2 |
|---|---|---|
| Age (years) | 80 | 88 |
| Height (cm) | 166 | 162 |
| Weight (kg) | 65 | 71 |
| Functional walking ability scorea | 2 | 0 |
| BI scoreb | 14 | 7 |
| PAM-RC scorec | 10 | 2 |
| 6-CIT scored | 8 | 8 |
Figure 13 shows the activities of the two residents over a 24-hour period, as recorded by the APAFOP questionnaire. Little walking or activities of any form were recorded. Both residents spent the majority of their time engaged in typically sedentary activities (sitting or lying). One resident who participated in completing the APAFOP was immobile and displayed no bouts of activity. The other resident was most active at 08.00, 12.00 and 19.00, coinciding with getting up, having lunch and going to bed.
FIGURE 13.
Activities of two residents in a 24-hour period, as recorded by the APAFOP. Cumulative energy expenditure (kcal) is shown for each category of activity undertaken.
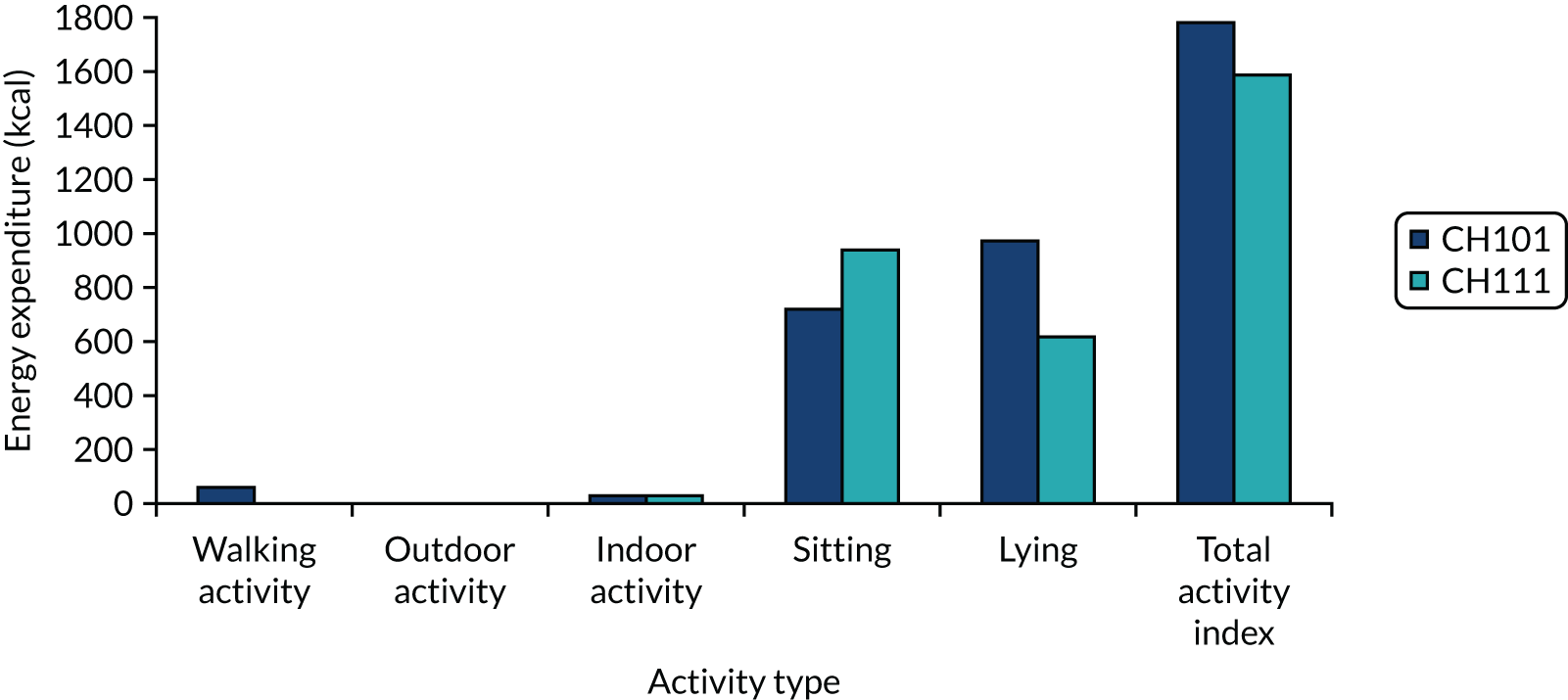
Feasibility of using the Assessment of Physical Activity in Frail Older People questionnaire
Administering the tool was relatively straightforward, given that the range of activities undertaken by residents in a typical day was fairly limited in scope. However, administering the questionnaire took > 1 hour to complete.
Discussion/preliminary conclusions
Recruitment and participation
The study took an inclusive approach to recruitment, in anticipation of the development of a ‘whole-home’ intervention in the later stages of the research programme, with few exclusion criteria for the study. In spite of this, only 49 (22.3%) of the 220 residents in the participating CHs were recruited, a lower rate than our provisional estimate of 80 recruited residents (20 residents in each of four CHs).
Over half of eligible residents did not have mental capacity confirmed by researchers. PC agreement was therefore sought from 75 of these residents (eight residents declined the approach to their PC). Twenty-two (29.3%) of the 75 PCs did not respond. NCs were not used in the study, as the CH manager of the first CH where recruitment was undertaken did not agree with this approach. The CH manager expressed concerns that PCs may have ‘actively’ not responded as they did not want their relative to take part in the study, and therefore did not feel comfortable advising on whether or not these residents would choose to be involved in the research. This represented a loss of potential residents for recruitment. This influenced our approach going forward to the feasibility trial in WS5, insofar as we aimed to maximise recruitment of all potential recruits in the CHs, thereby increasing generalisability. We aimed to do this by encouraging CH managers to speak to as many relatives as possible in person about the study prior to sending out information, and by ensuring that the research team was approachable and available should relatives have any queries. We also attended resident/relative meetings and meetings for staff to increase awareness of the research. Furthermore, we offered reassurance to CH managers regarding the process of consulting a NC.
Questionnaire outcome measures
We tested the suitability and feasibility of a number of outcome measures in the CH setting in preparation for the feasibility trial in WS5.
Barthel Index
The BI was completed in collaboration with the CH staff for all 46 residents participating in the study. The high completion rate is indicative of the method of completion and staff reporting that it was not onerous to complete. Proxy completion of the BI has been recommended as more valid in older and cognitively impaired populations. 56
The Physical Activity and Mobility in Residential Care Scale
The PAM-RC is a relatively new scale, with little evidence yet for its use in research. It has face validity for this population and has been reported to have excellent test–retest reliability, internal consistency and good construct validity (Dr Julie Whitney, personal communication). The PAM-RC was completed in collaboration with the CH staff for all 46 residents participating in the study.
Functional walking ability
The functional walking ability questionnaire was based on the FAC50 and was completed for all 46 residents included in the study. The reason the functional walking ability questionnaire was used in the study was that it was simpler and more accessible for CH staff. Going forward to the feasibility trial in WS5, however, it was decided to use the full FAC, to allow comparability with existing research.
The Timed Up and Go Test
The TUGT was trialled in the programme development work (September 2010–February 2011). 24 In the programme development work, eight (40%) residents who were approached to complete the test declined; reasons included a lack of motivation, pain and illness. In addition, five (25%) participants were unable to complete the test, as they required assistance. The test was therefore completed by only seven (35%), more able, residents. In the development work, there were no correlations between time spent in different PA intensities and TUGT scores.
The TUGT was recently reviewed in a Cochrane review of physical rehabilitation for older people in long-term care. 34 This review included 12 studies using the standard TUGT. Many studies were unable to be included in this review on the grounds of extensive missing data and substantial variation in individual results. Hoppitt et al. 130 stress that the low levels of completion associated with the TUGT make it inappropriate for use in RCTs. Reasons for this include the time taken to complete the task (e.g. one participant took 418 seconds to complete the TUGT); difficulty in understanding the task; and, for some residents, an inability to complete the task because of physical or cognitive impairments. Following this analysis, the test was deemed inappropriate for use in the current sample and going forward to the randomised trial.
Going forward to the feasibility trial in WS5, therefore, it was decided that the BI, the PAM-RC and the FAC would be suitable and feasible measures of physical function/mobility in this CH population.
Assessment of Physical Activity in Frail Older People questionnaire
In addition to our primary outcome measure, we were conscious of resource issues for further work in assessing PA in CH situations. We thus took the opportunity to assess the validity of assessing PA as time spent in equivalent MET activities using the newly developed APAFOP questionnaire. This interview-administered PA questionnaire had recently been purposely developed and reliability tested46 for older people with and without cognitive impairment. It is based on considerable development work, including a systematic review54 and robust psychometric testing. The assessment period is limited to the previous 24 hours to assist recall and there is a focus on ADL, making it a suitable tool for our work. 55 Although direct assessment of movement is not possible using this instrument, time spent in PAs of differing MET categories can be calculated. The instrument thus offers a more global assessment of habitual PA that might have generic value for CHs once the efficacy of the whole-home intervention has been established. We were also unsure of the adherence to accelerometer protocols, which may be a challenge among the study population.
Unfortunately, the manual to implement the APAFOP was not initially available. After having received it, we had concerns about the feasibility of administering the APAFOP and its validity in a population with high levels of cognitive impairment. We therefore decided, initially, to undertake a small feasibility assessment of the use of the APAFOP. The APAFOP was trialled with two purposively selected residents who had relatively strong capacity in CH1. Following this analysis, the test was deemed inappropriate for use in the current sample.
Accelerometers
Observational study
Accelerometers worn on the hip and accelerometers worn on the wrist were compared with observations of residents during a 2-hour ‘free-living’ period to measure criterion validity. Although the sensitivity for PA and PV for sedentary behaviour was higher for the wrist than for the hip counts, all of the other measures used to assess criterion validity suggested that the hip counts were superior to the wrist counts. Indeed, both the overall agreement and the kappa statistic indicated that the classification agreement was considerably better when using the hip counts than when using the wrist counts. Thus, despite the suggestion that a wrist-worn accelerometer may provide more valid estimates of PA and sedentary behaviour than a hip-worn monitor in older CH residents, the results suggest that the hip remains the preferred wear location when using accelerometers in this population group.
Feasibility of using accelerometers
Twenty-two (73%) of the 30 residents who wore an accelerometer on the hip had valid data sets for wear time, that is ≥ 8 hours of wear on ≥ 4 days of the week. The proportion of residents meeting the criteria for valid wear time was lower than that found in the development work (84.8%). This may, however, be attributed to differences in participant characteristics. For example, residents deemed to lack capacity were not included in the development work, whereas they were included in the current study. Therefore, residents in the current study probably needed greater support from CH staff with the administration of the accelerometers. Given the heavy workloads of staff, the study may not have been viewed as a priority, and thus they may not have prompted residents to wear their monitor or offered them assistance with putting them on. Moreover, a considerable number of the potential participants in the development work who declined to take part in the study [10/19 (52.6%)] cited not wishing to wear an accelerometer for so many days (5 days were needed for data to be considered valid) as their reason for doing so. Thus, it may be that those who wore the accelerometers were not representative of a CH population.
Compared with more recent studies conducted in long-term care settings that have employed similar criteria to define valid wear time, a similar or greater proportion of residents in the current study had valid data. For example, a recent study conducted in a population of older adults residing in assisted-living facilities reported that 114 out of 148 (77%) consented participants had valid accelerometer data (defined as ≥ 8 hours on ≥ 3 days). 58 Moreover, Corcoran et al. 59 reported that 77 out of 146 (52.7%) residents recruited from assisted-living facilities in a US study met the criteria for valid wear time (defined as ≥ 10 hours on ≥ 3 days). Similarly, 38 out of 70 (54.3%) participants in a recent study conducted in a CH setting provided valid accelerometer data (≥ 8 hours on ≥ 3 days). 23
In addition, of the eight participants who did not meet the valid wear time criteria, only three residents did not provide any valid data and the monitors were lost for another two participants. Of the remaining three participants, one provided valid data for 1 day and two provided valid data for 2 days, which leads to the conclusion that it is feasible to use the accelerometers.
Extended accelerometer wear: activity monitor logs
Correct identification of accelerometer wear time is imperative to ensure that accelerometer data are interpreted and analysed correctly. 60 Although different methods of identifying accelerometer non-wear are used in the literature, automated algorithms and activity logs are the most common. However, neither of these methods is without limitations. None of the automated algorithms has been specifically developed for a CH population; therefore, the applicability of these to this unique population may be questioned. Indeed, on looking at the data, it became apparent that the use of automated algorithms was particularly problematic in older CH residents, as they typically spent the majority of their time sedentary. Thus, it was possible that wear time was being underestimated as a result of sedentary time being mistakenly categorised as non-wear time. Consequently, although it was acknowledged that completion of activity logs may be viewed as burdensome, much emphasis was placed on attempting to collect accurate information about accelerometer wear using an activity log.
Unfortunately, completion of the logs in the study was poor, with only eight (19.5%) being fully completed and 20 (48.8%) partially completed; of these 28 logs, 13 (46.4%) were completed by a researcher, rather than the resident or CH staff. These low figures were despite the administration of the logs in a way in which the CH managers felt would meet with greatest success, for example locating the activity logs within care plans or in a centralised file. CH managers generally delegated the responsibility for the study to a senior carer or activity co-ordinator, and brought the research to the attention of individual staff or at staff meetings. However, completion of the logs was found to be onerous for the CH staff. They were therefore asked principally to record the times of administration and removal of the monitor. Recording reasons for removal was optional.
Accelerometers: extended accelerometer wear
The rate of extended wear of accelerometers by residents was high [41 (89%) of the 46 recruited residents]. Of these 41 residents, 30 (73.2%) wore an accelerometer on the hip; 10 (24.4%) wore it on the wrist, at the request of CH managers at two homes; and one resident (2.4%) was asked to wear a commercially available device so that we could explore the data collected by this device. As mentioned in Feasibility study: use of accelerometers to assess physical activity over extended periods, however, the decision was taken during the study not to analyse the data derived from wrist-worn accelerometers, as the results of the observation study suggested that data collected from a hip-worn accelerometer had better validity than wrist-worn accelerometer data in this population, and there is also limited guidance available on how best to interpret data collected from a wrist-worn accelerometer. In addition, algorithms only exist currently in relation to accelerometers worn on the hip.
The outcomes of the commercially available device were based on distance moved; therefore, it was decided that these data were unlikely to be sufficiently accurate for our purposes in this population.
Almost three-quarters [22 (73.3%) out of 30 residents] of residents wearing an accelerometer on the hip had valid data. The mean daily wear time for these 22 residents was 12 hours 24 minutes (SD 2 hours 36 minutes).
We found that cognitive impairment and poor physical function in residents and heavy workload for CH staff made it difficult for them to assist with administering the accelerometers and to complete the activity monitor logs. We therefore adopted a more pragmatic approach as the WS progressed:
-
Residents were asked to wear the accelerometers for as long as they were comfortable doing so. Sometimes, this was taken on a day-by-day basis, with continuous support from the researcher (in assisting with administering the accelerometers and completing the activity logs, during frequent visits to the home).
-
Accelerometers were collected once it was indicated that there were 5–7 days of data (not necessarily consecutive days) or when residents indicated that they no longer wanted to wear the monitor.
The vast majority of residents’ time was spent sedentary: mean 11 hours 11 minutes (SD 2 hours 21 minutes), which equated to 90.5% of time wearing the accelerometers. A mean of only 1 hour 13 minutes (SD 1 hour 8 minutes), that is 9.5% of accelerometer wear time, was accumulated in PA, and the majority of this was low-intensity PA. In addition, sedentary time was often spent in long ‘bouts’: 19.3% and 19.0% of total sedentary time was accumulated in bouts of 30–59 minutes and of at least 60 minutes, respectively.
It would initially appear, therefore, that the conclusions from the initial development work still hold, namely that there are two key opportunities to increase PA in CH residents:
-
Break up long sedentary periods with activity.
-
Increase the duration of bouts of PA towards a goal of 10-minute bouts of low- to light-intensity activity, and finally to an accumulation of 20–30 minutes of low- to light-intensity PA on 5 days per week, as per the guidance for interpreting the UK PA guidelines for frailer older people, published by the British Heart Foundation National Centre. 33
In addition, we have identified that there is an opportunity to increase bouts of low-intensity activity.
Key points
Data collection was labour intensive for both researchers and CH staff. Researchers need a significant presence in CHs to support staff to enable the collection of high-quality data.
Accelerometers worn on the hip (rather than the wrist) were a valid way to collect data for extended periods of wear. However, accelerometers worn on the wrist may be used to measure upper-body movement in situations in which such upper-body movement activities occur (e.g. exercise classes sitting down).
Resident recruitment was lower than expected. We considered each resident in six CHs for inclusion in WS2, but recruited only 49 (22.3%) residents out of the population of 220. Of the 49 residents recruited, nearly 40% were assented as a result of consultee approaches (see Figure 12). This recruitment rate should be borne in mind in future studies.
Based on learning from the current WS, a more pragmatic approach to the accelerometer data collection procedures was proposed for use in future WSs. First, the practice of administering accelerometers as soon as possible once informed consent/assent had been gained, coupled with the recruitment methods employed, meant that not all participants in a given home were wearing the accelerometer at the same time. As an example, in one of the CHs, accelerometers were administered to four participants on the Tuesday and to two participants on the Thursday of the same week. An additional two accelerometers were then administered on the following Tuesday. It was thought that this practice may have adversely affected compliance to the data collection procedures, as the monitoring period for the ‘whole home’ was protracted; therefore, the perceived burden of the research was probably greater. Consequently, it was planned for accelerometers to be administered more systematically (i.e. in batches) whenever possible.
Second, the CH staff had more need for support from the research team than was originally proposed. In the light of this, going forward, it was decided to increase the level of support for CH staff when assisting with accelerometers. This included a member of the research team visiting or telephoning the CH periodically (the frequency of visits/contacts was based on perceived need) over the measurement period, and, in addition, producing and providing written materials, namely a list of participants wearing an accelerometer and ‘reminder posters’ for CH staff to display prominently in the CH. As described previously, the activity log was also amended during this WS in an attempt to make it less burdensome to complete and to ensure that information regarding the time a participant’s accelerometer was put on and taken off each day was collected. The activity log will be considered further and additional amendments will be made, if deemed necessary, to make the activity log simpler to complete.
Appendix 3 Barriers to and opportunities for increasing physical activity from the qualitative research
| Observation/theme | Barrier | Opportunity |
|---|---|---|
| Resident profile | ||
Differing physical and mental capacity:
|
|
|
| Difficulty engaging with residents who are both physically and cognitively frail |
|
|
| Residents’ choice of activities? |
|
|
| Resident – roles | ||
| Purposeful movement is required |
|
|
| Environment (social) | ||
| Some residents acted differently outside their usual environments, for example pouring tea |
|
|
| Environment (physical) | ||
|
|
|
| Location of activities |
|
|
|
||
| Dining areas are underutilised | ||
| Physical barriers, for example locked doors and insufficient lighting |
|
|
| Assistance is needed to move between floors to utilise the whole home | ||
| Outdoor spaces are underused |
|
|
|
||
|
||
| Staff behaviours | ||
| Managing risk |
|
|
| Providing assistance |
|
|
| Finding time: conflict between providing care and activities |
|
|
| Encouragement of PA |
|
|
| Providing opportunities for PAs |
|
|
| Risks | ||
| Risk of falls/injury |
|
|
| Residents’ daily routine | ||
| Inactivity for large parts of the day |
|
|
| Staff routines |
|
|
| Scheduled activities |
|
|
Appendix 4 List of performance/change objectives
What needs to happen so that each resident can achieve their potential for movement (for the benefit of physical health and well-being)?
Care home managers/organisations to be enabled to:
-
manage risk of falls while maintaining movement (knowledge) (beliefs about consequences) (skills) (social influences) (beliefs about capabilities) (emotion)
-
create a physical environment that encourages safe movement and makes greater use of external space (e.g. garden/patio) (knowledge) (motivation and goals) (skills) (environment and resources)
-
develop systems for gaining knowledge of residents’ potential for movement (knowledge) (motivation and goals) (skills)
-
encourage staff to enable movement and to maintain regularity of movement throughout the day (knowledge) (motivation and goals) (beliefs about capabilities) (professional identity) (memory/attention)
-
encourage staff to engage in positive social interactions with residents (knowledge) (skills) (social influences) (beliefs about capabilities) (environment and resources)
-
support the role of the activity co-ordinator within the home and enable the training of all staff in effective ways to promote movement in daily routines (knowledge; beliefs about consequences) (motivation and goals) (professional identity) (memory/attention) (environment and resources)
-
promote opportunities for community engagement (beliefs about consequences) (motivation and goals) (beliefs about capabilities).
All CH staff to be enabled to:
-
develop different activities and methods of promoting movement suited to residents’ diverse physical and mental abilities (knowledge; beliefs about consequences) (motivation and goals) (skills) (social influences)
-
be aware of residents’ abilities and potential to increase movement, and regularly assess change (skills) (social influences) (beliefs about capabilities) (professional identity)
-
engage in practices that enable and do not curtail movement; for example, movement can be enabled by facilitating residents to take a greater role in ADL and self-care (social influences) (professional identity) (behavioural regulation)
-
develop a good knowledge of residents’ hobbies, interests, likes and aspirations, which can be used to plan activities and encourage engagement of residents in these activities (motivation and goals) (skills) (professional identity) (environment and resources)
-
provide residents with opportunities to take on roles in the CH; these roles may be based on residents’ previous employment (e.g. folding towels in the laundry, filing papers in an office, watering plants, taking dirty cups back to the kitchen, and personal tasks, such as closing their own curtains) (knowledge) (motivation and goals) (skills) (social influences)
-
support the work of the activity co-ordinator in planning and implementing relevant activities that engage residents (the advisory group felt that the word ‘activity’ should be modified; the objective should focus on utilising the skills and interests of CH staff and should be broader than an activity session) (motivation and goals) (beliefs about capabilities) (professional identity)
-
communicate information about residents’ movement to one another (behavioural regulation/action planning) (memory/attention) (environment and resources).
Activity co-ordinators (or nominated staff members) to be enabled to:
-
make best use of space in the home and enable participation in activities by using knowledge of where residents are most comfortable (knowledge; beliefs about consequences) (motivation and goals) (beliefs about capabilities) (environment and resources)
-
draw on knowledge of staff and residents in planning activities (knowledge; beliefs about consequences) (environment and resources)
-
have the confidence to try new activities and ideas, which may, or may not, work (beliefs about consequences) (skills) (social influences) (emotion)
-
model appropriate behaviours that enable movement (beliefs about consequences) (social influences) (beliefs about capabilities) (professional identity)
-
make residents aware of opportunities for activities (motivation and goals) (behavioural regulation) (memory/attention).
Residents to be enabled to:
-
provide feedback on movement and activities in the CH (social influences) (beliefs about capabilities) (environment and resources)
-
take a role in self-care and a role in the CH, when capable (beliefs about consequences) (motivation and goals) (beliefs about capabilities) (emotion).
Outside the CH, friends/relatives are to:
-
consider the enhancement of movement in their choice of CH (knowledge; beliefs about consequences)
-
understand the benefits of movement for residents’ health and well-being (knowledge; beliefs about consequences)
-
expect their relatives to be encouraged to do some tasks around the home (knowledge; beliefs about consequences) (emotion)
-
volunteer in the CH (activities to be suggested by the CH manager).
Appendix 5 Example of mapping of change objectives and theoretical domains
| What needs to happen so that each resident can achieve their potential for movement (for the benefit of physical health and well-being)? | Knowledge and skills | Social | Role at work | Planning | Environment | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Increase knowledge so . . . | Develop skills so . . . | Increase acknowledgement that certain activities are a good thing so . . . | Develop abilities to overcome pressure from others so . . . | Improve confidence so . . . | Increase motivation so . . . | Address emotional factors so . . . | Create a professional identity so . . . | Improve abilities to recollect so . . . | Develop abilities to plan ahead so . . . | Improve the environment and access to resources so . . . | |
| CH managers are enabled to | |||||||||||
| (1) Manage risk of falls while maintaining movement | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| (2) Create a physical environment that encourages safe movement and makes greater use of external space (e.g. garden/patio) | ✓ | ✓ | ✓ | ✓ | |||||||
| (3) Develop systems for gaining knowledge of residents’ potential for movement | ✓ | ✓ | ✓ | ||||||||
| (4) Encourage staff to enable movement and to maintain regularity of movement throughout the day | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||
| (5) Encourage staff to engage in positive social interactions with residents | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||
| (6) Support the role of the activity co-ordinator in the home and enable the training of all staff in effective ways to promote movement in daily routines | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| (7) Promote opportunities for community engagement | ✓ | ✓ | ✓ | ||||||||
Appendix 6 Testing out the acceptability and appropriateness of a range of outcome tools and measures
Aims and objectives
The aims and objectives of this work, undertaken in addition to those stated in the research proposal, were to:
-
evaluate outcome tools to measure PA in the CH population to inform the outcome assessment in WS5 (the feasibility cluster randomised trial)
-
evaluate outcome tools to assess staff job satisfaction and the CH environment
-
review methods of data collection at the level of the residents and CHs.
Methods
The service improvement work of WS4 also provided the opportunity to refine resident recruitment procedures and to clarify our proposed outcome assessment tools from WS2. Earlier WSs had highlighted the importance of PA on not only physical health/function (decelerating decline), but also more general well-being (to improve or maintain the quality of life of residents). It is also possible that depression may influence the take-up of PA and may be affected by PA. Therefore, we undertook further pilot assessment of outcome measures to assess these domains with CH residents (details can be found in the WS4 protocol; see Report Supplementary Material 6). We carried out additional feasibility work in relation to the testing of these outcome measures, which involved the ‘questerview’ method of voice-recording the outcome measure questionnaires completed with residents. This was to capture additional insights into the appropriateness of the various measures from a resident perspective. Through capturing the responses (by voice-recording residents’ answers and their conversations with researchers in relation to the questions posed), we hoped to gain an understanding of how residents interpret questions and the meanings attached to their responses.
The intention was not to collect complete data sets on all outcomes, but rather to determine what was feasible among this very challenging client group and, ultimately, to inform data collection for WS5. With this in mind, we did not use all of the outcome measures with all residents, choosing instead to test each of the outcome measures with a few residents and then, if a measure was deemed not to be fit for purpose (e.g. questions too complex), we did not pursue the use of that measure further.
For some key outcomes (e.g. measurement of PA, physical function, and health-related quality of life), we hoped to gain some preliminary insight into whether or not the tools might be sensitive to change, including the tools measuring PA, among CH residents.
All residents in the participating CHs were screened for eligibility. For a full description of recruitment procedures, see the study protocol (see Report Supplementary Material 6).
Resident recruitment
A total of 147 residents across the four CHs were eligible to participate in the research; of these, 136 were approached by researchers. Mental capacity was confirmed in 60 residents, and 75 letters were sent out to PCs. As a result of this process, 11 residents were assented to participate in the study by PCs, and 19 residents were assented by NCs. In total, 61 residents [mean 15 (range 8–31) residents per CH] were recruited for data collection. This is in line with our estimate of feasibly, being able to recruit 8–12 residents per home, as outlined in the protocol for the WS.
Evaluation of outcome measures
Questionnaire outcome measures
Working with residents and staff, we assessed the feasibility of a range of resident- and proxy-completed outcome measures.
Resident-completed outcome measures: the measures that were tested related to grip strength, physical function (EMS), mood (GDS), perceived health [EQ-5D-5L and ICEpop CAPability measure for Older people (ICECAP-O)] and quality of life [World Health Organization Quality of Life-BREF, Control, Autonomy, Self-Realization and Pleasure (CASP-19) and Ageing Well Profile]. We also tested the DEMQOL and DEMQOL Proxy, which were not included in the original grant application, as research within our unit has suggested that these are useful measures to use with frail older adults.
Proxy-completed outcome measures
The BI and PAM-RC were completed by researchers in collaboration with the CH staff for all (n = 61) participating residents at baseline. The mean BI score was 10.6 (SD 5.4) and the median score was 10 (IQR 6–14; range 1–20). More than half of the residents [n = 35 (57%)] had a score of ≤ 11, indicating dependence in ADL. The mean total PAM-RC score was 10.5 (SD 6.0), and the median score was 10 (IQR 5–15; range 1–21). The mobility and balance domains of the PAM-RC may be considered together as questions related to ‘abilities’, and thus comprise the first subsection of the scale. The mean ability subscore was 6.0 (SD 3.0), and the median score was 6 (IQR 3–8; range 1–10). Equally, walking frequency, wandering and outdoor mobility may be considered together as ‘activity’ questions, and make up the second subsection of the scale. The mean activity subscore was 4.5 (SD 3.4) and the median score was 4 (IQR 2–7; range 2–11).
At follow-up, one resident had died and one resident had moved out of the CH; therefore, 59 residents were available for data collection. As was the case at baseline, the BI and PAM-RC were to be completed by researchers in collaboration with the CH staff. However, one of the CHs (CH9) withdrew from data collection, and the data from an additional participant were marked as missing. Thus, the BI and PAM-RC were completed for 47 residents. The mean BI score was 10.0 (SD 5.6), and the median score was 9 (IQR 5.5–14.5; range 0–19). A considerable proportion [n = 29 (62%)] of these residents had a score of ≤ 11, indicating dependence in ADL.
The mean total PAM-RC score was 11.4 (SD 6.2), and the median score was 12 (IQR 5–17; range 1–20). The mean ability subscore was 6.7 (SD 3.2) and the median score was 7 (IQR 5–10; range 0–10). The mean activities subscore was 4.7 (SD 3.3) and the median score was 4 (IQR 1–7.5; range 0–10).
In accordance with the findings from WS2, the completion rates for the BI and PAM-RC were high, thus providing additional support for the feasibility of these measures.
Accelerometer
Feasibility of using accelerometers
Across the four homes, 50 (82%) of the 61 recruited residents agreed to wear a hip accelerometer at baseline. An accelerometer was not administered to the other participants for the following reasons: resident was ill during data collection (n = 1), consultee deemed it inappropriate (n = 3) and resident wore a wrist accelerometer (n = 7). There were no differences in the personal characteristics of those residents to whom a hip-worn accelerometer was administered (n = 50) and those who did not receive one (n = 11) (p > 0.05).
Of those 50 residents who wore a hip accelerometer, nine did not meet the criteria for valid wear time (i.e. ≥ 8 hours on ≥ 4 days of the week) and a further three accelerometers were lost. Thus, accelerometer data from 38 (62% of recruited residents) residents were valid. There were no differences in the personal characteristics and mobility scores of those residents who met the criteria for valid accelerometer data (n = 38) and those who did not (n = 11) (p > 0.05).
Those residents (n = 38) who provided valid wear time for analysis at baseline were approached and asked to wear the accelerometer again. Of these, 27 residents agreed to wear the accelerometer. An accelerometer was not administered to the other 11 residents for the following reasons: resident deceased (n = 1), resident moved out of home (n = 1), resident declined to wear (n = 6) and health had deteriorated (n = 3). Twenty-one of the 27 residents who agreed to wear an accelerometer met the criteria for valid wear. As was the case at baseline, there were no differences in the personal characteristics and mobility scores of those residents who met the criteria for valid accelerometer data (n = 21) and those who did not (n = 6) (p > 0.05).
Refinement of data collection procedures
Based on learning from this WS, a more structured approach to the accelerometer data collection procedures was proposed for use in the feasibility trial (WS5), in an attempt to ensure the quality of accelerometer data. Key aspects of the data collection procedures are detailed here.
First, whenever possible, accelerometers were to be administered to all participants by a researcher (with support from CH staff, when appropriate) between 09:00 and 11:00 in an attempt to ensure sufficient wear time (i.e. ≥ 8 hours per day). Furthermore, in an attempt to ensure that the accelerometer was worn on a weekend day, we proposed that accelerometers should be administered on either a Thursday or a Friday, given that compliance in the current WS tended to decline over the measurement period following initial enthusiasm. The need for more support from the research team than was originally proposed was acknowledged in this WS, and a member from the research team visited or telephoned each of the CHs periodically over the measurement period. However, these visits were predominantly done on an ad hoc basis, as the frequency was based on perceived need. It was felt that a more systematic approach to the provision of this support would be needed for a larger trial. Thus, we proposed that a prompting schedule was implemented in the feasibility trial. Specifically, a researcher would make a visit or telephone call to the CH two or three times over the measurement period. Flexibility would be afforded over when these prompts were made, with the exception that all homes would receive a prompt on day 2 of the measurement period.
In addition, we suggested that, when appropriate, the following techniques (each of which was trialled in the current WS) be employed, in an effort to improve compliance:
-
provide the research lead with a list of residents wearing the accelerometers and request that this is displayed prominently in the CH
-
provide CH staff with an ‘activity monitor how-to guide’ (which includes contact details for the research team).
Exploration of content and methods of collecting routine and anonymous data in care homes
The research assistant discussed with the CH managers in the four selected homes the content and method of collecting routine data at the level of the resident (e.g. age, sex, length of residence) and CH (e.g. number of beds, staff levels), clarifying what information is recorded, how it is reported and the frequency/time scale of reporting. This informed data collection in the feasibility study, including the economic evaluation.
Members of the research team also discussed with the manager the feasibility of collecting anonymised data at the level of the home and resident. Staff successfully completed the BI and PAM-RC for each of the residents in the home on an anonymised basis.
Evaluate tools to assess staff job satisfaction and the care home environment
A range of tools (see Report Supplementary Material 6) was considered. After review of the literature and discussion with the care managers and care staff, the P-CAT was chosen as an appropriate tool for staff completion.
Appendix 7 Statistical tables
Recruitment and follow-up
| Characteristic | MoveMore + UC (n = 5) | UC (n = 7) |
|---|---|---|
| Overall home size (number of beds), mean (SD) | 30.0 (2.92) | 38.0 (26.26) |
| Number of beds taking part, mean (SD) | 16.0 (8.51) | 20.0 (13.84) |
| Location, n (%) | ||
| Urban | 0 (0) | 2 (28.6) |
| Suburban | 3 (60.0) | 3 (42.9) |
| Semirural | 2 (40.0) | 1 (14.3) |
| Rural | 0 (0) | 1 (14.3) |
| Ownership, n (%) | ||
| Local authority | 1 (20.0) | 0 (0) |
| Independent | 2 (40.0) | 3 (42.9) |
| Chain | 1 (20.0) | 2 (28.6) |
| Not for profit | 1 (20.0) | 2 (28.6) |
| Participating CH/unit care provision, n (%) | ||
| Residential | 3 (60.0) | 5 (71.4) |
| Residential/nursing | 1 (20.0) | 0 (0) |
| Residential/dementia | 1 (20.0) | 2 (28.6) |
| Rehabilitation/intermediate care facility,a n (%) | 1 (20.0) | 1 (14.3) |
| Telemedicine facility, n (%) | 3 (60.0) | 1 (14.3) |
| Activity co-ordinator in post, n (%) | 3 (60.0) | 5 (71.4) |
| Taking part in initiatives to enhance resident care, n (%) | 1 (20.0) | 2 (28.6) |
| Resident profile, mean (SD) | ||
| Number of permanent residents | 26.0 (7.45) | 34.1 (23.32) |
| Number of permanent self-funded residents | 10.8 (8.58) | 15.3 (16.76) |
| Number of temporary residents | 2.2 (4.38) | 1.0 (1.15) |
| Average number of residents in previous 3 months | 30.6 (5.94) | 26.4 (12.12) |
| Staff profile, mean (SD) | ||
| Number of permanent staff | 34.2 (11.39) | 33.0 (16.05) |
| Number of agency staffb | 0.0 (0.00) | 0.6 (1.51) |
| Number of bank staffb | 2.2 (2.95) | 1.8 (1.94) |
| Number of staff who have face-to-face contact with residents | 36.4 (13.52) | 24.71 (18.12) |
| Demographic | Baseline | 3-month follow-up | 6-month follow-up | 9-month follow-up | ||||
|---|---|---|---|---|---|---|---|---|
| MoveMore + UC (n = 5) | UC (n = 7) | MoveMore + UC (n = 5) | UC (n = 6)a | MoveMore + UC (n = 5) | UC (n = 6)a | MoveMore + UC (n = 5) | UC (n = 7) | |
| Activity co-ordinator in post, n (%) | ||||||||
| Yes | 3 (60.0) | 5 (71.4) | 4 (80.0) | 4 (66.7) | 4 (80.0) | 5 (83.3) | 4 (80.0) | 6 (85.7) |
| No | 2 (40.0) | 2 (28.6) | 1 (20.0) | 2 (33.3) | 1 (20.0) | 1 (16.7) | 1 (20.0) | 1 (14.3) |
| Taking part in initiatives to enhance resident care, n (%) | ||||||||
| Yes | 1 (20.0) | 2 (28.6) | 2 (40.0) | 1 (16.7) | 2 (40.0) | 2 (33.3) | 1 (20.0) | 1 (14.3) |
| No | 4 (80.0) | 5 (71.4) | 3 (60.0) | 5 (83.3) | 3 (60.0) | 4 (66.7) | 4 (80.0) | 6 (85.7) |
| Resident profile, mean (SD) | ||||||||
| Number of permanent residents | 26.0 (7.45) | 34.1 (23.32) | 26.0 (8.12) | 32.7 (24.93) | 26.6 (7.02) | 26.5 (12.58) | 25.4 (6.07) | 25.0 (1.18) |
| Number of permanent self-funded residents | 10.8 (8.58) | 15.3 (16.76) | 11.6 (9.24) | 19.7 (19.18) | 10.6 (8.29) | 11.2 (11.13) | 9.2 (5.63) | 10.0 (11.47) |
| Number of temporary residents | 2.2 (4.38) | 1.0 (1.15) | 2.0 (3.39) | 2.0 (1.26) | 2.8 (5.72) | 1.3 (1.37) | 1.8 (3.49) | 1.3 (1.98) |
| Average number of residents in previous 3 months | 30.6 (5.94) | 26.4 (12.12) | 29.4 (3.44) | 24.3 (11.57) | 29.2 (3.03) | 27.7 (11.54) | 28.2 (3.49) | 25.6 (11.90) |
| Staff profile,b mean (SD) | ||||||||
| Number of permanent staff | 34.2 (11.39) | 33.0 (16.05) | 37.2 (12.58) | 35.5 (17.52) | 37.2 (20.54) | 35.3 (19.57) | 36.2 (14.04) | 25.5 (16.20) |
| Number of agency staffc | 0.0 (0.00) | 0.6 (1.51) | 0.6 (1.34) | 1.0 (2.00) | 0.8 (1.10) | 0.0 (0.00) | 0.4 (0.55) | 0.0 (0.00) |
| Number of bank staffc | 2.2 (2.95) | 1.8 (1.94) | 2.8 (2.59) | 2.0 (2.65) | 2.0 (2.92) | 3.3 (3.78) | 1.6 (2.19) | 2.0 (2.45) |
| Number of staff who have face-to-face contact with residents | 36.4 (13.52) | 24.71 (18.12) | 37.6 (15.44) | 37.7 (20.06) | 38.2 (20.91) | 36.2 (22.04) | 37.4 (14.26) | 27.2 (18.18) |
| Change in manager,d n (%) | – | – | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (14.3) |
| Staff joining in the previous 3 months, median (IQR) | 3.0 (2.0–4.0) | 2.0 (1.0–2.0) | 1.0 (0.0–2.0) | 2.0 (1.0–3.0) | 2.0 (0.0–3.0) | 1.0 (0.0–2.0) | ||
| Staff leaving in the previous 3 months, median (IQR) | 2.0 (1.0–2.0) | 1.0 (0.0–2.0) | 1.0 (1.0–2.0) | 1.5 (0.0–2.0) | 2.0 (0.0–2.0) | 1.0 (0.0–2.0) | ||
| Demographic | Baseline | |
|---|---|---|
| MoveMore + UC (N = 5) | UC (N = 7) | |
| Length of time as manager of the CH (months), mean (SD) | 89.2 (105.79) | 117.3 (110.52) |
| Length of time working in CHs, n (%) | ||
| ≤ 5 years | 0 (0.0) | 0 (0.0) |
| 6–10 years | 0 (0.0) | 1 (14.3) |
| > 10 years | 5 (100.0) | 6 (85.7) |
| Time working in a CH/unit manager role, n (%) | ||
| ≤ 2 years | 0 (0.0) | 0 (0.0) |
| 3–5 years | 0 (0.0) | 0 (0.0) |
| 6–10 years | 1 (20.0) | 4 (57.1) |
| > 10 years | 4 (80.0) | 3 (42.9) |
| Previous role in CH, n (%) | ||
| None (joined as manager) | 4 (80.0) | 3 (42.9) |
| Deputy manager or equivalent | 1 (20.0) | 1 (14.3) |
| Direct care worker | 0 (0.0) | 2 (28.6) |
| Other | 0 (0.0) | 1 (14.3) |
| Demographic | Baseline | 3-month follow-up | 6-month follow-up | 9-month follow-up | ||||
|---|---|---|---|---|---|---|---|---|
| MoveMore + UC | UC | MoveMore + UC | UC | MoveMore + UC | UC | MoveMore + UC | UC | |
| Number of booklets distributed | 178 | 232 | 178 | 143 | 188 | 190 | 181 | 155 |
| Number (%) of booklets returneda | 49 (27.5) | 91 (39.2) | 48 (27.0) | 54 (37.8) | 37 (19.7) | 42 (22.1) | 37 (20.4) | 47 (30.3) |
| Sex, n (%) | ||||||||
| Female | 47 (95.9) | 87 (95.6) | 44 (91.7) | 53 (98.1) | 25 (83.3) | 37 (92.5) | 23 (92.0) | 36 (97.3) |
| Male | 2 (4.1) | 4 (4.4) | 4 (8.3) | 1 (1.9) | 5 (16.7) | 3 (7.5) | 2 (8.0) | 1 (2.7) |
| First language, n (%) | ||||||||
| English | 40 (81.6) | 89 (97.8) | 38 (80.9) | 52 (96.3) | 24 (82.8) | 37 (92.5) | 22 (88.0) | 35 (94.6) |
| Other | 9 (18.4) | 2 (2.2) | 9 (19.1) | 2 (3.7) | 5 (17.2) | 2 (7.5) | 3 (12.0) | 2 (5.4) |
| Length of time spent working in CHs (years), mean (SD) | 12.4 (9.49) | 10.9 (10.29) | 6.6 (7.54) | 10.4 (9.31) | 9.5 (9.53) | 8.8 (9.72) | 7.3 (10.11) | 7.9 (9.77) |
| Length of time spent working in current home (years), mean (SD) | 4.4 (5.78) | 5.8 (7.15) | 3.2 (4.13) | 6.6 (6.71) | 5.3 (6.01) | 5.7 (7.13) | 1.3 (2.25) | 3.6 (5.8) |
| Highest qualification,b n (%) | ||||||||
| None | 6 (12.8) | 11 (12.8) | 3 (6.5) | 6 (11.8) | 0 (0.0) | 6 (15.4) | 3 (9.4) | 3 (6.8) |
| O Level/GCSE/NVQ 2/QCF level 1 or 2 | 18 (38.3) | 35 (40.7) | 21 (45.7) | 20 (39.2) | 12 (37.5) | 18 (46.2) | 12 (37.5) | 17 (38.6) |
| A Level/NVQ 3/QCF level 3/registered nursing qualification | 16 (34.0) | 22 (25.6) | 11 (23.9) | 18 (35.3) | 13 (40.6) | 9 (23.1) | 9 (28.1) | 15 (34.1) |
| NVQ 4/certificate or diploma of higher education/foundation degree/QCF level 4 or 5 | 3 (6.4) | 10 (11.6) | 5 (10.9) | 3 (5.9) | 2 (6.3) | 2 (5.1) | 3 (9.4) | 5 (11.4) |
| Advanced diploma/bachelor degree/QCF level 6 | 3 (6.4) | 1 (1.2) | 2 (4.3) | 1 (2.0) | 5 (15.6) | 2 (5.1) | 4 (12.5) | 0 (0.0) |
| Postgraduate certificate, diploma or master’s degree/QCF level 7 | 0 (0.0) | 4 (4.7) | 0 (0.0) | 1 (2.0) | 0 (0.0) | 1 (2.6) | 0 (0.0) | 1 (2.3) |
| Other | 1 (2.1) | 3 (3.5) | 4 (8.7) | 2 (3.9) | 0 (0.0) | 1 (2.6) | 1 (3.1) | 3 (6.8) |
| Job role,c n (%) | ||||||||
| Administration | 0 (0.0) | 3 (3.3) | 0 (0.0) | 2 (3.7) | 2 (5.6) | 1 (2.4) | 0 (0.0) | 2 (4.3) |
| Ancillary | 5 (10.2) | 10 (11.0) | 10 (20.8) | 3 (5.6) | 4 (11.1) | 8 (19.5) | 6 (16.7) | 3 (6.5) |
| Nurse | 4 (8.2) | 1 (1.1) | 2 (4.2) | 0 (0.0) | 2 (5.6) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Carer/senior carer | 36 (73.5) | 58 (63.7) | 32 (66.7) | 39 (72.2) | 21 (58.3) | 25 (61.0) | 22 (61.1) | 30 (65.2) |
| Specialist non-clinical role | 1 (2.0) | 3 (3.3) | 2 (4.2) | 2 (3.7) | 2 (5.6) | 2 (4.9) | 2 (5.6) | 3 (6.5) |
| Team leader | 0 (0.0) | 5 (5.5) | 0 (0.0) | 3 (5.6) | 1 (2.8) | 1 (2.4) | 1 (2.8) | 3 (6.5) |
| Deputy manager/unit manager | 1 (2.0) | 2 (2.2) | 1 (2.1) | 2 (3.7) | 2 (5.6) | 1 (2.4) | 2 (5.6) | 1 (2.2) |
| Manager/unit manager | 2 (4.1) | 6 (6.6) | 1 (2.1) | 3 (5.6) | 2 (5.6) | 3 (7.3) | 2 (5.6) | 4 (8.7) |
| Other | 0 (0.0) | 3 (3.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Work pattern,d n (%) | ||||||||
| Permanent full time | 33 (67.3) | 43 (47.8) | 34 (70.8) | 30 (55.6) | 22 (59.5) | 18 (43.9) | 24 (64.9) | 29 (64.4) |
| Permanent part time | 16 (32.7) | 40 (44.4) | 14 (29.2) | 21 (38.9) | 12 (32.4) | 22 (53.7) | 12 (32.4) | 15 (33.3) |
| Agency/bank/freelance | 0 (0.0) | 6 (6.7) | 0 (0.0) | 3 (5.6) | 2 (5.4) | 1 (2.4) | 1 (2.7) | 0 (0.0) |
| Other | 0 (0.0) | 1 (1.1) | 0 (0.0) | 0 (0.0) | 1 (2.7) | 0 (0.0) | 0 (0.0) | 1 (2.2) |
| P-CATe (score 13–65), mean (SD) | 51.2 (5.44) | 50.0 (7.09) | 51.9 (6.27) | 51.2 (7.13) | 52.3 (5.00) | 49.3 (6.84) | 50.5 (6.42) | 50.4 (7.43) |
| Residents | MoveMore + UC arm | UC arm | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CH1 | CH2 | CH3 | CH4 | CH5 | Total | CH6 | CH7 | CH8 | CH9 | CH10 | CH11 | CH12 | Total | |
| Number of residents screened | 12 | 25 | 34 | 29 | 26 | 126 | 39 | 13 | 39 | 20 | 31 | 15 | 17 | 174 |
| Eligible, n (% of screened) | 9 (75.0) | 24 (96.0) | 32 (94.1) | 24 (82.8) | 24 (92.3) | 113 (89.7) | 37 (94.9) | 12 (92.3) | 38 (97.4) | 19 (95.0) | 29 (93.5) | 15 (100.0) | 15 (88.2) | 165 (94.8) |
| Consent/assent given, n (% of eligible) | 8 (88.9) | 11 (45.8) | 15 (46.9) | 12 (50.0) | 18 (75.0) | 64 (56.6) | 15 (40.5) | 9 (75.0) | 18 (47.4) | 14 (73.7) | 22 (75.9) | 6 (40.0) | 11 (73.3) | 95 (57.6) |
| Registered, n (% of consented) | 6 (75.0) | 11 (100.0) | 15 (100.0) | 12 (100.0) | 18 (100.0) | 62 (96.9) | 15 (100.0) | 8 (88.9) | 18 (100.0) | 12 (85.7) | 22 (100.0) | 6 (100.0) | 10 (90.9) | 91 (95.8) |
| Followed up at 3 months, n (% of registered) | 4 (66.7) | 9 (81.8) | 14 (93.3) | 12 (100.0) | 15 (83.3) | 54 (87.1) | 0a | 7 (87.5) | 17 (94.4) | 11 (91.7) | 22 (100.0) | 4b (66.7) | 9b (90.0) | 70 (76.9) |
| Followed up at 6 months, n (% of registered) | 4 (66.7) | 9 (81.8) | 12 (80.0) | 12 (100.0) | 13 (72.2) | 50 (80.6) | 11 (73.3) | 7 (87.5) | 16 (88.9) | 9 (75.0) | 22 (100.0) | 3 (50.0) | 8 (80.0) | 76 (83.5) |
| Followed up at 9 months, n (% of registered) | 4c (66.7) | 8 (72.7) | 10 (66.7) | 10 (83.3) | 11 (61.1) | 43 (69.4) | 11 (73.3) | 6 (75.0) | 15 (83.3) | 8 (66.7) | 20 (90.9) | 3 (50.0) | 7 (70.0) | 70 (76.9) |
| Registered residents at baseline and profiles at follow-up | MoveMore + UC arm | UC arm | Difference in proportions (95% CI)a |
|---|---|---|---|
| Registered residents at baseline (N) | 62 | 91 | |
| 3-month follow-up (n) | 54 | 83b | –3.10 (–18.00 to 11.79) |
| Deaths, n (%) | 6 (9.7) | 6 (6.6) | 3.51 (–8.20 to 15.22) |
| Moved out of CH, n (%) | 2 (3.2) | 2 (2.2) | –0.40 (–7.73 to 6.92) |
| 6-month follow-up (n) | 50 | 76 | 0.90 (–18.20 to 20.00) |
| Deaths, n (%) | 2 (3.7) | 6 (7.2) | –6.45 (–17.29 to 4.40) |
| Moved out of CH, n (%) | 2 (3.7) | 1 (1.2) | 1.17 (–4.10 to 6.44) |
| 9-month follow-up (n) | 43 | 70 | –2.65 (–17.50 to 12.20) |
| Deaths, n (%) | 4 (8.0) | 4 (5.3) | 0.92 (–7.88 to 9.71) |
| Moved out of CH, n (%) | 3 (6.0) | 2 (2.6) | 3.44 (–3.26 to 10.15) |
| Cumulative over the 9 months’ follow-up (n) | 43 | 70 | |
| Deaths, n (%) | 12 (19.4) | 16 (17.6) | –0.22 (–13.1 to 12.70) |
| Moved out of CH, n (%) | 7 (11.3) | 5 (5.5) | 2.87 (–7.27 to 13.00) |
| Resident profile | Trial arm, median (IQR) | |
|---|---|---|
| MoveMore + UC | UC | |
| Baseline | ||
| Average number of permanent residents | 28 (25–29) | 32 (17–40) |
| Deaths | 4 (3–4) | 1 (1–3) |
| Moved into the CH in previous 3 months | – | – |
| Moved out of the CH in previous 3 months | – | – |
| 3-month follow-up | ||
| Average number of permanent residents | 28 (25–29) | 24.5 (16–41)a |
| Deaths | 2 (2–2) | 2 (1–2) |
| Moved into the CH in previous 3 months | 4 (3–5) | 1.5 (0–4) |
| Moved out of the CH in previous 3 months | 2 (2–3) | 0 (0–1) |
| 6-month follow-up | ||
| Average number of permanent residents | 28 (27–29) | 25 (16–39)a |
| Deaths | 0 (0–1) | 1 (0–2) |
| Moved into the CH in previous 3 months | 2 (1–3) | 1.5 (1–2) |
| Moved out of the CH in previous 3 months | 1 (1–4) | 1 (0–3) |
| 9-month follow-up | ||
| Average number of permanent residents | 26 (24–29) | 17 (17–35) |
| Deaths | 3 (2–4) | 1 (0–5) |
| Moved into the CH in previous 3 months | 4 (0–4) | 2 (0–2) |
| Moved out of the CH in previous 3 months | 2 (2–4) | 0 (0–2) |
| Characteristic | MoveMore + UC arm | UC arm | Overall |
|---|---|---|---|
| Screened residents (n) | 126 | 174 | 300 |
| Age (years), mean (SD) | 86.0 (9.42) | 86.5 (7.01) | 86.3 (8.10) |
| Sex, n (%) | |||
| Female | 103 (81.7) | 137 (78.7) | 240 (80.0) |
| Male | 23 (18.3) | 37 (21.3) | 60 (20.0) |
| Dementia,a n (%) | |||
| Yes | 80 (63.5) | 114 (65.9) | 194 (64.9) |
| No | 46 (36.5) | 59 (34.1) | 105 (35.1) |
| Previous stroke,a n (%) | |||
| Yes | 22 (17.5) | 18 (10.4) | 40 (13.4) |
| No | 104 (82.5) | 155 (89.6) | 259 (86.6) |
| Registered blind,a n (%) | |||
| Yes | 5 (4.0) | 12 (6.9) | 17 (5.7) |
| No | 121 (96.0) | 161 (93.1) | 282 (94.3) |
| Resident ethnicity, n (%) | |||
| White | 124 (98.4) | 173 (99.4) | 297 (99.0) |
| Asian | 2 (1.6) | 0 (0.0) | 2 (0.7) |
| Other ethnic group | 0 (0.0) | 1 (0.6) | 1 (0.3) |
| Length of stayb | |||
| Mean (SD) | 30.0 (34.52) | 30.8 (32.96) | 30.5 (33.57) |
| Median (IQR) | 18.0 (8.0–42.0) | 18.0 (7.0–43.0) | 18.0 (7.0–42.0) |
| Funding type,c n (%) | |||
| Continuing health care | 0 (0.0) | 2 (1.5) | 2 (0.9) |
| Local authority | 63 (67.0) | 67 (50.0) | 130 (57.0) |
| Local authority and self-funded | 2 (2.1) | 0 (0.0) | 2 (0.9) |
| Self-funded | 29 (30.9) | 65 (48.5) | 94 (41.2) |
| BI scored (score 0–20) | |||
| Mean (SD) | 9.0 (5.20) | 10.9 (6.09) | 10.1 (5.80) |
| PAM-RCe (score 0–21), mean (SD) | |||
| Total score | 8.7 (5.15) | 11.0 (5.56) | 10.0 (5.50) |
| Ability domain score | 5.6 (2.84) | 6.8 (3.03) | 6.3 (3.00) |
| Activity domain score | 3.1 (2.63) | 4.2 (2.97) | 3.8 (2.89) |
| Characteristic | Consented (n = 159) | Did not consent (n = 119) | Overall (eligible) (N = 278) |
|---|---|---|---|
| Age (years), mean (SD) | 86.3 (7.09) | 87.0 (7.85) | 86.6 (7.42) |
| Sex, n (%) | |||
| Female | 128 (80.5) | 97 (81.5) | 225 (80.9) |
| Male | 31 (19.5) | 22 (18.5) | 53 (19.1) |
| Dementia,a n (%) | |||
| Yes | 111 (69.8) | 70 (59.3) | 181 (65.3) |
| No | 48 (30.2) | 48 (40.7) | 96 (34.7) |
| Previously had a stroke,a n (%) | |||
| Yes | 24 (15.1) | 14 (11.9) | 38 (13.7) |
| No | 135 (84.9) | 104 (88.1) | 239 (86.3) |
| Registered blind,a n (%) | |||
| Yes | 6 (3.8) | 7 (5.9) | 13 (4.7) |
| No | 153 (96.2) | 111 (94.1) | 264 (95.3) |
| Resident ethnicity, n (%) | |||
| White | 158 (99.4) | 117 (98.3) | 275 (98.9) |
| Asian | 1 (0.6) | 1 (0.8) | 2 (0.7) |
| Other ethnic group | 0 (0.0) | 1 (0.8) | 1 (0.4) |
| Length of stay in the CH (months)a | |||
| Mean (SD) | 30.6 (35.48) | 30.2 (31.92) | 30.4 (33.95) |
| Median (IQR) | 17.0 (7.0–42.0) | 18.0 (7.0–42.0) | 18.0 (7.0–42.0) |
| Funding type,b n (%) | |||
| Continuing health care | 1 (0.8) | 0 (0.0) | 1 (0.5) |
| Local authority | 70 (55.6) | 51 (58.6) | 121 (56.8) |
| Local authority and self-funded | 2 (1.6) | 0 (0.0) | 2 (0.9) |
| Self-funded | 53 (42.1) | 36 (41.4) | 89 (41.8) |
| BI scorec (score 0–20) | |||
| Mean (SD) | 10.6 (5.61) | 10.1 (5.74) | 10.4 (5.66) |
| PAM-RCd (score 0–21), mean (SD) | |||
| Total score | 10.6 (5.37) | 9.9 (5.26) | 10.3 (5.32) |
| Ability domain score | 6.6 (2.89) | 6.2 (2.84) | 6.4 (2.87) |
| Activity domain score | 4.0 (2.83) | 3.7 (2.87) | 3.9 (2.85) |
| Residents | MoveMore + UC arm (N = 62) | UC arm (N = 91) | Overall (N = 153) |
|---|---|---|---|
| Age (years), mean (SD) | 87.1 (6.59) | 85.7 (7.35) | 86.2 (7.06) |
| Sex: female, n (%) | 51 (82.3) | 71 (78.0) | 122 (79.7) |
| Diagnosis of dementia, n (%) | 43 (69.4) | 64 (70.3) | 107 (69.9) |
| Previous history of stroke, n (%) | 14 (22.6) | 10 (11.0) | 24 (15.7) |
| Registered blind, n (%) | 1 (1.6) | 5 (5.5) | 6 (3.9) |
| Ethnicity, n (%) | |||
| White | 61 (98.4) | 91 (100.0) | 152 (99.3) |
| Asian | 1 (1.6) | 0 (0.0) | 1 (0.7) |
| Other ethnic group | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Length of stay in the CH (months) | |||
| Mean (SD) | 31.2 (36.82) | 29.2 (33.77) | 30.0 (34.93) |
| Median (IQR) | 16.5 (8.0–42.0) | 17.0 (7.0–37.0) | 17.0 (7.0–41.0) |
| Funding type,a n (%) | |||
| Continuing health care | 0 (0.0) | 1 (1.3) | 1 (0.8) |
| Local authority | 26 (59.1) | 39 (51.3) | 65 (54.2) |
| Local authority and self-funded | 2 (4.5) | 0 (0.0) | 2 (1.7) |
| Self-funded | 16 (36.4) | 36 (47.4) | 52 (43.3) |
| FAC,b n (%) | |||
| 0 – Non-functional ambulation | 14 (22.6) | 18 (20.0) | 32 (21.1) |
| 1 – Ambulatory dependent for physical assistance (level II) | 8 (12.9) | 3 (3.3) | 11 (7.2) |
| 2 – Ambulatory dependent for physical assistance (level I) | 7 (11.3) | 8 (8.9) | 15 (9.9) |
| 3 – Ambulatory dependent for supervision | 11 (17.7) | 4 (4.4) | 15 (9.9) |
| 4 – Ambulatory independent level surfaces only | 12 (19.4) | 32 (35.6) | 44 (28.9) |
| 5 – Ambulatory independent | 10 (16.1) | 25 (27.8) | 35 (23.0) |
| EMS scoreb (score 0–20) | |||
| Mean (SD) | 9.3 (6.81) | 10.7 (6.69) | 10.2 (6.75) |
| Median (IQR) | 12.0 (3.0–15.0) | 13.0 (4.0–16.0) | 13.0 (4.0–16.0) |
| BI scorec (score 0–20), mean (SD) | 9.2 (4.87) | 11.6 (5.96) | 10.6 (5.65) |
| PAM-RC scored (score 0–21), mean (SD) | |||
| Total score | 9.1 (4.92) | 11.5 (5.45) | 10.5 (5.36) |
| Ability domain score | 5.9 (2.75) | 7.1 (2.95) | 6.6 (2.92) |
| Activity domain score | 3.2 (2.42) | 4.5 (2.91) | 4.0 (2.79) |
| GDS scoree | |||
| Mean (SD) | 4.1 (3.11) | 3.9 (3.07) | 4.0 (3.07) |
| Median (IQR) | 4.0 (2.0–6.0) | 3.0 (1.5–5.0) | 3.5 (2.0–5.0) |
| WHOQOL-OLD score,f mean (SD) | |||
| Question 1 | 3.5 (1.04) | 3.1 (1.43) | 3.3 (1.27) |
| Question 2 | 3.7 (0.77) | 3.3 (1.19) | 3.5 (1.02) |
| Question 3 | 3.5 (0.90) | 2.9 (1.19) | 3.2 (1.09) |
| DEMQOL,g mean (SD) | |||
| Resident completed (score 0–112) | 90.5 (13.56) | 93.3 (11.35) | 92.0 (12.43) |
| 29th score | 2.3 (0.58) | 2.2 (0.88) | 2.2 (0.75) |
| Proxy completed (score 0–124) | 96.6 (9.31) | 97.2 (8.70) | 96.8 (9.07) |
| 32nd score | 2.0 (0.66) | 2.1 (0.63) | 2.1 (0.64) |
| EQ-5D-5L,h mean (SD) | |||
| Resident completed | 0.75 (0.23) | 0.80 (0.22) | 0.77 (0.23) |
| Visual analogue score | 70.6 (18.74) | 69.5 (21.07) | 70.0 (19.96) |
| Proxy completed | 0.60 (0.26) | 0.69 (0.24) | 0.65 (0.25) |
| Visual analogue score | 73.8 (16.62) | 71.3 (20.02) | 72.3 (18.73) |
| 6-CIT score,i mean (SD) | 18.6 (8.12) | 16.4 (8.27) | 17.4 (8.21) |
| Medical history | Trial arm, n (%) | Overall (N = 153), n (%) | |
|---|---|---|---|
| MoveMore + UC (N = 62) | UC (N = 91) | ||
| Dementia or Alzheimer’s disease | 45 (72.6) | 64 (70.3) | 109 (71.2) |
| Cerebrovascular disease or transient ischaemic disease | 16 (25.8) | 10 (11.0) | 26 (17.0) |
| Rheumatic or connective tissue disease | 18 (29.0) | 0 (0.0) | 18 (13.3) |
| Diabetes | 12 (19.4) | 8 (8.8) | 20 (13.1) |
| Cancer (lymphoma, leukaemia, solid tumour) | 10 (16.1) | 5 (5.5) | 15 (9.8) |
| Congestive heart failure | 9 (14.5) | 6 (6.6) | 15 (9.8) |
| Renal disease | 11 (17.7) | 4 (4.4) | 15 (9.8) |
| Pulmonary disease | 7 (11.3) | 6 (6.6) | 13 (8.5) |
| Gastric or peptic ulcer | 5 (8.1) | 1 (1.1) | 6 (3.9) |
| Peripheral vascular disease or bypass | 3 (4.8) | 3 (3.3) | 6 (3.9) |
| Hemiplegia | 5 (8.1) | 0 (0.0) | 5 (3.3) |
| Metastatic solid tumour | 3 (4.8) | 1 (1.1) | 4 (2.6) |
| Myocardial infarction | 2 (3.2) | 2 (2.2) | 4 (2.6) |
| Diabetes with end organ damage | 2 (3.2) | 0 (0.0) | 2 (1.3) |
| HIV or AIDS | 0 (0.0) | 1 (1.1) | 1 (0.7) |
| Mild liver disease | 1 (1.6) | 0 (0.0) | 1 (0.7) |
| Characteristic | Residents completing follow-up (N = 113) | Residents not completing follow-up (N = 40) |
|---|---|---|
| Age (years), mean (SD) | 86.4 (6.59) | 85.7 (8.33) |
| Sex, n (%) | ||
| Female | 94 (83.2) | 28 (70.0) |
| Male | 19 (16.8) | 12 (30.0) |
| Dementia, n (%) | ||
| Yes | 76 (67.3) | 31 (77.5) |
| No | 37 (32.7) | 9 (22.5) |
| Previously had a stroke, n (%) | ||
| Yes | 20 (17.7) | 4 (10.0) |
| No | 93 (82.3) | 36 (90.0) |
| Registered blind, n (%) | ||
| Yes | 4 (3.5) | 2 (5.0) |
| No | 109 (96.5) | 38 (95.0) |
| Resident ethnicity, n (%) | ||
| White | 112 (99.1) | 40 (100.0) |
| Asian | 1 (0.9) | 0 (0.0) |
| Length of stay in the CH (months) | ||
| Mean (SD) | 29.8 (33.66) | 30.8 (38.74) |
| Median (IQR) | 17.0 (8.0–37.0) | 15.0 (4.5–42.5) |
| Funding type,a n (%) | ||
| Continuing health care | 0 (0) | 1 (3.4) |
| Local authority | 49 (53.8) | 16 (55.2) |
| Local authority and self-funded | 1 (1.1) | 1 (3.4) |
| Self-funded | 41 (45.1) | 11 (37.9) |
| FAC,b n (%) | ||
| 0 – Non-functional ambulation | 22 (19.5) | 10 (25.6) |
| 1 – Ambulatory dependent for physical assistance (level II) | 7 (6.2) | 4 (10.3) |
| 2 – Ambulatory dependent for physical assistance (level I) | 10 (8.8) | 5 (12.8) |
| 3 – Ambulatory dependent for supervision | 13 (11.5) | 2 (5.1) |
| 4 – Ambulatory independent level surfaces only | 35 (31.0) | 9 (23.1) |
| 5 – Ambulatory independent | 26 (23.0) | 9 (23.1) |
| EMS scorec (score 0–20) | ||
| Mean (SD) | 10.5 (6.66) | 9.2 (7.01) |
| Median (IQR) | 13.0 (4.0–16.0) | 11.0 (2.0–16.0) |
| BI scored (score 0–20), mean (SD) | 10.9 (5.71) | 9.7 (5.46) |
| PAM-RC scoree (score 0–21), mean (SD) | ||
| Total score | 10.7 (4.96) | 10.2 (6.43) |
| Ability domain score | 6.7 (2.82) | 6.2 (3.19) |
| Activity domain score | 3.9 (2.49) | 4.1 (3.53) |
| GDS scoref (score 0–15) | ||
| Mean (SD) | 3.6 (2.80) | 5.2 (3.72) |
| Median (IQR) | 3.0 (2.0–5.0) | 5.0 (2.0–7.0) |
| WHOQOL-OLD,g mean (SD) | ||
| Q1. Enough to do each day | 3.3 (1.28) | 3.3 (1.30) |
| Q2. Satisfied with use of time | 3.5 (1.05) | 3.3 (0.90) |
| Q3. Satisfied with level of activity | 3.3 (1.02) | 2.9 (1.33) |
| DEMQOL score,h mean (SD) | ||
| Resident completed (score 0–112) | 92.8 (12.45) | 88.4 (12.24) |
| Proxy completed (score 0–124) | 97.7 (8.53) | 94.8 (10.15) |
| EQ-5D-5Li (resident completed) (score –0.281 to 1.000), mean (SD) | 0.80 (0.21) | 0.70 (0.26) |
| 6-CITj (score 0–28), mean (SD) | 16.8 (8.32) | 19.2 (7.82) |
Intervention delivery
| Implementation detail | CH1 | CH2 | CH3, visit 1 | CH3, visit 2a | CH4 | CH5 |
|---|---|---|---|---|---|---|
| Workshop details | ||||||
| Workshop went ahead on planned dateb | No | No | No | Yes | Yes | Yes |
| Did another workshop take place? | Yes | Yes | Yes | – | – | – |
| Duration of workshop | 2 h 30 min | 2 h 15 min | 1 h 30 min | 1 h 30 min | 1 h 45 min | 2 h 00 min |
| Location | CH | CH | CH | CH | CH | External |
| Physiotherapist present | Yes | Yes | No | No | Yes | Yes |
| Workshop content | ||||||
| Pre-workshop preparation completed | Yes | Yes | Yes | No | Yes | Yes |
| Observation tool covered | Yes | Yes | Yes | Yes | Yes | Yes |
| Observation tool practised | No | No | No | No | No | No |
| Intervention folder provided | Yes | Yes | Yes | Noc | Yes | Yes |
| Attendance | ||||||
| Number of attendees | 5 | 5 | 6 | 8 | 5 | 8 |
| MoveMore lead present | Yes | Yes | Yes | No | Yes | Yes |
| Type of attendee, n (%) | ||||||
| Resident or relative | 1 (20.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Staff | 4 (80.0) | 5 (100.0) | 6 (100.0) | 8 (100.0) | 5 (100.0) | 8 (100.0) |
| Type of staff,d n (%) | ||||||
| Permanent | 4 (100.0) | 5 (100.0) | 5 (83.3) | 5 (83.3) | 2 (40.0) | 8 (100.0) |
| Bank | 0 (0.0) | 0 (0.0) | 1 (16.7) | 1 (16.7) | 0 (0.0) | 0 (0.0) |
| Agency | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Role of attendee (for staff), n (%) | ||||||
| Administration | 0 (0.0) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) | 1 (12.5) |
| Ancillary | 1 (25.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (20.0) | 2 (25.0) |
| Nurse | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (12.5) | 0 (0.0) | 0 (0.0) |
| Carer/care assistant | 2 (50.0) | 3 (60.0) | 2 (33.3) | 7 (87.5) | 2 (40.0) | 1 (12.5) |
| Specialist clinical role | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Specialist non-clinical role | 0 (0.0) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) | 1 (12.5) |
| Manager/deputy manager | 1 (25.0) | 2 (40.0) | 1 (16.7) | 0 (0.0) | 2 (40.0) | 2 (25.0) |
| Team leader | 0 (0.0) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) | 1 (12.5) |
| Implementation detail | CH1 | CH2 | CH3 | CH4 | CH5 |
|---|---|---|---|---|---|
| Workshop details | |||||
| Did workshop go ahead on planned date? | Yes | No | Yes | Yes | Yes |
| Did another workshop take place? | – | Yes | – | – | – |
| Duration of workshop | 1 h 45 min | 1 h 45 min | 1 h 30 min | 1 h 30 min | 2 h 00 min |
| Location | CH | CH | CH | CH | External |
| Intervention providers | |||||
| Artist present | No | Yes | No | No | No |
| Physiotherapist present | No | No | No | No | Yes |
| Observation and reflection | |||||
| Observation and reflection sheets brought to workshop 2 | Yes | Yes | Yes | Yes | Yes |
| Number of observation sheets completed | 9 | 10 | 3 | 5 | 11 |
| Number of reflection sheets completed | 9 | 0 | 3 | 1 | 11 |
| Workshop content | |||||
| Review of observations | Yes | Yes | Yes | Yes | Yes |
| Introduction to action-planning and review | Yes | Yes | Yes | Yes | Yes |
| Action-planning and review tool | Yes | Yes | Yes | Yes | Yes |
| Use of action plan examples | Yes | Yes | Yes | Yes | Yes |
| Action plans completed during workshop 2 | No | Yes | No | No | No |
| Dissemination of MoveMore | Yes | Yes | Yes | Yes | Yes |
| Attendance | |||||
| Number of attendees | 3 | 5 | 3 | 3 | 8 |
| MoveMore lead present | Yes | Yes | Yes | No | Yes |
| Type of attendee, n (%) | |||||
| Resident or relative | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Staff | 3 (100.0) | 5 (100.0) | 3 (100.0) | 3 (60.0) | 8 (100.0) |
| Type of staff, n (%) | |||||
| Permanent | 3 (100.0) | 5 (100.0) | 3 (100.0) | 3 (100.0) | 6 (75.0) |
| Bank | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Agency | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (25.0) |
| Role of attendee (for staff), n (%) | |||||
| Administration | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (12.5) |
| Ancillary | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (33.3) | 2 (25.0) |
| Nurse | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Carer/care assistant | 2 (66.7) | 3 (60.0) | 2 (66.7) | 0 (0.0) | 1 (12.5) |
| Specialist clinical role | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Specialist non-clinical role | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (12.5) |
| Manager/deputy manager | 1 (33.3) | 2 (40.0) | 0 (0.0) | 2 (66.7) | 2 (25.0) |
| Team leader | 0 (0.0) | 0 (0.0) | 1 (33.3) | 0 (0.0) | 0 (0.0) |
| Executive director | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (12.5) |
| Implementation detail | CH1 | CH2 | CH3, visit 1 | CH3, visit 2 | CH4 | CH5 |
|---|---|---|---|---|---|---|
| Workshop details | ||||||
| Did workshop go ahead on planned date? | Yes | Yes | No | Yes | Yes | Yes |
| Did another workshop take place? | – | – | Yes | – | – | |
| Duration of workshop | 1 h 15 min | 1 h 00 min | 1 h 00 min | 1h 30 min | 0 h 45 min | 2 h 00 min |
| Location | CH | CH | CH | CH | CH | External |
| Artist present | Yes | No | No | Yes | Yes | Yes |
| Internal MoveMore meetings since workshop 2 | No | Yes | No | Yes | No | Yes |
| Observation and reflection | ||||||
| Observation and reflection sheets brought to workshop 3 | No | Yes | Yes | No | Yes | Yes |
| Number of observation sheets completed | – | 10 | 3 | – | 1 | 13 |
| Number of reflection sheets completed | – | 0 | 0 | – | 1 | 13 |
| Workshop content | ||||||
| Number of completed action plans brought to workshop 3 | 0 | 0 | 3 | 0 | 2 | 7 |
| Number of completed review sheets brought to workshop 3 | 0 | 0 | 3 | 0 | 0 | 0 |
| Ideas bank used | Not known | Not known | No | No | Not known | Yes |
| Use of ideas not part of the ideas bank | Yes | Not known | Yes | No | Not known | Yes |
| Attendance | ||||||
| Number of attendees | 3 | 3 | 2 | 4 | 2 | 6 |
| MoveMore lead present | Yes | Yes | Yes | Yes | Yes | Yes |
| Type of attendee, n (%) | ||||||
| Resident or relative | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Staff | 3 (100.0) | 3 (100.0) | 2 (100.0) | 4 (100.0) | 2 (100.0) | 6 (100.0) |
| Type of staff, n (%) | ||||||
| Permanent | 3 (100.0) | 3 (100.0) | 2 (100.0) | 4 (100.0) | 2 (100.0) | 6 (100.0) |
| Bank | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Agency | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Role of attendee (for staff), n (%) | ||||||
| Administration | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (16.7) |
| Ancillary | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (33.3) |
| Nurse | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Carer/care assistant | 2 (66.7) | 2 (66.7) | 1 (50.0) | 3 (75.0) | 0 (0.0) | 1 (16.7) |
| Specialist clinical role | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Specialist non-clinical role | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (16.7) |
| Manager/deputy manager | 1 (33.3) | 1 (33.3) | 0 (0.0) | 0 (0.0) | 2 (100.0) | 1 (16.7) |
| Team leader | 0 (0.0) | 0 (0.0) | 1 (50.0) | 1 (25.0) | 0 (0.0) | 0 (0.0) |
| Time point | MoveMore + UC arm | UC arm | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CH1 | CH2 | CH3 | CH4 | CH5 | CH6a | CH7 | CH8 | CH9 | CH10 | CH11 | CH12a | |
| 3-month follow-up | ||||||||||||
| Number of staff with face-to-face contact with residentsb | 60 | 43 | 32 | 18 | 35 | – | – | 57 | 15 | – | 52 | 27 |
| Staff joining in the previous 3 months, n (%) | 3 (5.0) | 2 (4.6) | 4 (12.5) | 1 (5.6) | 4 (11.4) | – | 2 | 2 (3.5) | 4 (26.7) | 0 | 2 (3.8) | 1 (3.7) |
| Staff leaving in the previous 3 months, n (%) | 2 (3.3) | 2 (4.6) | 1 (3.1) | 1 (5.6) | 2 (5.7) | – | 2 | 0 (0.0) | 1 (6.7) | 1 | 2 (3.8) | 0 (0.0) |
| 6-month follow-up | ||||||||||||
| Number of staff with face-to-face contact with residentsb | 72 | 36 | 26 | 17 | 40 | 55 | 16 | 68 | 14 | 40 | – | 24 |
| Staff joining in the previous 3 months, n (%) | 0 (0.0) | 5 (13.9) | 2 (7.7) | 0 (0.0) | 1 (2.5) | 5 (9.1) | 2 (12.5) | 1 (1.5) | 3 (21.4) | 2 (5.0) | – | 1 (4.2) |
| Staff leaving in the previous 3 months, n (%) | 1 (1.4) | 3 (8.3) | 2 (7.7) | 1 (5.9) | 0 (0.0) | 2 (3.6) | 0 (0.0) | 0 (0.0) | 2 (14.3) | 2 (5.0) | – | 1 (4.2) |
| 9-month follow-up | ||||||||||||
| Number of staff with face-to-face contact with residentsb | 59 | 39 | 31 | 20 | 38 | 46 | 15 | 53 | 15 | – | 9 | 25 |
| Staff joining in the previous 3 months, n (%) | 0 (0.0) | 2 (5.1) | 3 (9.7) | 3 (15.0) | 0 (0.0) | 2 (4.3) | 1 (6.7) | 0 (0.0) | 3 (20.0) | 2 | 0 (0.0) | 0 (0.0) |
| Staff leaving in the previous 3 months, n (%) | 0 (0.0) | 3 (7.7) | 2 (6.4) | 2 (10.0) | 0 (0.0) | 1 (2.2) | 0 (0.0) | 2 (3.8) | 2 (13.3) | 0 | 1 (11.1) | 0 (0.0) |
| Baseline | 3-month follow-up | 6-month follow-up | 9-month follow-up | |||||
|---|---|---|---|---|---|---|---|---|
| MoveMore + UC arm | UC arm | MoveMore + UC arm | UC arm | MoveMore + UC arm | UC arm | MoveMore + UC arm | UC arm | |
| Number of CHs | 5 | 7 | 5 | 6a | 5 | 6a | 5 | 7 |
| Taking part in initiatives to enhance care, n (%) | ||||||||
| Yes | 1 (20.0) | 2 (28.6) | 2 (40.0) | 1 (16.7) | 2 (40.0) | 2 (33.3) | 1 (20.0) | 1 (14.3) |
| No | 4 (80.0) | 5 (71.4) | 3 (60.0) | 5 (83.3) | 3 (60.0) | 4 (66.7) | 4 (80.0) | 6 (85.7) |
| AO in post, , n (%) | ||||||||
| Yes | 3 (60.0) | 5 (71.4) | 4 (80.0) | 4 (66.7) | 4 (80.0) | 5 (83.3) | 4 (80.0) | 6 (85.7) |
| No | 2 (40.0) | 2 (28.6) | 1 (20.0) | 2 (33.3) | 1 (20.0) | 1 (16.7) | 1 (20.0) | 1 (14.3) |
| Display of materials related to movement, n (%) | ||||||||
| Yesb | 3 (75.0) | 3 (50.0) | 3 (60.0) | 3 (42.9) | 2 (40.0) | 3 (42.9) | ||
| No | 1 (25.0) | 3 (50.0) | 2 (40.0) | 4 (57.1) | 3 (60.0) | 4 (57.1) | ||
Assessment of outcome measures
| Questionnaire | Baseline | 3-month follow-up | 6-month follow-up | 9-month follow-up | ||||
|---|---|---|---|---|---|---|---|---|
| MoveMore + UC arm | UC arm | MoveMore + UC arm | UC arm | MoveMore + UC arm | UC arm | MoveMore + UC arm | UC arm | |
| Number of consenting residents | 62 | 91 | 54 | 70a | 50 | 76 | 43 | 70 |
| FACb | ||||||||
| Questionnaire completion, n (%) | ||||||||
| Completed | 62 (100.0) | 90 (98.9) | 52 (96.3) | 70 (100.0) | 50 (100.0) | 76 (100.0) | 42 (97.7) | 70 (100.0) |
| Not completed | 0 (0.0) | 1 (1.1) | 2 (3.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (2.3) | 0 (0.0) |
| Time taken to complete (minutes), n | 42 | 75 | 45 | 70 | 50 | 40 | 31 | 58 |
| Mean time (SD) | 1.3 (0.45) | 1.6 (0.74) | 1.5 (1.42) | 1.3 (0.56) | 1.5 (0.58) | 1.5 (0.78) | 1.3 (0.44) | 1.1 (0.68) |
| Median time (IQR) | 1.0 (1.0–2.0) | 1.0 (1.0–2.0) | 1.0 (1.0–2.0) | 1.0 (1.0–1.0) | 1.0 (1.0–2.0) | 1.0 (1.0–2.0) | 1.0 (1.0–2.0) | 1.0 (1.0–1.0) |
| EMS | ||||||||
| Questionnaire completion, n (%) | ||||||||
| Completed | 52 (83.9) | 82 (90.1) | 46 (85.2) | 68 (97.1) | 49 (98.0) | 61 (80.3) | 37 (86.0) | 57 (81.4) |
| Partially completed | 10 (16.1) | 8 (8.8) | 6 (11.1) | 2 (2.9) | 1 (2.0) | 12 (15.8) | 5 (11.6) | 12 (17.1) |
| Not completed | 0 (0.0) | 1 (1.1) | 2 (3.7) | 0 (0.0) | 0 (0.0) | 3 (3.9) | 1 (2.3) | 1 (1.4) |
| Prorated,c n (%) | 10 (100.0) | 8 (100.0) | 6 (100.0) | 2 (100.0) | 1 (100.0) | 10 (83.3) | 5 (100.0) | 11 (91.7) |
| Missing scores,c n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (16.7) | 0 (0.0) | 1 (8.3) |
| Time taken to complete (minutes), n | 41 | 75 | 46 | 69 | 49 | 40 | 31 | 57 |
| Mean time (SD) | 3.1 (1.56) | 4.0 (2.45) | 4.3 (4.11) | 3.5 (2.00) | 2.7 (1.32) | 3.5 (2.41) | 3.4 (2.33) | 2.5 (1.59) |
| Median time (IQR) | 3.0 (2.0–4.0) | 3.0 (2.0–5.0) | 2.0 (2.0–5.0) | 3.0 (2.0–5.0) | 2.0 (2.0–4.0) | 3.0 (2.0–4.5) | 2.0 (2.0–6.0) | 2.0 (1.0–3.0) |
| BI | ||||||||
| Questionnaire completion, n (%) | ||||||||
| Completed | 59 (95.2) | 90 (98.9) | 52 (96.3) | 66 (94.3) | 46 (92.0) | 67 (88.2) | 38 (88.4) | 62 (88.6) |
| Partially completed | 3 (4.8) | 1 (1.1) | 0 (0.0) | 4 (5.7) | 4 (8.0) | 7 (9.2) | 4 (9.3) | 7 (10.0) |
| Not completed | 0 (0.0) | 0 (0.0) | 2 (3.7) | 0 (0.0) | 0 (0.0) | 2 (2.6) | 1 (2.3) | 1 (1.4) |
| Prorated,c n (%) | 3 (100.0) | 1 (100.0) | – | 4 (100.0) | 4 (100.0) | 6 (85.7) | 4 (100.0) | 7 (100.0) |
| Missing scores,c n (%) | 0 (0.0) | 0 (0.0) | – | 0 (0.0) | 0 (0.0) | 1 (14.3) | 0 (0.0) | 0 (0.0) |
| Time taken to complete (minutes), n | 46 | 70 | 50 | 40 | 30 | 59 | ||
| Mean time (SD) | 2.4 (0.93) | 1.8 (0.54) | 2.3 (0.67) | 2.4 (1.48) | 2.0 (0.56) | 1.9 (0.85) | ||
| Median time (IQR) | 2.0 (2.0–3.0) | 2.0 (1.0–2.0) | 2.0 (2.0–3.0) | 2.0 (2.0–2.5) | 2.0 (1.0–2.0) | 2.0 (2.0–2.0) | ||
| PAM-RC | ||||||||
| Questionnaire completion, n (%) | ||||||||
| Completed | 62 (100.0) | 91 (100.0) | 51 (94.4) | 69 (98.6) | 50 (100.0) | 75 (98.7) | 42 (97.7) | 63 (90.0) |
| Partially completedd | 0 (0.0) | 0 (0.0) | 1 (1.9) | 1 (1.4) | 0 (0.0) | 1 (1.3) | 0 (0.0) | 6 (8.6) |
| Not completed | 0 (0.0) | 0 (0.0) | 2 (3.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (2.3) | 1 (1.4) |
| Time taken to complete (minutes), n | 47 | 70 | 50 | 40 | 31 | 58 | ||
| Mean time (SD) | 2.4 (0.77) | 1.8 (0.52) | 2.2 (0.51) | 2.5 (0.85) | 2.4 (3.30) | 2.1 (1.00) | ||
| Median time (IQR) | 2.0 (2.0–3.0) | 2.0 (1.0–2.0) | 2.0 (2.0–2.0) | 2.0 (2.0–3.0) | 2.0 (2.0–2.0) | 2.0 (2.0–2.0) | ||
| Questionnaire items | Baseline | 3-month follow-up | 6-month follow-up | 9-month follow-up | ||||
|---|---|---|---|---|---|---|---|---|
| MoveMore + UC | UC | MoveMore + UC | UC | MoveMore + UC | UC | MoveMore + UC | UC | |
| EMS items completed | ||||||||
| Number of residents | 62 | 90 | 52 | 70 | 50 | 73 | 42 | 69 |
| Items complete, n (%) | ||||||||
| 1. Lying to sitting | 62 (100.0) | 90 (100.0) | 52 (100.0) | 70 (100.0) | 50 (100.0) | 72 (98.6) | 42 (100.0) | 69 (100.0) |
| 2. Sitting to lying | 62 (100.0) | 90 (100.0) | 52 (100.0) | 70 (100.0) | 49 (98.0) | 72 (98.6) | 42 (100.0) | 69 (100.0) |
| 3. Sit to stand | 62 (100.0) | 89 (98.9) | 52 (100.0) | 70 (100.0) | 50 (100.0) | 72 (98.6) | 41 (97.6) | 67 (97.1) |
| 4. Stand | 62 (100.0) | 90 (100.0) | 52 (100.0) | 70 (100.0) | 49 (98.0) | 70 (95.9) | 40 (95.2) | 67 (97.1) |
| 5. Gait | 62 (100.0) | 89 (98.9) | 50 (96.2) | 70 (100.0) | 50 (100.0) | 70 (95.9) | 41 (97.6) | 67 (97.1) |
| 6. Timed walk | 53 (85.5) | 84 (93.3) | 47 (90.4) | 68 (97.1) | 50 (100.0) | 66 (90.4) | 39 (92.9) | 62 (89.9) |
| 7. Functional reach | 54 (87.1) | 84 (93.3) | 47 (90.4) | 68 (97.1) | 50 (100.0) | 65 (89.0) | 40 (95.2) | 59 (85.5) |
| BI items completed | ||||||||
| Number of residents | 62 | 91 | 52 | 70 | 50 | 74 | 42 | 69 |
| Items complete, n (%) | ||||||||
| Bowels | 62 (100.0) | 90 (98.9) | 52 (100.0) | 69 (98.6) | 50 (100.0) | 74 (100.0) | 42 (100.0) | 69 (100.0) |
| Bladder | 62 (100.0) | 91 (100.0) | 52 (100.0) | 70 (100.0) | 49 (98.0) | 74 (100.0) | 42 (100.0) | 69 (100.0) |
| Feeding | 62 (100.0) | 91 (100.0) | 52 (100.0) | 70 (100.0) | 49 (98.0) | 73 (98.6) | 41 (97.6) | 69 (100.0) |
| Grooming | 60 (96.8) | 91 (100.0) | 52 (100.0) | 68 (97.1) | 49 (98.0) | 73 (98.6) | 40 (95.2) | 64 (92.8) |
| Dressing | 61 (98.4) | 91 (100.0) | 52 (100.0) | 70 (100.0) | 50 (100.0) | 73 (98.6) | 42 (100.0) | 69 (100.0) |
| Transfer from bed to chair and back | 62 (100.0) | 91 (100.0) | 52 (100.0) | 70 (100.0) | 50 (100.0) | 71 (95.9) | 42 (100.0) | 69 (100.0) |
| Toilet use | 62 (100.0) | 91 (100.0) | 52 (100.0) | 69 (98.6) | 50 (100.0) | 73 (98.6) | 42 (100.0) | 68 (98.6) |
| Indoor mobility | 61 (98.4) | 91 (100.0) | 52 (100.0) | 70 (100.0) | 49 (98.0) | 72 (97.3) | 42 (100.0) | 69 (100.0) |
| Stairs | 62 (100.0) | 91 (100.0) | 52 (100.0) | 70 (100.0) | 50 (10.0) | 67 (90.5) | 42 (100.0) | 69 (100.0) |
| Bathing | 62 (100.0) | 91 (100.0) | 52 (100.0) | 70 (100.0) | 50 (10.0) | 72 (97.3) | 41 (97.6) | 68 (98.6) |
| PAM-RC items completed | ||||||||
| Number of residents | 62 | 91 | 52 | 70 | 50 | 76 | 42 | 69 |
| Items complete, n (%) | ||||||||
| Mobility | 62 (100.0) | 91 (100.0) | 52 (100.0) | 69 (98.6) | 50 (100.0) | 76 (100.0) | 42 (100.0) | 68 (98.6) |
| Balance | 62 (100.0) | 91 (100.0) | 52 (100.0) | 70 (100.0) | 50 (100.0) | 76 (100.0) | 42 (100.0) | 69 (100.0) |
| Walking frequency | 62 (100.0) | 91 (100.0) | 52 (100.0) | 70 (100.0) | 50 (100.0) | 76 (100.0) | 42 (100.0) | 69 (100.0) |
| Outdoor mobility | 62 (100.0) | 91 (100.0) | 52 (100.0) | 70 (100.0) | 50 (100.0) | 76 (100.0) | 42 (100.0) | 67 (97.1) |
| Wandering | 62 (100.0) | 91 (100.0) | 51 (98.1) | 70 (100.0) | 50 (100.0) | 75 (98.7) | 42 (100.0) | 66 (95.7) |
| Questionnaire | Baseline | 3-month follow-up | 6-month follow-up | 9-month follow-up | ||||
|---|---|---|---|---|---|---|---|---|
| MoveMore + UC | UC | MoveMore + UC | UC | MoveMore + UC | UC | MoveMore + UC | UC | |
| Number of consenting residents | 62 | 91 | 54 | 70a | 50 | 76 | 43 | 70 |
| GDS | ||||||||
| Questionnaire completion, n (%) | ||||||||
| Completed | 34 (54.8) | 41 (45.1) | 34 (63.0) | 28 (40.0) | 33 (66.0) | 31 (40.8) | 26 (60.5) | 29 (41.4) |
| Partially completed | 10 (16.1) | 6 (6.6) | 7 (13.0) | 5 (7.1) | 4 (8.0) | 7 (9.2) | 4 (9.3) | 3 (4.3) |
| Not completed | 18 (29.0) | 44 (48.4) | 13 (24.1) | 37 (52.9) | 13 (26.0) | 38 (50.0) | 13 (30.2) | 38 (54.3) |
| Prorated,b n (%) | 8 (80.0) | 3 (50.0) | 6 (85.7) | 5 (100.0) | 4 (100.0) | 6 (85.7) | 3 (75.0) | 3 (100.0) |
| Missing scores,b n (%) | 2 (20.0) | 3 (50.0) | 1 (14.3) | 0 (0.0) | 0 (0.0) | 1 (14.3) | 1 (25.0) | 0 (0.0) |
| Time taken to complete (minutes), n | 44 | 45 | 39 | 33 | 37 | 35 | 30 | 31 |
| Mean (SD) | 7.7 (4.45) | 8.6 (6.12) | 7.4 (3.10) | 5.6 (2.91) | 6.5 (3.30) | 8.0 (4.34) | 7.0 (3.78) | 8.2 (4.22) |
| Median (IQR) | 7.0 (5.0–9.0) | 5.0 (5.0–10.0) | 6.0 (5.0–10.0) | 5.0 (3.0–6.0) | 5.0 (4.0–8.0) | 7.0 (5.0–10.0) | 6.5 (4.0–8.0) | 8.0 (6.0–10.0) |
| WHOQOL-OLD questionnaire for elderly persons | ||||||||
| Questionnaire completion, n (%) | ||||||||
| Completed | 33 (53.2) | 35 (38.5) | 36 (66.7) | 24 (34.3) | 33 (66.0) | 32 (42.1) | 30 (69.8) | 32 (45.7) |
| Partially completedc | 3 (4.8) | 4 (4.4) | 2 (3.7) | 5 (7.1) | 3 (6.0) | 3 (3.9) | 0 (0.0) | 1 (1.4) |
| Not completed | 26 (41.9) | 52 (57.1) | 16 (29.6) | 41 (58.6) | 14 (28.0) | 41 (53.9) | 13 (30.2) | 37 (52.9) |
| Time taken to complete (minutes), n | 36 | 39 | 37 | 28 | 36 | 32 | 30 | 30 |
| Mean (SD) | 3.3 (2.50) | 3.5 (1.65) | 3.2 (1.47) | 3.0 (1.35) | 2.7 (0.92) | 3.2 (1.64) | 3.0 (1.07) | 2.5 (1.20) |
| Median (IQR) | 3.0 (2.0–3.0) | 3.0 (2.0–5.0) | 3.0 (2.0–4.0) | 3.0 (2.0–4.0) | 3.0 (2.0–3.0) | 3.0 (2.0–4.0) | 3.0 (2.0–3.0) | 2.0 (2.0–3.0) |
| DEMQOL | ||||||||
| Questionnaire completion, n (%) | ||||||||
| Completed | 29 (46.8) | 31 (34.1) | 32 (59.3) | 25 (35.7) | 32 (64.0) | 32 (42.1) | 25 (58.1) | 25 (35.7) |
| Partially completed | 7 (11.3) | 4 (4.4) | 5 (9.3) | 3 (4.3) | 5 (10.0) | 3 (3.9) | 6 (14.0) | 5 (7.1) |
| Not completed | 26 (41.9) | 56 (61.5) | 17 (31.5) | 42 (60.0) | 13 (26.0) | 41 (53.9) | 12 (27.9) | 40 (57.1) |
| Prorated,b n (%) | 2 (28.6) | 3 (75.0) | 3 (60.0) | 3 (100.0) | 4 (80.0) | 2 (67.7) | 4 (66.7) | 3 (60.0) |
| Missing scores,b n (%) | 5 (71.4) | 1 (25.0) | 2 (40.0) | 0 (0.0) | 1 (20.0) | 1 (33.3) | 2 (33.3) | 2 (40.0) |
| Time taken to complete (minutes), n | 35 | 35 | 37 | 28 | 37 | 31 | 31 | 27 |
| Mean (SD) | 13.0 (5.77) | 14.1 (11.43) | 12.1 (5.39) | 9.5 (4.09) | 11.7 (7.36) | 13.2 (9.31) | 11.6 (7.60) | 15.0 (8.43) |
| Median (IQR) | 12.0 (10.0–16.0) | 10.0 (5.0–22.0) | 13.0 (8.0–15.0) | 8.0 (6.0–13.5) | 10.0 (5.0–18.0) | 12.0 (6.0–19.0) | 10.0 (5.0–18.0) | 14.0 (8.0–19.0) |
| EQ-5D-5L | ||||||||
| Questionnaire completion, n (%) | ||||||||
| Completed | 42 (67.7) | 48 (52.7) | 38 (70.4) | 30 (42.9) | 37 (74.0) | 36 (47.4) | 29 (67.4) | 33 (47.1) |
| Partially completedc | 2 (3.2) | 5 (5.5) | 3 (5.6) | 4 (5.7) | 0 (0.0) | 0 (0.0) | 2 (4.7) | 2 (2.9) |
| Not completed | 18 (29.0) | 38 (41.8) | 13 (24.1) | 36 (51.4) | 13 (26.0) | 40 (52.6) | 12 (27.9) | 35 (50.0) |
| Time taken to complete (minutes), n | 44 | 48 | 39 | 32 | 37 | 32 | 31 | 32 |
| Mean (SD) | 5.7 (5.84) | 5.4 (4.05) | 4.4 (2.12) | 4.2 (2.18) | 3.8 (1.33) | 4.4 (1.86) | 4.2 (1.41) | 4.8 (1.93) |
| Median (IQR) | 4.5 (3.0–5.0) | 5.0 (3.0–6.5) | 4.0 (3.0–5.0) | 4.0 (3.0–5.0) | 3.0 (3.0–4.0) | 4.0 (3.0–5.0) | 4.0 (3.0–5.0) | 4.0 (3.5–5.5) |
| 6-CIT | ||||||||
| Questionnaire completion, n (%) | ||||||||
| Completed | 33 (53.2) | 36 (39.6) | 27 (50.0) | 23 (32.9) | 31 (62.0) | 26 (34.2) | 26 (60.5) | 23 (32.9) |
| Partially completedc | 10 (16.1) | 8 (8.8) | 13 (24.1) | 4 (5.7) | 5 (10.0) | 7 (9.2) | 4 (9.3) | 8 (11.4) |
| Not completed | 19 (30.6) | 47 (51.6) | 14 (25.9) | 43 (61.4) | 14 (28.0) | 43 (56.6) | 13 (30.2) | 39 (55.7) |
| Time taken to complete (minutes), n | 43 | 42 | 38 | 27 | 36 | 30 | 30 | 30 |
| Mean (SD) | 6.1 (3.39) | 7.0 (6.31) | 6.5 (2.55) | 5.1 (2.27) | 5.4 (2.20) | 6.3 (2.89) | 5.5 (2.80) | 6.7 (3.02) |
| Median (IQR) | 5.0 (5.0–6.0) | 5.0 (3.0–8.0) | 5.5 (5.0–8.0) | 5.0 (3.0–7.0) | 5.0 (4.0–6.5) | 6.0 (4.0–8.0) | 5.0 (4.0–7.0) | 6.0 (4.0–8.0) |
| Questionnaire | Baseline | 3-month follow-up | 6-month follow-up | 9-month follow-up | ||||
|---|---|---|---|---|---|---|---|---|
| MoveMore + UC | UC | MoveMore + UC | UC | MoveMore + UC | UC | MoveMore + UC | UC | |
| GDS | ||||||||
| Number of residents | 44 | 47 | 41 | 33 | 37 | 38 | 30 | 32 |
| Item, n (%) | ||||||||
| 1 | 44 (100.0) | 46 (97.9) | 40 (97.6) | 32 (97.0) | 37 (100.0) | 37 (97.4) | 30 (100.0) | 31 (96.9) |
| 2 | 44 (100.0) | 45 (95.7) | 41 (100.0) | 33 (100.0) | 37 (100.0) | 37 (97.4) | 29 (96.7) | 32 (100.0) |
| 3 | 43 (97.7) | 44 (93.6) | 41 (100.0) | 32 (97.0) | 37 (100.0) | 37 (97.4) | 29 (96.7) | 31 (96.9) |
| 4 | 43 (97.7) | 45 (95.7) | 41 (100.0) | 33 (100.0) | 37 (100.0) | 38 (100.0) | 29 (96.7) | 32 (100.0) |
| 5 | 43 (97.7) | 44 (93.6) | 41 (100.0) | 33 (100.0) | 36 (97.3) | 37 (97.4) | 29 (96.7) | 32 (100.0) |
| 6 | 41 (93.2) | 42 (89.4) | 40 (97.6) | 32 (97.0) | 37 (100.0) | 38 (100.0) | 28 (93.3) | 31 (96.9) |
| 7 | 41 (93.2) | 46 (97.9) | 41 (100.0) | 33 (100.0) | 37 (100.0) | 37 (97.4) | 29 (96.7) | 32 (100.0) |
| 8 | 41 (93.2) | 42 (89.4) | 39 (95.1) | 33 (100.0) | 37 (100.0) | 37 (97.4) | 28 (93.3) | 31 (96.9) |
| 9 | 39 (88.6) | 44 (93.6) | 38 (92.7) | 32 (97.0) | 37 (100.0) | 38 (100.0) | 27 (90.0) | 32 (100.0) |
| 10 | 42 (95.5) | 43 (91.5) | 38 (92.7) | 30 (90.9) | 36 (97.3) | 37 (97.4) | 29 (96.7) | 32 (100.0) |
| 11 | 39 (88.6) | 44 (93.6) | 41 (100.0) | 33 (100.0) | 36 (97.3) | 36 (94.7) | 28 (93.3) | 32 (100.0) |
| 12 | 39 (88.6) | 42 (89.4) | 37 (90.2) | 33 (100.0) | 37 (100.0) | 36 (94.7) | 29 (96.7) | 30 (93.8) |
| 13 | 42 (95.5) | 46 (97.9) | 39 (95.1) | 32 (97.0) | 37 (100.0) | 37 (97.4) | 30 (100.0) | 31 (96.9) |
| 14 | 40 (90.9) | 43 (91.5) | 37 (90.2) | 33 (100.0) | 36 (97.3) | 37 (97.4) | 28 (93.3) | 31 (96.9) |
| 15 | 38 (86.4) | 43 (91.5) | 39 (95.1) | 32 (97.0) | 36 (97.3) | 34 (89.5) | 27 (90.0) | 32 (100.0) |
| WHOQOL-OLD questionnaire for elderly persons | ||||||||
| Number of residents | 36 | 39 | 38 | 29 | 36 | 35 | 30 | 33 |
| Question, n (%) | ||||||||
| 1. Enough to do each day | 35 (97.2) | 39 (100.0) | 36 (94.7) | 26 (89.7) | 33 (91.7) | 33 (94.3) | 30 (100.0) | 32 (97.0) |
| 2. Satisfied with use of time | 34 (94.4) | 36 (92.3) | 38 (100.0) | 26 (89.7) | 36 (100.0) | 35 (100.0) | 30 (100.0) | 33 (100.0) |
| 3. Satisfied with level of activity | 34 (94.4) | 36 (92.3) | 37 (97.4) | 28 (96.6) | 36 (100.0) | 33 (94.3) | 30 (100.0) | 33 (100.0) |
| DEMQOL | ||||||||
| Number of residents | 36 | 35 | 37 | 28 | 37 | 35 | 31 | 30 |
| Item, n (%) | ||||||||
| 1 | 36 (100.0) | 35 (100.0) | 37 (100.0) | 28 (100.0) | 37 (100.0) | 34 (97.1) | 31 (100.0) | 29 (96.7) |
| 2 | 36 (100.0) | 35 (100.0) | 37 (100.0) | 28 (100.0) | 36 (97.3) | 35 (100.0) | 30 (96.8) | 30 (100.0) |
| 3 | 35 (97.2) | 35 (100.0) | 36 (97.3) | 28 (100.0) | 36 (97.3) | 35 (100.0) | 27 (97.1) | 29 (96.7) |
| 4 | 35 (97.2) | 34 (97.1) | 37 (100.0) | 28 (100.0) | 36 (97.3) | 34 (97.1) | 30 (96.8) | 29 (96.7) |
| 5 | 34 (94.4) | 34 (97.1) | 36 (97.3) | 28 (100.0) | 33 (89.2) | 34 (97.1) | 30 (96.8) | 27 (90.0) |
| 6 | 35 (97.2) | 35 (100.0) | 36 (97.3) | 28 (100.0) | 36 (97.3) | 34 (97.1) | 28 (90.3) | 28 (93.3) |
| 7 | 35 (97.2) | 35 (100.0) | 36 (97.3) | 28 (100.0) | 36 (97.3) | 34 (97.1) | 30 (96.8) | 28 (93.3) |
| 8 | 34 (94.4) | 35 (100.0) | 35 (94.6) | 28 (100.0) | 36 (97.3) | 33 (94.3) | 29 (93.5) | 28 (93.3) |
| 9 | 32 (88.9) | 35 (100.0) | 35 (94.6) | 28 (100.0) | 36 (97.3) | 34 (97.1) | 28 (90.3) | 28 (93.3) |
| 10 | 33 (91.7) | 35 (100.0) | 35 (94.6) | 28 (100.0) | 36 (97.3) | 33 (94.3) | 29 (93.5) | 28 (93.3) |
| 11 | 33 (91.7) | 34 (97.1) | 34 (91.9) | 28 (100.0) | 36 (97.3) | 34 (97.1) | 29 (93.5) | 28 (93.3) |
| 12 | 33 (91.7) | 35 (100.0) | 35 (94.6) | 28 (100.0) | 36 (97.3) | 34 (97.1) | 30 (96.8) | 29 (96.7) |
| 13 | 32 (88.9) | 35 (100.0) | 35 (94.6) | 28 (100.0) | 36 (97.3) | 34 (97.1) | 29 (93.5) | 28 (93.3) |
| 14 | 31 (86.1) | 34 (97.1) | 35 (94.6) | 28 (100.0) | 37 (100.0) | 34 (97.1) | 30 (96.8) | 28 (93.3) |
| 15 | 31 (86.1) | 34 (97.1) | 35 (94.6) | 28 (100.0) | 37 (100.0) | 34 (97.1) | 30 (96.8) | 28 (93.3) |
| 16 | 31 (86.1) | 34 (97.1) | 35 (94.6) | 28 (100.0) | 37 (100.0) | 34 (97.1) | 29 (93.5) | 28 (93.3) |
| 17 | 30 (83.3) | 34 (97.1) | 35 (94.6) | 28 (100.0) | 37 (100.0) | 34 (97.1) | 30 (96.8) | 28 (93.3) |
| 18 | 31 (86.1) | 34 (97.1) | 35 (94.6) | 28 (100.0) | 37 (100.0) | 34 (97.1) | 30 (96.8) | 28 (93.3) |
| 19 | 31 (86.1) | 34 (97.1) | 35 (94.6) | 27 (96.4) | 37 (100.0) | 34 (97.1) | 30 (96.8) | 28 (93.3) |
| 20 | 31 (86.1) | 34 (97.1) | 36 (97.3) | 28 (100.0) | 35 (94.6) | 34 (97.1) | 29 (93.5) | 28 (93.3) |
| 21 | 31 (86.1) | 34 (97.1) | 36 (97.3) | 28 (100.0) | 35 (94.6) | 34 (97.1) | 28 (90.3) | 27 (90.0) |
| 22 | 31 (86.1) | 34 (97.1) | 36 (97.3) | 28 (100.0) | 35 (94.6) | 34 (97.1) | 28 (90.3) | 27 (90.0) |
| 23 | 31 (86.1) | 33 (94.3) | 36 (97.3) | 28 (100.0) | 35 (94.6) | 34 (97.1) | 28 (90.3) | 27 (90.0) |
| 24 | 31 (86.1) | 34 (97.1) | 35 (94.6) | 27 (96.4) | 35 (94.6) | 34 (97.1) | 29 (93.5) | 27 (90.0) |
| 25 | 31 (86.1) | 34 (97.1) | 34 (91.9) | 28 (100.0) | 35 (94.6) | 34 (97.1) | 28 (90.3) | 27 (90.0) |
| 26 | 31 (86.1) | 34 (97.1) | 36 (97.3) | 26 (92.9) | 35 (94.6) | 34 (97.1) | 29 (93.5) | 26 (86.7) |
| 27 | 31 (86.1) | 34 (97.1) | 35 (94.6) | 27 (96.4) | 35 (94.6) | 34 (97.1) | 29 (93.5) | 27 (90.0) |
| 28 | 31 (86.1) | 34 (97.1) | 35 (94.6) | 28 (100.0) | 35 (94.6) | 34 (97.1) | 29 (93.5) | 27 (90.0) |
| EQ-5D-5L | ||||||||
| Number of residents | 44 | 53 | 41 | 34 | 37 | 36 | 31 | 35 |
| Domain, n (%) | ||||||||
| Mobility | 43 (97.7) | 52 (98.1) | 39 (95.1) | 33 (97.1) | 37 (100.0) | 36 (100.0) | 30 (96.8) | 35 (100.0) |
| Self-care | 43 (97.7) | 50 (94.3) | 41 (100.0) | 30 (88.2) | 37 (100.0) | 36 (100.0) | 30 (96.8) | 34 (97.1) |
| Usual activities | 42 (95.5) | 48 (90.6) | 40 (97.6) | 30 (88.2) | 37 (100.0) | 36 (100.0) | 30 (96.8) | 35 (100.0) |
| Pain/discomfort | 44 (100.0) | 51 (96.2) | 40 (97.6) | 32 (94.1) | 37 (100.0) | 36 (100.0) | 31 (100.0) | 35 (100.0) |
| Anxiety/depression | 44 (100.0) | 50 (94.3) | 40 (97.6) | 31 (91.2) | 37 (100.0) | 36 (100.0) | 31 (100.0) | 34 (97.1) |
| 6-CIT | ||||||||
| Number of residents | 43 | 44 | 40 | 27 | 36 | 33 | 30 | 31 |
| Year, n (%) | 41 (95.3) | 43 (97.7) | 38 (95.0) | 27 (100.0) | 36 (100.0) | 32 (97.0) | 30 (100.0) | 30 (96.8) |
| Month, n (%) | 41 (95.3) | 42 (95.5) | 38 (95.0) | 27 (100.0) | 35 (97.2) | 32 (97.0) | 30 (100.0) | 29 (93.5) |
| Time, n (%) | 43 (100.0) | 40 (90.9) | 37 (92.5) | 27 (100.0) | 36 (100.0) | 33 (100.0) | 29 (96.7) | 29 (93.5) |
| Counting backwards, n (%) | 40 (93.0) | 40 (90.9) | 34 (85.0) | 23 (85.2) | 32 (88.9) | 27 (81.8) | 26 (86.7) | 26 (83.9) |
| Months of the year, n (%) | 36 (83.7) | 40 (90.0) | 32 (80.0) | 23 (85.2) | 32 (88.9) | 27 (81.8) | 26 (86.7) | 24 (77.4) |
| Address phrase, n (%) | 41 (95.3) | 39 (88.6) | 35 (97.5) | 26 (96.3) | 35 (97.2) | 29 (87.9) | 28 (93.3) | 29 (93.5) |
| Questionnaire | Baseline | 3-month follow-up | 6-month follow-up | 9-month follow-up | ||||
|---|---|---|---|---|---|---|---|---|
| MoveMore + UC | UC | MoveMore + UC | UC | MoveMore + UC | UC | MoveMore + UC | UC | |
| DEMQOL Proxy | ||||||||
| Number of expected questionnairesa | 26 | 56 | 17 | 42 | 13 | 41 | 12 | 40 |
| Questionnaire completion, n (%) | ||||||||
| Completed | 25 (96.2) | 56 (100.0) | 14 (82.4) | 40 (95.2) | 13 (100.0) | 39 (95.1) | 9 (75.0) | 33 (82.5) |
| Partially completed | 1 (3.8) | 0 (0.0) | 1 (5.9) | 1 (2.4) | 0 (0.0) | 1 (2.4) | 1 (8.3) | 7 (17.5) |
| Not completed | 0 (0.0) | 0 (0.0) | 2 (11.8) | 1 (2.4) | 0 (0.0) | 1 (2.4) | 2 (16.7) | 0 (0.0) |
| Prorated,b n (%) | 1 (100.0) | – | 1 (100.0) | 1 (100.0) | – | 1 (100.0) | 1 (100.0) | 7 (100.0) |
| Missing scores,b n (%) | 0 (0.0) | – | 0 (0.0) | 0 (0.0) | – | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Time taken to complete (minutes), n | 17 | 45 | 11 | 41 | 13 | 23 | 5 | 34 |
| Mean (SD) | 8.7 (2.96) | 9.0 (7.93) | 8.4 (3.53) | 4.0 (2.66) | 6.3 (3.25) | 6.1 (2.86) | 11.4 (1.34) | 6.3 (2.12) |
| Median (IQR) | 19.0 (7.0–11.0) | 5.0 (3.0–13.0) | 9.0 (4.0–11.0) | 3.0 (2.0–7.0) | 5.0 (4.0–9.0) | 5.0 (4.0–9.0) | 12.0 (12.0–12.0) | 5.0 (5.0–9.0) |
| EQ-5D-5L Proxy | ||||||||
| Number of expected questionnairesa | 62 | 91 | 54 | 70c | 50 | 76 | 43 | 70 |
| Questionnaire completion, n (%) | ||||||||
| Completed | 61 (98.4) | 91 (100.0) | 52 (96.3) | 70 (100.0) | 50 (100.0) | 70 (92.1) | 41 (95.3) | 64 (91.4) |
| Partially completedb | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 4 (5.3) | 1 (2.3) | 3 (4.3) |
| Not completed | 1 (1.6) | 0 (0.0) | 2 (3.7) | 0 (0.0) | 0 (0.0) | 2 (2.6) | 1 (2.3) | 3 (4.3) |
| Time taken to complete (minutes), n | 40 | 76 | 46 | 70 | 50 | 40 | 30 | 58 |
| Mean (SD) | 3.4 (1.17) | 3.5 (1.99) | 2.8 (1.13) | 2.3 (0.88) | 3.7 (5.31) | 2.6 (0.93) | 2.8 (0.65) | 2.8 (0.94) |
| Median (IQR) | 3.0 (3.0 to 4.0) | 3.0 (2.0 to 4.5) | 3.0 (2.0 to 3.0) | 2.0 (2.0 to 3.0) | 2.0 (2.0 to 3.0) | 3.0 (2.0 to 4.0) | 3.0 (3.0 to 3.0) | 3.0 (2.0 to 3.0) |
| P-CAT | Baseline | 3-month follow-up | 6-month follow-up | 9-month follow-up | ||||
|---|---|---|---|---|---|---|---|---|
| MoveMore + UC | UC | MoveMore + UC | UC | MoveMore + UC | UC | MoveMore + UC | UC | |
| Number of staff completing booklets | 49 | 91 | 48 | 54 | 37 | 42 | 37 | 47 |
| Questionnaire completion, n (%) | ||||||||
| Completed | 45 (91.8) | 85 (93.4) | 39 (81.3) | 49 (90.7) | 36 (97.3) | 39 (92.9) | 35 (94.6) | 41 (87.2) |
| Partially completed | 4 (8.2) | 6 (6.6) | 9 (18.8) | 5 (9.3) | 1 (2.7) | 3 (7.1) | 2 (5.4) | 5 (10.6) |
| Not completed | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (2.1) |
| Prorated,a n (%) | 4 (100.0) | 6 (100.0) | 8 (88.9) | 5 (100.0) | 1 (100.0) | 3 (100.0) | 2 (100.0) | 5 (100.0) |
| Missing scores,a n (%) | 0 (0.0) | 0 (0.0) | 1 (11.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Item-level completion | ||||||||
| Number of staff | 49 | 91 | 48 | 54 | 37 | 42 | 37 | 46 |
| Question, n (%) | ||||||||
| 1 | 49 (100.0) | 91 (100.0) | 45 (93.8) | 53 (98.1) | 37 (100.0) | 42 (100.0) | 37 (100.0) | 46 (100.0) |
| 2 | 49 (100.0) | 90 (98.9) | 46 (95.8) | 54 (100.0) | 37 (100.0) | 42 (100.0) | 37 (100.0) | 45 (97.8) |
| 3 | 49 (100.0) | 90 (98.9) | 46 (95.8) | 54 (100.0) | 37 (100.0) | 42 (100.0) | 36 (97.3) | 46 (100.0) |
| 4 | 49 (100.0) | 91 (100.0) | 46 (95.8) | 54 (100.0) | 37 (100.0) | 42 (100.0) | 36 (97.3) | 46 (100.0) |
| 5 | 49 (100.0) | 89 (97.8) | 46 (95.8) | 53 (98.1) | 37 (100.0) | 42 (100.0) | 37 (100.0) | 46 (100.0) |
| 6 | 49 (100.0) | 91 (100.0) | 47 (97.9) | 54 (100.0) | 37 (100.0) | 42 (100.0) | 37 (100.0) | 45 (97.8) |
| 7 | 49 (100.0) | 90 (98.9) | 46 (95.8) | 52 (96.3) | 37 (100.0) | 42 (100.0) | 37 (100.0) | 46 (100.0) |
| 8 | 48 (98.0) | 90 (98.9) | 47 (97.9) | 52 (96.3) | 37 (100.0) | 42 (100.0) | 36 (97.3) | 44 (95.7) |
| 9 | 49 (100.0) | 91 (100.0) | 47 (97.9) | 54 (100.0) | 37 (100.0) | 42 (100.0) | 36 (97.3) | 46 (100.0) |
| 10 | 49 (100.0) | 89 (97.8) | 45 (93.8) | 53 (98.1) | 37 (100.0) | 40 (95.2) | 37 (100.0) | 46 (100.0) |
| 11 | 47 (95.9) | 90 (98.9) | 44 (91.7) | 53 (98.1) | 36 (97.3) | 40 (95.2) | 36 (97.3) | 45 (97.8) |
| 12 | 49 (100.0) | 90 (98.9) | 48 (100.0) | 54 (100.0) | 37 (100.0) | 42 (100.0) | 37 (100.0) | 46 (100.0) |
| 13 | 48 (98.0) | 91 (100.0) | 46 (95.8) | 54 (100.0) | 37 (100.0) | 42 (100.0) | 37 (100.0) | 46 (100.0) |
| Questionnaire | Time Point | Individual point estimates | Cluster point estimatesa | Mean difference (95% CI) (80% CI) (67% CI)b | ICCc (95% CI) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| MoveMore | UC | MoveMore | UC | ||||||||
| n/Nd | Mean (SD) | n/Nd | Mean (SD) | n/Nd | Mean (SD) | n/Nd | Mean (SD) | ||||
| EMS (score 0–20; higher score = greater mobility) | Baseline | 62/62 | 9.3 (6.81) | 90/91 | 10.7 (6.69) | 5/5 | 9.2 (4.51) | 7/7 | 11.3 (3.07) | 2.10
|
0.20 (0.07 to 0.43) |
| 3 months | 52/54 | 9.3 (6.76) | 70/70 | 10.1 (6.74) | 5/5 | 8.9 (3.85) | 6/7 | 10.3 (1.96) | 1.42
|
0.10 (0.02 to 0.34) | |
| 6 months | 50/50 | 8.8 (7.13) | 71/76 | 10.6 (6.89) | 5/5 | 8.5 (4.30) | 7/7 | 11.7 (3.27) | 3.23
|
0.15 (0.04 to 0.42) | |
| 9 months | 42/43 | 8.9 (7.21) | 68/70 | 9.8 (6.55) | 5/5 | 7.9 (5.53) | 7/7 | 11.2 (3.81) | 3.31
|
0.27 (0.10 to 0.55) | |
| BI (score 0–20; higher score = greater self-care ability) | Baseline | 62/62 | 9.2 (4.87) | 91/91 | 11.6 (5.96) | 5/5 | 8.7 (2.79) | 7/7 | 11.8 (2.18) | 3.07
|
0.11 (0.03 to 0.36) |
| 3 months | 52/54 | 9.6 (5.54) | 70/70 | 10.1 (6.05) | 5/5 | 9.0 (3.65) | 6/7 | 10.4 (2.16) | 1.41
|
0.09 (0.02 to 0.37) | |
| 6 months | 50/50 | 8.2 (5.92) | 73/76 | 10.4 (6.26) | 5/5 | 7.6 (4.10) | 7/7 | 11.1 (3.09) | 3.40
|
0.16 (0.04 to 0.44) | |
| 9 months | 42/43 | 8.4 (5.92) | 69/70 | 9.5 (6.55) | 5/5 | 7.6 (4.46) | 7/7 | 10.1 (3.10) | 2.55
|
0.16 (0.04 to 0.45) | |
| PAM-RC (score 0–21; higher score = greater physical ability and activity) | Baseline | 62/62 | 9.1 (4.92) | 91/91 | 11.5 (5.45) | 5/5 | 9.4 (2.29) | 7/7 | 12.0 (2.75) | 2.67
|
0.14 (0.04 to 0.39) |
| 3 months | 51/54 | 9.4 (5.12) | 69/70 | 11.4 (6.24) | 5/5 | 9.9 (2.72) | 6/7 | 11.6 (2.71) | 1.70
|
0.12 (0.03 to 0.37) | |
| 6 months | 50/50 | 8.9 (5.55) | 75/76 | 10.6 (5.81) | 5/5 | 9.2 (3.47) | 7/7 | 11.1 (1.82) | 1.88
|
0.11 (0.03 to 0.36) | |
| 9 months | 42/43 | 9.1 (5.40) | 63/70 | 10.4 (6.31) | 5/5 | 9.1 (3.37) | 7/7 | 11.1 (2.58) | 2.06
|
0.14 (0.04 to 0.40) | |
| PAM-RC (ability) (score 0–10) | Baseline | 62/62 | 5.9 (2.75) | 91/91 | 7.1 (2.95) | 5/5 | 6.0 (1.22) | 7/7 | 7.2 (1.20) | 1.18
|
0.10 (0.03 to 0.32) |
| 3 months | 51/54 | 5.8 (2.64) | 69/70 | 6.6 (3.02) | 5/5 | 6.0 (1.44) | 6/7 | 6.7 (1.05) | 0.77
|
0.11 (0.03 to 0.35) | |
| 6 months | 50/50 | 5.7 (2.94) | 75/76 | 6.6 (3.20) | 5/5 | 5.9 (1.72) | 7/7 | 6.7 (1.20) | 0.87
|
0.09 (0.02 to 0.34) | |
| 9 months | 42/43 | 5.9 (3.08) | 63/70 | 6.2 (3.32) | 5/5 | 5.9 (1.83) | 7/7 | 6.7 (1.37) | 0.77
|
0.10 (0.02 to 0.38) | |
| PAM-RC (activity) (score 0–11) | Baseline | 62/62 | 3.2 (2.42) | 91/91 | 4.5 (2.91) | 5/5 | 3.9 (1.23) | 7/7 | 4.9 (1.76) | 1.49
|
0.20 (0.07 to 0.46) |
| 3 months | 51/54 | 3.6 (2.75) | 69/70 | 4.8 (3.51) | 5/5 | 3.9 (1.43) | 6/7 | 4.8 (1.71) | 0.93
|
0.13 (0.03 to 0.38) | |
| 6 months | 50/50 | 3.2 (2.90) | 75/76 | 4.0 (3.02) | 5/5 | 3.3 (1.87) | 7/7 | 4.3 (1.04) | 1.00
|
0.14 (0.04 to 0.39) | |
| 9 months | 42/43 | 3.2 (2.55) | 63/70 | 4.2 (3.34) | 5/5 | 3.2 (1.55) | 7/7 | 4.5 (1.41) | 1.29
|
0.15 (0.04 to 0.41) | |
| Questionnaire | Time Point | Individual point estimates | Cluster point estimatesa | Mean difference (95% CI) (80% CI) (67% CI)b | ICCc (95% CI) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| MoveMore | UC | MoveMore | UC | ||||||||
| n/Nd | Mean (SD) | n/Nd | Mean (SD) | n/Nd | Mean (SD) | n/Nd | Mean (SD) | ||||
| GDS (score 0–15; score ≥ 5 indicative of depression) | Baseline | 42/62 | 4.1 (3.11) | 44/91 | 3.9 (3.07) | 4/5 | 4.0 (0.54) | 7/7 | 4.3 (2.91) | 0.26
|
– |
| 3 months | 40/54 | 4.5 (3.70) | 33/70 | 3.9 (3.11) | 4/5 | 4.6 (1.59) | 5/7 | 3.4 (1.57) | –1.21
|
– | |
| 6 months | 37/50 | 4.2 (3.34) | 37/76 | 3.5 (3.08) | 4/5 | 4.1 (1.10) | 6/7 | 3.1 (1.56) | –1.06
|
0.04 (0.001 to 0.67) | |
| 9 months | 29/43 | 3.2 (2.36) | 32/70 | 2.2 (1.94) | 4/5 | 3.2 (0.78) | 6/7 | 2.4 (0.95) | –0.82
|
– | |
| WHOQOL-OLD questionnaire for elderly persons (score 1–5; higher score = greater quality of life) | |||||||||||
| Question 1 | Baseline | 35/62 | 3.5 (1.04) | 39/91 | 3.1 (1.43) | 4/5 | 3.6 (0.41) | 7/7 | 3.1 (0.71) | –0.41
|
0.07 (0.01 to 0.53) |
| 3 months | 36/54 | 2.9 (1.30) | 26/70 | 3.0 (1.48) | 4/5 | 2.9 (0.18) | 5/7 | 3.0 (0.57) | 0.12
|
– | |
| 6 months | 33/50 | 2.9 (1.28) | 33/76 | 3.4 (1.48) | 4/5 | 2.9 (0.67) | 6/7 | 3.4 (0.72) | 0.55
|
0.10 (0.01 to 0.49) | |
| 9 months | 30/43 | 3.3 (1.26) | 32/70 | 3.4 (1.36) | 4/5 | 3.3 (0.36) | 6/7 | 3.6 (0.59) | 0.28
|
– | |
| Question 2 | Baseline | 34/62 | 3.7 (0.77) | 36/91 | 3.3 (1.19) | 4/5 | 3.7 (0.26) | 7/7 | 3.5 (0.61) | –0.22
|
0.05 (0.001 to 0.66) |
| 3 months | 38/54 | 3.2 (1.17) | 26/70 | 3.5 (1.10) | 4/5 | 3.2 (0.23) | 5/7 | 3.6 (0.55) | 0.40
|
– | |
| 6 months | 36/50 | 3.1 (1.17) | 35/76 | 3.4 (1.35) | 4/5 | 3.1 (0.36) | 6/7 | 3.6 (0.65) | 0.49
|
0.02 (0.00 to 0.99) | |
| 9 months | 30/43 | 3.4 (1.10) | 33/70 | 3.5 (1.42) | 4/5 | 3.4 (0.31) | 6/7 | 3.7 (0.47) | 0.33
|
– | |
| Question 3 | Baseline | 34/62 | 3.5 (0.90) | 36/91 | 2.9 (1.19) | 4/5 | 3.5 (0.31) | 7/7 | 3.2 (0.72) | –0.32
|
0.13 (0.02 to 0.47) |
| 3 months | 37/54 | 3.2 (1.01) | 28/70 | 3.1 (1.18) | 4/5 | 3.1 (0.30) | 5/7 | 3.2 (0.49) | 0.11
|
– | |
| 6 months | 36/50 | 3.1 (1.19) | 33/76 | 3.2 (1.21) | 4/5 | 3.1 (0.37) | 6/7 | 3.2 (0.37) | 0.14
|
– | |
| 9 months | 30/43 | 3.2 (0.97) | 33/70 | 3.6 (1.27) | 4/5 | 3.2 (0.06) | 6/7 | 3.7 (0.39) | 0.49
|
– | |
| DEMQOL (score 0–112; higher score = better quality of life) | Baseline | 31/62 | 90.5 (13.56) | 34/91 | 93.3 (11.35) | 4/5 | 91.5 (6.81) | 7/7 | 90.3 (16.03) | –1.24
|
0.11 (0.01 to 0.62) |
| 3 months | 35/54 | 88.2 (12.41) | 28/70 | 93.6 (11.39) | 4/5 | 88.4 (1.96) | 5/7 | 93.5 (7.73) | 5.16
|
– | |
| 6 months | 36/50 | 89.4 (11.85) | 34/76 | 94.1 (9.89) | 4/5 | 89.8 (2.61) | 6/7 | 95.0 (4.85) | 5.24
|
0.03 (0.0002 to 0.85) | |
| 9 months | 29/43 | 92.1 (11.35) | 28/70 | 94.1 (10.59) | 4/5 | 92.0 (3.42) | 6/7 | 93.9 (3.42) | 1.83
|
– | |
| EQ-5D-5L (index value –0.281 to 1.000) | Baseline | 42/62 | 0.75 (0.23) | 48/91 | 0.80 (0.22) | 4/5 | 0.7 (0.09) | 7/7 | 0.8 (0.15) | 0.05
|
0.17 (0.05 to 0.47) |
| 3 months | 38/54 | 0.69 (0.22) | 30/70 | 0.78 (0.23) | 4/5 | 0.7 (0.05) | 6/7 | 0.8 (0.16) | 0.12
|
0.16 (0.03 to 0.53) | |
| 6 months | 37/50 | 0.71 (0.24) | 36/76 | 0.79 (0.24) | 4/5 | 0.7 (0.07) | 6/7 | 0.8 (0.12) | 0.10
|
0.02 (0.0001 to 0.95) | |
| 9 months | 29/43 | 0.77 (0.22) | 33/70 | 0.78 (0.27) | 4/5 | 0.8 (0.07) | 6/7 | 0.8 (0.13) | 0.05
|
– | |
| 6-CIT (score 0–28; higher scores = greater impairment) | Baseline | 33/62 | 18.6 (8.12) | 36/91 | 16.4 (8.27) | 4/5 | 17.5 (3.38) | 7/7 | 17.2 (5.48) | –0.29
|
0.07 (0.01 to 0.48) |
| 3 months | 27/54 | 18.5 (7.87) | 23/70 | 14.0 (7.49) | 4/5 | 18.0 (3.08) | 5/7 | 14.4 (4.08) | –3.57
|
0.06 (0.002 to 0.62) | |
| 6 months | 31/50 | 17.6 (7.59) | 26/76 | 13.6 (9.50) | 4/5 | 17.3 (2.14) | 6/7 | 14.5 (4.56) | –2.76
|
0.03 (0.0001 to 0.88) | |
| 9 months | 26/43 | 17.1 (7.98) | 23/70 | 14.6 (7.94) | 4/5 | 16.3 (4.74) | 6/7 | 14.2 (2.70) | –2.02
|
0.14 (0.03 to 0.49) | |
Safety data
| Time point and falls | MoveMore + UC | UC |
|---|---|---|
| Baseline | n = 5 CHs | n = 7 CHs |
| Total home size (n residents) | 150 | 192 |
| Number of falls | 147 | 132 |
| Number (%) of residents who had a fall | 80 (53.3) | 49 (25.5) |
| Mean number of falls per resident (95% CI) | 2.67 (0.44 to 4.89) | 1.98 (0.66 to 3.29) |
| 3 monthsa | n = 5 CHs | n = 6 CHs |
| Total home size (n residents) | 150 | 152 |
| Number of falls | 99 | 64 |
| Number (%) of residents who had a fall | 51 (34.0) | 58 (38.2) |
| Mean number of falls per resident (95% CI) | 1.96 (1.51 to 2.40) | 1.40 (0.28 to 2.52) |
| 6 monthsb | n = 4 CHs | n = 5 CHs |
| Total home size (n residents) | 122 | 134 |
| Number of falls | 98 | 45 |
| Number (%) of residents who had a fall | 52 (42.6) | 27 (20.1) |
| Mean number of falls per resident (95% CI) | 2.08 (1.15 to 3.00) | 1.59 (0.57 to 2.61) |
| 9 months | n = 5 CHs | n = 7 CHs |
| Total home size (n residents) | 150 | 192 |
| Number of falls | 113 | 74 |
| Number (%) of residents who had a fall | 62 (41.3) | 47 (24.5) |
| Mean number of falls per resident (95% CI) | 1.96 (1.17 to 2.75) | 1.23 (0.58 to 1.88) |
| Details of falls | MoveMore + UC | UC |
|---|---|---|
| Registered residents (n) | 62 | 91 |
| Resident booklet dataa | ||
| Number of falls in previous 3 months at baseline | 70 | 42 |
| Number (%) of residents who had a fall | 28 (45.2) | 26 (28.6) |
| Mean number of falls per resident (95% CI) | 2.50 (2.00 to 3.00) | 1.62 (1.10 to 2.13) |
| Number of falls at follow-up | 91 | 66 |
| Number (%) of residents who had a fall | 26 (41.9) | 29 (31.9) |
| Mean number of falls per resident (95% CI) | 3.50 (2.17 to 4.83) | 2.28 (1.58 to 2.97) |
| Safety reporting datab | ||
| Number of falls at follow-up | 91 | 70 |
| Number (%) of residents who had a fall | 27 (43.5) | 35 (38.5) |
| Mean number of falls per resident (95% CI) | 3.37 (2.03 to 4.71) | 2.00 (1.57 to 2.43) |
| Time (days) from randomisation to first fallc | ||
| Mean (SD) | 121.1 (76.55) | 99.9 (82.88) |
| Median (IQR) | 119.0 (61.0–183.0) | 75.0 (32.0–148.0) |
| Fall resulted in hospitalisation, n (%) | ||
| Yes | 7 (7.7) | 9 (12.9) |
| No | 84 (92.3) | 61 (87.1) |
| Outcome of fall, n (%) | ||
| No injury | 77 (84.6) | 53 (75.7) |
| Soft-tissue injury | 14 (15.4) | 13 (18.6) |
| Fracture | 0 (0.0) | 1 (1.4) |
| Visit from health-care professional | 0 (0.0) | 3 (4.3) |
| Reason for fall, n (%) | ||
| Found on floor | 17 (18.7) | 11 (15.7) |
| Not known | 28 (30.8) | 17 (24.3) |
| Fall from bed (slipped, rolled, fell) | 24 (26.4) | 18 (25.7) |
| Fall from or ‘missed’ other furniture | 7 (7.7) | 8 (11.4) |
| Loss of balance | 4 (4.4) | 3 (4.3) |
| Otherd | 11 (12.1) | 13 (18.6) |
| Hospital admissions, A&E visits, GP call-outs and deaths | MoveMore + UC | UC |
|---|---|---|
| Hospital admissions | ||
| Number (%) of unplanned admissionsa | 37 (8.8) | 44 (9.2) |
| Number of inpatient admissions | 131 | 318 |
| Planned, n (%) | 105 (80.2) | 281 (88.4) |
| Unplanned, n (%) | 26 (19.8) | 37 (11.6) |
| Number of residents with inpatient admissions | 82 | 224 |
| Mean number of admissions per resident (95% CI) | 1.64 (1.33 to 1.95) | 1.47 (1.34 to 1.61) |
| Average length of stay (days), mean (SD) | 10.8 (5.51) | 10.0 (3.94) |
| A&E visits | ||
| Number of A&E visits | 118 | 293 |
| Number of residents attending A&E | 81 | 190 |
| Mean number of A&E visits per resident (95% CI) | 1.45 (1.27 to 1.64) | 1.57 (1.40 to 1.74) |
| Average length of stay (minutes), mean (SD) | 211.0 (105.12) | 232.5 (101.36) |
| GP call-outs | ||
| Number (%) of emergency GP call-outsa | 179 (42.4) | 77 (16.1) |
| Deaths | ||
| Number (%) of deathsa | 29 (6.9) | 31 (6.5) |
| Details of hospital admissions | MoveMore + UC | UC |
|---|---|---|
| Registered residents (n) | 62 | 91 |
| Resident booklet dataa | ||
| Number of hospitalisations in previous 3 months at baseline | 5 | 9 |
| Number (%) of residents with hospitalisations | 4 (6.4) | 7 (7.7) |
| Mean number of hospitalisations per resident (95% CI) | 1.25 (0.45 to 2.05) | 1.29 (0.83 to 1.74) |
| Number of hospitalisations over follow-up | 11 | 25 |
| Number (%) of residents with hospitalisations | 10 (16.1) | 17 (18.7) |
| Mean number of hospitalisations per resident (95% CI) | 1.10 (0.87 to 1.33) | 1.47 (1.10 to 1.84) |
| Safety reporting datab | ||
| Number of hospitalisations at follow-up | 19 | 40 |
| Number (%) of residents with hospitalisations | 15 (24.2) | 25 (27.5) |
| Mean number of hospitalisations per resident (95% CI) | 1.27 (0.94 to 1.60) | 1.60 (1.20 to 2.00) |
| Time (days) from randomisation to first admission | ||
| Mean (SD) | 87.6 (47.57) | 100.8 (98.93) |
| Median (IQR) | 88.5 (57.0–114.0) | 65.5 (19.0–181.5) |
| Outcome of hospitalisation,c n (%) | ||
| Recovered | 9 (50.0) | 17 (43.6) |
| Recovered with sequelae | 1 (5.6) | 2 (5.1) |
| Condition improving | 3 (16.7) | 8 (20.5) |
| Condition still present and unchanged | 2 (11.1) | 2 (5.1) |
| Condition deteriorated | 1 (5.6) | 3 (7.7) |
| Death | 2 (11.1) | 7 (17.9) |
| Number of hospitalisations | 36 | 44 |
| Planned, n (%) | 8 (22.2) | 4 (9.1) |
| Unplanned, n (%) | 28 (77.8) | 40 (90.0) |
| Number (%) of residents with hospitalisations | 24 (38.7) | 32 (35.2) |
| Number of hospitalisations per resident | 1.50 | 1.38 |
| Average length of stay (days) | ||
| Median (range) | 1.0 (0.0–48.0) | 2.0 (0.0–273.0) |
| MoveMore + UC | UC | |
|---|---|---|
| Registered residents (n) | 62 | 91 |
| Via follow-up visits every 3 months and completed from residents’ care notes | ||
| Baseline | ||
| Number of A&E visits in the previous 3 months at baseline | 5 | 15 |
| Number (%) of residents who had an A&E visit | 5 (8.1) | 14 (15.4) |
| Mean number of A&E visits per resident (95% CI) | 1.00 (–) | 1.07 (0.92 to 1.23) |
| Follow-up | ||
| Number of A&E visits over follow-up | 11 | 24 |
| Number (%) of residents who had an A&E visit | 9 (14.5) | 19 (20.9) |
| Mean number of A&E visits per resident (95% CI) | 1.22 (0.88 to 1.56) | 1.26 (0.99 to 1.53) |
| Via NHS Digital | ||
| Number of A&E visits over follow-up | 38 | 76 |
| Number (%) of residents who had an A&E visit | 27 (43.5) | 48 (52.7) |
| Number of A&E visits per resident | 1.41 | 1.58 |
| Average length of stay (minutes) | ||
| Median (range) | 212.5 (24.0–519.0) | 234.5 (44.0–923.0) |
| MoveMore + UC | UC | |
|---|---|---|
| Number of registered residents | 62 | 91 |
| Number (%) of deaths | 12 (19.4) | 16 (17.6) |
| Time (days) from randomisation to deatha | ||
| Mean (SD) | 128.7 (92.54) | 134.8 (91.65) |
| Median (IQR) | 92.0 (51.0–233.5) | 145.0 (56.0–207.0) |
| Place of death, n (%) | ||
| CH | 9 (75.0) | 8 (50.0) |
| Hospital | 3 (25.0) | 8 (50.0) |
| Cause of death, n (%) | ||
| Dementia | 2 (16.7) | 1 (6.3) |
| General deterioration | 4 (33.3) | 4 (25.0) |
| Respiratory condition | 2 (16.7) | 3 (18.8) |
| Other | 2 (16.7) | 6 (37.5) |
| Not known | 2 (16.7) | 2 (12.5) |
Appendix 8 Accelerometer results
Accelerometer wear
At baseline, the proportion of registered residents agreeing to wear the accelerometer was large and similar across arms (96.8% in the MoveMore arm and 93.4% in the UC arm) (Table 54). At 9 months, the proportion wearing the accelerometer in the MoveMore arm was maintained [93.0% (64.5% of registered residents at baseline)], whereas in the UC arm the proportion decreased [71.4% (54.9% of registered residents at baseline)] (see Table 54).
| Details of accelerometer wear | Baseline | 3-month follow-up | 6-month follow-up | 9-month follow-up | ||||
|---|---|---|---|---|---|---|---|---|
| MoveMore + UC | UC | MoveMore + UC | UCa | MoveMore + UC | UC | MoveMore + UC | UC | |
| Number of registered residents | 62 | 91 | 54 | 70 | 50 | 76 | 43 | 70 |
| Number (% of those available; % registered) wearing an accelerometer | 60 (96.8) | 85 (93.4) | 50 (92.6; 80.6) | 62 (88.6; 68.1) | 46 (92.0; 74.2) | 67 (88.2; 73.6) | 40 (93.0; 64.5) | 50 (71.4; 54.9) |
| Number of days’ wearb | ||||||||
| Mean (SD) | 6.9 (0.33) | 6.9 (0.30) | 6.9 (0.42) | 6.3 (1.20) | 6.9 (0.36) | 6.5 (0.78) | 6.6 (0.71) | 6.2 (1.43) |
| Median (range) | 7 (5–7) | 7 (6–7) | 7 (4–7) | 7 (3–7) | 7 (5–7) | 7 (3–7) | 7 (5–7) | 7 (2–7) |
| Mean (SD) daily wear timec | 10 h 42 min (4 h 43 min) | 11 h 36 min (5 h 26 min) | 11 h 0 min (4 h 52 min) | 10 h 18 min (5 h 52 min) | 10 h 48 min (4 h 45 min) | 10 h 24 min (6 h 11 min) | 10 h 42 min (4 h 32 min) | 10 h 24 min (6 h 44 min) |
| Number (% of those wearing the accelerometer) with minimum weard | 49 (81.7) | 77 (90.6) | 39 (78.0) | 41 (66.1) | 38 (82.6) | 46 (68.7) | 29 (72.5) | 30 (60.0) |
Reasons for non-wear included the resident being confined to bed, on end-of-life or palliative care, in hospital, declining, disliking the belt/monitor uncomfortable or having a stoma/wearing a colostomy bag, which meant that the accelerometer was not deemed suitable for them to wear.
The proportion of residents wearing the accelerometer who met the minimum wear criterion for analysis (at least 8 hours 25 minutes per day for ≥ 4 days) differed between the arms at baseline; the proportion was lower in the MoveMore arm than in the UC arm (MoreMore arm, 81.7%; UC arm, 90.6%). Although the proportion meeting the minimum wear criteria decreased in both arms across the study period, the decrease was less marked in the MoveMore arm, with 72.5% of residents meeting the minimum wear criteria at 9 months, compared with 60.0% in the UC arm. Hence, there was evidence of differential wear rates, which might have been driven by knowledge of allocation status (see Table 54).
The number of days that residents wore the accelerometers was similar between the arms, and during wear days residents wore the accelerometers for around 10 or 11 hours (see Table 54).
The number of non-wear periods in a day was similar between the arms across the study period (0 to 5 periods for 120 minutes and 0 to 3 periods for 240 minutes) (Table 55). However, there were differences between the arms in the duration of non-wear from 6 months, with residents in the MoveMore arm having a shorter duration of non-wear (lasting, on average, 3.7 hours) than residents in the UC arm (4.9 hours) (based on 120 minutes of non-wear time) (see Table 55). Similarly, the number of residents with at least one non-wear period on wear days was similar between arms at baseline, but by 9 months differences were observed: a greater proportion of residents in the MoveMore arm had at least one shorter (120 minutes) non-wear period (95% vs. 84%) and a smaller proportion had at least one longer (240 minutes) non-wear period (43% vs. 72%) (see Table 55).
| Details of accelerometer non-wear | Baseline | 3-month follow-up | 6-month follow-up | 9-month follow-up | ||||
|---|---|---|---|---|---|---|---|---|
| MoveMore + UC | UC | MoveMore + UC | UC | MoveMore + UC | UC | MoveMore + UC | UC | |
| Registered residents (n) | 62 | 91 | 54 | 70 | 50 | 76 | 43 | 70 |
| Mean number of non-wear periodsa (SD) (range) | ||||||||
| 120 minutes | 0.6 (0.78) (0.0–4.0) | 0.4 (0.73) (0.0–5.0) | 0.6 (0.88) (0.0–4.0) | 0.6 (0.79) (0.0–4.0) | 0.5 (0.79) (0.0–3.0) | 0.6 (0.90) (0.0–4.0) | 0.5 (0.75) (0.0–4.0) | 0.6 (0.93) (0.0–5.0) |
| 180 minutes | 0.3 (0.57) (0.0–3.0) | 0.3 (0.55) (0.0–4.0) | 0.3 (0.54) (0.0–2.0) | 0.3 (0.53) (0.0–3.0) | 0.3 (0.58) (0.0–3.0) | 0.4 (0.68) (0.0–3.0) | 0.3 (0.53) (0.0–3.0) | 0.4 (0.7) (0.0–4.0) |
| 240 minutes | 0.2 (0.45) (0.0–2.0) | 0.2 (0.43) (0.0–2.0) | 0.2 (0.41) (0.0–2.0) | 0.2 (0.43) (0.0–2.0) | 0.2 (0.38) (0.0–2.0) | 0.3 (0.52) (0.0–3.0) | 0.1 (0.33) (0.0–2.0) | 0.3 (0.52) (0.0–3.0) |
| Duration (hours) of non-wear periods,a mean (range) | ||||||||
| 120 minutes | 4.4 (2.0–19.3) | 4.4 (2.0–18.0) | 4.9 (2.0–18.3) | 4.6 (2.0–20.1) | 4.5 (2.0–18.9) | 5.7 (2.0–20.1) | 3.7 (2.0–20.4) | 4.9 (2.0–19.5) |
| 180 minutes | 5.6 (3.0–19.3) | 5.5 (3.0–18.0) | 6.0 (3.1–18.3) | 5.0 (3.1–19.0) | 5.2 (3.0–18.9) | 5.7 (3.0–18.1) | 3.9 (3.0–20.4) | 6.2 (3.2–19.5) |
| 240 minutes | 6.1 (4.0–19.3) | 6.5 (4.0–18.0) | 6.0 (4.0–18.3) | 6.2 (4.0–19.0) | 8.0 (4.1–15.8) | 6.1 (4.0–18.1) | 5.3 (4.1–16.7) | 6.2 (4.0–19.5) |
| Number (%) of residents with at least one non-wear period on wear days | ||||||||
| 120 minutes | 54 (90.0) | 72 (84.7) | 44 (88.0) | 57 (91.9) | 41 (89.1) | 61 (91.0) | 38 (95.0) | 42 (84.0) |
| 180 minutes | 41 (68.3) | 56 (65.9) | 35 (70.0) | 53 (85.5) | 35 (76.1) | 52 (77.6) | 29 (72.5) | 38 (76.0) |
| 240 minutes | 34 (56.7) | 48 (56.5) | 32 (64.0) | 33 (53.2) | 29 (63.0) | 45 (67.2) | 17 (42.5) | 36 (72.0) |
Preliminary review suggests that the data recorded on the activity logs provided incomplete information on when the accelerometer had been put on and taken off each wear day.
Levels of physical activity and sedentary behaviour
The levels of PA and sedentary behaviour at baseline and follow-up were summarised for those residents meeting the minimum wear time criteria and were based on data directly from the accelerometers (Tables 56–59). For each outcome measure, individual-level and cluster-level estimates, alongside a range of CIs, have been provided. For the majority of outcomes, both approaches give similar estimates. Given that (1) our CHs are likely to be a representative sample, (2) our resident sampling reflects the varying CH populations and (3) we have a small number of CHs with varying numbers of residents per CH, the individual-level point estimates are likely to be preferred where there is a discrepancy. Hence, for clarity, salient individual-level estimates data from Tables 56–59 are described and reported in Tables 60–66.
| Level of sedentary behaviour and PA | Individual point estimates | Cluster point estimatesa | ICC (95% CI)b | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MoveMore | UC | MoveMore | UC | ||||||||||
| Participants (n) | Mean (SD) | 95% CI; 80% CI; 67% CIc | Participants (n) | Mean (SD) | 95% CI; 80% CI; 67% CIc | Clusters (n) | Mean (SD) | 95% CI; 80% CI; 67% CIc | Clusters (n) | Mean (SD) | 95% CI; 80% CI; 67% CIc | ||
| Sedentary behaviour | |||||||||||||
| Time (minutes) per day spent sedentary | 49 | 697.9 (118.60) |
|
77 | 701.2 (158.54) |
|
5 | 695.7 (36.56) |
|
7 | 696.0 (75.50) |
|
0.06 (0.01 to 0.29) |
| Percentage of wear time per day spent sedentary | 49 | 91.4 (4.65) |
|
77 | 86.6 (10.00) |
|
5 | 91.5 (2.82) |
|
7 | 85.3 (3.37) |
|
0.05 (0.004 to 0.45) |
| Number of days engaged in sedentary bout of ≥ 30 minutesd | 49 | 6.0 (1.03) |
|
77 | 5.8 (1.13) |
|
5 | 6.1 (0.39) |
|
7 | 5.9 (0.48) |
|
0.01 (0.00 to 1.00) |
| Number of daily sedentary bouts of ≥ 30 minutesd | 49 | 6.4 (1.62) |
|
77 | 5.9 (1.90) |
|
5 | 6.3 (0.87) |
|
7 | 5.8 (0.76) |
|
0.11 (0.03 to 0.35) |
| Duration of sedentary bout of ≥ 30 minutese | 49 | 89.1 (34.33) |
|
77 | 84.6 (33.17) |
|
5 | 89.0 (21.41) |
|
7 | 81.4 (13.10) |
|
0.13 (0.03 to 0.37) |
| Number of days engaged in sedentary bout of ≥ 60 minutesb | 49 | 5.8 (1.12) |
|
77 | 5.3 (1.32) |
|
5 | 5.9 (0.39) |
|
7 | 5.4 (0.60) |
|
0.02 (0.001 to 0.81) |
| Number of daily sedentary bouts of ≥ 60 minutesb | 49 | 3.3 (0.82) |
|
77 | 3.0 (1.42) |
|
5 | 3.2 (0.44) |
|
7 | 2.8 (0.51) |
|
0.07 (0.01 to 0.33) |
| Duration of sedentary bout of ≥ 60 minutese | 49 | 121.4 (33.93) |
|
77 | 116.4 (35.50) |
|
5 | 120.8 (19.96) |
|
7 | 113.0 (14.50) |
|
0.09 (0.02 to 0.35) |
| Any intensity of PA | |||||||||||||
| Time (minutes) per day spent in any intensity of PA | 49 | 66.7 (39.67) |
|
77 | 112.9 (94.46) |
|
5 | 65.8 (24.39) |
|
7 | 127.2 (45.25) |
|
0.06 (0.004 to 0.48) |
| Percentage of wear time per day spent in any intensity of PA | 49 | 8.5 (4.65) |
|
77 | 13.4 (10.00) |
|
5 | 8.5 (2.82) |
|
7 | 14.7 (3.37) |
|
0.05 (0.004 to 0.45) |
| Number of breaks in any sedentary behaviour | 49 | 32.6 (16.46) |
|
77 | 45.6 (27.78) |
|
5 | 32.4 (11.27) |
|
7 | 49.3 (12.74) |
|
0.08 (0.01 to 0.42) |
| Low-intensity PA | |||||||||||||
| Time (minutes) per day spent in low-intensity PA | 49 | 57.4 (36.33) |
|
77 | 97.6 (82.62) |
|
5 | 56.8 (22.14) |
|
7 | 108.2 (35.51) |
|
0.05 (0.003 to 0.47) |
| Percentage of wear time per day spent in low-intensity PA | 49 | 7.3 (4.33) |
|
77 | 11.6 (8.85) |
|
5 | 7.3 (2.57) |
|
7 | 12.5 (2.65) |
|
0.05 (0.004 to 0.43) |
| Number of days engaged in low-intensity bout of ≥ 5 minutesd | 43 | 3.7 (1.89) |
|
72 | 4.2 (2.20) |
|
5 | 3.6 (0.63) |
|
7 | 4.4 (0.83) |
|
0.00 (0.00 to 0.00) |
| Number of daily low-intensity PA bouts of ≥ 5 minutesd | 43 | 2.0 (2.01) |
|
72 | 4.0 (5.06) |
|
5 | 1.8 (1.01) |
|
7 | 4.5 (1.72) |
|
0.00 (0.00 to 0.00) |
| Duration of low-intensity PA bout of ≥ 5 minutese | 43 | 6.5 (1.16) |
|
72 | 7.1 (1.64) |
|
5 | 6.4 (0.39) |
|
7 | 6.9 (0.50) |
|
0.05 (0.01 to 0.30) |
| Number of days engaged in low-intensity PA bout of ≥ 10 minutesd | 19 | 2.0 (1.05) |
|
49 | 2.7 (1.73) |
|
5f | 2.1 (0.80) |
|
7f | 3.0 (0.98) |
|
0.00 (0.00 to 0.00) |
| Number of daily low-intensity PA bouts of ≥ 10 minutesd | 19 | 0.4 (0.32) |
|
49 | 1.1 (1.30) |
|
5f | 0.5 (0.32) |
|
7f | 1.1 (0.45) |
|
0.00 (0.00 to 0.00) |
| Duration of low-intensity PA bout of ≥ 10 minutese | 19 | 12.5 (1.89) |
|
49 | 13.4 (2.97) |
|
5f | 12.7 (1.81) |
|
7f | 13.1 (0.82) |
|
0.03 (0.002 to 0.73) |
| Light-intensity PA | |||||||||||||
| Time (minutes) per day spent in light-intensity PA | 49 | 7.0 (3.78) |
|
77 | 13.0 (18.22) |
|
5 | 6.7 (1.94) |
|
7 | 16.6 (10.76) |
|
0.04 (0.0004 to 0.83) |
| Percentage of wear time per day spent in light-intensity PA | 49 | 0.9 (0.45) |
|
77 | 1.5 (1.98) |
|
5 | 0.9 (0.23) |
|
7 | 1.9 (0.98) |
|
0.02 (0.00 to 1.00) |
| Number of days engaged in light-intensity PA bout of ≥ 5 minutesd | 10 | 1.2 (0.42) |
|
24 | 1.6 (1.02) |
|
4f | 1.2 (0.24) |
|
7f | 1.8 (0.86) |
|
0.17 (0.005 to 0.89) |
| Number of daily light-intensity PA bouts of ≥ 5 minutesd | 10 | 0.2 (0.07) |
|
24 | 0.7 (1.40) |
|
4f | 0.2 (0.06) |
|
7f | 0.9 (1.19) |
|
0.10 (0.00 to 0.99) |
| Duration of light-intensity PA bout of ≥ 5 minutese | 10 | 5.9 (1.29) |
|
24 | 6.2 (1.78) |
|
4f | 5.8 (0.85) |
|
7f | 6.2 (0.66) |
|
0.00 (0.00 to 0.00) |
| Number of days engaged in light-intensity PA bout of ≥ 10 minutesd | 1 | 1.0 (–) | – | 4 | 1.3 (0.50) |
|
1f | 1.0 (–) | – | 4f | 1.3 (0.50) |
|
– |
| Number of daily light-intensity PA bouts of ≥ 10 minutesd | 1 | 0.1 (–) | – | 4 | 0.5 (0.23) |
|
1f | 0.1 (–) | – | 4f | 0.5 (0.23) |
|
– |
| Duration of light-intensity PA bout of ≥ 10 minutese | 1 | 10.0 (–) | – | 4 | 12.9 (1.11) |
|
1f | 10.0 (–) | – | 4f | 12.9 (1.11) |
|
– |
| Moderate-intensity PA | |||||||||||||
| Time (minutes) per day spent in moderate-intensity PA | 49 | 2.4 (1.83) |
|
77 | 2.3 (2.73) |
|
5 | 2.3 (0.74) |
|
7 | 2.4 (1.17) |
|
0.00 (0.00 to 0.00) |
| Percentage of wear time per day spent in moderate-intensity PA | 49 | 0.3 (0.23) |
|
77 | 0.3 (0.36) |
|
5 | 0.3 (0.09) |
|
7 | 0.3 (0.13) |
|
0.00 (0.00 to 0.00) |
| Number of days engaged in a moderate-intensity PA bout of ≥ 5 minutesd | 10 | 1.1 (0.32) |
|
7 | 1.0 (0.00) |
|
3f | 1.1 (0.12) | – | 5f | 1.0 (0.00) | – | – |
| Number of daily moderate-intensity PA bouts of ≥ 5 minutesd | 10 | 0.2 (0.12) |
|
7 | 0.2 (0.13) |
|
3f | 0.3 (0.17) | – | 5f | 0.3 (0.14) | – | – |
| Duration of moderate-intensity PA bout of ≥ 5 minutese | 10 | 8.2 (3.96) |
|
7 | 6.3 (1.11) |
|
3f | 11.0 (6.68) | – | 5f | 6.5 (1.00) | – | – |
| Number of days engaged in moderate-intensity PA bout of ≥ 10 minutesd | 2 | 1.0 (0.00) | – | 1 | 1.0 (–) | – | 2f | 1.0 (0.00) | – | 1f | 1.0 (–) | – | – |
| Number of daily moderate-intensity PA bouts of ≥ 10 minutesd | 2 | 0.2 (0.08) | – | 1 | 0.1 (–) | – | 2f | 0.2 (0.08) | – | 1f | 0.1 (–) | – | – |
| Duration of moderate-intensity PA bout of ≥ 10 minutese | 2 | 28 (21.21) | – | 1 | 11.0 (–) | – | 2f | 28 (21.21) | – | 1f | 11.0 (–) | – | – |
| Level of sedentary behaviour and PA | Individual point estimates | Cluster point estimatesa | ICC (95% CI)b | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MoveMore | UC | MoveMore | UC | ||||||||||
| Participants (n) | Mean (SD) | 95% CI; 80% CI; 67% CIc | Participants (n) | Mean (SD) | 95% CI; 80% CI; 67% CIc | Clusters (n) | Mean (SD) | 95% CI; 80% CI; 67% CIc | Clusters (n)d | Mean (SD) | 95% CI; 80% CI; 67% CIc | ||
| Sedentary behaviour | |||||||||||||
| Time (minutes) per day spent sedentary | 39 | 709.7 (117.66) |
|
41 | 715.6 (139.44) |
|
5 | 697.0 (51.22) |
|
5 | 707.3 (70.24) |
|
0.06 (0.01 to 0.42) |
| Percentage of wear time per day spent sedentary | 39 | 90.5 (5.49) |
|
41 | 89.1 (10.75) |
|
5 | 91.1 (2.99) |
|
5 | 87.8 (4.51) |
|
0.03 (0.003 to 0.81) |
| Number of days engaged in sedentary bout of ≥ 30 minutese | 39 | 6.1 (0.99) |
|
41 | 5.4 (1.34) |
|
5 | 6.0 (0.47) |
|
5 | 5.4 (0.54) |
|
0.12 (0.02 to 0.44) |
| Number of daily sedentary bouts of ≥ 30 minutese | 39 | 6.4 (1.56) |
|
41 | 6.3 (2.09) |
|
5 | 6.2 (0.48) |
|
5 | 6.5 (1.37) |
|
0.01 (0.00 to 1.00) |
| Duration of sedentary bout of ≥ 30 minutesf | 39 | 89.0 (33.30) |
|
41 | 90.7 (32.77) |
|
5 | 91.1 (15.63) |
|
5 | 84.5 (16.77) |
|
0.00 (0.00 to 1.00) |
| Number of days engaged in sedentary bout of ≥ 60 minutese | 39 | 5.8 (1.05) |
|
40 | 5.2 (1.25) |
|
5 | 5.8 (0.31) |
|
5 | 5.2 (0.27) |
|
0.02 (0.0001 to 0.82) |
| Number of daily sedentary bouts of ≥ 60 minutese | 39 | 3.2 (0.80) |
|
40 | 3.5 (1.26) |
|
5 | 3.2 (0.31) |
|
5 | 3.3 (0.53) |
|
0.09 (0.02 to 0.36) |
| Duration of sedentary bout of ≥ 60 minutesf | 39 | 123.9 (37.86) |
|
40 | 124.5 (36.69) |
|
5 | 126.6 (19.26) |
|
5 | 119.8 (18.47) |
|
0.00 (0.00 to 1.00) |
| Any intensity of PA | |||||||||||||
| Time (minutes) per day spent in any intensity of PA | 39 | 77.8 (54.03) |
|
41 | 91.8 (94.41) |
|
5 | 70.9 (29.69) |
|
5 | 106.6 (45.76) |
|
0.02 (0.00 to 0.98) |
| Percentage of wear time per day spent in any intensity of PA | 39 | 9.5 (5.49) |
|
41 | 10.8 (10.75) |
|
5 | 8.9 (2.99) |
|
5 | 12.2 (4.51) |
|
0.03 (0.0003 to 0.81) |
| Number of breaks in any sedentary behaviour | 39 | 35.4 (21.06) |
|
41 | 37.3 (26.94) |
|
5 | 33.1 (11.71) |
|
5 | 41.6 (13.57) |
|
0.02 (0.00 to 0.98) |
| Low-intensity PA | |||||||||||||
| Time (minutes) per day spent in low-intensity PA | 39 | 67.3 (51.32) |
|
41 | 80.9 (85.88) |
|
5 | 61.6 (27.21) |
|
5 | 93.3 (39.68) |
|
0.01 (0.00 to 1.00) |
| Percentage of wear time per day spent in low-intensity PA | 39 | 8.2 (5.16) |
|
41 | 9.5 (9.87) |
|
5 | 7.7 (2.80) |
|
5 | 10.7 (4.04) |
|
0.03 (0.0002 to 0.85) |
| Number of days engaged in low-intensity PA bout of ≥ 5 minutese | 36 | 3.9 (2.27) |
|
35 | 3.6 (2.24) |
|
5 | 3.7 (1.44) |
|
5 | 4.0 (0.97) |
|
0.12 (0.02 to 0.49) |
| Number of daily low-intensity PA bouts of ≥ 5 minutese | 36 | 2.4 (2.49) |
|
35 | 3.8 (5.46) |
|
5 | 2.1 (1.27) |
|
5 | 4.4 (2.50) |
|
0.05 (0.001 to 0.76) |
| Duration of low-intensity PA bout of ≥ 5 minutesf | 36 | 6.8 (1.48) |
|
35 | 6.7 (1.44) |
|
5 | 6.7 (0.44) |
|
5 | 6.6 (0.71) |
|
0.00 (0.00 to 1.00) |
| Number of days engaged in low-intensity PA bout of ≥ 10 minutese | 23 | 2.3 (1.39) |
|
18 | 3.1 (1.81) |
|
5g | 2.1 (0.62) |
|
5g | 3.6 (1.22) |
|
0.09 (0.001 to 0.87) |
| Number of daily low-intensity PA bouts of ≥ 10 minutese | 23 | 0.5 (0.50) |
|
18 | 1.4 (1.48) |
|
5g | 0.5 (0.16) |
|
5g | 1.3 (0.80) |
|
0.16 (0.02 to 0.70) |
| Duration of low-intensity PA bout of ≥ 10 minutesf | 23 | 12.5 (1.90) |
|
18 | 13.5 (2.88) |
|
5g | 12.2 (1.33) |
|
5g | 13.0 (1.06) |
|
0.00 (0.00 to 1.00) |
| Light-intensity PA | |||||||||||||
| Time (minutes) per day spent in light-intensity PA | 39 | 8.6 (6.49) |
|
41 | 9.3 (9.91) |
|
5 | 7.7 (3.00) |
|
5 | 11.4 (6.20) |
|
0.01 (0.00 to 1.00) |
| Percentage of wear time per day spent in light-intensity PA | 39 | 1.1 (0.81) |
|
41 | 1.1 (1.06) |
|
5 | 1.0 (0.35) |
|
5 | 1.3 (0.54) |
|
0.02 (0.0001 to 0.84) |
| Number of days engaged in light-intensity PA bout of ≥ 5 minutese | 10 | 1.6 (0.84) |
|
11 | 1.4 (0.67) |
|
5g | 1.3 (0.45) |
|
5g | 1.3 (0.30) |
|
0.00 (0.00 to 1.00) |
| Number of daily light-intensity PA bouts of ≥ 5 minutese | 10 | 0.5 (0.41) |
|
11 | 0.3 (0.19) |
|
5g | 0.4 (0.25) |
|
5g | 0.3 (0.13) |
|
0.00 (0.00 to 1.00) |
| Duration of light-intensity PA bout of ≥ 5 minutesf | 10 | 6.1 (0.80) |
|
11 | 6.1 (1.45) |
|
5g | 6.0 (0.99) |
|
5g | 6.0 (0.86) |
|
0.00 (0.00 to 1.00) |
| Number of days engaged in light-intensity PA bout of ≥ 10 minutese | 2 | 1.0 (0.00) | – | 1 | 1.0 (–) | – | 2g | 1.0 (0.00) | – | 1g | 1.0 (–) | – | – |
| Number of daily light-intensity PA bouts of ≥ 10 minutese | 2 | 0.2 (0.02) | – | 1 | 0.2 (–) | – | 2g | 0.2 (0.02) | – | 1g | 0.2 (–) | – | – |
| Duration of light-intensity PA bout of ≥ 10 minutesf | 2 | 12.0 (1.41) | – | 1 | 14.0 (–) | – | 2g | 12.0 (1.41) | – | 1g | 14.0 (–) | – | – |
| Moderate-intensity PA | |||||||||||||
| Time (minutes) per day spent in moderate-intensity PA | 39 | 1.8 (1.49) |
|
41 | 1.6 (1.77) |
|
5 | 1.5 (0.89) |
|
5 | 2.0 (0.97) |
|
0.09 (0.01 to 0.42) |
| Percentage of wear time per day spent in moderate-intensity PA | 39 | 0.2 (0.19) |
|
41 | 0.2 (0.20) |
|
5 | 0.2 (0.11) |
|
5 | 0.2 (0.11) |
|
0.10 (0.02 to 0.41) |
| Number of days engaged in moderate-intensity PA bout of ≥ 5 minutese | 2 | 1.0 (0.00) | – | 2 | 1.0 (0.00) | – | 1g | 1.0 (–) | – | 2g | 1.0 (0.00) | – | – |
| Number of daily moderate-intensity bouts of ≥ 5 minutese | 2 | 0.1 (0.00) | – | 2 | 0.4 (0.23) | – | 1g | 0.1 (–) | – | 2g | 0.4 (0.23) | – | – |
| Duration of moderate-intensity bout of ≥ 5 minutesf | 2 | 5.0 (0.00) | – | 2 | 11.1 (7.25) | – | 1g | 5.0 (–) | – | 2g | 11.1 (7.25) | – | – |
| Number of days engaged in moderate-intensity PA bout of ≥ 10 minutese | 0 | – | – | 1 | 1.0 (–) | – | 0 | – | – | 1g | 1.0 (–) | – | – |
| Number of daily moderate-intensity PA bouts of ≥ 10 minutese | 0 | – | – | 1 | 0.6 (–) | – | 0 | – | – | 1g | 0.6 (–) | – | – |
| Duration of moderate-intensity PA bout of ≥ 10 minutesf | 0 | – | – | 1 | 16.2 (–) | – | 0 | – | – | 1g | 16.2 (–) | – | – |
| Level of sedentary behaviour and PA | Individual point estimates | Cluster point estimatesa | ICC (95% CI)b | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MoveMore | UC | MoveMore | UC | ||||||||||
| n | Mean (SD) | 95% CI; 80% CI; 67% CIc | n | Mean (SD) | 95% CI; 80% CI; 67% CIc | n | Mean (SD) | 95% CI; 80% CI; 67% CIc | n | Mean (SD) | 95% CI; 80% CI; 67% CIc | ||
| Sedentary behaviour | |||||||||||||
| Time (minutes) per day spent sedentary | 38 | 696.8 (117.74) |
|
46 | 739.6 (155.47) |
|
5 | 685.9 (58.48) |
|
7 | 716.8 (71.79) |
|
0.04 (0.001 to 0.56) |
| Percentage of wear time per day spent sedentary | 38 | 90.3 (5.53) |
|
46 | 88.6 (7.74) |
|
5 | 91.1 (2.82) |
|
7 | 87.5 (3.52) |
|
0.02 (0.00 to 0.95) |
| Number of days engaged in sedentary bout of ≥ 30 minutesd | 38 | 5.9 (1.08) |
|
46 | 5.5 (1.09) |
|
5 | 5.7 (0.71) |
|
7 | 5.4 (0.77) |
|
0.28 (0.10 to 0.57) |
| Number of daily sedentary bouts of ≥ 30 minutesd | 38 | 6.4 (1.63) |
|
46 | 6.7 (2.03) |
|
5 | 6.1 (0.90) |
|
7 | 6.6 (1.20) |
|
– |
| Duration of sedentary bout of ≥ 30 minutese | 38 | 88.8 (35.96) |
|
46 | 82.6 (26.56) |
|
5 | 96.0 (21.67) |
|
7 | 79.0 (14.52) |
|
0.07 (0.003 to 0.62) |
| Number of days engaged in sedentary bout of ≥ 60 minutesd | 38 | 5.7 (1.15) |
|
46 | 5.0 (1.43) |
|
5 | 5.5 (0.73) |
|
7 | 4.7 (1.23) |
|
0.33 (0.11 to 0.65) |
| Number of daily sedentary bouts of ≥ 60 minutesd | 38 | 3.3 (1.03) |
|
46 | 3.3 (1.41) |
|
5 | 3.3 (0.67) |
|
7 | 2.9 (1.07) |
|
0.16 (0.03 to 0.57) |
| Duration of sedentary bout of ≥ 60 minutese | 38 | 124.0 (47.42) |
|
46 | 118.0 (31.25) |
|
5 | 131.9 (29.82) |
|
7 | 115.1 (16.27) |
|
0.08 (0.005 to 0.61) |
| Any intensity of PA | |||||||||||||
| Time (minutes) per day spent in any intensity of PA | 38 | 75.9 (47.06) |
|
46 | 96.5 (67.45) |
|
5 | 67.8 (26.86) |
|
7 | 105.7 (34.91) |
|
0.06 (0.002 to 0.64) |
| Percentage of wear time per day spent in any intensity of PA | 38 | 9.7 (5.53) |
|
46 | 11.4 (7.74) |
|
5 | 8.9 (2.82) |
|
7 | 12.5 (3.52) |
|
0.02 (0.00 to 0.95) |
| Number of breaks in any sedentary behaviour | 38 | 34.9 (17.64) |
|
46 | 41.9 (25.60) |
|
5 | 31.9 (10.56) |
|
7 | 44.8 (13.29) |
|
0.05 (0.001 to 0.69) |
| Low-intensity PA | |||||||||||||
| Time (minutes) per day spent in low-intensity PA | 38 | 64.1 (42.51) |
|
46 | 85.1 (63.08) |
|
5 | 57.5 (22.86) |
|
7 | 93.7 (30.23) |
|
0.04 (0.0004 to 0.79) |
| Percentage of wear time per day spent in low-intensity PA | 38 | 8.2 (5.04) |
|
46 | 10.1 (7.28) |
|
5 | 7.5 (2.43) |
|
7 | 11.1 (3.23) |
|
0.01 (0.00 to 1.00) |
| Number of days engaged in low-intensity PA bout of ≥ 5 minutesd | 35 | 3.9 (1.78) |
|
43 | 3.7 (1.89) |
|
5 | 3.6 (0.82) |
|
7 | 3.7 (0.58) |
|
0.00 (0.00 to 0.00) |
| Number of daily low-intensity PA bouts of ≥ 5 minutesd | 35 | 2.1 (2.47) |
|
43 | 3.3 (3.25) |
|
5 | 1.9 (0.98) |
|
7 | 4.0 (2.28) |
|
0.03 (0.00 to 0.97) |
| Duration of low-intensity PA bout of ≥ 5 minutese | 35 | 6.8 (1.04) |
|
43 | 7.0 (1.44) |
|
5 | 6.7 (0.31) |
|
7 | 7.2 (1.10) |
|
0.00 (0.00 to 0.00) |
| Number of days engaged in low-intensity PA bout of ≥ 10 minutesd | 18 | 2.0 (1.78) |
|
27 | 2.4 (1.36) |
|
5f | 1.6 (0.87) |
|
7f | 2.7 (0.87) |
|
0.00 (0.00 to 0.00) |
| Number of daily low-intensity PA bouts of ≥ 10 minutesd | 18 | 0.6 (0.67) |
|
27 | 0.9 (0.90) |
|
5f | 0.5 (0.38) |
|
7f | 0.9 (0.44) |
|
0.02 (0.00 to 1.00) |
| Duration of low-intensity PA bout of ≥ 10 minutese | 18 | 12.2 (2.02) |
|
27 | 13.7 (4.04) |
|
5f | 13.3 (2.03) |
|
7f | 13.8 (2.94) |
|
0.09 (0.002 to 0.84) |
| Light-intensity PA | |||||||||||||
| Time (minutes) per day spent in light-intensity PA | 38 | 8.9 (5.20) |
|
46 | 9.5 (8.25) |
|
5 | 7.8 (3.59) |
|
7 | 10.1 (5.23) |
|
0.08 (0.01 to 0.55) |
| Percentage of wear time per day spent in light-intensity PA | 38 | 1.2 (0.65) |
|
46 | 1.1 (0.95) |
|
5 | 1.0 (0.40) |
|
7 | 1.2 (0.50) |
|
0.05 (0.002 to 0.55) |
| Number of days engaged in light-intensity PA bout of ≥ 5 minutesd | 9 | 1.3 (0.71) |
|
10 | 1.4 (0.70) |
|
4f | 1.2 (0.31) |
|
5f | 1.5 (0.50) |
|
0.00 (0.00 to 0.00) |
| Number of daily light-intensity PA bouts of ≥ 5 minutesd | 9 | 0.3 (0.18) |
|
10 | 0.4 (0.51) |
|
4f | 0.4 (0.21) |
|
5f | 0.4 (0.33) |
|
0.00 (0.00 to 0.00) |
| Duration of light-intensity PA bout of ≥ 5 minutese | 9 | 5.9 (1.02) |
|
10 | 5.4 (0.94) |
|
4f | 5.9 (0.17) |
|
5f | 5.3 (0.54) |
|
0.00 (0.00 to 0.00) |
| Number of days engaged in light-intensity PA bout of ≥ 10 minutesd | 0 | – | – | 1 | 2.0 (–) | – | 0 | – | – | 1f | 2.0 (–) | – | – |
| Number of daily light-intensity PA bouts of ≥ 10 minutesd | 0 | – | – | 1 | 0.3 (–) | – | 0 | – | – | 1f | 0.3 (–) | – | – |
| Duration of light-intensity PA bout of ≥ 10 minutese | 0 | – | – | 1 | 12.0 (–) | – | 0 | – | – | 1f | 12.0 (–) | – | – |
| Moderate-intensity PA | |||||||||||||
| Time (minutes) per day spent in moderate-intensity PA | 38 | 2.9 (4.61) |
|
46 | 1.9 (1.68) |
|
5 | 2.5 (1.10) |
|
7 | 1.9 (1.07) |
|
0.00 (0.00 to 0.00) |
| Percentage of wear time per day spent in moderate-intensity PA | 38 | 0.4 (0.50) |
|
46 | 0.2 (0.21) |
|
5 | 0.3 (0.11) |
|
7 | 0.2 (0.14) |
|
0.00 (0.00 to 0.00) |
| Number of days engaged in moderate-intensity PA bout of ≥ 5 minutesd | 3 | 1.3 (0.58) | – | 7 | 1.0 (0.00) | – | 3f | 1.3 (0.58) | – | 4f | 1.0 (0.00) | – | – |
| Number of daily moderate intensity bouts ≥ 5 minutesd | 3 | 0.6 (0.50) | – | 7 | 0.2 (0.05) | – | 3f | 0.3 (0.17) | – | 4f | 0.2 (0.03) | – | – |
| Duration of moderate-intensity PA bout of ≥ 5 minutese | 3 | 15.1 (8.88) | – | 7 | 6.3 (1.50) | – | 3f | 15.1 (8.88) | – | 4f | 5.9 (1.03) | – | – |
| Number of days engaged in moderate-intensity PA bout of ≥ 10 minutesd | 2 | 1.0 (–) | – | 0 | – | – | 2f | 1.0 (–) | – | 0 | – | – | – |
| Number of daily moderate-intensity PA bouts of ≥ 10 minutesd | 2 | 0.6 (0.20) | – | 0 | – | – | 2f | 0.6 (0.20) | – | 0 | – | – | – |
| Duration of moderate-intensity PA bout of ≥ 10 minutese | 2 | 26.7 (5.23) | – | 0 | – | – | 2f | 26.7 (5.23) | – | 0 | – | – | – |
| Level of sedentary behaviour and PA | Individual point estimates | Cluster point estimatesa | ICCb (95% CI) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MoveMore | UC | MoveMore | UC | ||||||||||
| Participants (n) | Mean (SD) | 95% CI; 80% CI; 67% CId | Participants (n) | Mean (SD) | 95% CI; 80% CI; 67% CId | Clusters (n) | Mean (SD) | 95% CI; 80% CI; 67% CId | Clusters (n)e | Mean (SD) | 95% CI; 80% CI; 67% CId | ||
| Sedentary behaviour | |||||||||||||
| Time (minutes) per day spent sedentary | 29 | 691.0 (102.34) |
|
30 | 752.93 (155.39) |
|
5 | 667.9 (63.79) |
|
6 | 758.7 (86.40) |
|
0.00 (0.00 to 0.00) |
| Percentage of wear time per day spent sedentary | 29 | 89.1 (5.50) |
|
30 | 87.4 (10.78) |
|
5 | 90.61 (3.48) |
|
6 | 87.4 (4.49) |
|
0.03 (0.0001 to 0.93) |
| Number of days engaged in sedentary bout of ≥ 30 minutesf | 29 | 5.8 (1.23) |
|
30 | 5.4 (1.10) |
|
5 | 5.3 (1.06) |
|
6 | 5.5 (0.58) |
|
0.17 (0.03 to 0.52) |
| Number of daily sedentary bouts of ≥ 30 minutesf | 29 | 6.3 (1.52) |
|
30 | 6.7 (2.11) |
|
5 | 6.2 (0.51) |
|
6 | 6.7 (1.55) |
|
0.08 (0.002 to 0.77) |
| Duration of sedentary bout of ≥ 30 minutesg | 29 | 80.7 (35.45) |
|
30 | 79.4 (24.80) |
|
5 | 81.5 (23.50) |
|
6 | 79.1 (16.82) |
|
0.17 (0.03 to 0.57) |
| Number of days engaged in sedentary bout of ≥ 60 minutesf | 29 | 5.2 (1.26) |
|
29 | 5.0 (1.22) |
|
5 | 4.9 (0.73) |
|
6 | 5.0 (0.33) |
|
0.03 (0.0003 to 0.78) |
| Number of daily sedentary bouts of ≥ 60 minutesf | 29 | 2.9 (1.08) |
|
29 | 3.3 (1.33) |
|
5 | 2.9 (0.32) |
|
6 | 3.3 (0.57) |
|
0.001 (0.00 to 1.00) |
| Duration of sedentary bout of ≥ 60 minutesg | 29 | 118.9 (49.16) |
|
29 | 114.2 (28.96) |
|
5 | 117.9 (35.38) |
|
6 | 117.0 (21.00) |
|
0.21 (0.05 to 0.59) |
| Any intensity of PA | |||||||||||||
| Time (minutes) per day spent in any intensity of PA | 29 | 85.4 (46.88) |
|
30 | 119.5 (135.98) |
|
5 | 71.3 (33.40) |
|
6 | 118.1 (57.36) |
|
0.04 (0.001 to 0.80) |
| Percentage of wear time per day spent in any intensity of PA | 29 | 10.9 (5.50) |
|
30 | 12.6 (10.78) |
|
5 | 9.4 (3.48) |
|
6 | 12.6 (4.49) |
|
0.03 (0.0001 to 0.93) |
| Number of breaks in sedentary behaviour | 29 | 39.3 (17.93) |
|
30 | 47.1 (30.21) |
|
5 | 35.65 (11.48) |
|
6 | 48.35 (15.31) |
|
0.03 (0.00 to 0.97) |
| Low-intensity PA | |||||||||||||
| Time (minutes) per day spent in low-intensity PA | 29 | 72.5 (42.48) |
|
30 | 103.4 (112.95) |
|
5 | 61.0 (29.25) |
|
6 | 102.6 (47.71) |
|
0.05 (0.001 to 0.79) |
| Percentage of wear time per day spent in low-intensity PA | 29 | 9.2 (4.98) |
|
30 | 11.0 (9.37) |
|
5 | 8.0 (3.04) |
|
6 | 10.9 (3.86) |
|
0.02 (0.00 to 1.00) |
| Number of days engaged in low-intensity PA bout of ≥ 5 minutesf | 26 | 4.2 (2.27) |
|
27 | 3.9 (2.08) |
|
5 | 3.3 (1.71) |
|
6 | 3.8 (1.46) |
|
0.09 (0.01 to 0.65) |
| Number of daily low-intensity PA bouts of ≥ 5 minutesf | 26 | 2.4 (0.44) |
|
27 | 4.5 (1.43) |
|
5 | 1.9 (1.46) |
|
6 | 3.9 (2.79) |
|
0.02 (0.00 to 1.00) |
| Duration of low-intensity PA bout of ≥ 5 minutesg | 26 | 6.7 (0.97) |
|
27 | 6.9 (1.59) |
|
5 | 6.5 (0.97) |
|
6 | 6.8 (0.85) |
|
– |
| Number of days engaged in low-intensity PA bout of ≥ 10 minutesf | 17 | 2.1 (1.11) |
|
14 | 3.2 (1.67) |
|
4c | 2.1 (1.11) |
|
5c | 3.0 (0.98) |
|
0.28 (0.04 to 0.76) |
| Number of daily low-intensity PA bouts of ≥ 10 minutesf | 17 | 0.4 (0.23) |
|
14 | 1.6 (2.18) |
|
4c | 0.5 (0.22) |
|
5c | 1.4 (0.72) |
|
0.06 (0.001 to 0.86) |
| Duration of low-intensity PA bout of ≥ 10 minutesg | 17 | 12.9 (1.72) |
|
14 | 13.8 (3.17) |
|
4c | 12.8 (1.07) |
|
5c | 13.7 (2.17) |
|
0.12 (0.002 to 0.89) |
| Light-intensity PA | |||||||||||||
| Time (minutes) per day spent in light-intensity PA | 29 | 10.4 (7.90) |
|
30 | 13.6 (25.33) |
|
5 | 8.0 (5.07) |
|
6 | 13.2 (9.88) |
|
0.03 (0.01 to 0.95) |
| Percentage of wear time per day spent in light-intensity PA | 29 | 1.3 (0.96) |
|
30 | 1.4 (1.84) |
|
5 | 1.1 (0.59) |
|
6 | 1.3 (0.73) |
|
0.06 (0.003 to 0.59) |
| Number of days engaged in light-intensity PA bout of ≥ 5 minutesf | 9 | 1.2 (0.67) | – | 7 | 2.1 (2.19) | – | 3c | 1.1 (0.16) | – | 3c | 1.8 (0.90) | – | – |
| Number of daily light-intensity PA bouts of ≥ 5 minutesf | 9 | 0.3 (0.29) | – | 7 | 0.9 (1.79) | – | 3c | 0.2 (0.14) | – | 3c | 0.7 (0.68) | – | – |
| Duration of light-intensity PA bout of ≥ 5 minutesg | 9 | 5.9 (1.42) | – | 7 | 5.9 (0.79) | – | 3c | 5.7 (0.58) | – | 3c | 5.7 (0.66) | – | – |
| Number of days engaged in light-intensity PA bout of ≥ 10 minutesf | 1 | 1.0 (–) | – | 1 | 4.0 (–) | – | 1c | 1.0 (–) | – | 1c | 4.0 (–) | – | – |
| Number of daily light-intensity PA bouts of ≥ 10 minutesf | 1 | 0.1 (–) | – | 1 | 0.7 (–) | – | 1c | 0.1 (–) | – | 1c | 0.7 (–) | – | – |
| Duration of light-intensity PA bout of ≥ 10 minutesg | 1 | 11.0 (–) | – | 1 | 13.0 (–) | – | 1c | 11.0 (–) | – | 1c | 13.0 (–) | – | – |
| Moderate-intensity PA | |||||||||||||
| Time (minutes) per day spent in moderate-intensity PA | 29 | 2.5 (1.15) |
|
30 | 2.5 (3.32) |
|
5 | 2.3 (0.65) |
|
6 | 2.4 (1.30) |
|
0.03 (0.00 to 0.91) |
| Percentage of wear time per day spent in moderate-intensity PA | 29 | 0.3 (0.16) |
|
30 | 0.3 (0.45) |
|
5 | 0.3 (0.09) |
|
6 | 0.3 (0.17) |
|
0.02 (0.00 to 0.98) |
| Number of days engaged in moderate-intensity PA bout of ≥ 5 minutesf | 6 | 1.0 (0.00) | – | 5 | 1.0 (0.00) | – | 3c | 1.0 (0.00) | – | 3c | 1.0 (0.00) | – | – |
| Number of daily moderate-intensity PA bouts of ≥ 5 minutesf | 6 | 0.2 (0.04) | – | 5 | 0.3 (0.29) | – | 3c | 0.2 (0.04) | – | 3c | 0.4 (0.37) | – | – |
| Duration of moderate-intensity PA bout of ≥ 5 minutesg | 6 | 6.8 (1.47) | – | 5 | 8.9 (5.87) | – | 3c | 6.4 (1.23) | – | 3c | 10.3 (7.79) | – | – |
| Number of days engaged in moderate-intensity PA bout of ≥ 10 minutesf | 0 | – | – | 1 | 1.0 (–) | – | 0 | – | – | 1c | 1.0 (–) | – | – |
| Number of daily moderate-intensity PA bouts of ≥ 10 minutesf | 0 | – | – | 1 | 0.6 (–) | – | 0 | – | – | 1c | 0.6 (–) | – | – |
| Duration of moderate-intensity PA bout of ≥ 10 minutesg | 0 | – | – | 1 | 23.3 (–) | – | 0 | – | – | 1c | 23.3 (–) | – | – |
Time and percentage of time that residents spent sedentary and in PA are shown in Tables 60 and 61, respectively. At baseline, residents in both arms spent, on average, > 11.5 hours sedentary (> 85% of their time).
| Time point | MoveMore + UC | UC | ||||
|---|---|---|---|---|---|---|
| Participants (n) | Mean (SD) | 80% CI | Participants (n) | Mean (SD) | 80% CI | |
| Sedentary time | ||||||
| Baseline | 49 | 11 h 38 min (1 h 59 min) | 11 h 16 min to 12 h 0 min | 77 | 11 h 41 min (2 h 39 min) | 11 h 18 min to 12 h 5 min |
| 3 months | 39 | 11 h 50 min (1 h 58 min) | 11 h 25 min to 12 h 14 min | 41a | 11 h 56 min (2 h 19 min) | 11 h 27 min to 12 h 24 min |
| 6 months | 38 | 11 h 37 min (1 h 58 min) | 11 h 12 min to 12 h 2 min | 46 | 12 h 20 min (2 h 35 min) | 11 h 50 min to 12 h 49 min |
| 9 months | 29 | 11 h 31 min (1 h 42 min) | 11 h 6 min to 12 h 0 min | 30 | 12 h 33 min (2 h 35 min) | 11 h 56 min to 13 h 10 min |
| Time per day spent in any intensity of PA | ||||||
| Baseline | 49 | 1 h 7 min (40 min) | 59 min to 1 h 14 min | 77 | 1 h 53 min (1 h 35 min) | 1 h 39 min to 2 h 7 min |
| 3 months | 39 | 1 h 18 min (54 min) | 1 h 7 min to 1 h 29 min | 41a | 1 h 32 min (1 h 34 min) | 1 h 13 min to 1 h 51 min |
| 6 months | 38 | 1 h 16 min (47 min) | 1 h 6 min to 1 h 26 min | 46 | 1 h 36 min (1 h 7 min) | 1 h 24 min to 1 h 49 min |
| 9 months | 29 | 1 h 25 min (47 min) | 1 h 14 min to 1 h 37 min | 30 | 2 h 0 min (2 h 16 min) | 1 h 27 min to 2 h 32 min |
| Time per day spent in low-intensity PA | ||||||
| Baseline | 49 | 57 min (36 min) | 51 min to 1 h 4 min | 77 | 1 h 38 min (1 h 23 min) | 1 h 25 min to 1 h 50 min |
| 3 months | 39 | 1 h 7 min (51 min) | 57 min to 1 h 18 min | 41a | 1 h 21 min (1 h 26 min) | 1 h 3 min to 1 h 38 min |
| 6 months | 38 | 1 h 4 min (43 min) | 55 min to 1 h 13 min | 46 | 1 h 25 min (1 h 3 min) | 1 h 13 min to 1 h 37 min |
| 9 months | 29 | 1 h 13 min (43 min) | 1 h 2 min to 1 h 23 min | 30 | 1 h 43 min (1 h 53min) | 1 h 17 min to 2 h 10 min |
| Time per day spent in light-intensity PA | ||||||
| Baseline | 49 | 7.0 min (3.8 min) | 6.3 min to 7.7 min | 77 | 13.0 min (18.2 min) | 10.3 min to 15.7 min |
| 3 months | 39 | 8.6 min (6.5 min) | 7.3 min to 10.0 min | 41a | 9.3 min (9.9 min) | 7.3 min to 11.4 min |
| 6 months | 38 | 8.9 min (5.2 min) | 7.8 min to 10.0 min | 46 | 9.5 min (8.3 min) | 7.9 min to 11.1 min |
| 9 months | 29 | 10.4 min (7.9 min) | 8.5 min to 12.3 min | 30 | 13.6 min (25.3 min) | 7.5 min to 19.7 min |
| Time per day spent in moderate-intensity PA | ||||||
| Baseline | 49 | 2.4 min (1.8 min) | 2.0 min to 2.7 min | 77 | 2.3 min (2.7 min) | 1.9 min to 2.7 min |
| 3 months | 39 | 1.8 min (1.5 min) | 1.5 min to 2.2 min | 41a | 1.6 min (1.8 min) | 1.3 min to 2.0 min |
| 6 months | 38 | 2.9 min (4.6 min) | 1.9 min to 3.9 min | 46 | 1.9 min (1.7 min) | 1.6 min to 2.2 min |
| 9 months | 29 | 2.5 min (1.2 min) | 2.2 min to 2.8 min | 30 | 2.5 min (3.3 min) | 1.7 min to 3.0 min |
| Time point | MoveMore + UC | UC | ||||
|---|---|---|---|---|---|---|
| Participants (n) | Mean (SD) (%) | 80% CI (%) | Participants (n) | Mean (SD) (%) | 80% CI (%) | |
| Proportion of wear time per day spent sedentary | ||||||
| Baseline | 49 | 91.4 (4.7) | 90.6 to 92.3 | 77 | 86.6 (10.0) | 85.2 to 88.1 |
| 3 months | 39 | 90.5 (5.5) | 89.4 to 91.7 | 41a | 89.1 (10.8) | 87.0 to 91.3 |
| 6 months | 38 | 90.3 (5.5) | 89.1 to 91.5 | 46 | 88.6 (7.7) | 87.1 to 90.1 |
| 9 months | 29 | 89.1 (5.5) | 87.8 to 90.5 | 30 | 87.4 (10.8) | 84.8 to 89.9 |
| Proportion of wear time per day spent in any intensity of PA | ||||||
| Baseline | 49 | 8.5 (4.7) | 7.7 to 9.4 | 77 | 13.4 (10.0) | 11.9 to 14.9 |
| 3 months | 39 | 9.5 (5.5) | 8.3 to 10.6 | 41a | 10.8 (10.8) | 8.7 to 13.0 |
| 6 months | 38 | 9.7 (5.5) | 8.5 to 10.9 | 46 | 11.4 (7.7) | 9.9 to 12.9 |
| 9 months | 29 | 10.9 (5.5) | 9.6 to 12.2 | 30 | 12.6 (10.8) | 10.1 to 15.2 |
| Proportion of wear time per day spent in low-intensity PA | ||||||
| Baseline | 49 | 7.3 (4.3) | 6.5 to 8.1 | 77 | 11.6 (8.9) | 10.3 to 12.9 |
| 3 months | 39 | 8.2 (5.2) | 7.1 to 9.3 | 41a | 9.5 (9.9) | 7.5 to 11.6 |
| 6 months | 38 | 8.2 (5.0) | 7.1 to 9.2 | 46 | 10.1 (7.3) | 8.7 to 11.5 |
| 9 months | 29 | 9.2 (5.0) | 8.0 to 10.4 | 30 | 11.0 (9.4) | 8.7 to 13.2 |
| Proportion of wear time per day spent in light-intensity PA | ||||||
| Baseline | 49 | 0.9 (0.5) | 0.8 to 1.0 | 77 | 1.5 (2.0) | 1.2 to 1.8 |
| 3 months | 39 | 1.1 (0.8) | 0.9 to 1.3 | 41a | 1.1 (1.1) | 0.9 to 1.3 |
| 6 months | 38 | 1.2 (0.7) | 1.0 to 1.3 | 46 | 1.1 (1.0) | 1.0 to 1.3 |
| 9 months | 29 | 1.3 (1.0) | 1.1 to 1.6 | 30 | 1.4 (1.8) | 0.9 to 1.8 |
| Proportion of wear time per day spent in moderate-intensity PA | ||||||
| Baseline | 49 | 0.3 (0.2) | 0.3 to 0.4 | 77 | 0.3 (0.4) | 0.2 to 0.3 |
| 3 months | 39 | 0.2 (0.2) | 0.2 to 0.3 | 41a | 0.2 (0.2) | 0.2 to 0.2 |
| 6 months | 38 | 0.4 (0.5) | 0.3 to 0.5 | 46 | 0.2 (0.2) | 0.2 to 0.3 |
| 9 months | 29 | 0.3 (0.2) | 0.3 to 0.4 | 30 | 0.3 (0.5) | 0.2 to 0.4 |
Physical activity
At baseline, there was an observed difference between the percentage of time residents spent in any intensity of PA at baseline [MoveMore arm: mean 8.5% (SD 4.7%); UC arm: mean 13.4% (SD 10.0%)] (see Table 61). Related to this, the number of breaks in sedentary behaviour that residents had per day was lower among residents in the MoveMore arm than among residents in the UC arm [MoveMore arm: mean 32.6 (SD 16.5); UC arm: mean 45.6 (SD 27.8)] (Table 62).
| Time point | MoveMore + UC | UC | ||||
|---|---|---|---|---|---|---|
| Participants (n) | Mean (SD) | 80% CI | Participants (n) | Mean (SD) | 80% CI | |
| Baseline | 49 | 32.6 (16.5) | 29.5 to 35.6 | 77 | 45.6 (27.8) | 41.5 to 49.7 |
| 3 months | 39 | 35.4 (21.1) | 31.0 to 39.8 | 41a | 37.3 (26.9) | 31.8 to 42.8 |
| 6 months | 38 | 34.9 (17.6) | 31.2 to 38.6 | 46 | 41.9 (25.6) | 37.0 to 46.9 |
| 9 months | 29 | 39.3 (17.9) | 35.0 to 43.7 | 30 | 47.1 (30.2) | 39.9 to 54.4 |
At each follow-up, the percentage of time spent in any PA and the number of breaks in sedentary behaviour increased in both arms, but by a greater amount in the MoveMore arm (see Table 62). At 9 months, there was no suggestion of any differences in the proportion of wear time spent in any intensity of PA [MoveMore arm: mean 10.9% (SD 5.5%); UC arm: mean 12.6% (SD 10.8%)] (see Table 61) or in the number of breaks in sedentary behaviour between the arms [MoveMore arm: mean 39.3 (SD 17.9); UC arm: mean 47.1 (SD 30.2)] (see Table 62).
The increased proportions of time spent in PA were mainly reflected in periods of low-intensity PA (see Table 61). On average, at baseline, residents in the MoveMore arm spent a mean of 7.3% (SD 4.3%) of their day engaging in low-intensity PA, compared with a mean of 11.6% (SD 8.9%) for residents in the UC arm (see Table 61). In both arms, all residents meeting the minimum wear criteria engaged in some level of light- and moderate-intensity activity, although this was for < 2% of the day (see Table 61).
At baseline, there was evidence of a difference between the MoveMore and UC arms in the number and duration of low-intensity PA bouts of at least 5 minutes’ duration (Table 63) and in the number of days and number of bouts per day of 10-minute low-intensity PA bouts (see Table 64):
-
mean number of daily low-intensity PA bouts of ≥ 5 minutes: MoveMore arm 2.0 (SD 2.0), UC arm 4.0 (SD 5.1);
-
mean duration of daily low-intensity PA bouts of ≥ 5 minutes: MoveMore arm: 6.5 (SD 1.2) minutes, UC arm 7.1 (SD 1.6) minutes;
-
mean number of days engaged in low-intensity PA bouts of ≥ 10 minutes: MoveMore arm 2.0 (SD 1.1), UC arm 2.7 (SD 1.7)
-
mean number of daily low-intensity PA bouts of ≥ 10 minutes: MoveMore arm 0.4 (SD 0.3), UC arm 1.1 (SD 1.3)
-
mean duration of daily low-intensity PA bouts of ≥ 10 minutes: MoveMore arm 12.5 (SD 1.9) minutes, UC arm 13.4 (SD 3.0) minutes.
| Time point | MoveMore + UC | UC | ||||
|---|---|---|---|---|---|---|
| Participants (n) | Mean (SD) | 80% CI | Participants (n) | Mean (SD) | 80% CI | |
| Number of days engaged in low-intensity PA bout of ≥ 5 minutesa | ||||||
| Baseline | 43 | 3.7 (1.9) | 3.4 to 4.1 | 72 | 4.2 (2.2) | 3.8 to 4.5 |
| 3 months | 36 | 3.9 (2.3) | 3.4 to 4.4 | 35b | 3.6 (2.2) | 3.1 to 4.1 |
| 6 months | 35 | 3.9 (1.8) | 3.5 to 4.3 | 43 | 3.7 (1.9) | 3.3 to 4.1 |
| 9 months | 26 | 4.2 (2.3) | 3.6 to 4.7 | 27 | 3.9 (2.1) | 3.4 to 4.4 |
| Number of daily low-intensity PA bouts of ≥ 5 minutesa | ||||||
| Baseline | 43 | 2.0 (2.0) | 1.6 to 2.4 | 72 | 4.0 (5.1) | 3.2 to 4.8 |
| 3 months | 36 | 2.4 (2.5) | 1.9 to 3.0 | 35b | 3.8 (5.5) | 2.6 to 5.0 |
| 6 months | 35 | 2.1 (2.5) | 1.6 to 2.7 | 43 | 3.3 (3.3) | 2.6 to 3.9 |
| 9 months | 26 | 2.4 (0.4) | 1.9 to 3.0 | 27 | 4.5 (1.4) | 2.6 to 6.4 |
| Duration of low-intensity PA bout of ≥ 5 minutesc (minutes) | ||||||
| Baseline | 43 | 6.5 (1.2) | 6.2 to 6.7 | 72 | 7.1 (1.6) | 6.8 to 7.3 |
| 3 months | 36 | 6.8 (1.5) | 6.5 to 7.1 | 35b | 6.7 (1.4) | 6.4 to 7.0 |
| 6 months | 35 | 6.8 (1.0) | 6.5 to 7.0 | 43 | 7.0 (1.4) | 6.7 to 7.3 |
| 9 months | 26 | 6.7 (1.0) | 6.5 to 7.0 | 27 | 6.9 (1.6) | 6.5 to 7.3 |
However, the proportion of residents engaging in low-intensity PA bouts of at least 10 minutes’ duration was lower in the MoveMore arm [19/49 (38.8%)] than in the UC arm [49/77 (63.6%)]; hence, comparisons should be interpreted with caution (Table 64).
| Time point | MoveMore + UC | UC | ||||
|---|---|---|---|---|---|---|
| Participants (n) | Mean (SD) | 80% CI | Participants (n) | Mean (SD) | 80% CI | |
| Number of days engaged in low-intensity PA bout of ≥ 10 minutesa | ||||||
| Baseline | 19 | 2.0 (1.1) | 1.7 to 2.3 | 49 | 2.7 (1.7) | 2.4 to 3.1 |
| 3 months | 23 | 2.3 (1.4) | 1.9 to 2.6 | 18b | 3.1 (1.8) | 2.5 to 3.7 |
| 6 months | 18 | 2.0 (1.8) | 1.4 to 2.6 | 27 | 2.4 (1.4) | 2.0 to 2.7 |
| 9 months | 17 | 2.1 (1.1) | 1.8 to 2.5 | 14 | 3.2 (1.7) | 2.6 to 3.8 |
| Number of daily low-intensity PA bouts of ≥ 10 minutesa | ||||||
| Baseline | 19 | 0.4 (0.3) | 0.3 to 0.5 | 49 | 1.1 (1.3) | 0.8 to 1.3 |
| 3 months | 23 | 0.5 (0.5) | 0.4 to 0.7 | 18b | 1.4 (1.5) | 0.9 to 1.8 |
| 6 months | 18 | 0.6 (0.7) | 0.4 to 0.8 | 27 | 0.9 (0.9) | 0.7 to 1.1 |
| 9 months | 17 | 0.4 (0.2) | 0.4 to 0.5 | 14 | 1.6 (2.2) | 0.8 to 2.4 |
| Duration of low-intensity PA bout of ≥ 10 minutesc (minutes) | ||||||
| Baseline | 19 | 12.5 (1.9) | 11.9 to 13.1 | 49 | 13.4 (3.0) | 12.8 to 13.9 |
| 3 months | 23 | 12.5 (1.9) | 12.0 to 13.0 | 18a | 13.5 (2.9) | 12.6 to 14.4 |
| 6 months | 18 | 12.2 (2.0) | 11.6 to 12.8 | 27 | 13.7 (4.0) | 12.7 to 14.7 |
| 9 months | 17 | 12.9 (1.7) | 12.3 to 13.4 | 14 | 13.8 (3.2) | 12.6 to 14.9 |
During follow-up, fluctuations in low-intensity PA were observed in both arms. Overall, there was an increase from baseline among residents in the MoveMore arm in the proportion of time engaged in low-intensity PA, whereas there was no suggestion of an overall change among residents in the UC arm (see Table 61).
In the MoveMore arm, there was a gradual increase in the number of days on which residents engaged in low-intensity PA bouts of 5 minutes’ duration [mean number of bouts: baseline, 3.7 (SD 1.9); 9 months, 4.2 (SD 2.3)] (see Table 63) and in the number of 5-minute bouts per day [mean number of bouts: baseline, 2.0 (SD 2.0); 9 months, 2.4 (SD 0.4)] (see Table 63).
There were fluctuations during follow-up among residents in the UC arm in low-level intensity bouts of PA of ≥ 5 minutes’ and ≥ 10 minutes’ duration in the number of days that residents engaged in at least one bout, the number of bouts per day and the average duration of the bouts. However, by 9 months, there was a suggestion that residents engaged in low-intensity bouts of 5 minutes’ duration on fewer days than at baseline [at 9 months, mean 3.9 (SD 2.1) days; at baseline: 4.2 (SD 2.2) days] (see Table 63), but, on the days they did engage, they had more bouts [at 9 months: mean 4.5 (SD 1.4) bouts; at baseline: mean 4.0 (SD 5.1) bouts] (see Table 63), although the average duration of the bouts did not appear to change [at baseline: 7.1 (SD 1.6) minutes; at 9 months: 6.9 (SD 1.6) minutes] (see Table 63).
At 9 months, there was no suggestion of a difference between the arms in the 5-minute low-intensity PA bout outcomes (see Table 63), but the difference in the number of days and number of bouts per day for 10-minute low-intensity PA bouts that was observed at baseline remained (see Table 64). However, few residents were engaging in low-intensity PA bouts of 5 minutes’ and 10 minutes’ duration by 9 months; therefore, it is difficult to draw robust conclusions on such small sample sizes.
Sedentary behaviour
Given the imbalance between the arms at baseline in the percentage of time spent in PA, a high proportion of residents’ days were also spent sedentary in both arms [MoveMore arm: mean 91.4% (SD 4.7%); UC arm: mean 86.6% (SD 10.0%)] (see Table 61). As the CIs for these figures did not overlap, there was a suggestion that the proportion of time in sedentary behaviour was greater in the MoveMore arm. This is consistent with residents in the MoveMore arm having a lower level of physical function and more comorbidities than those in the UC arm.
At baseline, all residents engaged in sedentary bouts of at least 30 minutes’ duration. On average, residents engaged in at least one 30-minute sedentary bout on 6 of the days that they wore the accelerometer (Table 65): the average number of days’ wear was 6.9, and, on each of these days, residents had a mean of 6.4 (SD 1.6) bouts in the MoveMore arm and 5.9 (SD 1.9) bouts in the UC arm (see Table 65). The duration of the bouts was similar between arms, lasting, on average, 1.5 hours (see Table 65) before the bout was broken by a period of PA, even if this was for only 1 minute.
| Time point | MoveMore + UC | UC | ||||
|---|---|---|---|---|---|---|
| Participants (n) | Mean (SD) | 80% CI | Participants (n) | Mean (SD) | 80% CI | |
| Number of days engaged in sedentary bout of ≥ 30 minutesa | ||||||
| Baseline | 49 | 6.0 (1.0) | 5.8 to 6.2 | 77 | 5.8 (1.1) | 5.6 to 5.9 |
| 3 months | 39 | 6.1 (1.0) | 5.9 to 6.3 | 41b | 5.4 (1.3) | 5.1 to 5.6 |
| 6 months | 38 | 5.9 (1.1) | 5.7 to 6.2 | 46 | 5.5 (1.1) | 5.3 to 5.7 |
| 9 months | 29 | 5.8 (1.2) | 5.5 to 6.1 | 30 | 5.4 (1.1) | 5.2 to 5.7 |
| Number of daily sedentary bouts of ≥ 30 minutesa | ||||||
| Baseline | 49 | 6.4 (1.6) | 6.1 to 6.7 | 77 | 5.9 (1.9) | 5.7 to 6.2 |
| 3 months | 39 | 6.4 (1.6) | 6.0 to 6.7 | 41b | 6.3 (2.1) | 5.8 to 6.7 |
| 6 months | 38 | 6.4 (1.6) | 6.0 to 6.7 | 46 | 6.7 (2.0) | 6.3 to 7.1 |
| 9 months | 29 | 6.3 (1.5) | 5.9 to 6.7 | 30 | 6.7 (2.1) | 6.2 to 7.2 |
| Duration of sedentary bout of ≥ 30 minutesc | ||||||
| Baseline | 49 | 1 h 29 min (34 min) | 1 h 23 min to 1 h 35 min | 77 | 1 h 25 min (33 min) | 1 h 20 min to 1 h 29 min |
| 3 months | 39 | 1 h 29 min (33 min) | 1 h 22 min to 1 h 36 min | 41b | 1 h 31 min (33 min) | 1 h 24 min to 1 h 37 min |
| 6 months | 38 | 1 h 29 min (36 min) | 1 h 21 min to 1 h 36 min | 46 | 1 h 23 min (27 min) | 1 h 18 min to 1 h 28 min |
| 9 months | 29 | 1 h 21 min (36 min) | 1 h 12 min to 1 h 29 min | 30 | 1 h 19 min (25 min) | 1 h 13 min to 1 h 25 min |
The number and duration of 60-minute sedentary bouts were also similar between the arms at baseline (Table 66), although residents in the MoveMore arm appeared to engage in 60-minute sedentary bouts on more days than residents in the UC arm [MoveMore arm: mean 5.8 (SD 1.1) days; UC arm: mean 5.3 (SD 1.3) days] (see Table 66). Therefore, although residents in the MoveMore arm appeared to spend a greater percentage of their day sedentary at baseline, there was a suggestion that the difference was in shorter bouts.
| Time point | MoveMore + UC | UC | ||||
|---|---|---|---|---|---|---|
| Participants (n) | Mean (SD) | 80% CI | Participants (n) | Mean (SD) | 80% CI | |
| Number of days engaged in sedentary bout of ≥ 60 minutesa | ||||||
| Baseline | 49 | 5.8 (1.1) | 5.6 to 6.0 | 77 | 5.3 (1.3) | 5.0 to 5.5 |
| 3 months | 39 | 5.8 (1.1) | 5.6 to 6.0 | 40b | 5.2 (1.3) | 5.0 to 5.5 |
| 6 months | 38 | 5.7 (1.2) | 5.4 to 5.9 | 46 | 5.0 (1.4) | 4.8 to 5.3 |
| 9 months | 29 | 5.2 (1.3) | 4.9 to 5.1 | 29 | 5.0 (1.2) | 4.7 to 5.3 |
| Number of daily sedentary bouts of ≥ 60 minutesa | ||||||
| Baseline | 49 | 3.3 (0.8) | 3.1 to 3.4 | 77 | 3.0 (1.4) | 2.8 to 3.2 |
| 3 months | 39 | 3.2 (0.8) | 3.0 to 3.4 | 40b | 3.5 (1.3) | 3.3 to 3.8 |
| 6 months | 38 | 3.3 (1.0) | 3.1 to 3.6 | 46 | 3.3 (1.4) | 3.0 to 3.6 |
| 9 months | 29 | 2.9 (1.1) | 2.6 to 3.1 | 29 | 3.3 (1.3) | 3.0 to 3.7 |
| Duration of sedentary bout of ≥ 60 minutesc | ||||||
| Baseline | 49 | 2 h 1 min (34 min) | 1 h 55 min to 2 h 8 min | 77 | 1 h 56 min to (36 min) | 1 h 51 min to 2 h 2 min |
| 3 months | 39 | 2 h 4 min (38 min) | 1 h 56 min to 2 h 12 min | 40b | 2 h 5 min to (37 min) | 1 h 57 min to 2 h 12 min |
| 6 months | 38 | 2 h 4 min (47 min) | 1 h 54 min to 2 h 14 min | 46 | 1 h 58 min to (31 min) | 1 h 52 min to 2 h 4 min |
| 9 months | 29 | 1 h 59 min (49 min) | 1 h 47 min to 2 h 11 min | 29 | 1 h 54 min to (29 min) | 1 h 47 min to 2 h 1 min |
Changes in sedentary behaviour were observed in both arms during follow-up. In summary, at 9 months, residents in the MoveMore arm engaged in 30-minute sedentary bouts on the same number of days (see Table 65) and had the same number of bouts per day as at baseline (see Table 65), but the duration of these bouts was shorter [mean duration: at 9 months, 1 hour 21 minutes (SD 36 minutes); at baseline, 1 hour 29 minutes (SD 34 minutes)] (see Table 65). Residents in the UC arm engaged in 30-minute sedentary bouts on fewer days at 9 months than at baseline [9 months: mean 5.4 (SD 1.1) days; baseline: mean 5.8 (SD 1.1) days] (see Table 65), but had more bouts per day [9 months: mean 6.7 (SD 2.1) bouts; baseline: mean 5.9 (SD 1.9) bouts] (see Table 65), although the duration of these bouts was also shorter [mean duration: at 9 months, 1 hour 19 minutes (SD 25 minutes); at baseline, 1 hour 25 minutes (SD 33 minutes)] (see Table 65).
A similar pattern was observed for the 60-minute sedentary bouts (see Table 66), although residents in the MoveMore arm also engaged in these bouts on fewer days at 9 months [mean 5.2 (SD 1.3) days] than at baseline [mean 5.8 (SD 1.1) days] (see Table 66) and had fewer bouts per day at 9 months [mean 2.9 (SD 1.1) bouts] than at baseline [mean 3.3 (SD 0.8) bouts] (see Table 66). Overall, there was a decrease from baseline among residents in the MoveMore arm in the proportion of time engaged in sedentary behaviour, whereas there was no suggestion of an overall change among residents in the UC arm (see Table 66). However, at 9 months, there was no suggestion of a difference between the arms in the outcomes (see Table 66).
Variation in outcomes between care homes
The ICCs (see Tables 56–59) provide an estimate of the amount of variation in each outcome, explained by the variation between CHs. These data inform sample size calculations for a definitive trial. In this feasibility study, we had a small number of CHs (clusters) with varying cluster size, with a maximum of between three residents and 20 residents per home, which led to an unbalanced design, for which there is limited research on the performance of ICC estimates.
Individual-level profiles
Displaying the profile of individual residents’ activity within CHs allowed us to examine whether or not there were any observed changes that may or may not be reflected at the level of the CH. It also allowed us to see the contribution of each resident to the analysis at the different time points.
There was a large amount of variation between residents in all homes in both arms when examining the percentage of time per day spent sedentary (Figures 14 and 15). In particular, in the MoveMore arm, there was marked fluctuation in individuals’ sedentary behaviour over the study duration. However, there did appear to be a number of residents in CHs in the MoveMore arm who showed a decrease in the percentage of time spent sedentary, most notably in CH3 and CH4 up to the 6-month follow-up (after which sedentary behaviour increased again) and in CH5 between the 6- and 9-month follow-ups. In the UC CHs, there was a clear increase in the percentage of time per day spent sedentary for all residents in CH7, CH8 and CH11, whereas, in the other CHs, this stayed at a similar level or increased slightly. The presence of an activity co-ordinator did not appear to affect residents’ profiles.
FIGURE 14.
Profile of sedentary behaviour during the study among residents in MoveMore CHs. (a) CH2; (b) CH3; (c) CH5; (d) CH1; and (e) CH4. CHs 2, 3 and 5 had an activity co-ordinator in place at baseline and follow-up. CHs 1 and 4 did not have an activity co-ordinator in place at baseline; however, CH1 had a co-ordinator in place at follow-up. All homes were of similar size (28–35 beds). BL, baseline; m, months.
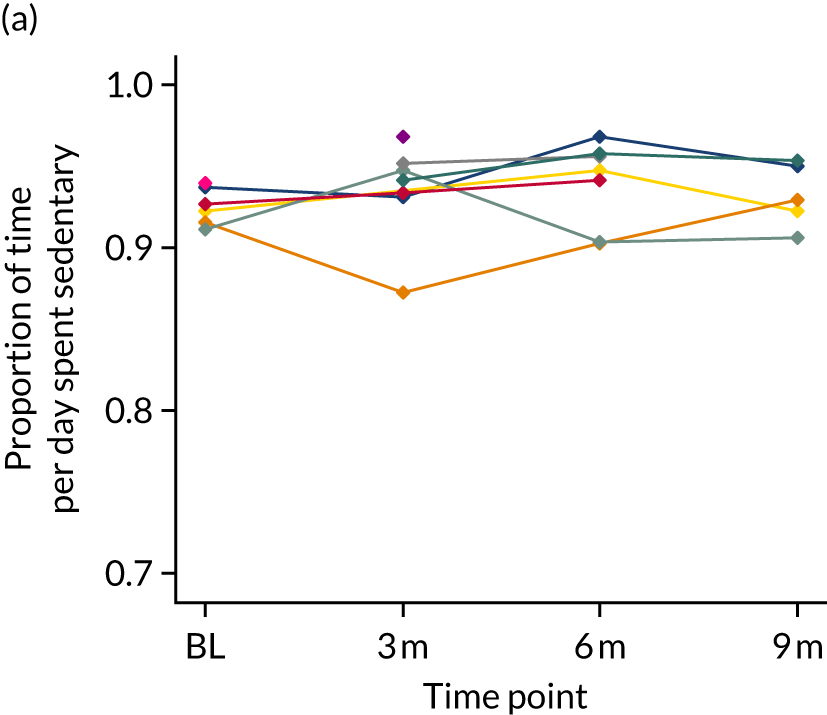
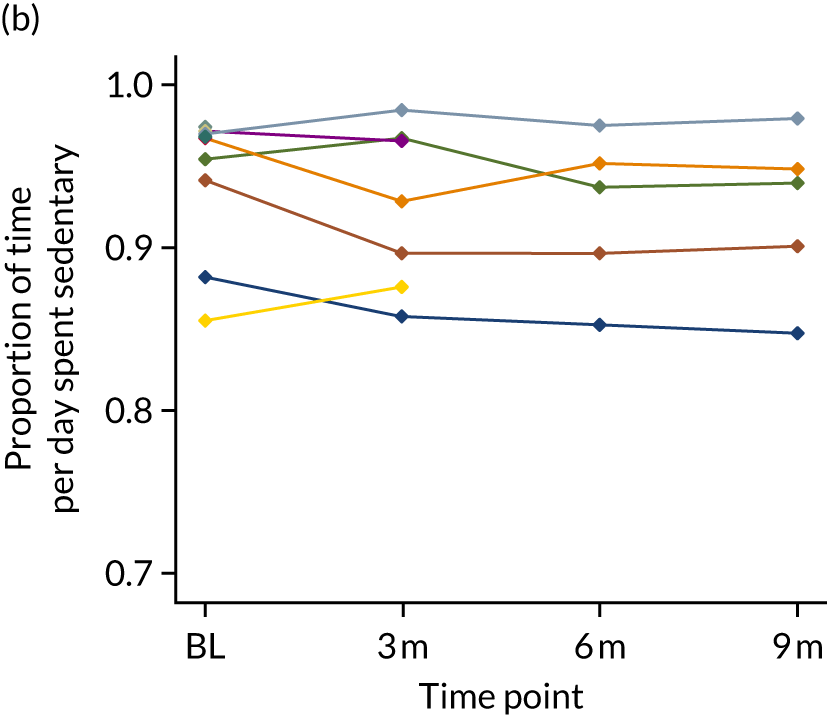
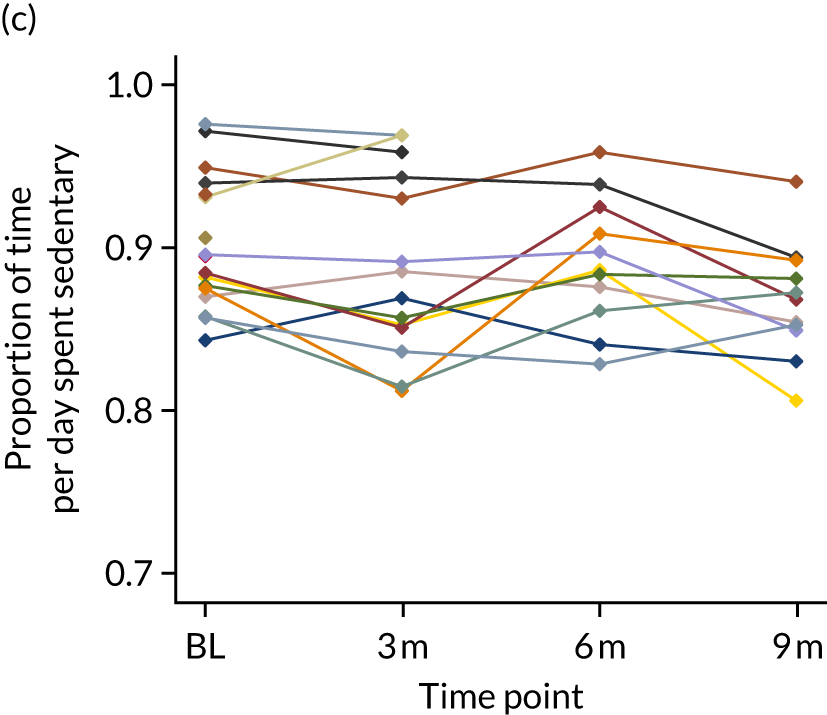
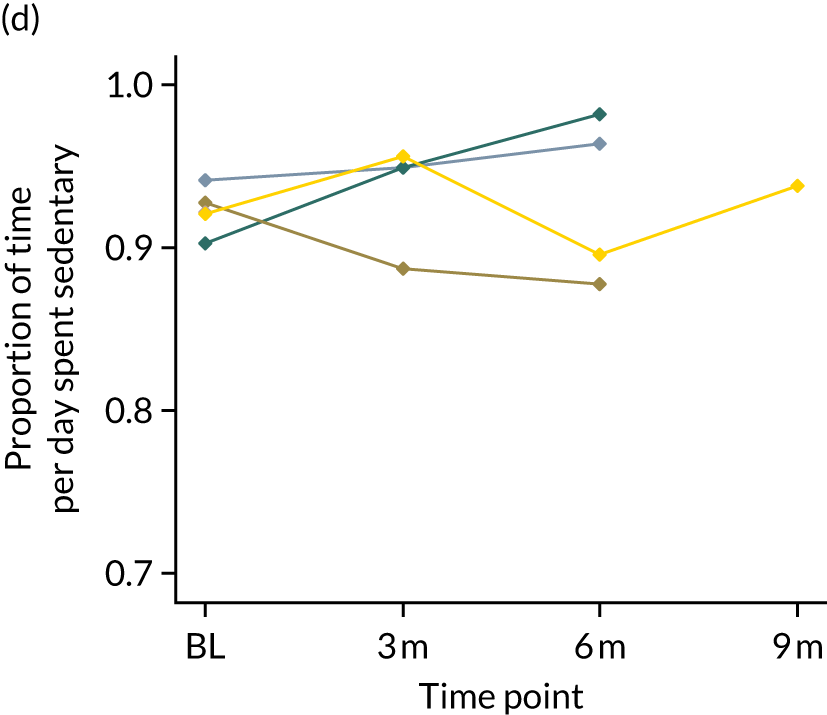
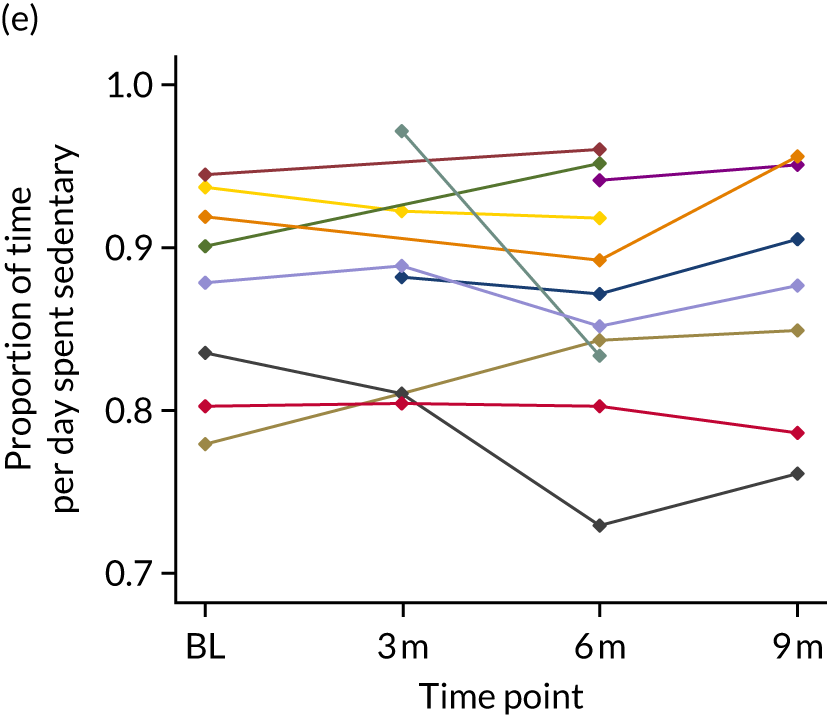
FIGURE 15.
Profile of sedentary behaviour during the study among residents in UC homes. (a) CH6; (b) CH8; (c) CH9; (d) CH10; (e) CH11; (f) CH7; and (g) CH12. CHs 6 and 8–11 had an activity co-ordinator in place at baseline and follow-up. These homes varied in size (21–92 beds). CHs 7 and 12 did not have an activity co-ordinator in place at baseline; however, CH7 had a co-ordinator in place at the 6- and 9-month follow-ups. These homes were much smaller in size (16 and 18 beds in CHs 7 and 12, respectively). BL, baseline; m, months.
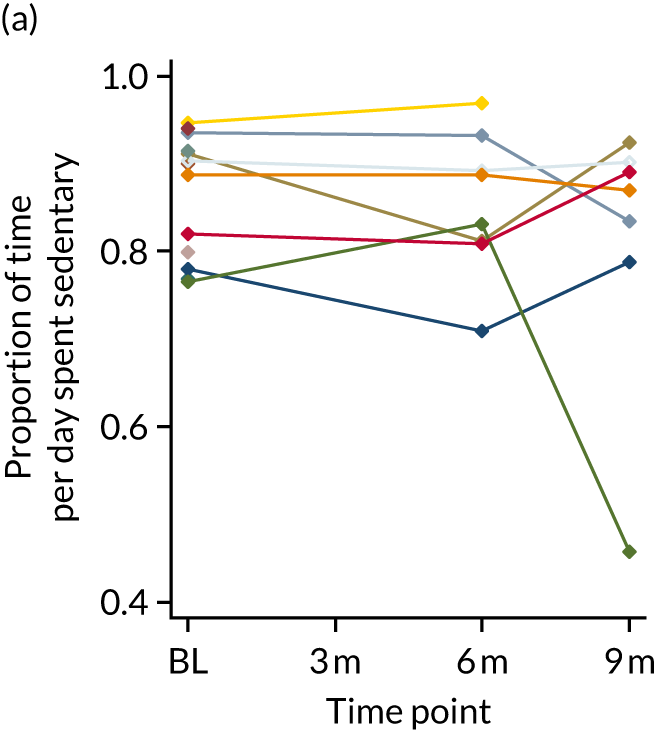
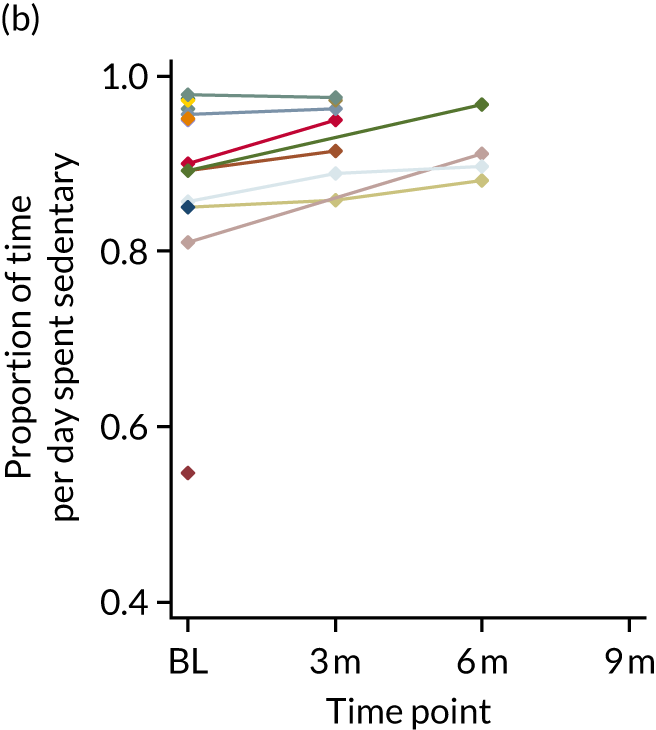
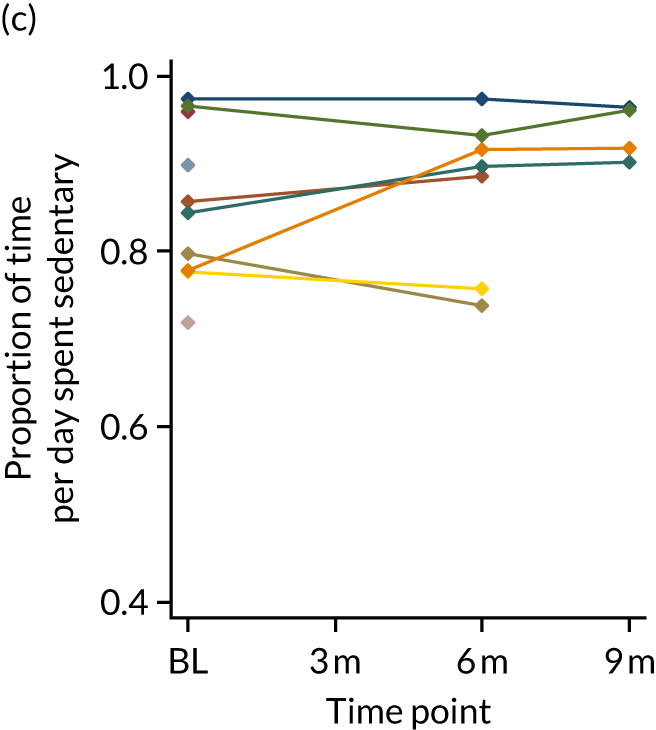
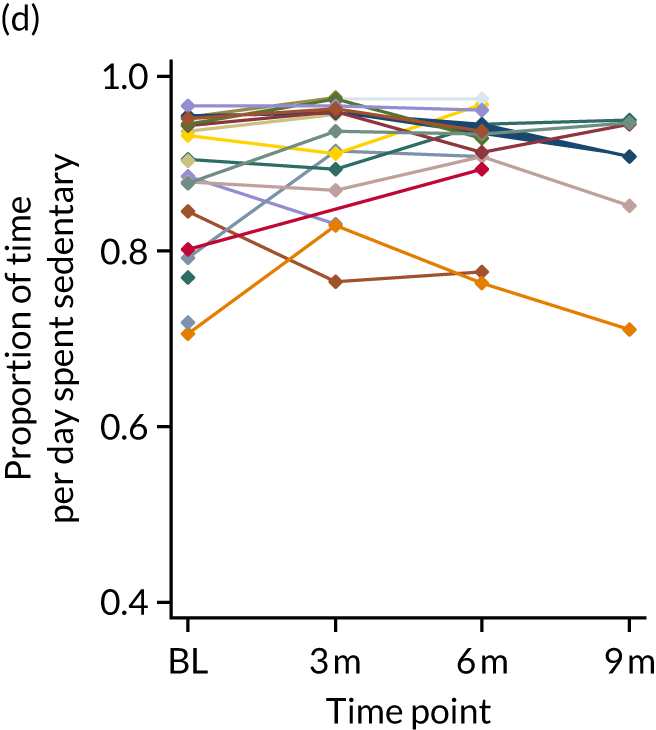
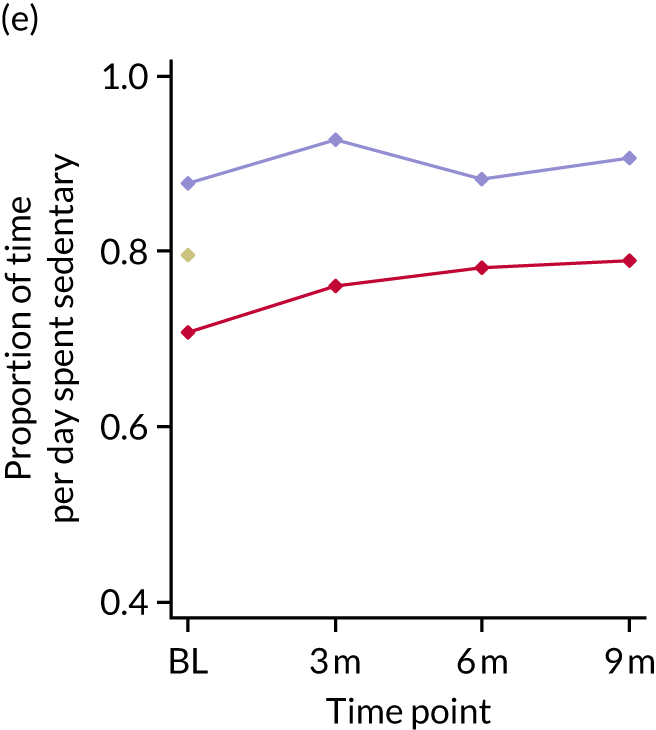
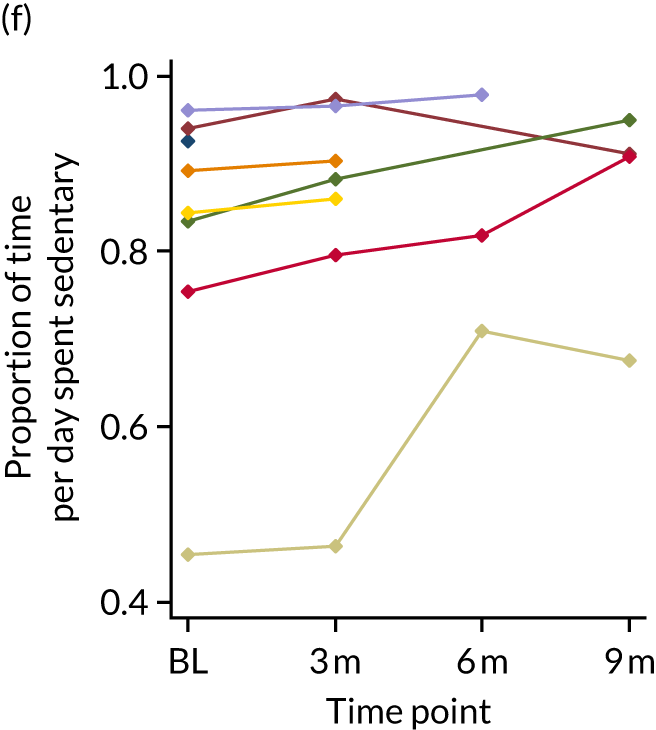
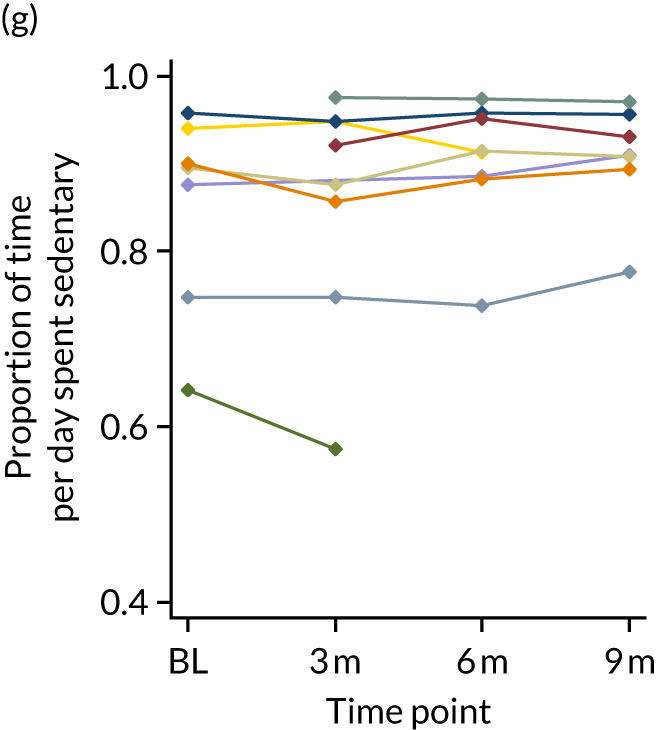
The number of breaks in sedentary behaviour per day also showed variation between residents within homes and for individual residents across the study duration (Figures 16 and 17). The most notable change in the MoveMore CHs was a general decreasing trend for the majority of residents in CH5 up to 6 months, after which time the number of breaks increased in line with the observed decrease in the percentage of time spent sedentary.
FIGURE 16.
Profile of breaks in sedentary behaviour during the study among residents in MoveMore CHs. (a) CH1; (b) CH2; (c) CH3; (d) CH4; and (e) CH5. BL, baseline; m, months.
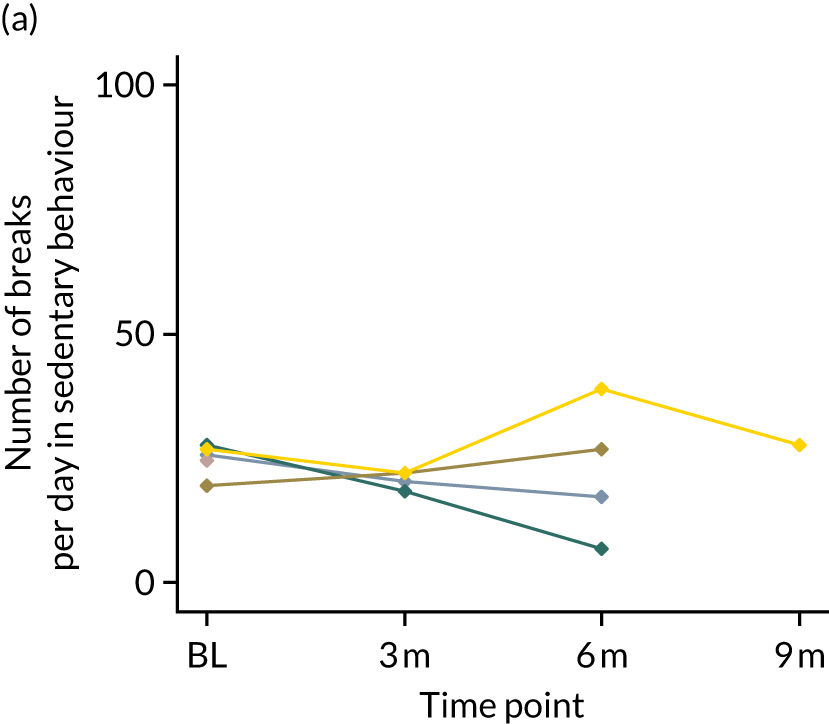
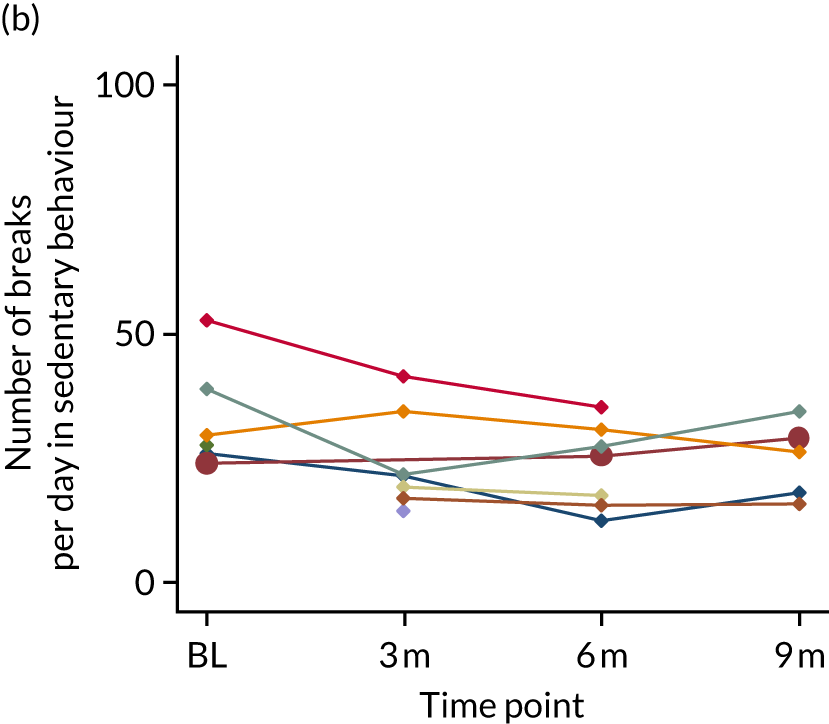
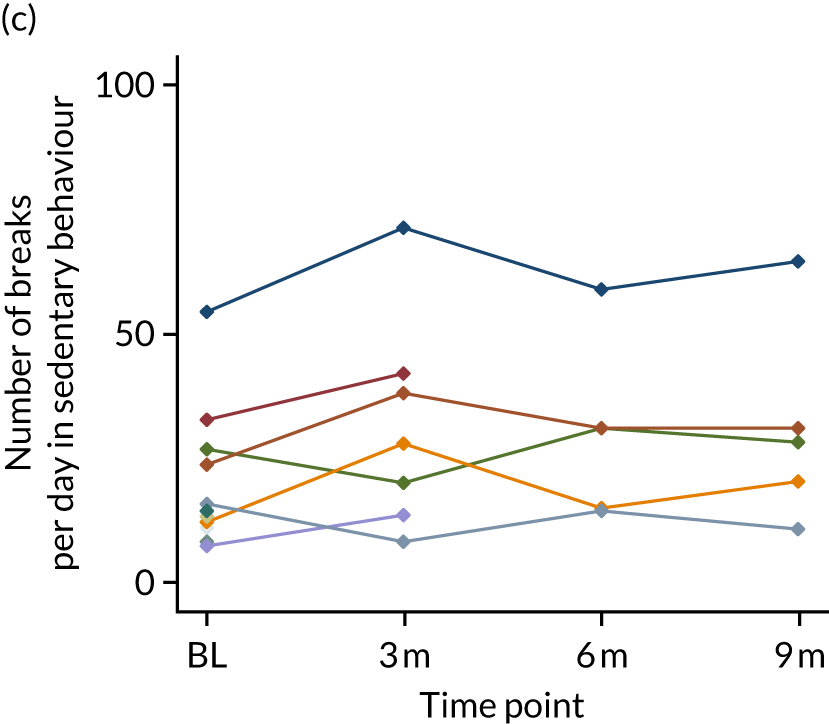
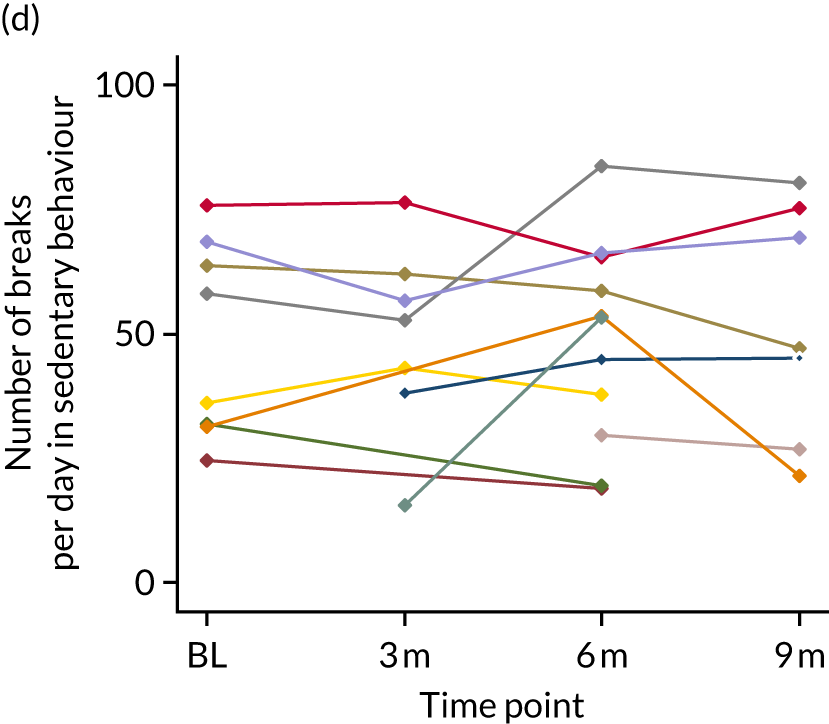
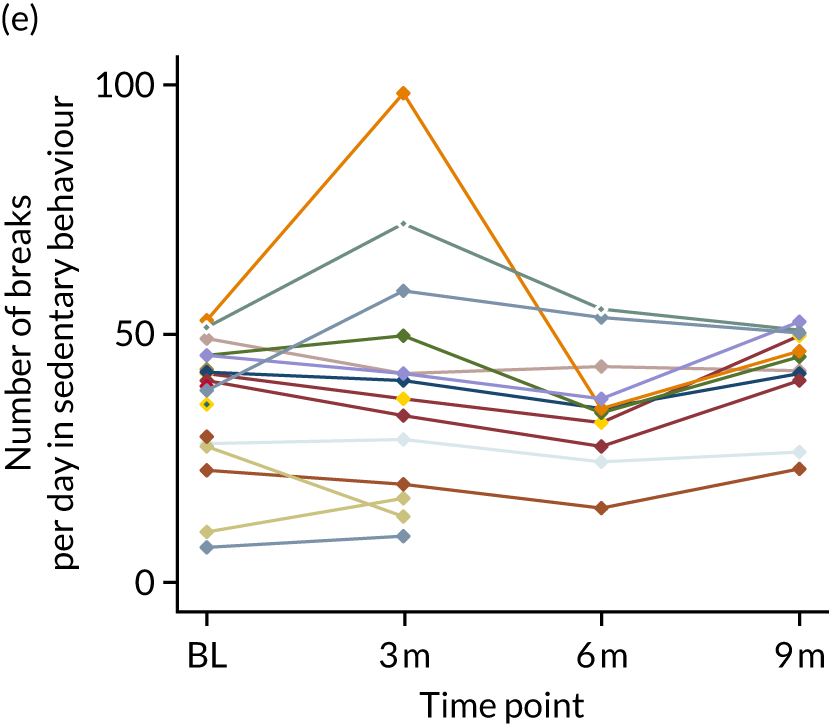
FIGURE 17.
Profile of breaks in sedentary behaviour during the study among residents in UC homes. (a) CH6; (b) CH8; (c) CH9; (d) CH10; (e) CH11; (f) CH7; and (g) CH12. BL, baseline; m, months.
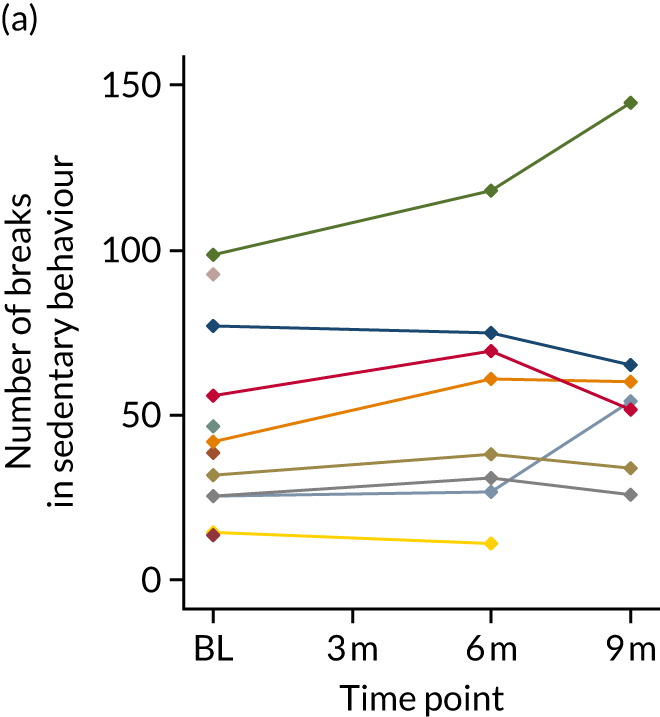
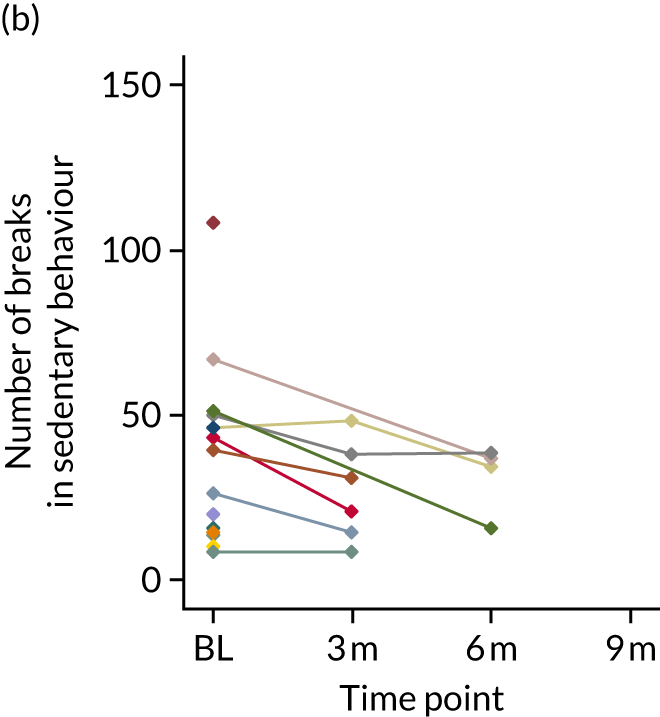
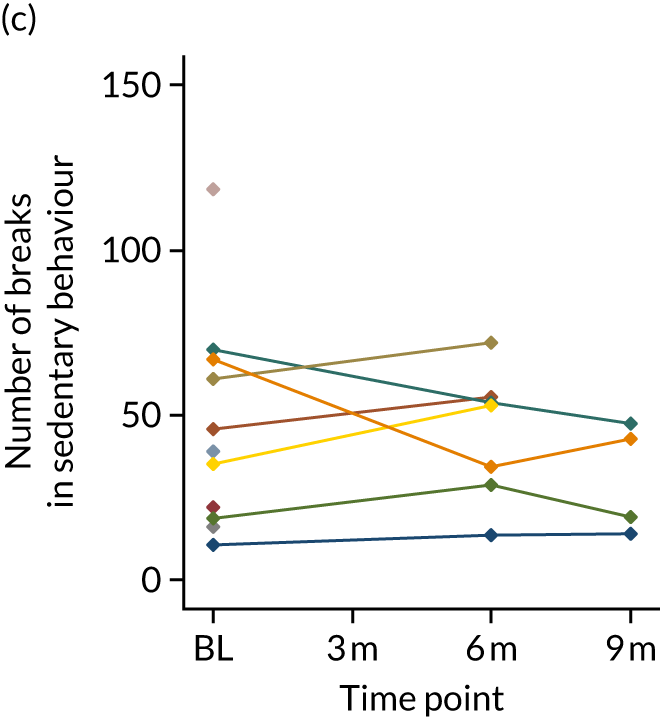
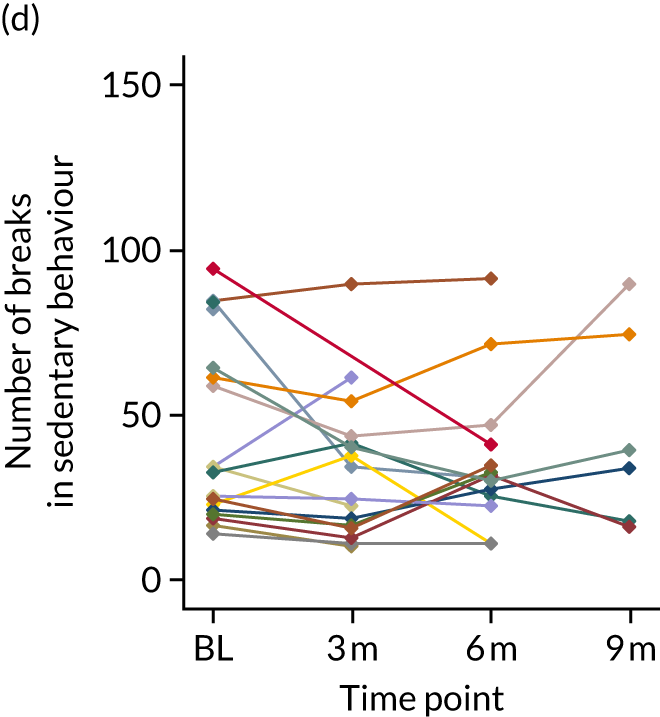
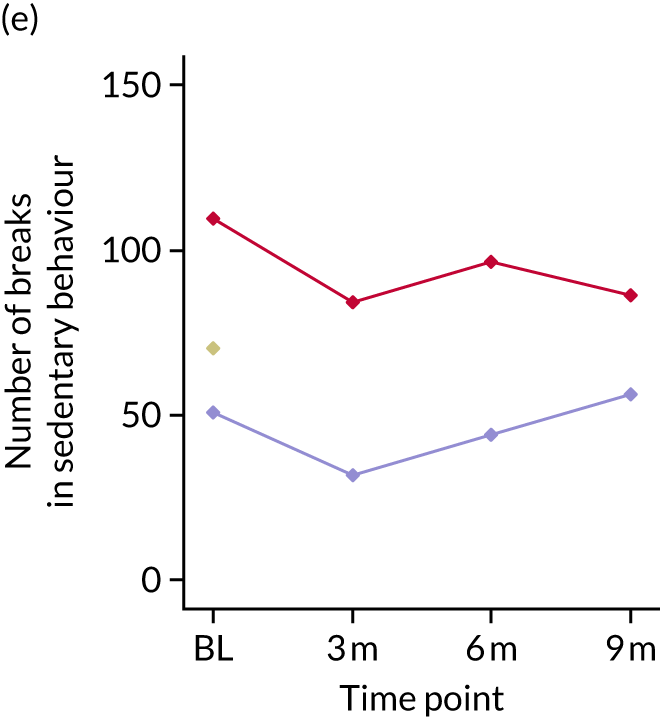
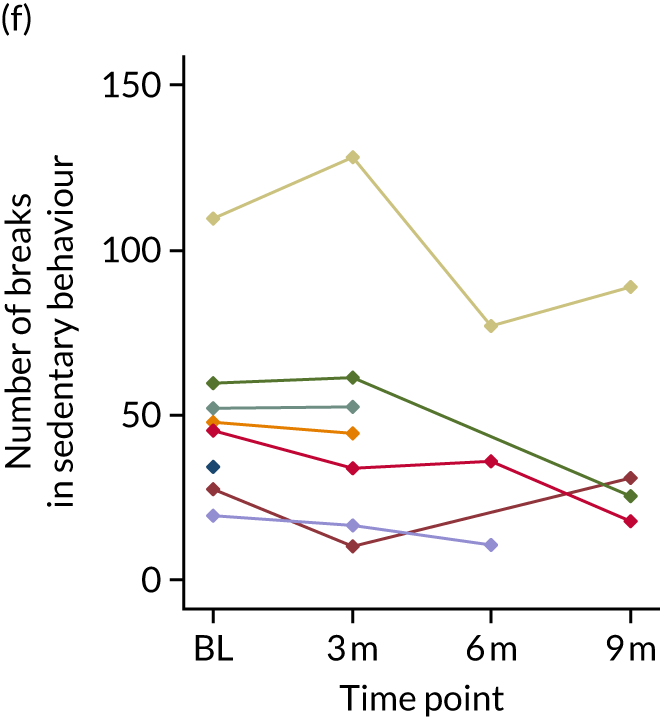
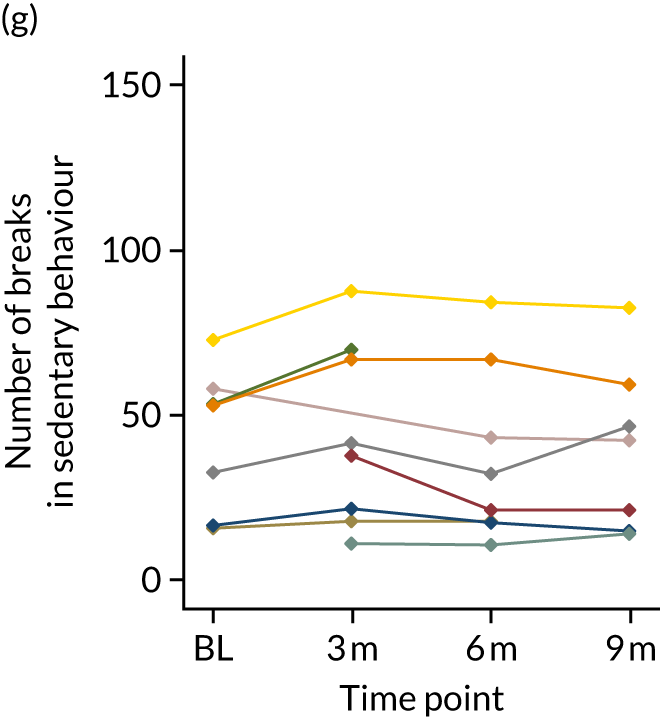
Appendix 9 Workstream 5: feasibility cluster randomised controlled trial – process evaluation
Introduction
There are limits to what randomised controlled feasibility trials of a complex intervention can achieve in isolation. PEs alongside such trials provide additional information to understand implementation (what is delivered), the theory and mechanisms of change (how the intervention and its components operate to effect change) and the contextual factors that shape outcomes. 61,131 PEs are also important in exploring programme theories, in facilitating understanding of the varied effects programme theories may have in different contexts, and in considering choice of process criteria and measures and approaches to examining implementation fidelity.
Although there is growing consensus on the need for PEs in trials and feasibility trials, there is a lack of consistency on what their appropriate content and scope should be, and there is considerable diversity in the design and methods employed. 131–134 Most PEs, for example, collect data retrospectively from participants about what occurred, so their perceptions are based on reflections from the vantage point of looking back in time. Longitudinal studies that focus on implementation processes as these occur over time are less common, yet they are important in that they allow us to distinguish between post hoc justifications of what happened and contemporaneous accounts of how it happened. In reporting the MoveMore PE, we describe the theory of change underpinning MoveMore, the evaluation methods employed and the key findings, including their temporal and contextual features.
MoveMore
MoveMore is a whole-home intervention and implementation process designed to reduce the amount of time that residents spend sedentary in the course of their day. It is aimed at changing how the routine work of care staff is carried out such that residents are encouraged and supported to move more in every facet of their day-to-day lives. Targeted at several organisational levels (CH, multiple staff roles and individual staff), implementation requires ‘buy-in’ from staff at individual and collective levels to make change happen. The heterogeneity of residents’ needs and circumstances, and the individual tailoring of the intervention to these, adds another level of complexity. The programme is intended to modify the way in which staff think, act and organise themselves, so as to initiate a process of change in the way residents think and act, and to reduce sedentary time. Thus, outcomes are produced through long implementation chains, operating through recursive feedback loops. 135
The programme adopts a systematic approach and set of steps to implement and embed the intervention in routine care delivery. This comprises a cyclical process of change, guidance and tools for staff to review current practice (observation), identifying goals and action plans to reduce sedentary time (from reflection on current practice to action planning), action (pursue action plans) and reviewing progress (evaluate what has been achieved). Implementation is conceived as a process, not as a one-off event. 136 Therefore, change is likely to be non-linear and multidirectional,137 in that the perceived success (or failure) of action plans will create the conditions for subsequent review and further action-planning. The commitment and skill of those leading the change and in working through each phase will affect the implementation and outcomes. Thus, there is a degree of unpredictability in the process (and outcomes).
Implementation is led by a team comprising key stakeholders in the change: staff, relatives and residents (if possible), facilitated by a senior member of staff. This synthesises a top-down and bottom-up approach to leading change. 138 Active involvement of senior staff with the authority and legitimacy to drive the change process forward is aimed at securing organisational commitment to introducing and embedding the programme, and the engagement of those directly involved in action to deliver it means that their views and experiences will inform its pace and direction. 139–141
Several strategies are in place to support implementation: provision of a manual, including an ideas bank of resources to assist staff in getting started and keeping going; training and support, comprising a series of three interactive workshops to introduce staff to the programme and to take them through each step in the observation, action-planning, action and review cycle; and facilitation support as necessary to respond to problems. In addition, ‘expert’ professional input to the workshops on the benefit of movement in CH routines is provided via a physiotherapist working in this setting, and an artist translates observations and action plans discussed in the workshops into visual images to communicate methods and ideas for change to the residents and wider staff group.
MoveMore is an exemplar of a complex intervention:61 it contains multiple interacting components, several organisational levels are targeted, and the change process is emergent and flexible. 142 In addition, the CH setting where the intervention is being introduced and with which it interacts is also dynamic, adding another element of complexity. 143
Research aims and objectives
The purpose of this PE was to test out and refine the theory of change underpinning the programme, to explore how and what was delivered over time and the factors that contributed to and/or inhibited change, and to explore the programme’s feasibility and acceptability in a CH setting. Research questions were as follows:
-
How was the programme understood by staff, and how and in what ways was it different from UC in the way it was enacted?
-
What were the necessary conditions to achieve the intended outcomes (‘active’ ingredients or essential components)?
-
How did what actually happened compare with what was intended (fidelity, including reach and ‘dose’)?
-
How did the intervention and implementation process interface with the organisational, relational and care context within which it was inserted?
Research design
We adopted a multiple-method, comparative case study design. The case study method is characterised by the depth and detail of information collected within naturally occurring bounded settings. 78–81 The aim was twofold: to convey what UC was across all study homes; and to provide a descriptive and analytic account of the MoveMore implementation process over time and the contextual factors that contributed to and/or inhibited it. We drew on different sources and types of data to provide breadth and depth of understanding about the intervention and implementation process from the perspective of different stakeholders (staff and residents), including those involved in leading the change.
Methods
All homes
A common set of qualitative and quantitative data was collected across all 12 trial homes to explore UC. This encompassed the pattern of sedentary time and features of the care environment relevant to care delivery. Trial researchers employed the trial-specific observational (Figure 18) tool at each measurement time point across all 12 homes to obtain a snapshot of resident movement at different times, in different locations and in respect of residents with different types of need. They also provided a narrative summary of any organisational and practice changes that had occurred over the preceding 3 months at each data collection time point.
FIGURE 18.
Observation tool and reflection sheet.
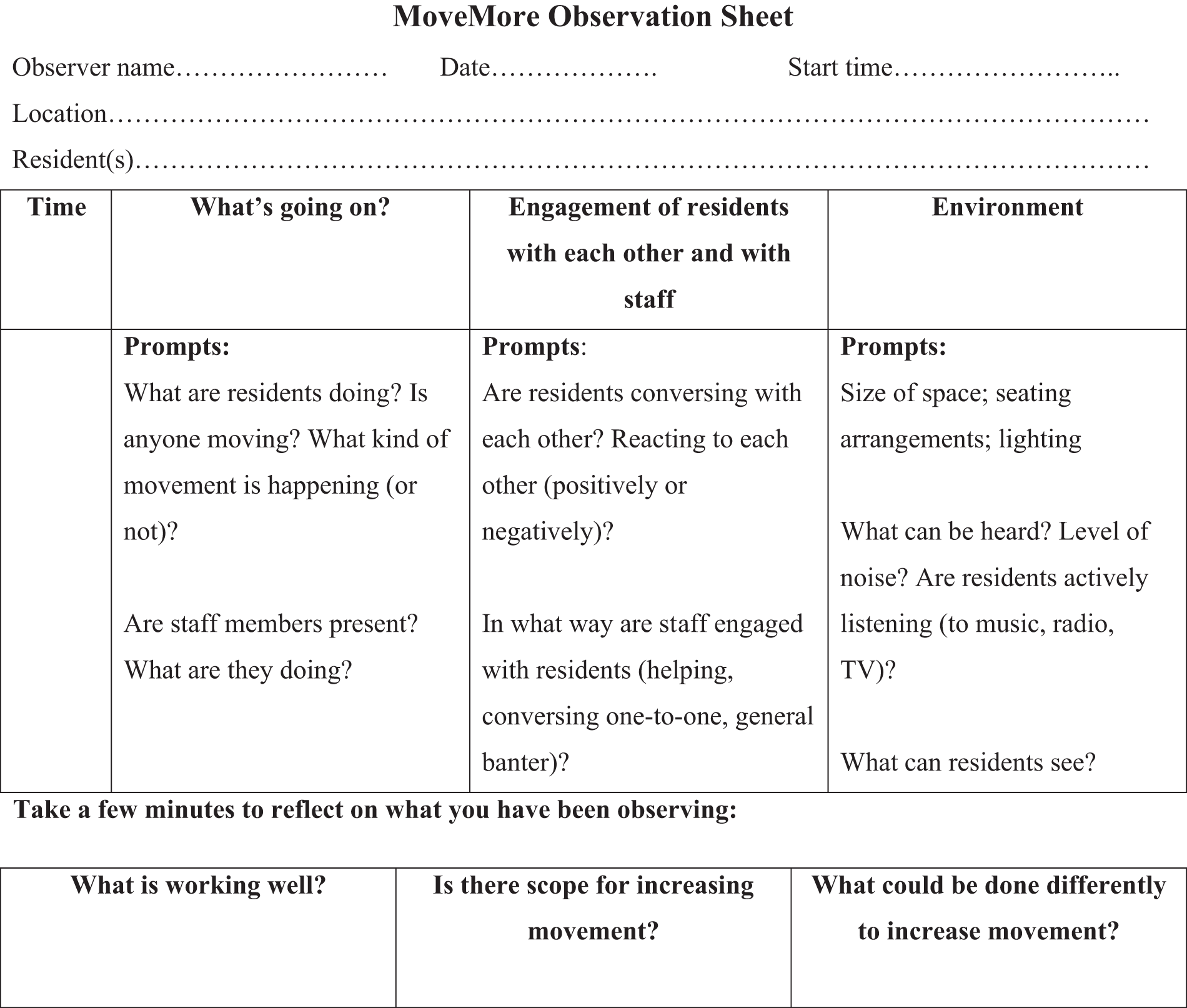
The PE researcher used ethnographic methods41,144,145 of observation, conversations and informant interviews to examine care delivery at baseline (approximately 5 hours in each home). Qualitative audio-recorded interviews were completed by the PE researcher at the conclusion of the trial with at least one senior member of staff in each home. Interviews adopted an open, flexible style, using a topic guide as an aide memoire. 146,147 This covered their experience of participation in the study, the value they attached to resident PA and movement, and how and in what ways this might have changed over the study. Fifteen interviews (with 17 participants) were completed.
Intervention homes
A common data set on the intervention and implementation process across all intervention homes explored how it was understood and engaged with by different stakeholders, and how it was enacted over time in the real-life context of each CH. We were particularly interested in the content, form and completeness of delivery, and the programme’s reach beyond the implementation team and the domains of movement targeted. 148 Multiple methods of data collection were employed:
-
Audio-recordings of the workshops provided a contemporaneous picture of the engagement of implementation teams, their conception of the intervention and how it was enacted during the preparatory and installation phases.
-
Collection of documents produced by implementation teams of their observations, action plans and reviews.
-
Ethnographic observation of care delivery and informant conversations with staff and residents at critical points in the study (prior to the introduction of the intervention, during implementation and at the conclusion of the trial). Approximately 15 hours were spent in each intervention home to capture the process and impact of the intervention.
-
Qualitative interviews with members of the implementation teams to explore the process of change over time and the factors constraining or facilitating it (16 interviews, 21 participants).
-
Conversations with residents – in our previous work, we found that informal conversations with residents proved particularly informative. For those with a cognitive impairment, for example, conversation in the context of concrete experience of activities produced richer and more meaningful information than the formal interview. These conversations covered residents’ perceptions of life in the home; views on movement, including the value they attached to it; and the opportunities provided to support movement in the home.
-
Conversations with staff – in addition to formal interviews, conversations with members of implementation teams and care staff occurred over the intervention period. Notes of all conversations were written up as part of fieldnotes.
Homes have been assigned a code to protect anonymity and individuals have been given pseudonyms.
Analysis
Interviews were fully transcribed and ethnographic fieldnotes were written up as expanded accounts as soon as possible after fieldwork. 41,149 Field journals were maintained for each home, documenting all contacts and summaries in chronological order. We employed an interpretive approach to analysis using grounded theory methods: concurrent data collection and analysis, constant comparison, search for negative cases and memo-writing. 82 The emerging data from individual CHs were discussed in regular research team meetings and topics for more focused data collection were identified.
We constructed each home as a case study, drawing together all data relating to it. We employed processes of familiarisation (multiple readings of all data sets), data reduction (coding) and connecting strategies150 (narrative structure and contextual relationships) to develop analytic themes and categories relating to UC. From the empirical data and an iterative review of the literature, we delineated key concepts, their properties and dimensions to characterise UC and its pattern of variation between homes. We adopted the same analytic approach in respect of the intervention to provide a within-case descriptive account of implementation over time, the engagement of staff with each step in the process and the barriers encountered. Emphasis was on delineating the sequence of implementation steps over time in the real-life context of the home and the factors that affected the temporal flow of action. We then compared implementation processes through cross-case comparison to discern generalisable features that might account for variation. Throughout, data analysis was conducted manually, moving iteratively between the empirical data, sense-making in relation to it and the review of the literature.
Research team roles and relationships
We gave careful thought to the distinct roles and relationships of research team members. Trial researchers collecting routine outcome data at designated intervals were blinded to the intervention and control homes. The PE researcher was unblinded: collection of implementation would not have been feasible otherwise. Facilitation support and problem-solving regarding the intervention were provided by the researcher facilitators organising and delivering the workshops. Separation of these roles was deemed necessary to convey to participants that the research was aimed at understanding how things happened and not about judging ‘performance’. The facilitation role was problematic at times in managing the line between providing support and proffering solutions. Across the research teams as a whole, systems were in place to prevent ‘contamination’ between trial researchers, PE researchers and research facilitators: separate offices, separate password-protected data folders and separate research team meetings.
Normalisation process theory
A sensitising framework
In framing data collection and analysis on programme implementation, we used NPT151–153 as a sensitising lens. In contrast to psychological theories of change that address individual behaviour, NPT focuses on microsocial processes that affect the implementation of a practice (or technique) in an organisation or clinical setting. NPT postulates four generative mechanisms that operate individually and collectively to explain how practices become embedded and ‘normalised’ in routine care: coherence, cognitive participation, collective action and reflexive monitoring (Box 5).
NPT contends that new practices become embedded when:
-
The work that defines and organises a practice/intervention is understood as meaningful and invested in, in respect of the knowledge, skills, behaviours and actions required to implement it, at an individual and collective level. This sense-making relies on people working together to build a shared understanding, including their specific roles and responsibilities, around a set of practices. (Coherence.)
-
The work is perceived as something worthwhile and appropriate to commit time and effort to, so as to bring about the intended changes and to drive new practices forward. It may involve rethinking individual and group relationships, including ensuring that other participants believe that it is right for them to be involved and that they can make valid contribution to the work. (Cognitive participation.)
-
The interactional work that people do operationalises a set of new practices in everyday settings; the allocation work underpinning the division of labour is built up around these practices as they are enacted in the real world; the resource work that relies on allocation of different kinds of resources and the execution of protocols, policies and procedures is directed at engagement of individuals and groups in these practices. (Collective action.)
-
The work of individual and collective appraisal on the worth of a new set of practices considers that the effects of the changes are attributable to these practices and that they fit with valued goals, and may lead to redefining procedures or modifying practices. (Reflexive monitoring.)
Normalisation process theory is useful in respect of the MoveMore implementation process. MoveMore does not simply involve individual behaviour change: it requires individual and joint action to secure change at the cultural, organisational and practice levels. Implementation uses and alters the roles and relationships between staff, and between staff and residents, and the new meanings, practices, roles and relationships are aimed at changing organisational culture, that is they become part of ‘the way we do things here’.
Although NPT locates implementation within the setting in which the intervention is being delivered, the dynamic nature of the context as it interacts with the intervention and implementation process has not been fully explored. Hawe et al. 143 offer important insights. They argue that an intervention may be viewed as ‘a critical event in the history of a system leading to the introduction of new structures of interaction and new shared meanings’. 143 The corollary is that pre-existing patterns of activity and shared meanings along with the social networks that connect people and settings operate in dynamic relationship with the intervention. In our study, this posed the need to explore how the introduction of MoveMore affects the organisational and interactional environment of the CH over time and how the latter, in turn, acts back to sustain or subvert it. This conception of context differs from the levels of analysis view154 in important respects. It directs attention to the ways in which individuals and groups are not passive recipients of context, but interact with and mobilise aspects of context to effect change, so that the same contextual factors may play out differently in different local situations. Moreover, context is not static but is evolving and changing, and features of context are not discrete but conceived of as configurations of forces. 155
Implementation fidelity
Implementation fidelity is generally defined as the degree to which a programme is implemented as intended. It is viewed as a potential mediator of the relationship between interventions and their intended outcomes156 and, therefore, as a key component to evaluating evidence-informed interventions. Even so, there is no consensus on the dimensions of fidelity that should be covered. Some authors157 consider that fidelity embraces five distinct dimensions: adherence, exposure or dose, quality of delivery, participant responsiveness and programme differentiation. Although all of these dimensions are important in ascertaining the scope and quality of what is delivered and their relationship to desired outcomes, some of them, for example how far participants engage with or respond to the intervention (participant responsiveness) and identification of the unique or essential features of programmes (programme differentiation), address aspects of programme theories, and therefore may be considered part of the wider PE, as we have suggested in Appendix 9, Introduction.
Carroll et al. 156 propose a conceptual model to explore fidelity. They distinguish between components of fidelity and the factors that moderate its achievement. Components of fidelity, they suggest, should include measurement of adherence and its subcategories: content, frequency, duration and coverage, where content refers to the ‘active’ ingredients of the programme of change. The degree to which the intended content or frequency of an intervention is implemented, they argue, is the degree of implementation fidelity achieved for that intervention. Factors that affect or moderate the level of fidelity achieved are intervention complexity, facilitation strategies, quality of delivery and participant responsiveness. One of the dilemmas here, however, is that the ‘active’ ingredients are subject to empirical investigation in respect of the intervention and implementation process. Thus, although the conceptual framework offers a sensitising lens for considering fidelity, there are particular features of complex interventions that require further consideration.
With regard to complex interventions, the meaning and significance of ‘fidelity’ is contested. Although there is acknowledgement that adaptation necessarily happens with implementation,158 some would argue that adaptations from the original model may have a positive effect if they make the intervention more contextually relevant. 158,159 Others160,161 report that programmes with high fidelity have better outcomes than those with low fidelity, based on research conducted in different settings (e.g. mental health).
Hawe et al. 142 consider that, although the conventional view of fidelity is that the form of the intervention has to be standardised (such that ‘fidelity’ means that the intervention is standard and replicable across sites), for community- or organisational-based interventions, it is the function of the intervention that is standardised and the form may vary across contexts. Moreover, for interventions relating to organisations, groups or communities, these authors143 suggest that a useful heuristic is to think of interventions as events in systems that either ‘leave a lasting imprint or wash out depending on how well the dynamic properties of the system are harnessed’. 143 For MoveMore, this would mean that, although the steps in the change process are standard, the form of the changes implemented will be shaped by the local CH context (level of movement at baseline, resident and staff profile, and organisational culture and practice). Fidelity, then, involves exploration of how the programme is enacted in the specific context of each CH over time.
One approach to fidelity that problematises the relationship between the innovation and the system within which it is enacted is that developed by Century et al. 148 They distinguish between ‘innovation implementation’ and the ‘implementation process’. Innovation implementation is the extent to which the innovation itself is enacted in whole or in part (which, in the case of MoveMore, is reduction in sedentary time in the four domains of daily life routines). The implementation process, on the other hand, includes how the change is implemented, as well as the contextual factors that contribute to and/or inhibit innovation implementation. In respect of each of these aspects, they suggest that the question for consideration is not simply ‘did it work?’, but rather ‘what parts worked and to what degree at different points?’.
This PE in the feasibility trial focuses on adherence at two levels: (1) the engagement of the implementation team in the cyclical process of change within and between the workshops and CH environments, and (2) the programme’s reach beyond the implementation team to effect change at the CH level.
Findings
What is usual care?
In delineating UC, we considered, first, features of the overall care environment and, second, how movement was understood and enacted in daily life routines.
Care environment
The features of the care environment examined were the person-centredness and flexibility of routines.
Person-centred care
Although the concept of ‘person-centred’ care is ubiquitous in UK health and social care policy discourse as synonymous with care quality, there is no consensus on its meaning either in policy134 or in research,162,163 so it is difficult to determine what it might look like in practice. Common dimensions of ‘person-centredness’ include care that is individualised, caring and enabling. 164 Although these components are not exhaustive, they are helpful for our purposes in characterising person-centredness in a CH practice context.
Drawing on observation and interviews, we defined ‘individualised care’ as care that was based on staff having meaningful knowledge of the person (biographical, current preferences and needs); ‘caring’ as reflected in a style of communication that was respectful, warm and responsive to residents’ expressed emotion; and ‘enabling’ as care that involved providing assistance such that a person’s level of competence and confidence was enhanced and independent action was supported. These features were interconnected.
We found that, in the majority of homes at baseline (n = 9), staff demonstrated meaningful knowledge of residents, which was reflected in their encounters with them:
I sit in a chair in between two residents, Betty (smiling and alert) and Peter (who is dozing) . . . we talk for a while about Betty’s family . . . local places to visit, and what she liked to do when she was younger . . . and coming into the home . . . Betty became distressed after saying this with tears in her eyes and I was concerned that my question had upset her. I apologised . . . she replied ‘Oh no, I get like this, I have days like these’. Tina, a carer nearby, remarks to Betty ‘we have our good and bad days, don’t we Betty? And today is one of them bad days.’ Betty agrees with Tina and then thanks her for helping her in her room this morning.
CH9, fieldnote 1035
Engaging with residents in a personally meaningful way was also used to encourage and support residents to take part in leisure activities:
Pat is asleep in a double chair curled up. Two residents are dozing in lounge chairs, sat either side of Pat. Eileen swaps activities so that residents are now using polystyrene sticks to hit a balloon backwards and forwards to her as she throws it towards them and calls out their name. Eileen gives the residents lots of encouragement, e.g. ‘you are doing so well’, ‘come on, keep it going’, and the residents, on the whole, appear to be enjoying the activity. Fred asks every so often ‘Can I just go and talk to somebody?’ Eileen tells him to hang on 5 minutes. She engages Fred in a brief conversation about where he rode his bicycle and asks Maisie if she used to play rounders at school as she is very good at throwing. Eileen often tries to get the residents engaged in a dialogue about their past and their skills, and I think that they enjoy this interaction (smiling, answering back, although it is not always understandable to me).
CH12, fieldnote 1105
In three homes, personally meaningful knowledge of residents was less evident, because of either high staff turnover or poor staffing, such that encounters were predominantly focused on the task, with little or no attention on the resident as a person:
I notice two carers using a hoist. At first I thought that they were putting it away because I could not see from where I was seated the residents who sat in this area, and because the carers were talking over the hoist to each other . . . As the hoist was raised, I see a female resident sat in it. One carer remarks to her ‘don’t be so grumpy’. The resident’s facial expression to me was one of distress. The carers continue to talk amongst themselves whilst lowering the woman into a chair. They then move the hoist out of the lounge area . . .
CH3, fieldnote 1510
In most homes and among most staff, communication with residents was warm, respectful and responsive. In some homes, we observed specific incidents involving individual staff in which the style of communication did not take account of residents’ expressed emotions, especially those with a cognitive impairment. In a couple of homes with a high proportion of residents with dementia who had poor verbal ability, communication practices reflected awareness of and sensitivity to observational cues and individuals’ expressed emotion:
Ted is uttering something that I cannot understand. His voice gets louder and he moves his upper body erratically, as if in distress. Carrie comes back into the room and goes immediately to him. She sits next to him, placing her hand on his and asks in a soothing, gentle tone if he is alright. Ted replies ‘no’ and says something else which I cannot hear. Carrie gets up and returns a few moments later with a beaker full of juice. Ted thanks her and gulps down the entire contents. He then sits back into his chair, more relaxed. Carrie leaves when Ted appears to have calmed down . . . Ten minutes later, there is shouting and distress from Ted again. Carrie comes in and goes to him straight away, gently touching his arm . . . Ted relaxes back into the chair and the quietness in the room returns.
CH1, fieldnote 1341
Care homes were more variable in their practice in providing assistance to residents. Six homes adopted a consistently enabling approach in respect of most tasks of daily living. This involved balancing risk and resident choice, and putting strategies in place to manage risk. In a conversation with the PE researcher, a 90-year-old resident, George, recounted how he had walked to the polling station to vote in the recent parliamentary election and often took the bus into the local town. The manager drew on George’s experience in one of the workshops to convey their enabling approach:
George is physically frail and at risk of falling but he’s able to understand the risks involved. We’ve done a risk assessment and taken steps to reduce the impact of a fall (protective clothing). Some staff are nervous about it but we want to support him in keeping going.
CH2 manager
Although the extent to which enabling was pursued in this example was unusual, it illustrates features of the care processes involved in the approach: supporting resident action and ensuring that potential risks are actively managed.
In a further four homes, practice with regard to enabling was inconsistent between staff and/or practice was enabling in some tasks but not others. For example, some staff provided support and encouragement to residents with mobility difficulties to take some steps in transferring between their chair and wheelchair, whereas others did not; in some homes, individual drinks were given to residents with an accompanying snack directly into their hands or on a table, whereas, in others, residents were encouraged to add milk and sugar themselves, and to lean over and choose a snack from a proffered box/plate. In two homes, practice overall was characterised as ‘care done to’ as opposed to ‘enabling’. In one of them (CH3), although the level of physical dependency of residents was very high, a hoist was used routinely to transfer people who required the support of two carers (around half of residents). Staff acknowledged that this was what was expected of them and was ‘normal’ practice, even though some residents were capable, with encouragement, of walking a few steps.
Flexibility of routines and practices
All homes adopted some flexibility with regard to some aspects of day-to-day routines. Typically, residents were enabled to get up and dressed at a time of their choosing and have breakfast in their room or in the dining room. For those who were dependent on carer support to wash and dress, the degree of flexibility was constrained by staff availability. Similarly, residents chose the time they went to bed, subject to similar constraints.
The main meals of the day (lunch and evening meal) were, in all homes, provided at set times (12.00–12.30 and 16.30–17.30) and were to be taken in the dining room or a person’s own room. There was generally a permissive approach to residents staying in their own rooms during the day if they wished, although some homes actively encouraged residents to socialise with others in the communal spaces or to come out of their rooms to take part in organised social and leisure activities. In all homes, relatives and friends of residents were welcomed. In most homes, there were one or two people who spent time in the home with their relative on most days, providing practical assistance at mealtimes, conversing or reading aloud, playing games or doing crosswords. They also interacted with and kept an eye out for other residents.
More variability existed between homes in the extent to which residents could get a hot drink between set times: in some, this occurred routinely as epitomising the ‘homely’ environment staff espoused to create; in others, residents would be asked to wait until the designated time. A small number of homes enabled residents who were deemed able to get a drink from the kitchen. There were several where residents moved freely between spaces, including between floors. In others, there was little movement from lounge areas beyond that relating to regenerative activities (eating, toileting), which not only reinforced the time spent sedentary, but was a factor that contributed to minimal resident-to-resident interaction. All homes had access to outdoor spaces, most of which were attractively landscaped. With a couple of exceptions, residents were able to access these only if accompanied by a member of the care staff.
Across all homes, a notable feature was how most residents’ daily lives were lived within the spatial boundary of the CH. In two homes, some residents were regularly (weekly) taken to a local community centre/club; in others, organised trips out occurred as special events or celebrations (a birthday treat with a visit to a pub or cafe); in yet others, relatives might take a resident out. The narrow spatial organisation of CH life also contributed to the narrowness of residents’ social lives.
Opportunities for engagement
Here, we consider UC in respect of resident access to social, leisure and stimulating activities, and conceptions of ‘movement’ and the significance attached to it in daily life routines.
Social, leisure and stimulating activities
Homes varied considerably in the opportunities available for engagement in social, leisure and stimulating activities. Not all homes had dedicated AOs in post, and even those that did (three of five intervention homes and five of seven control homes) varied in the level of resource available. Thus, AOs mostly worked part time (a couple of full week days, or mornings or afternoons on weekdays only). Three of these eight homes had varied and extensive short-interval (weekly) and medium-interval (monthly) organised activities for mental and physical stimulation (e.g. quizzes, games, discussions, creative writing, crafts, baking, indoor bowling, chair exercises) and special events at longer intervals internal and external to the home (e.g. external entertainers, mini-bus outings, theatre/cinema trips). The rest had a narrower range of organised activities [games, weekly trip out to a community centre for dancing and a drink, music and special events (external entertainers)]. Of those homes without an AO, there were spontaneous short-interval events (e.g. music and singalong, games, chair exercises) and organised medium-interval events using external resources (e.g. Music for Health, exercise class) or CH staff (e.g. film nights, reminiscence). In all homes, care staff engaged in some one-to-one pampering work (e.g. manicure) and there was access to a hairdresser/barber. This pattern of variation existed across intervention and control homes. Although the home with the most extensive and varied programme of social, leisure and stimulating activities was a control home, it was rivalled in its range of stimulating and creative activities for a ‘healthy mind’ by one of the intervention homes.
Understanding the significance of movement in daily life routines
Overall, most care managers conveyed a general belief that ‘exercise’ and keeping ‘active’ was a ‘good thing’ to maintain residents’ well-being and to facilitate their engagement in social life. This awareness was a factor in their interest in taking part in the study. By contrast, thinking about everyday life activities through the lens of movement was not common.
MoveMore implementation
We examined the process of implementing MoveMore as it evolved over 9 months. Focus on process over time conceptualises improvement interventions not as single, discrete changes, but as ‘facilitated evolution’. 165
Once homes were randomised to the intervention, it was envisaged that the MoveMore lead, a senior member of staff identified by the home on recruitment to the study, would be contacted by telephone to establish a date for the first workshop. The MoveMore lead would then bring together interested individuals from among the staff group (and relatives/residents if they wished) to form an implementation team and take the intervention forward. At the first workshop, the implementation team would be introduced to the programme. Homes had only been provided with general information about the purpose of the study and its aims when they were recruited.
An important change in how the programme was introduced occurred following the experience of the first intervention home. It proved difficult for the MoveMore lead to commit staff to participation in the workshops in the absence of clear information on what they were signing themselves up to do. An additional step pursued in all subsequent intervention homes was a face-to-face meeting between the MoveMore lead and research facilitator to introduce the manual; supporting resources; and the role, purpose and composition of the implementation team.
Stages of implementation
Two homes were ‘full implementers’, pursuing change broadly as intended; two others were ‘partial’ implementers; and one was a ‘failed’ implementer. We drew on a stages-of-implementation framework from a review of implementation research8 to examine the stage reached and to determine what were barriers to or facilitators of progress. The framework comprises six stages (Box 6).
-
Exploration and adoption: making a decision about whether or not to proceed based on the match between the needs of the organisation, assessment of the intervention as relevant, and willingness/capacity to deploy the resources necessary to carry it through.
-
Programme installation: active preparation to begin implementation, for example introducing the programme to staff, recruiting people to lead the work and organising training.
-
Initial implementation: first steps in making change happen. Typically a challenging period during which confidence in the decision to adopt is being tested and the implications of the resource investment are becoming evident.
-
Full adoption: programme becomes fully operational.
-
Innovation: period during which the programme is being refined and expanded, and desirable changes are being considered for inclusion as part of routine practices.
-
Sustainability: the goal at this stage is long-term survival of the practices introduced.
The MoveMore exploration and adoption stage occurred through the lengthy process by which homes were recruited to the study and pursued through meetings with CH managers. Programme installation comprised identifying a lead and individuals who would take implementation forward in the home and participate in the workshops. This overlapped, in part, with the next stage: initial implementation. This started with observations, then action-planning and review as reciprocal, interactive processes: learning from each workshop was enacted in the home, brought back to the subsequent workshop to reflect on the experience of doing so, the barriers and successes encountered, and then moving forward in the home to the next stage in the cycle. Full adoption involved completing the full workshop sequence and enacting the cycle of observations, action-planning and review over the 9-month trial. Stages of innovation and sustainability are those during which the programme is refined and expanded, and desirable changes are considered for inclusion as part of routine practice. Sustainability is a goal for long-term survival of the practices introduced. The two ‘full implementer’ homes had begun to introduce organisational and practice changes that had potential to embed implementation in CH life.
We describe these varied implementation types, comparing implementation processes, to draw out generalisable features that might account for variation.
‘Full implementers’
Two homes proceeded to full adoption: they completed the three workshops, conducted observations in their homes, developed action plans flowing from these and carried through work to effect change (CH4 and CH5). Their local contexts were similar in some respects and dissimilar in others. Both care environments were person-centred in all dimensions and were flexible in their routines and practices. They were similar in their mean level of resident dependency based on mean BI scores [CH5: 11.5 (SD 4.02), CH4: 11.9 (SD 4.95)]. CH5 was better resourced in terms of space, staff-to-resident ratio and skill mix (including having an AO). Their respective resident profiles were different in terms of age {the mean age of residents was lower in CH4 [78.6 (SD 11.84) years] than in CH5 [91.3 (SD 6.10) years]} and in the proportion of residents with dementia (just under half in CH4 and nearly two-thirds in CH5).
An ‘exemplary’ implementer
Care home 5 was an ‘exemplary’ implementer. Installation of MoveMore was pursued through participation in the workshops; each step in the change process was taken back and enacted in the CH environment (observation), and reflected on in the subsequent workshop (action-planning); and the action plans that were developed were tried out in the home and then reviewed (review and forward movement). Initial implementation was achieved within 8 weeks from the introductory meeting following randomisation.
Engagement in MoveMore
The implementation team included a range of stakeholders: senior home staff (manager and deputy manager), catering manager, AO, team leader, care worker, housekeeper and chef. Although the deputy manager assumed the work of intervention ‘driver’ and the AO took responsibility for ensuring completion of the documentation, other members of the team played a part in the implementation work, as either active facilitators (the manager) or contributors within their own spheres (the chef conducted observations, reflecting on and developing action plans in relation to them with the catering manager). The workshop venue was a room in the organisation’s head office, in a separate location to the CH. This offered space for uninterrupted discussion.
From the outset, there was an understanding that, for change to occur, communication and engagement of the wider staff group was necessary. Thus, the deputy manager involved care staff outside the team in carrying out observations and opening up discussion on ideas for facilitating movement. In this respect, observation, reflection and action-planning were conceived of as iterative and linked processes brought together through discussion between individual members of the team, including in the workshops and in established forums, such as handovers and staff meetings.
Installation and initial implementation
From a care environment perspective, there was acknowledgement in the first workshop and in conversations with staff that the home had hitherto been very good at promoting activities for a ‘healthy’ mind. However, movement, and its benefits for well-being, had not been at the forefront of staff awareness. There was much talk about the changing resident profile – physical frailty at point of admission and increasing cognitive impairment – that required re-evaluation of how they delivered care. Even so, it also seemed that the dominance in discussion of the challenges of residents living with dementia was at odds with the actual proportion of residents with moderate/severe dementia in the home.
In common with other study homes, prior to taking part in MoveMore, senior staff had begun to consider movement in the context of their resident profile and the physical environment. Their hope regarding participation was that movement could be incorporated into care routines, notwithstanding the cultural, normative and environmental obstacles they would encounter.
Between the first and second workshop, a period of 2 weeks, team members conducted observations and reflections within their different spheres. There was a sense from senior staff that the creation of momentum was critical to moving forward. By the second workshop, team members had completed six observations and reflections. These embraced observations of individual residents in the main home selected on account of their poor mobility, use of communal space in the dementia unit and its effect on resident movement, and the breakfast routine in the dining room. A learning point emphasised by participants was that, if residents were to be encouraged to move more, the strategies adopted had to be meaningful to them.
Among participants, their experiences of observing practice had enabled them to ‘see’ things not only as staff going about their work, but also how the environment might be felt from the perspective of residents with varying interests and needs. Furthermore, individual, joint and team reflections on their observations provided the head room to consider creative ways to explore ‘out of the box’ solutions and how they might go about making change happen. Action-planning in this respect was seen to flow from the observation and reflective process, with the additional element of establishing the ‘how-to’ steps to secure desired changes. The artist translated ‘challenges’ and ‘solutions’ (observations, reflections and action plans) into visual images. These were subsequently presented as pictures and displayed in the communal and staff spaces as a means of communication, and as an aide memoire to foreground movement in routine practice.
Two issues in particular were reinforced in this second workshop and picked up by the team: action plans might not work and so should be open to review (both the objective of the action plan and the steps to achieve it); and an aspect of the process should include how to engage the wider group of staff in the work. Preparatory to the third workshop, team members were to develop, write up and try out action plans based on their observations.
Fieldwork in the period between the second and third workshops revealed that work on translating observations into action plans was proceeding and several action plans relating to individual residents were being tried out. These involved negotiation with the resident and, when possible, support and encouragement was sought from family members. As a means of engaging care staff beyond the team, the MoveMore lead had also elicited care staff in conducting observations, freeing up time from usual routines by helping out with care tasks. Nine observations and reflections were completed by care staff in different settings, at different times, focusing on individual residents and small groups. Discussing observations with individuals subsequently had generated lots of ideas on how movement could be enabled and these were being written up by the MoveMore lead as action plans.
From initial implementation to full adoption
The third workshop considered action plans developed by the team, drawing out key learning points. What might appear initially as relatively simple changes could have unanticipated consequences requiring further action. For example, expanding ‘meaningful activity’ for residents, a goal of the AO, involved shifting the focus of her work a little from group to one-on-one activity. This involved the development of further action plans relating to supporting care workers to take on some group activities. PE observation at 6 months noted that a new care staff member was confidently leading a group activity with nine residents: a quiz, followed by music and enthusiastic rhythmic swaying and foot-tapping. The example in Box 7 illustrates an action plan that was incorporated as part of the home routine.
Martin (chef) and Liz (catering manager) observed the breakfast routine together. They noted that residents were brought into the dining room, seated and waited to be served their usual preference (choice of cereal, toast, etc.). Although apparently the most efficient method, they reflected on whether or not residents could be enabled to make their way to the serving hatch and choose what they wanted (workshop 2). An action plan was developed and action ensued. At 6 months, the MoveMore lead, when interviewed, described what followed: cereals were placed in brightly coloured boxes at the serving hatch, visually indicating their varied content (observed by the PE researcher). Residents were encouraged to go to the hatch and choose what they wanted. The result was seen as more ‘person centred’ and movement orientated, and visual cues were regarded as more meaningful for residents with a cognitive impairment.
A significant development from the work was an initiative of the MoveMore lead and catering manager aimed at routinising the process of change as part of the care culture. In outline, this involved training all staff in MoveMore principles and processes, including observation and action-planning, which would be reviewed in staff’s quarterly supervision sessions.
From innovation towards sustainability
Over the subsequent 6 months, action plans were reviewed in routine forums, for example those relating to individual residents were incorporated in their care plans, specific organisational changes became part of the care culture, and the process of embedding movement through training and supervision had begun. At the 9-month time point, one training session had been delivered to staff in varied care roles across the home and others were planned. Enacting such systemic change had involved considerable work over a 6-month period, which was more sustained and less immediate in its impact than some of the practice changes for individual residents.
For senior managers and staff involved in implementation, the MoveMore intervention had resulted in movement being placed at the forefront of CH culture, and in systems and processes being put in place (training and supervision) to embed this change in routine care delivery.
A ‘delayed’ full implementer
Engagement in MoveMore
Care home 4 was characterised as a ‘full implementer’, albeit delayed. Similar to CH5, initial steps in programme installation were embraced by the manager with enthusiasm. The first workshop was organised within 2.5 weeks of the programme induction meeting and the second workshop within 3 weeks of the first. There was then a hiatus (14 weeks) before the third workshop took place, meaning that MoveMore installation was completed only shortly before the 6-month data collection point. This was a consequence of contextual factors with direct impact on the organisational and care environment in which the intervention was delivered and which, in turn, affected the priority attached to the work of MoveMore implementation. In the following narrative, we draw out the temporal sequence of events and our interpretations of them to inform understanding of the implementation process.
At the induction meeting, preparatory to installation, the manager had indicated that implementation would be pursued by a ‘loose’ group of staff. Although she would take responsibility for pushing forward the change process, participation in the workshops would depend on who was working in the home on the day.
Installation and initial implementation
The first workshop allayed some of the research facilitator’s concerns about leadership and commitment: taking part were the manager, one of two deputies, a senior care worker, a care assistant and a cook. The venue (dining room off the main lounge) meant that proceedings were subject to interruptions. These included residents making their way into the dining room and adjoining kitchen, and participants rushing off to deal with a crisis event: episodes which were revelatory of residents’ ease of access to spaces within and across the home, and the absence of uninterrupted headspace for staff to reflect and plan.
Conveyed in this first workshop was a staff group committed to improving the care of residents. From the manager’s perspective, the main challenge was that many of the staff, although very caring in their relationships and encounters with residents, were resistant to changes in established work routines and very task focused. Many had worked for many years in the home (both deputies had been employed there for > 20 years, working their way up from being care assistants). The manager was relatively new, being < 3 years in post. This picture of an established staff group was also evidenced in the annual staff turnover rate (11% – one of the lowest of all participating homes).
The value of resident movement, conveyed by the physiotherapist, found resonance among participants. They also indicated that increasing movement would require changing staff culture and practice so as to motivate residents. Similar to CH5 staff, the team considered that movement had to be incorporated as part of a resident’s daily life (i.e. that it was purposeful and meaningful).
Participants, especially the deputy and team leader, were keen to try out the observation tool. In accordance with the significance she attached to engaging the wider staff team, the manager proposed to discuss the study in the next staff meeting.
Between the first and second workshop, five observations were completed by individuals within the implementation group and by other care staff. These formed the basis for reflection and discussion of action plans in the second workshop. Continuity of participation was provided by the deputy manager (Marion) and the second deputy (Cheryl); a carer also took part. The manager was occupied elsewhere, and the senior carer and care worker who had previously attended were not on shift. The artist was unable to attend.
Observations embraced individual residents with poor mobility, the pattern of movement in the main lounge and the reluctance of residents to move from ‘established’ seats to take part in activities elsewhere. The process of observation was perceived as valuable: ‘seeing’ and reflecting on positive and negative features. As in CH5, discussion on observations and reflections appeared to ‘free up’ thinking about changes that could be made. For example, observation of how specific staff encouraged a resident to improve mobility with assistance, and its effect on the resident’s mood and in reducing isolation, offered a mirror for other staff and a basis for action-planning to change practice. The extended periods of sedentary time spent by residents in the main lounge directed attention to the seating arrangements and established resident routines. Chairs were organised in two parallel lines facing each other, discouraging interaction between residents. Several residents had ‘their own’ seats and were reluctant to move from the lounge for fear of losing them, limiting participation in activities not centred on this space. Ideas for challenging routines included reconfiguring the seating in the main lounge and introducing ‘chair-swopping’: periods during which residents were asked to ‘swop’ seats. Ideas were to be written up as action plans and tried out in anticipation of the third workshop, to include the artist. With 1 month before the 3-month data collection point, programme installation appeared on track for completion within or around 3 months, as in CH5. Box 8 provides an example of action for an individual resident.
Gladys, a resident who mainly stayed in her room, sitting in her chair, was observed being assisted by two care staff to get up in the morning. She was assisted with every aspect of personal care and in transferring from bed to chair, grimacing in pain with every movement. Although chronic obstructive pulmonary disease restricted and made movement painful, prolonged lying in bed was exacerbating difficulties breathing. First steps in the action plan were initiating a medication review by her GP, observing her response to increased medication and further review to optimise the balance between securing pain relief and reducing the adverse side effects of medication (drowsiness and hallucinations). Next steps involved negotiating with Gladys to do a little more for herself: leaving the breakfast tray by her chair so that she had to get out of bed to eat, then encouraging her to come down to the dining room for lunch, then to spend a little time in the lounge. Over a period, there were still days when Gladys would not move from her room, but, on most days, she spent some time in the smaller lounge. She was observed here by the PE researcher.
Informal discussion with a member of the implementation team during the 3-month data collection point suggested that work to develop and test action plans was being pursued. For example, chairs in the lounge were reconfigured to facilitate ‘chair-swopping’. This was successful in initiating interaction between different residents and in generating short bursts of movement, also documented in the PE fieldnotes. The refusal of one resident to move, after reluctantly agreeing initially, involved further negotiation with her, including enlisting her relative’s support to persist with the initiative. This resulted in some revisions: ‘swopping’ at some times and on some days only, as long as it was achieving the objective of enhancing interaction and movement. The experience had also directed attention on other initiatives to address the same goals. Despite progress, written action plans were not available. It seemed timely to organise the third workshop to examine the change process and how it was being captured.
Momentum falters
Over the subsequent weeks, it proved difficult to arrange a time for the third workshop; a support meeting, involving both research facilitators, was organised. Although the manager indicated interest in continuing with the intervention, there was a palpable sense of loss of energy, as well as frustration with some staff who persisted in the view that a colleague was ‘slacking’ by spending time in conversation with a resident. The recent CQC inspection (within weeks of the second workshop) and assessment (‘requires improvement’ in documenting systems and processes) had also affected staff morale and prioritised work in response to the inspection by senior staff.
A third workshop was planned to include the artist – now 14 weeks after the second workshop, and between the 3- and 6-month data collection points. Staff appeared unprepared for the workshop and the manager was preoccupied. The deputy (Marion) had taken on the work of steering MoveMore, but was not on shift. There was the possibility that we had reached the nadir of the intervention in the home.
Resuming momentum
The desultory response was somewhat belied by location of the MoveMore documentation with several newly completed observations and action plans, suggesting that work was under way. Discussion with the second deputy manager (Cheryl) indicated that progress was being made in each of the areas that were the subjects of action plans. The artist created images capturing aspects of the work that had been described for the team to use in engaging the wider group of staff with MoveMore, which were subsequently displayed prominently in the communal spaces.
Full adoption
From around the fifth month of the intervention, the deputy manager (Marion) emerged as the de facto MoveMore steer, facilitated by support from the manager. In addition to the focus on reducing sedentary time, there were two features of the implementation process that extended the programme’s reach to the wider staff group: (1) new care staff were enlisted in conducting observations, including two night staff; and (2) the requirement on the home from the CQC inspection to develop more detailed resident care plans was used by senior staff, led by Marion, as a vehicle to incorporate action plans around movement for individual residents. This drew on staff observations and direct work with residents to elicit preferences to inform plans. The work involved was time-consuming and slow, but was regarded as setting the ground for incorporating observation and action-planning into CH routines. By the end of the intervention, there were specific examples from conversations with residents that action plans for individuals were in place; for example, a resident with very limited movement was being supported daily by care staff to practise exercises developed by the physiotherapist.
As care plans became the means through which action plans were pursued, a communication book was initiated for staff to record and sign the action and progress, reviewed on a monthly basis by the manager.
Interviews with senior staff and carers at the 6- and 9-month time points were positive about the impact of MoveMore. The journey was described as very difficult (some staff were resistant to change, but the team was persevering), but the benefits for residents were seen as worthwhile. For staff, the process of change had altered their approach:
You’re always rushing about and you don’t, sort of, take stock of what is really going on. But . . . now I do sit back and take stock; who’s doing what, when and where and what times and . . . it’s just what I do.
Senior member of staff, CH4
Other changes from what was ‘UC’ at the outset of the study were in place or being planned in the home: an opportunity for a collaborative project with an external organisation for a dancer to work with residents was taken up, and a group providing physical and mental stimulation through exercise and games was engaged to come in on a monthly basis. These ‘external’ events were regarded as additional to but not a substitute for the day-to-day work of care staff with residents in supporting movement.
Innovation and towards sustainability
A primary route through which MoveMore was adopted – incorporating movement as part of the care-planning process and as a specific aspect of individual resident’s care plans – was also a strategy for routinising movement in CH routines. At the home level, initiatives were also being pursued. Individual care staff were encouraged to take forward ideas for regular ‘events’ with residents, for example advocating and securing funding for a karaoke machine to enable them to enhance movement through music, purchase of a broader range of materials to work with residents and new garden furniture in conjunction with the development of the external space as a safe environment for residents to spend outdoors.
‘Partial implementers’
We characterised two homes as ‘partial implementers’ (CH1 and CH3). They differed in how far they moved towards full adoption, in the extent to which they embraced the MoveMore objectives, and the degree to which they were able to extend the reach of the intervention beyond the implementation team.
Structurally and in their care environments, their local contexts were very different. CH1 was a specialist, local authority-managed dementia facility; CH3 was a dual-registered nursing home and CH, which was owned and managed by a small national provider. CH1 was characterised as person-centred in all dimensions; CH3 was task focused, risk averse and exemplified a ‘cared-for’ culture. The nature of their respective resident profiles posed particular, albeit different, challenges. All residents in CH1 had dementia, the highest proportion of all study homes. The permanent residents – those eligible to take part – were those who remained after a policy was introduced in 2012 to reduce the number of permanent beds. This meant that there were no new permanent admissions until after the trial started, when the policy was reversed and the numbers of permanent beds increased. This was reflected in their high median length of stay (64.8 months, range 36.5–88.5 months), compared with that of CH3 (14 months, range 8–24 months). Self-care ability of residents in both of these homes, as measured by the BI, was the lowest of all study homes, with less variation in CH1 [mean 5.0 (SD 2.86)] than in CH3 [mean 6.3 (SD 5.46)].
Partial implementation: process extended in time
Care home 1 proceeded in the direction of ‘full adoption’, although it did not quite attain it. At the same time, the process of implementation ensued over an extended time in flurries of action and long periods of inaction.
Engagement in MoveMore
There was a lengthy gap (10 weeks) between randomisation and the first workshop, which took place within 1 month of the 3-month data collection stage. The difficulties experienced prefaced a change in the process of engaging homes in MoveMore implementation.
The first workshop was attended by the deputy manager (and designated implementation lead), team leader, senior carer, a member of the domestic staff and a relative: all staff had worked in the home for between 8 and > 20 years. In addition to the two research facilitators, the physiotherapist also took part. Key challenges in increasing movement in the home from the perspective of staff were twofold: the level of physical frailty and cognitive impairment among their permanent residents, and the multiple and complex demands on staff in working with diverse groups of people (i.e. permanent residents, those receiving intermediate care and those on short-term respite). In terms of their residents, they saw the benefit of PA in terms of mental well-being, and were enthusiastic about opportunities for increasing movement in residents’ daily life routines and for trying out the observation tool.
Installation extended in time
Following the first workshop, there was a further time lag in getting the second workshop organised. In part, this was caused by the fact that the 3-month data collection for the trial was due which would put demands on the home. In addition, the implementation lead was preoccupied with preparing documentation for their CQC inspection visit. A support meeting involving the research facilitators 6 weeks after the first workshop elicited continuing commitment to engaging in MoveMore implementation and frustration at being unable to prioritise working on it. Both the implementation lead and the care team leader had undertaken observations, but were concerned as to whether or not they ‘had done it right.’ The research facilitators reiterated the purpose of observation as taking time out from routine work to ‘look at’ an aspect of practice through the lens of movement and to reflect on whether or not, and in what ways, there was potential to increase movement. It was a tool to explore current practice as a launching pad to identify aspects for improvement. It was for them to decide what was right. We discussed a couple of observations both had done and assured them that they provided a basis for considering next steps as envisaged in the programme.
The second workshop occurred 1 month later, involving the implementation lead, the care team leader and a senior carer. Four observations had been completed relating to general features of practice: reinforcing an enablement approach in illness recovery, extending meaningful activities that incorporated movement (use of outdoor space), providing opportunities for interaction between residents, and developing action plans in respect of an individual resident around engagement in meaningful activities. Following discussion of the action-planning process, they considered that they had enough to work on to expand their reflections into action plans and try them out prior to the next workshop. An additional point was to involve the newly appointed AO as part of the implementation team. Although involvement of the artist in the second workshop to capture discussion on action plans was conceived of as part of delivery at this point, it was not possible to synchronise mutual availability. It was agreed that this would occur at the following workshop.
The third workshop, with the artist, occurred just over 4 weeks after the second workshop and shortly after the 6-month data collection. It was intended to review the action plans developed and action arising from them. Days before it was due to happen, the implementation lead communicated that he had been under ongoing pressure relating to both the audits being carried out in preparation for the CQC inspection and taking on managerial responsibilities on account of sickness among senior staff. It was agreed, however, that the workshop would go ahead, attended by the de facto implementation team – team leader, care team leader and senior carer.
Initial implementation
Although action plans had not been formally written up, action in relation to several of the ideas discussed had been pursued (Box 9). The team leader recounted using the staff meeting, the usual forum in which to discuss improvements in practice, to generate discussion about encouraging movement. Team members talked in detail about how the work of the AO was offering new leisure and social activities for residents. As the implementation team had not met, it was less clear whether it viewed the work of the AO as one vehicle through which MoveMore was being pursued or as the expression of it. Nevertheless, it was also evident that organisational difficulties in the home – imminence of the CQC inspection, demands on the lead and team leader to take on management tasks in absence of the manager – were a constraint on time. The artist captured the discussion on action plans and action for development as a poster. This was subsequently displayed in prominent communal areas, giving rise to speculation among residents as to who was who on the poster!
Muriel (a resident) comes up to me and says: ’I work here and don’t expect to be paid for it’. She talks about her ‘work’ as personnel manager whereby she ‘helps [the deputy manager] with the filing and keeping things tidy’.
The care worker explains later that it was very difficult to get Muriel out of bed in the morning; involving her in the office, reprising her working role in personnel, had encouraged her to get up. She had been ‘interviewed’ for the job by the deputy manager and given a start date.
Fieldnote 1145
From fieldwork, conversations and interviews with members of the implementation team and AO over the last 3 months of the study, individual members had sought to pursue specific initiatives on movement in the prolonged absence of the team lead on account of illness. Issues arising from the CQC inspection assessment (‘requires improvement’ – relating to documentation of processes and procedures, and providing more detailed care plans) diverted the attention of senior staff in responding to them (in contrast to CH4, where the solution to the same problem was to mobilise MoveMore to address it).
Pursuing change systematically did not occur, or did so in fits and starts only. Aspects of implementation, observation and reflection on what needed to change and the steps necessary to make it happen were perceived as valuable. Although the concept of action-planning was understood (unlike in the ‘failed implementer’ site; see ‘Failed’ implementer), pursuit lacked momentum. In the absence of a clear steer, beliefs about the worth of the intervention were not translated into consistent action to make it happen. Alignment and integration of movement in context of the routine work of care and the provision of social and leisure activities was still a work in progress, as care staff and the AO negotiated mutually supportive working relationships that acknowledged each other’s perspective.
Conversations and interviews with the MoveMore lead and team members, including the AO, at the conclusion of the study reported that change had occurred as a consequence of their engagement in MoveMore. They also expressed regret that they ‘had not [had] more time to spend with it and to become more organised around it’, but felt constrained by internal and external factors affecting the home. It came at the ‘wrong’ time: it was ‘untimely’. Nevertheless, they expressed interest in taking the work forward in the future.
‘Partial implementer’: between installation and adoption
Engagement in MoveMore
Care home 3 was a ‘partial implementer’ and, similar to CH1, the process of installing MoveMore extended in time. The CH manager was enthusiastic about taking part in the research: on many occasions during baseline and pre randomisation, the manager asked that the researcher ‘put in a good word’ so that the home would be selected for the intervention, despite explanations about the nature of randomisation. As considered in Person-centred care, the pattern of ‘UC’ in this home presented some challenges.
The first workshop was organised to take place within 3 weeks of the introductory meeting with the CH manager, using a common script: components of the programme, implementation team driving the change, workshops, manual and supporting resources. The workshop was cancelled on the day: the manager was on compassionate leave and, although the deputy indicated that it would go ahead, it became evident to the fieldworker in the home that no work had been done for it. It was also considered unlikely that staff would be released: the home was short-staffed and several senior staff members from the care organisation’s head office were at the home carrying out a review, preparatory to the CQC inspection.
After several attempts, the first workshop was held 8 weeks after the introductory meeting. Participants included the CH manager (identified as the MoveMore lead), receptionist, a senior carer (team leader), carer and both part-time AOs (between them they covered one full-time post; one of them also worked as a bank carer). Discussion about current practice and challenges experienced was slow to get going and staff were hesitant about taking part. One of the care staff and AOs presented the challenges in terms of residents becoming very quickly institutionalised, expecting that staff would care for them, focusing the discussion on work that should be undertaken at the point of admission. The manager acknowledged the challenges, but considered that improvements were possible. Presentation of MoveMore and the use of observation as a tool to see things differently was picked up by a team leader and one of the AOs; there was, however, no sense of collective engagement around a common purpose and there was the absence of a driver to move it forward. A date for the second workshop was set and agreed with the manager for 3 weeks after the first.
A week before the second workshop, the manager commented to the PE researcher who was observing in the home: ‘We have another training session, do you know why?’. The significance of the question was revealed at the workshop. Of the seven participants, none had attended the first workshop. With the exception of a nurse, all were care workers. Their expectation was that they had come to a training event on how to increase residents’ movement. The facilitators agreed to proceed with the programme with the content of the first workshop.
Care staff conveyed the physical demands of the work: most residents were very dependent and needed hoisting to move between wheelchair and chair. Further probing suggested that ‘need’ was more ambiguous: some residents could transfer from wheelchair to armchair on some days and not on other days; others required the assistance of two carers to transfer and they were required to use the hoist; for yet others, lack of time meant that it was quicker and easier to use the hoist. With a complement of four care staff, a ‘floater’ on the morning shift and four in the afternoon, a team leader and a nurse, tasks relating to the ‘bodywork’ of care166 were seen to dominate. Although highlighting how organisational and cultural factors might be implicated in work practices, care staff were unconvinced that the programme could work in their home. Neither could they conceive of having the time or space to observe practice. The nurse present disagreed: it was possible for care and nursing staff to carve out time to conduct observations and take part in the intervention.
Installation: one step forward, two steps back
As the 3-month data collection began, a research facilitator organised a meeting with senior staff in the home (the manager and deputy). One observation had been carried out by the team leader after the first workshop, but the manager and deputy were not aware of any further developments nor had they undertaken any work to pursue it. Following negotiation between the team leader, the manager and the deputy, it was agreed that the team leader would take on the work of MoveMore lead and would pursue the programme with support from the research facilitator.
Following a further delay of around 8 weeks, and within weeks of the 6-month data collection point, the second of the three workshops focusing on completed observations and implications for change occurred, involving the team leader and two care workers, together with the research facilitator. Two new observations had been carried out at different time points: one in the early morning, which opened up the possibility of residents doing more for themselves with enabling support, and one in the early evening, which highlighted the paucity of stimulating activities. Although the first appeared more of a ‘fit’ with the objective of MoveMore, it was not pursued: support from the wider team was not considered feasible. Work pressures on care staff had increased as a consequence of the departure of one of the two AOs, and were exacerbated by care staff vacancies. The second observation, over the following months, was developed as an action plan to introduce a stimulating leisure event in the early evening. This was enacted as a musical event and ‘movie night’ during which these care staff were on shift. Regarded as successful in that the events facilitated interaction between some participating residents, the team found it difficult to consider how they could proceed further forward. Passive support from the CH manager had enabled them to pursue one-off initiatives, yet team members considered that the lack of active support from senior managers overall undermined what they sought to do, reinforcing the already tense relationships with senior staff.
Initial implementation
The team had proceeded through the stage of installation and initial MoveMore implementation: participation in the workshops, and taking the observation, action-planning and review process back into their work environment. However, the limited temporal and spatial spheres of engagement (action relating to one-off events and within their own work arena only) and lack of focus on movement per se, suggests that full adoption had not occurred.
Interviews with senior staff at the conclusion of the study revealed a mixed picture, both in their assessment of the outcome of the intervention and their expectations of it. The CH manager considered that the intervention had made a positive difference in encouraging residents to move, with the team leader actively encouraging staff to work in a more enabling way with residents. The expectation was that this would have been translated into training for the wider group of staff. The deputy manager was more critical: senior staff had provided these workers with the time and space to participate in the MoveMore implementation, but they had not shared their experience with the wider team:
I want everybody to get involved, but because they [implementation team] are the only ones [it was explained to], they didn’t manage to share with them . . . everybody needs to have knowledge about what they’re doing so that when they’re not there, I can instruct [staff] . . . ‘can you do your REACH training?’ . . . my hopes were that you will help us to find the solution to those residents who’s unable to move properly because . . . the programme is about mobility.
Deputy Manager, CH3
The departure of the team leader signified a natural end to MoveMore. Service change was moving in a different direction with the introduction of external entertainers and exercise classes.
‘Failed’ implementer
We characterised CH2 as a ‘failed’ implementer. Similar to the two ‘partial implementer’ homes, the process of installation proceeded in fits and starts over a lengthy period of time, but came to an abrupt stop at action-planning. Although three workshops were provided, the implementation cycle was not completed.
Engagement in MoveMore
This was the first home in which the introductory one-to-one meeting occurred post randomisation, based on the experience with the first intervention home (CH1). Nevertheless, there was a delay in starting. Between the introductory meeting with the CH manager (MoveMore lead) and the first workshop, there was a gap of 6 weeks. The first planned workshop was intended to occur jointly with CH1 (both were in the same locality). Participation of CH2 was cancelled on the day by the manager, citing staffing difficulties, and a further date was negotiated. There were no further joint initiatives between these homes during the study and no other homes expressed interest in working together.
Five staff took part in the first workshop: manager/owner, one of two deputy managers and three care staff, of whom two had worked in the home for several years and one was new to the post. In terms of seniority and experience, the team spanned ‘top-down’ and ‘bottom-up’ participation. As well as the two facilitators, the research team also included the physiotherapist.
First steps in installation
Initial presentation of the programme generated some scepticism: care staff suggested that they were already doing as much as they could to facilitate resident PA. The manager interjected that he had specifically involved them in the implementation team because they understood the value of movement, but that this was not necessarily shared by the wider staff group. This opened up discussion of the challenges of enhancing movement perceived to be located at two levels: the reluctance of residents to move and the limitations of time on carers. Encouraging residents to move more required time, which was difficult to envisage within the constraints of the tasks required of them.
Discussion of the concept underpinning MoveMore, the discomfort people of any age experience from prolonged inactivity and the possibility of small changes making a difference, generated multiple ideas as to what could be done differently; they appeared open to trying out observation as a means of establishing goals for change. There were concerns expressed by one of the carers that other care staff might perceive the ‘observer’ as shirking and ‘not pulling their weight’. How the MoveMore programme was conveyed to the staff team by senior staff was seen as critical.
Fieldwork conducted following the workshop established that 10 observations had been carried out and written up by care staff in the implementation team within a little over 3 weeks following the workshop. This meant that the first stage of programme installation coincided with the start of the 3-month data collection. There were difficulties in securing a firm date from the implementation lead, in part because of the preparatory work required for an imminent CQC inspection and the demands of REACH data collection within the home. The second workshop finally took place nearly 9 weeks after the first, several weeks after the CQC inspection (although prior to the published report), and involved the artist.
There was continuity of participation of members of the implementation team. Those who had conducted observations considered the process useful: as care workers, their focus was on completing the task in hand. Tacit knowledge (‘what I’ve always done because it works’) based on experience shaped practice, but opportunities to stand back and reflect on what was happening through the prism of ‘movement’ provided a different perspective. It was evident, however, that the team had not shared their observations with each other, and shifting from the content of what they had ‘seen’ to what it might pose for working differently was more difficult for some participants. Others, as experienced in the ‘full implementer’ homes, were more skilled at thinking about options for movement flowing from observations. Overall, the discussion, moving between what was observed and action to effect movement, resulted in agreement on a division of labour on who would pursue what: ideas relating to individual residents were to be developed by care staff, and those about home-level action were to be pursued by the team lead. It was noted by the team lead that their recent appointment of an AO (during the 3-month data collection period) to work weekday mornings would enable carers to be less pressured in getting through their morning regenerative work (getting residents up, dressed, toileted, breakfasted and settled), a particularly busy time. The artist captured the discussion in sketches for development as a poster, which was picked up with enthusiasm by participants. A time frame for the third workshop was agreed to enable action on plans to be tried out and for progress to be reviewed.
Process evaluation, observation and conversations in the home following on from the workshop suggested that the implementation team was planning to meet ‘to get our thinking together about what to do next’. Concurrently, the new AO was pursuing quizzes and board games, particularly in the middle lounge, building on and supporting interaction between residents. Her focus was getting to know residents a little and acquiring knowledge of their interests and preferences. Residents in the top lounge remained largely seated and dozing, occasionally taking note when something happened, for example the ‘home’ dog running about. Music featured strongly in routine and organised events: different types of music shaped the atmosphere in different spaces. A monthly ‘Music for Health’ event was popular as a source of stimulation, interaction and movement.
When the third workshop took place as planned, team members seemed unprepared. The impression was that the salience of MoveMore in context of their day-to-day work had been lost. Members of the care team had got together only briefly prior to the workshop and concluded that they lacked understanding as to how to develop action plans, nor did they recollect their completed observations. The research facilitators drew on the images produced by the artist as an aide memoire and revisited the action-planning and review process with concrete examples. A further workshop to review progress was offered, accepted and then not pursued by the implementation lead. No further work on MoveMore occurred; the poster developed from the artist’s images was not displayed in the home.
MoveMore ‘washes out’143 prior to initial implementation
Although a conjuncture of external and internal factors contributed to implementation failure, deeper issues relating to leadership and the coherence of the intervention as worthwhile to invest in were implicated. These included temporal features of the organisational context and the coherence of MoveMore to staff as a means of effecting change.
Temporal features of organisational context
A series of events that began around the 6-month data collection point presaged organisational, social and interpersonal difficulties for the home and its staff over several months. The report of the CQC inspection with an overall assessment of ‘requires improvement’ was felt keenly by the manager and staff, as they prided themselves on the quality of care they delivered. The findings were widely publicised in the local newspapers and were subject of talk outside, as well as within, the home. That the care delivered was deemed ‘good’ was ‘heard’ by care staff, but did not assuage their felt distress. For the manager, breaches of regulations relating to the systems and procedures in place for collecting, recording and reporting accurate information pertinent to, for example, safety, safeguarding, and staff appraisal and supervision imposed an immediate and considerable burden of work. This coincided with an expansion of the business into day-care provision in the home and a personal bereavement – a close relative who was also a resident in the CH.
Fieldnotes over several months conveyed a picture of some disarray over and above what was usual. There were observable indicators of lack of attention, notable for how they departed from what was ‘typical’:
I notice that the menu board on the entrance to the dining room has Tuesday’s menu written on it (it is now Thursday) and the activity boards in the top lounge still read July/August (in October) . . . there is a stale smell of urine and faeces in the room, stronger than what I have previously experienced.
CH2, fieldnote 0950
Staff appeared under considerable strain, reflected in short, abrupt exchanges with each other, based on PE researcher fieldnotes, conversations and interviews. Many new residents were also observed typically seated in the first lounge, which was dominated by those with a cognitive impairment. This had resulted in the displacement of residents usually seated in this area to the other two lounges, which also filled up. The environment seemed cramped and less easily navigable, as the following fieldnote extract illustrates:
Eddie is seated by the entrance to the middle lounge with his walking frame directly in front of him . . . Peter moves slowly out of the lounge holding on to his rollator. The care worker, Marie, is with him. As he comes towards where Eddie is seated, Marie takes his walking frame from in front of him to allow Peter to pass, then immediately puts it back in front of him as before . . . Later, Vanessa (a new carer) comes through from the bottom lounge pushing an empty folded wheelchair. She moves Eddie’s frame to the opposite side of the entrance from where Eddie is seated to make room for her to get through, and moves on. Eddie, who had been dozing, looks around with a puzzled look, then directs his eyes to the frame out of his reach.
CH2, fieldnote 1130
The multiple, interactive contextual factors that were operating in this home resulted in a temporal confluence of disruptive events, which affected care processes and care delivery. Nevertheless, even in the absence of such factors, it appeared that what was decisive in the ‘failure to implement’ was that the objectives of change lacked coherence for the identified ‘driver’, whose position and authority was critical to change happening.
Coherence of MoveMore
Interviews with workshop participants throw further light on the ‘failure’ of implementation. The manager, at the conclusion of the trial, conveyed an expectation of the intervention that was at odds with our conception of it. Each component in itself was seen as being of value, but as carried out by researchers rather than CH staff. Thus, although observation was regarded as a way of seeing things differently, the expectation was that researchers’ observations would provide fresh eyes and lead to suggestions as to what homes could do better. Researchers were seen to have the advantage that ‘seeing’ multiple homes would better identify and communicate good practice, which, in turn, would facilitate sharing and take-up. Change resulting from ‘good practice’ ideas could be measured through analysis of homes’ existing documentation: handover notes and care plans. In addition, it was argued that ‘as you’ve got to have enough staff to mobilise people . . . because you’ve got to have enough time . . . the issue of funding has to be raised’.
Individual care staff in the team held mixed views about the value of the programme in their setting. Theresa argued that ‘. . . we came up with lots of ideas . . . when we were a group [in the workshops] but because we stopped at the next bit, we didn’t put other things into place that we maybe could’ve’. Andrea was less convinced that pursuing the programme would have made a difference: they were doing what they could. She noted that the home had a group in for 1 hour per month doing exercises and games, and that ‘maybe it should be a bit more regular . . . and the ones that can’t walk can move their arms and their legs a bit’. Both agreed that they lacked the legitimacy and power to take the work forward in the absence of positive engagement from the manager.
Following on from the trial, there was investment in external providers to enhance movement (a monthly exercise group) and expand leisure activities (musicians). With a further CQC inspection assessing the home as ‘good’ in all dimensions and ‘outstanding’ in caring, the home reappraised its designation as a successful home.
Discussion and conclusions
MoveMore was distinct from UC in its conception of ‘movement’, and contrasted with the common understanding of PA as time limited and medium- to long-interval exercise classes. It was also distinctive in its goal of encouraging and supporting movement for all residents, regardless of their needs, in their routines of daily life. At the same time, there existed considerable variability between homes in the range, frequency and type of social and leisure activities available; the resources accessed by staff; and their deployment across their resident profile. Even when homes provided a wide array of leisure activities, movement was not necessarily at the forefront of thinking in relation to them; similarly, the inclusion of residents of all needs was not often considered in the activities that were provided. Homes also varied in their adoption of an enabling approach to care, a key component of ‘movement’ in MoveMore.
The theory of change that underpinned MoveMore was broadly supported in its key ‘active’ ingredients. Observation by staff to ‘see’ practice through the lens of movement was a powerful factor in developing an understanding of MoveMore as a set of practices with potential benefits over and above UC. Nevertheless, what distinguished ‘full implementers’ from others was that observations and reflections were discussed informally between individuals and within groups to create a shared understanding of what needed to change, and to generate ideas about goals, priorities and creative solutions from different perspectives to make change happen. The workshops provided an important forum for this to occur; the work of the artist in capturing and communicating ideas for change to take into the home environment was another. Both facilitated interchange, but were not substitutes for the communication and negotiation work that needed to occur within the homes. In NPT terms, sense-making (coherence) and mobilising participants to work at taking change forward (cognitive participation) required time and space to forge a shared understanding of what new practices might look like. Allied with and contributing to this was the existence of a strong ‘steer’ to guide the work of change and to take responsibility for making things happen, whether this existed from the outset (CH5) or emerged over the implementation process (CH4). Each of these mechanisms operated interactively and cumulatively.
The ‘full implementer’ homes embraced the complexities of change, including pursuing negotiations with residents and with the wider group of staff to work around new sets of practices (and relationships) (collective action at multiple levels). Mechanisms to engage these ‘significant others’, including communication strategies, were essential to securing the ‘reach’ of the programme beyond the implementation team. Indeed the ‘depth’ (action in multiple domains and in relation to residents with different needs) and ‘reach’ of the intervention was necessary to move to full adoption. The work of generating collective action then, for this intervention in this setting, although initiated within the implementation team, had to move beyond it.
The ‘full implementer’ homes had, within the period of the trial, moved a little beyond the stage of ‘full adoption.’ They had begun to harness the change process in ways that were feasible for them to embed aspects of change into their existing systems and procedures. This had the potential to sustain movement in routine practice. Indeed, some practices in both full implementer homes had become routinised.
The two ‘partial implementer’ homes, we suggest, were very different in their potential to pursue the intervention to full adoption. Among senior staff in CH1, who also comprised members of the MoveMore implementation team, there was an understanding of MoveMore as an intervention to increase movement in CH routines and that there was value in the work involved to effect practice change (observation and action-planning). They also had legitimacy to secure engagement of the CH in the endeavour, given their seniority, experience and the respect accorded to them by staff in different relationships to them. MoveMore made sense as an intervention to pursue (coherence) and what it asked of them (cognitive participation). The concept of action-planning was understood and partially enacted, albeit in fits and starts, and embraced multiple areas for action in respect of care routines and practices pertinent to movement. Providing a consistent and sustained steer was more problematic, as was translating rich discussion of ideas for action to increase movement in the workshops into action plans that established a clear direction of action for change. In part, this reflected contextual factors in the home that inhibited or delayed implementation. But it also reflected how contextual factors operated to limit opportunities for time and headspace to develop and pursue the work of action. As a consequence of multiple, concurrent contextual factors operating within and on the home, the implementation team lead was unable to enact the work of steering the programme, and the absence of senior staff for prolonged periods meant that other team members also assumed different roles and relationships in the home that negatively affected their capacity to pick up the steer. A strategy to engage the newly appointed AO in the work of steering the programme and to integrate movement in social and leisure activities was only partially successful: the post-holder was also in the process of developing the role and building relationships with care staff in relation to it. Here, the absence of a key participant to drive the programme forward was seen as reflecting a particular conjuncture or confluence of circumstances and posed the question of the ‘timeliness’ of the intervention.
Care home 3 similarly lacked a steer with the legitimacy to pursue change at the CH level. Although responsibility was delegated to a number of care workers who were interested in taking it forward, in practice they did not have the legitimacy to enact it. The changes pursued were in their own temporal and spatial spheres, providing stimulation to residents during their evening shift, which, in the context of this CH, involved considerable work for them to pursue: it was not ‘usual’ care work. They were unable to engage colleagues in the work and there were conflicting expectations on them among senior staff, reflecting a lack of coherence about the MoveMore intervention; the effort and work petered out. The impasse reinforced the significance of senior staff’s active engagement in the implementation process to legitimise change with the wider staff team, but also the importance of action plans and mobilising action to extend the reach of the intervention beyond the implementation team.
From the literature, considered previously, there is consensus that context matters in implementing complex interventions. A significant factor in all of the homes was the CQC inspection: for all study homes, this was the first inspection under new criteria, intended to be more searching and in-depth than previously, and generated both considerable preparatory work and uncertainty. Three of the five intervention homes were appraised as ‘requiring improvement’ following the inspection, primarily related to systems for detailed and accurate recording of information pertinent to care plans, medication management and safeguarding; care in all cases was described as ‘good’. Nevertheless, although subject to the same external contextual factor, the response of the home and its interface with the intervention differed. In CH4, the ‘problem’ of inadequately detailed care plans was a spur to mobilising the MoveMore intervention as part of resolving it; in CH1, it was a factor in disrupting work in relation to the intervention. This reinforces the conception of the inter-relationships between characteristics of context and participants,143,155 in which interventions are conceived of as ‘events in systems that either leave a lasting footprint or wash out depending on how well the dynamic properties of the system are harnessed’. 143
There were aspects of the intervention and implementation process that could have been done better. The requirements of documentation were considered overly onerous for most participants in this setting. Simplification of the tools and alternative methods for documenting them (e.g. audio-recording) need consideration and testing for a full trial.
Three specific features of the implementation process need further elaboration. First, although the interactive and participatory approach to installing the intervention was successful in securing ‘buy-in’, more explicit guidelines are required about the time frame within which this should occur in negotiating participation with CHs. Second, the active role of the implementation team as a vehicle for creating a shared understanding about and goals for action needs to be made more explicit, as has the work of communicating the change process beyond the team to effect full adoption. Third, the sequencing of the ‘external’ experts in the workshops was important for optimal impact: the physiotherapist in conveying movement as part of daily routines in the introductory workshop and the artist in translating observation into action plans.
In conclusion, the PE findings contribute to the understanding of how the intervention works in the context of CHs and, therefore, the factors that facilitate successful uptake. It also identifies aspects of the implementation process that require further work to finesse.
Appendix 10 Health economic report
Background
The economic evaluation was conducted in two parts: a within-trial economic evaluation was conducted to evaluate the costs and benefits associated with the MoveMore intervention that occurred during the trial, and an economic model was developed to analyse future costs and benefits beyond the trial time horizon. The analysis was guided by the recommendations of the National Institute for Health and Care Excellence (NICE) methods guide. 167
Within-trial analysis
An economic evaluation was conducted alongside the REACH feasibility trial to produce preliminary estimates of the cost-effectiveness of the MoveMore intervention to increase PA in the daily lives of CH residents.
Methods
Aims and end points
The primary aim of this analysis was to produce preliminary estimates of the cost-effectiveness of the MoveMore intervention to inform future research. The primary end point was the cost per quality-adjusted life-year (QALY)168 gained from the REACH intervention, compared with UC, at 9 months post randomisation.
Perspective and time frame
The study adopted a health-care and Personal Social Services provider perspective. Direct costs and outcomes of residents in CHs randomised to the MoveMore intervention were compared with those in CHs randomised to UC over the 9-month time horizon of the trial. As the time frame of the trial was < 1 year, discounting of the costs and benefits was not required.
Measurement of outcomes
Health-state utility values were obtained from resident responses to the EQ-5D-5L questionnaire,169 which was administered at baseline and at 3, 6 and 9 months post randomisation. Resident responses were converted to utility values using the standard UK general population tariff values. 170 The utility values represent residents’ quality of life and were multiplied by the duration (t) in each health state to generate QALYs, which were used as the main outcome measure for this analysis, using an area under the curve approach:
where EQ-5DBaseline, EQ-5D3, EQ-5D6 and EQ-5D9 are the EQ-5D-5L scores at baseline, 3 months, 6 months and 9 months, respectively. If an individual died during the trial, we assumed that their utility value was zero from the date of death to trial end and assumed a linear transition to this value from their last completed EQ-5D-5L.
Health-state utility values were also obtained from proxy responses to the EQ-5D-5L. In the base-case analysis, proxy responses to the EQ-5D-5L were used when self-reported responses were missing.
Total QALYs were calculated for each resident over the 9 months and summary statistics were generated by treatment group. Multivariate regression was used to analyse the difference in QALYs between treatment groups, controlling for baseline quality of life, age, sex and length of stay at the CH.
Measurement of resource use
All health-care resource use was estimated from the perspective of the health-care and Personal Social Services provider, and was collected for the trial period of 9 months from randomisation using resident-completed questionnaires and hospital records. This included primary care, such as GP visits and nurse home visits, as well as secondary care, such as outpatient visits and other hospital admissions.
Cost analysis
All use of health-care services that occurred during the trial period were converted to costs using appropriate UK unit costs estimated for the price year 2016. Unit costs were assigned to health-care resource use from the Personal Social Services Research Unit’s Unit Costs of Health and Social Care 2016,171 NHS reference costs172 and hourly pay rates. 173 Residents’ use of health-care resources and total costs were calculated for the ITT population.
A cost associated with the workshops provided to the CHs in the MoveMore arm was estimated as the sum of the cost of attendee time, the cost of the time of the workshop leads and the cost of a training folder/intervention pack that was given to each CH. Costs associated with trainer and attendee time were calculated using a human capital approach in which hourly wage rates of trainers and attendees were multiplied by the workshop duration and summed. Each CH also received an intervention folder, the cost of which (£47.15) was added to the cost associated with trainer and attendee time to attend workshops to estimate the total intervention cost for each CH. This was then divided by the average number of permanent residents in CHs in the MoveMore arm of the trial to obtain an intervention cost per resident. The intervention delivery was assumed to be subsumed within current practice; therefore, no additional costs were included for delivery of the intervention.
Total costs for each resident were calculated as the sum of costs assigned for hospital, community health and social services, and the intervention cost. Multivariate regression was used to analyse the difference in costs between treatment groups, controlling for age, sex and length of stay at the CH.
Adjusting for baseline imbalance
As a resident’s baseline utility is likely to be correlated with their utility over the follow-up period, any imbalance in baseline utilities must be accounted for when calculating differential effects between treatment groups. 174,175 Multiple regression analysis was used to estimate differential mean QALYs and to predict adjusted QALYs, controlling for utility at baseline.
Missing data
Based on descriptive analysis of the missing data, the analysis was conducted under the assumption that the missing data were missing at random. 176 Consequently, when there were missing quality-of-life or cost follow-up data, multiple imputation methods were used to generate estimates of missing values based on the distribution of observed data, as per recommended best practices for economic evaluation alongside clinical trials. 177
When choosing the level at which to impute missing data (more or less aggregated), a balance needs to be struck between maintaining the data structure and achieving a stable imputation model. 176 Consequently, for quality-of-life data, missing EQ-5D-5L index values were imputed at each follow-up. For costs, missing data were imputed for each follow-up at the level of total health and social services costs and total hospital costs, not at the unit of resource level. Missing baseline EQ-5D-5L values were imputed using mean imputation to ensure that imputed values were independent of treatment allocation. 178 EQ-5D-5L index values were recorded as missing if any EQ-5D-5L items were missing in both the self-reported and proxy EQ-5D-5L questionnaires for a given time point. Costs were counted as missing if all resource items on the case report form were missing.
The imputation was performed in Stata® version 15 (StataCorp LP, College Station, TX, USA) using predictive mean matching to perform multiple imputation by chained equations. Predictive mean matching ensures that only plausible values of the missing variable are imputed, as the imputed value is drawn from another individual whose predicted value is close to the predicted value of the individual with the missing observation. 176
Cost-effectiveness analysis
Primary analysis
The cost-effectiveness analysis adopted an ITT perspective for analysing and summarising the health economic trial data. The primary analysis consisted of a cost–utility analysis over the 9-month trial period and included adjustment for baseline variables and imputation of missing data. The incremental cost per QALY gained as a result of the MoveMore intervention, compared with UC, was calculated, producing an incremental cost-effectiveness ratio (ICER)179 as follows:
The ICER was calculated using the two-stage method, as recommended for cluster randomised trials with < 20 clusters. 94 Therefore, resident-level costs and QALYs were used to estimate average costs and QALYs for each CH, and CH-level average costs and QALYs were used in the ICER calculation (Equation 5).
NICE considers a cost per QALY within the range of £20,000–30,000 to be acceptable. 167 Therefore, the lower limit of this threshold (£20,000) was used to determine cost-effectiveness.
Sensitivity analyses
The robustness of the main trial analysis results was tested in a number of sensitivity analyses. ICERs from each of the sensitivity analyses were compared with the main trial results to identify areas of uncertainty.
The effect of adjusting for baseline imbalance on cost-effectiveness was explored in an analysis with no adjustment for baseline differences between groups. In addition, the effect of not imputing missing data was considered in an analysis including complete cases only.
The base-case analysis used combined EQ-5D-5L scores: self-reported EQ-5D-5L responses were used if available, and proxy-reported EQ-5D-5L responses were used when self-reported values were missing. However, it is noted in the literature that there may be differences between EQ-5D-5L scores obtained directly from residents and those obtained from a proxy. 180–186 We therefore explored the effect of this in sensitivity analyses using self-reported EQ-5D-5L scores alone and proxy-reported EQ-5D-5L scores alone. In each case, we present ICERs for the ITT sample (including imputed data) and for the complete-case sample.
In November 2018, NICE released a position statement (updated in October 2019) with regard to the use of the EQ-5D-5L in reference case analyses and recommended using a mapping function to map EQ-5D-5L responses to the EuroQol-5 Dimensions, three-level version (EQ-5D-3L), value set. 187 Consequently, we conducted an additional sensitivity analysis using EQ-5D-3L values obtained from the van Hout et al. 188 crosswalk.
It was identified in the PE that the CHs in the MoveMore arm of the trial implemented the intervention to differing degrees; in particular, one CH was classed as a ‘failed implementer’. To explore the impact of this CH’s failed implementation, an additional sensitivity analysis was run that excluded the residents in this CH.
Uncertainty analysis
The level of sampling uncertainty around the ICER was determined using a non-parametric bootstrap to generate 1000 estimates of incremental costs and benefits. The bootstrapped estimates were plotted on the cost-effectiveness plane to illustrate the uncertainty surrounding the cost-effectiveness estimates. 189 A cost-effectiveness acceptability curve illustrating the probability that the REACH intervention is cost-effective at a range of threshold values (£0–100,000) was also constructed using the bootstrapped samples. 190
Results
Sample
Of the 153 residents recruited to the trial, 126 residents had complete resource use and EQ-5D-5L results for all follow-ups.
Resource use and costs
Table 67 shows the average resource use of participants in each trial arm over the 9 months of the trial.
| Item | Mean (SD); participants with data available (n) | |||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 9 months | |||||
| UC | MoveMore | UC | MoveMore | UC | MoveMore | UC | MoveMore | |
| Hospital services | ||||||||
| A&E visits | 0.167 (0.404); 90 | 0.082 (0.277); 61 | 0.072 (0.261); 69 | 0.02 (0.141); 50 | 0.118 (0.325); 76 | 0.14 (0.351); 50 | 0.143 (0.391); 70 | 0.073 (0.264); 41 |
| Hospital admissions | 0.101 (0.371); 89 | 0.082 (0.331); 61 | 0.129 (0.378); 70 | 0.08 (0.274); 50 | 0.092 (0.291); 76 | 0.12 (0.328); 50 | 0.129 (0.378); 70 | 0.024 (0.156); 41 |
| Community health and social services | ||||||||
| Routine GP consultations | 1.233 (2.399); 86 | 1.304 (1.736); 56 | 0.071 (0.31); 70 | 1.1 (1.389); 50 | 0.618 (0.979); 76 | 1.367 (2.079); 49 | 0.522 (1.066); 69 | 0.659 (0.656); 41 |
| Unplanned GP consultations | 0.337 (0.954); 83 | 0.222 (0.42); 45 | 1.696 (7.232); 69 | 1.179 (1.412); 39 | 0.368 (1.221); 68 | 0.182 (0.446); 44 | 1.074 (2.482); 68 | 0.775 (1.577); 40 |
| Nurse visits | 2.211 (6.403); 90 | 1.429 (2.802); 56 | 2.929 (10.511); 70 | 4.333 (13.521); 51 | 2.9 (6.099); 70 | 1.021 (2.188); 48 | 3.063 (6.066); 63 | 2.395 (6.808); 38 |
| Physiotherapist visits | 0.132 (0.521); 91 | 0.129 (0.461); 62 | 0 (0); 70 | 0.196 (0.53); 51 | 0.139 (0.539); 72 | 0.1 (0.303); 50 | 0.188 (0.55); 69 | 0.119 (0.328); 42 |
| Occupational therapist visits | 0.011 (0.105); 91 | 0.016 (0.127); 62 | 0 (0); 70 | 0 (0); 49 | 0.12 (0.716); 75 | 0.04 (0.198); 50 | 0.174 (0.822); 69 | 0.071 (0.342); 42 |
| Community matron visits | 0.187 (0.515); 91 | 0.226 (0.422); 62 | 0.261 (0.634); 69 | 0.235 (0.428); 51 | 0.093 (0.408); 75 | 0.32 (0.844); 50 | 0.188 (0.522); 69 | 0.19 (0.397); 42 |
Average health-care costs over the trial period are presented in Table 68.
| Total costs (£) | UC | MoveMore | ||||
|---|---|---|---|---|---|---|
| Mean (SD); participants (n) | Minimum | Maximum | Mean (SD); participants (n) | Minimum | Maximum | |
| Hospital services | 509.13 (1509.01); 81 | 0 | 8791.63 | 546.73 (1985.61); 52 | 0 | 13,280.56 |
| Community health and social services | 631.41 (1123.29); 81 | 0 | 8417.6 | 603.01 (705.17); 52 | 0 | 3689.52 |
| Intervention cost | 0 (0); 81 | 0 | 0 | 26.23 (4.75); 52 | 18.71 | 31.48 |
| Total NHS cost | 1140.54 (1941.78); 81 | 0 | 9861.03 | 1175.97 (2173.01); 52 | 50.71 | 13,732.46 |
The mean total cost associated with the use of community health and social services was £631.41 (SD £1123.29) for the UC group and £603.01 (SD £705.17) for the MoveMore group. The mean total cost associated with the use of hospital services was £509.13 (SD £1509.01) for the UC group and £546.73 (SD £1985.61) for the MoveMore group. Multiple regression analysis indicated that there was no significant difference in the total costs between groups (p > 0.05). Table 69 presents all unit costs used in the analysis.
| Resource item | Unit cost (£) | Source | Details (including currency/service codes) |
|---|---|---|---|
| Community health and social services | |||
| GP visit, routine (assume surgery visit) | 36.00 | PSSRU 2016171 p. 145 | GP, per patient contact lasting 9.22 minutes, including direct care staff costs |
| GP visit, unplanned (assume home visit) | 82.76 | PSSRU 2016171 p. 145 | (Per patient contact lasting 9.22 minutes + average 12-minute travel time) × £3.90 per minute |
| District nurse visit | 38.00 | NHS Reference Costs 2015 to 2016 172 | District nurse, adult, face to face. Currency code: N02AF; SC: NURS |
| Physiotherapy | 32.00 | PSSRU 2016171 pp. 135–7 | Physiotherapist, band 5, face to face, 1 hour |
| Occupational therapist | 32.00 | PSSRU 2016171 pp. 135–7 | Occupational therapist, band 5, face to face, 1 hour |
| Community matron | 61.00 | PSSRU 2016171 pp. 186 and 142 | Hospital matron defined as grade 8a (PSSRU 2016171 p. 186). Assume community matron also grade 8a. Face to face, 1 hour |
| Chiropodist/podiatrist | 32.00 | PSSRU 2016171 pp. 135–7 | Chiropodist/podiatrist, band 5, face to face, 1 hour |
| Mental health nurse | 36.00 | PSSRU 2016171 p. 142 | Mental health nurse, band 5, per working hour |
| Memory nurse | 44.00 | PSSRU 2016171 pp. 31 and 142 | Memory nurse, band 6, per working hour |
| Diabetic nurse | 52.00 | PSSRU 2016171 p. 142 | Diabetes specialist nurse, band 7, per working hour |
| Heart failure nurse | 44.00 | PSSRU 2016171 p. 142 | Nurse specialist, band 6, per working hour |
| Warfarin nurse | 44.00 | PSSRU 2016171 p. 142 | Nurse specialist, band 6, per working hour |
| Dietitian | 42.00 | PSSRU 2016171 pp. 136–7 | Scientific and professional staff, band 6, per working hour |
| Dentist (assumed band 1) | 51.75 | PSSRU 2016171 p. 181 | Dentist, 15 minutes at £207 per patient-hour |
| Psychiatrist | 74.00 | PSSRU 2016171 p. 137 | Psychiatrist, band 8, per working hour |
| Psychologist | 52.00 | PSSRU 2016171 pp.135–7 | Clinical psychologist, band 7, face to face, 1 hour |
| Social worker | 79.00 | PSSRU 2016171 p. 156 | Social worker, per hour of client-related work |
| Speech and language therapist | 32.00 | PSSRU 2016171 pp. 135–7 | Speech and language therapist, band 5, per working hour |
| Phlebotomy | 61.00 | NHS Reference Costs 2015 to 2016172 and PSSRU 2016171 p. 169 | Phlebotomy DAPS08, at £3 + community nurse (1 hour) at £58 |
| Blood test | 15.14 | NHS Reference Costs 2015 to 2016 172 | 15.5-minute consultation with practice nurse (PSSRU 2015191) at £43 per hour plus blood test at £3 |
| (12.14 + 3.00) | Directly accessed pathology services – haematology. Currency code: DAPS05 | ||
| Pharmacist | 7.00 | PSSRU 2016171 pp. 135–7 | Assume 10-minute consultation with pharmacist at £42 per hour |
| Hospital-based or residential care services | |||
| Hospital inpatient | 298.41 per day | NHS Reference Costs 2015 to 2016 172 | Total HRGs, average of all non-elective inpatient excess bed-days |
| A&E | 137.74 per visit | NHS Reference Costs 2015 to 2016 172 | Emergency medicine, average unit costs of all emergency medicine attendances |
| Hospital outpatient (medical outpatient appointment) | 116.00 | NHS Reference Costs 2015 to 2016 172 | Weighted average of all outpatient attendances |
| Audiology | 58.33 | NHS Reference Costs 2015 to 2016 172 | Outpatient audiology, SC: 840 |
| Bone clinic | 706.26 | NHS Reference Costs 2015 to 2016 172 | Non-inflammatory, bone or joint disorders with CC score 0–1, HD24H |
| Cataract surgery | 166.98 | NHS Reference Costs 2015 to 2016 172 | Minor cataract or lens procedures, BZ33Z |
| Dermatology | 101.63 | NHS Reference Costs 2015 to 2016 172 | Dermatology outpatient, SC: 330 |
| Ear, nose and throat | 96.87 | NHS Reference Costs 2015 to 2016 172 | Outpatient; ear, nose and throat; SC: 120 |
| Eye clinic/ophthalmologist/optometry outpatient | 79.19 | NHS Reference Costs 2015 to 2016 172 | Optometry outpatient, SC: 662 |
| Oncology | 151.12 | NHS Reference Costs 2015 to 2016 172 | Medical oncology outpatient, SC: 370 |
| Radiology | 84.52 | NHS Reference Costs 2015 to 2016 172 | Interventional radiology, SC: 811 |
| Ultrasonography – outpatient | 58.59 | NHS Reference Costs 2015 to 2016 172 | Ultrasonography with duration of ≥ 20 minutes, with contract, RD43Z |
| Wheelchair services | 186.77 | NHS Reference Costs 2015 to 2016 172 | Specialist complex wheelchair services, WC13 |
| Radiography | 30.00 | NHS Reference Costs 2015 to 2016 172 | Direct access plain film DAPF |
| CH staff costs | |||
| Care worker | 7.79 | National Minimum Data Set for Social Care173 | Median hourly pay rate |
| Senior care worker | 8.51 | National Minimum Data Set for Social Care173 | Median hourly pay rate |
| Registered nurse | 14.73 | National Minimum Data Set for Social Care173 | Median hourly pay rate |
| Other job roles directly involved in providing care | 8.06 | National Minimum Data Set for Social Care173 | Median hourly pay rate |
| Other job roles not directly involved in providing care | 7.82 | National Minimum Data Set for Social Care173 | Median hourly pay rate |
| Ancillary staff, not care providing | 7.50 | National Minimum Data Set for Social Care173 | Median hourly pay rate |
| Administrative/office staff, not care providing | 9.94 | National Minimum Data Set for Social Care173 | Median hourly pay rate |
| Activities worker or co-ordinator | 8.12 | National Minimum Data Set for Social Care173 | Median hourly pay rate |
| Supervisor | 10.49 | National Minimum Data Set for Social Care173 | Median hourly pay rate |
| Managers and staff, care related but not care providing (deputy manager) | 13.55 | National Minimum Data Set for Social Care173 | Median hourly pay rate |
| Home manager (first line manager) | 14.38 | National Minimum Data Set for Social Care173 | Median hourly pay rate |
| Registered manager | 15.25 | National Minimum Data Set for Social Care173 | Median hourly pay rate |
| Senior management | 16.51 | National Minimum Data Set for Social Care173 | Median hourly pay rate |
| Intervention folder cost | |||
| One ream of paper | 2.56 | Office Depot, University of Leeds, Science Warehousea | Based on £12.83 per five-ream box |
| One lever arch file | 0.94 | Office Depot, University of Leeds, Science Warehousea | |
| Dividers (10 part) | 0.19 | Office Depot, University of Leeds, Science Warehousea | |
| Printing cost | 20.46 | University of Leeds printing charges [URL: https://leeds.service-now.com/it?id=kb_article&sysparm_article=KB0011092 (accessed 20 January 2020)] | Assume 124 pages based on Pre-fit study,192 at 16.5 p per sheet for colour double-sided printing |
| Staff time to put together | 23.00 | PSSRU 2016171 pp. 135–7 | Clinical support worker, cost per working hour. Assume 1 hour based on Pre-fit study192 |
The cost of the intervention is broken down by workshop in Table 70. Not all sites implemented the intervention in the same way (e.g. different durations of workshops, and different numbers and types of attendees), which influenced the overall costs associated with the intervention in different CHs.
| Component | Workshop 1 | Workshop 2 | Workshop 3 | |||
|---|---|---|---|---|---|---|
| Mean (SD) | Minimum, maximum | Mean (SD) | Minimum, maximum | Mean (SD) | Minimum, maximum | |
| Workshop duration (hours) | 1.92 (0.41) | 1.5, 2.5 | 1.7 (0.21) | 0.5, 2 | 1.25 (0.45) | 0.75, 2 |
| Number of attendees | 6.17 (1.47) | 5, 8 | 4.4 (2.19) | 3, 8 | 3.33 (1.51) | 2, 6 |
| Cost of attendee time (£) | 109.13 (28.38) | 87.77, 163.26 | 81.53 (55.56) | 39.11, 175.3 | 44.85 (34.84) | 18.28, 111.78 |
| Number of trainers | 2.5 (0.55) | 2, 3 | 2.2 (0.45) | 2, 3 | 2 (0) | 2, 2 |
| Cost of trainer time (£) | 157.33 (61.28) | 96, 240 | 120 (29.93) | 96, 168 | 80 (28.62) | 48, 128 |
Quality of life
The mean (SD) self-reported and proxy-reported EQ-5D-5L scores for each trial arm at each time point are presented in Table 71. There is little difference in the EQ-5D-5L scores over the trial period in either arm, and multiple regression analysis indicated that there was no significant difference in total QALYs gained between groups (p > 0.05). However, differences were observed between the scores in the self-reported EQ-5D-5L and those in the proxy-reported EQ-5D-5L.
| Time point | UC | MoveMore | ||
|---|---|---|---|---|
| EQ-5D-5L score, mean (SD); participants (n) | Change from baseline, mean (SD); participants (n) | EQ-5D-5L score, mean (SD); participants (n) | Change from baseline, mean (SD); participants (n) | |
| Self-reported EQ-5D-5L score | ||||
| Baseline | 0.8 (0.224); 48 | 0.745 (0.233); 42 | ||
| 3 months | 0.779 (0.231); 30 | 0.005 (0.155); 27 | 0.693 (0.224); 38 | –0.03 (0.194); 36 |
| 6 months | 0.795 (0.245); 36 | –0.014 (0.177); 31 | 0.709 (0.242); 37 | –0.024 (0.284); 35 |
| 9 months | 0.776 (0.267); 33 | –0.02 (0.189); 25 | 0.774 (0.22); 29 | –0.011 (0.178); 27 |
| Proxy-reported EQ-5D-5L score | ||||
| Baseline | 0.685 (0.245); 91 | 0.595 (0.262); 61 | ||
| 3 months | 0.668 (0.256); 70 | –0.021 (0.179); 70 | 0.552 (0.256); 52 | –0.055 (0.221); 52 |
| 6 months | 0.675 (0.264); 70 | –0.026 (0.16); 70 | 0.571 (0.294); 50 | –0.037 (0.205); 50 |
| 9 months | 0.636 (0.303); 64 | –0.071 (0.2); 64 | 0.576 (0.298); 41 | –0.052 (0.232); 41 |
The correlations between the self-reported and the proxy-reported EQ-5D-5L scores are presented in Table 72. This shows that, for each follow-up, the EQ-5D-5L scores obtained by self-report and by proxy are significantly correlated. However, the coefficients (Pearson’s coefficient) indicate that the correlation between the two measures is not perfect.
| Parameter | Correlation between self-reported and proxy EQ-5D-5L | |||
|---|---|---|---|---|
| Baseline | 3 months | 6 months | 9 months | |
| Correlation coefficient | 0.5398 | 0.4726 | 0.4748 | 0.5516 |
| Significance | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| Sample participants (n) | 90 | 68 | 68 | 60 |
Missing data
Complete and missing resource use and EQ-5D-5L data are presented in Tables 73 and 74, respectively. A total of 129 residents completed resource use questionnaires for all follow-ups. A total of 43 residents had complete self-reported EQ-5D-5L scores across all time points, and 98 residents had complete proxy-reported EQ-5D-5L scores across all time points. Initially, completion of resource use and proxy EQ-5D-5L questionnaires was very good, but this started to tail off over the course of the trial. Completion of self-reported EQ-5D-5L questionnaires followed a similar trend, but also started from a low base.
| Item | Baseline | 3 months | 6 months | 9 months | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| UC | MoveMore | UC | MoveMore | UC | MoveMore | UC | MoveMore | |||||||||
| Participants, n valid (n missing) | % complete | Participants, n valid (n missing) | % complete | Participants, n valid (n missing) | % complete | Participants, n valid (n missing) | % complete | Participants, n valid (n missing) | % complete | Participants, n valid (n missing) | % complete | Participants, n valid (n missing) | % complete | Participants, n valid (n missing) | % complete | |
| Hospital services | ||||||||||||||||
| A&E visits | 90 (1) | 99 | 61 (1) | 98 | 69 (22) | 76 | 50 (12) | 81 | 76 (15) | 84 | 50 (12) | 81 | 70 (21) | 77 | 41 (21) | 66 |
| Hospital admissions | 89 (2) | 98 | 61 (1) | 98 | 70 (21) | 77 | 50 (12) | 81 | 76 (15) | 84 | 50 (12) | 81 | 70 (21) | 77 | 41 (21) | 66 |
| Community health and social services | ||||||||||||||||
| Routine GP consultations | 86 (5) | 95 | 56 (6) | 90 | 70 (21) | 77 | 50 (12) | 81 | 76 (15) | 84 | 49 (13) | 79 | 69 (22) | 76 | 41 (21) | 66 |
| Unplanned GP consultations | 83 (8) | 91 | 45 (17) | 73 | 69 (22) | 76 | 39 (23) | 63 | 68 (23) | 75 | 44 (18) | 71 | 68 (23) | 75 | 40 (22) | 65 |
| Nurse visits | 90 (1) | 99 | 56 (6) | 90 | 70 (21) | 77 | 51 (11) | 82 | 70 (21) | 77 | 48 (14) | 77 | 63 (28) | 69 | 38 (24) | 61 |
| Physiotherapist visits | 91 (0) | 100 | 62 (0) | 100 | 70 (21) | 77 | 51 (11) | 82 | 72 (19) | 79 | 50 (12) | 81 | 69 (22) | 76 | 42 (20) | 68 |
| Occupational therapist visits | 91 (0) | 100 | 62 (0) | 100 | 70 (21) | 77 | 49 (13) | 79 | 75 (16) | 82 | 50 (12) | 81 | 69 (22) | 76 | 42 (20) | 68 |
| Community matron visits | 91 (0) | 100 | 62 (0) | 100 | 69 (22) | 76 | 51 (11) | 82 | 75 (16) | 82 | 50 (12) | 81 | 69 (22) | 76 | 42 (20) | 68 |
| Time point | Self-reported EQ-5D-5L | Proxy-reported EQ-5D-5L | ||||||
|---|---|---|---|---|---|---|---|---|
| UC | MoveMore | UC | MoveMore | |||||
| Participants, n valid (n missing) | % complete | Participants, n valid (n missing) | % complete | Participants, n valid (n missing) | % complete | Participants, n valid (n missing) | % complete | |
| Baseline | 48 (43) | 53 | 42 (20) | 68 | 91 (0) | 100 | 61 (1) | 98 |
| 3 months | 30 (61) | 33 | 38 (24) | 61 | 70 (21) | 77 | 52 (10) | 84 |
| 6 months | 36 (55) | 40 | 37 (25) | 60 | 70 (21) | 77 | 50 (12) | 81 |
| 9 months | 33 (58) | 36 | 29 (33) | 47 | 64 (27) | 70 | 41 (21) | 66 |
When using combined self-reported and proxy-reported EQ-5D-5L scores in the base case, 127 residents had complete EQ-5D-5L scores across all time points. There was 1 (< 1%) missing EQ-5D-5L score at baseline, which was imputed independently of treatment allocation. A total of 42 (9%) scores were missing across the remaining follow-ups (months 3–9) and were imputed for the cost-effectiveness analysis.
Cost-effectiveness results
Cost-effectiveness results are presented in Table 75. The UC group had the highest number of QALYs gained over the trial period, but the mean total cost was lowest for the MoveMore group. This suggests that the MoveMore intervention would not be cost-effective, compared with UC.
| Treatment group | Cost (£), mean (SD) | Incremental cost (£) | QALY, mean (SD) | Incremental QALY | ICER (£/QALY) |
|---|---|---|---|---|---|
| UC | 1082.08 (711.51) | 0.446 (0.006) | |||
| MoveMore | 1011.15 (561.42) | –70.93 | 0.436 (0.01) | –0.011 | 6448 |
Bootstrapped estimates of the incremental costs and incremental effects are plotted on the cost-effectiveness plane in Figure 19. This shows the joint distribution of the incremental costs and effects for MoveMore, compared with UC. The majority of points lie above the cost-effectiveness threshold line and to the left of the y-axis, indicating that the MoveMore intervention is unlikely to be a cost-effective use of resources and that more QALYs are gained by participants in the UC group.
FIGURE 19.
The cost-effectiveness plane: the MoveMore intervention vs. UC.
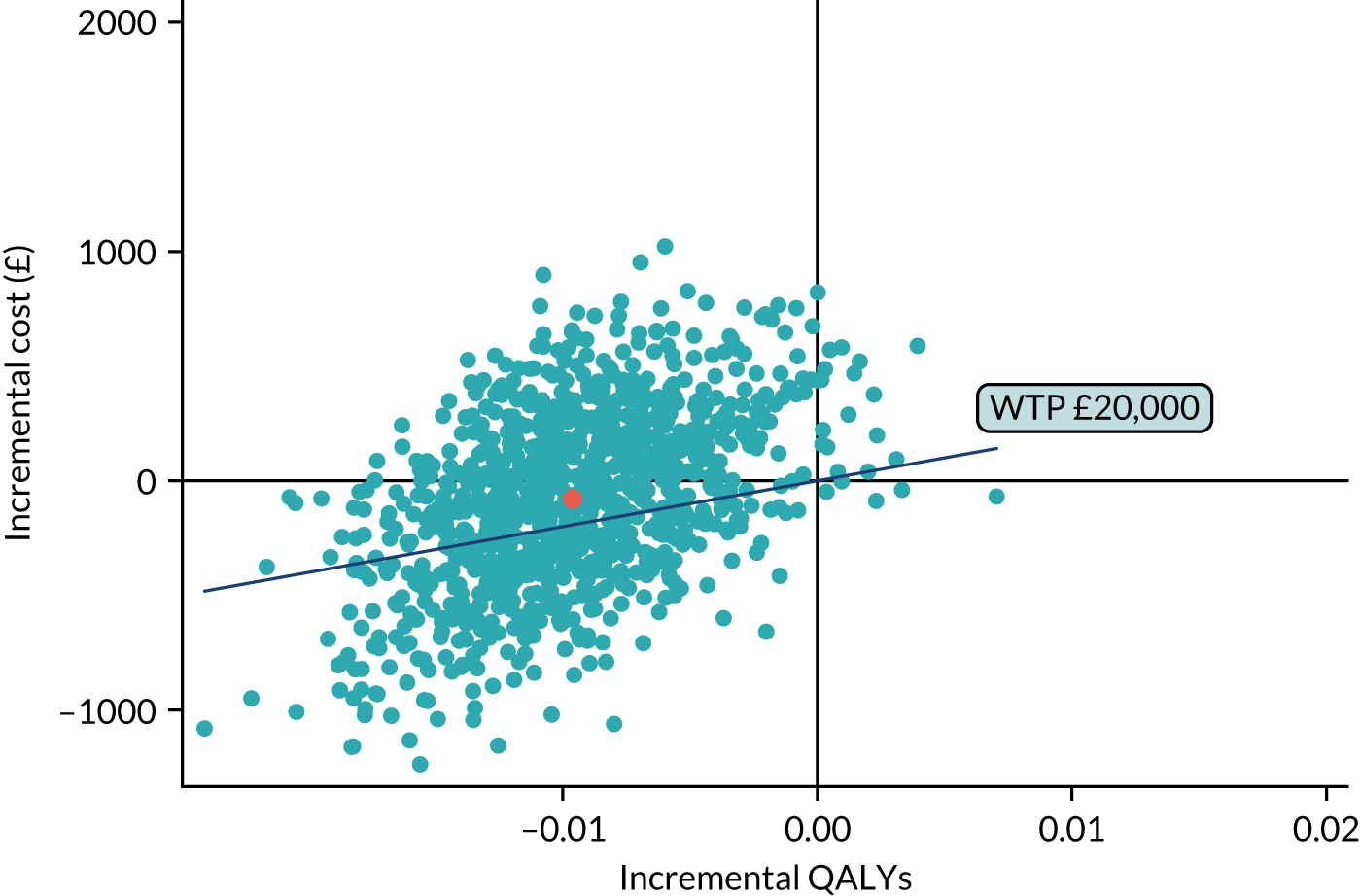
The probability that the MoveMore intervention is cost-effective is presented on the cost-effectiveness acceptability curve shown in Figure 20. At a cost-effectiveness threshold of £20,000 per QALY, the MoveMore intervention has a 38% probability of being cost-effective. As UC has been shown to produce more QALYs, the probability that the MoveMore intervention is cost-effective decreases as the cost-effectiveness threshold increases.
FIGURE 20.
Cost-effectiveness acceptability curve: the MoveMore intervention vs. UC.
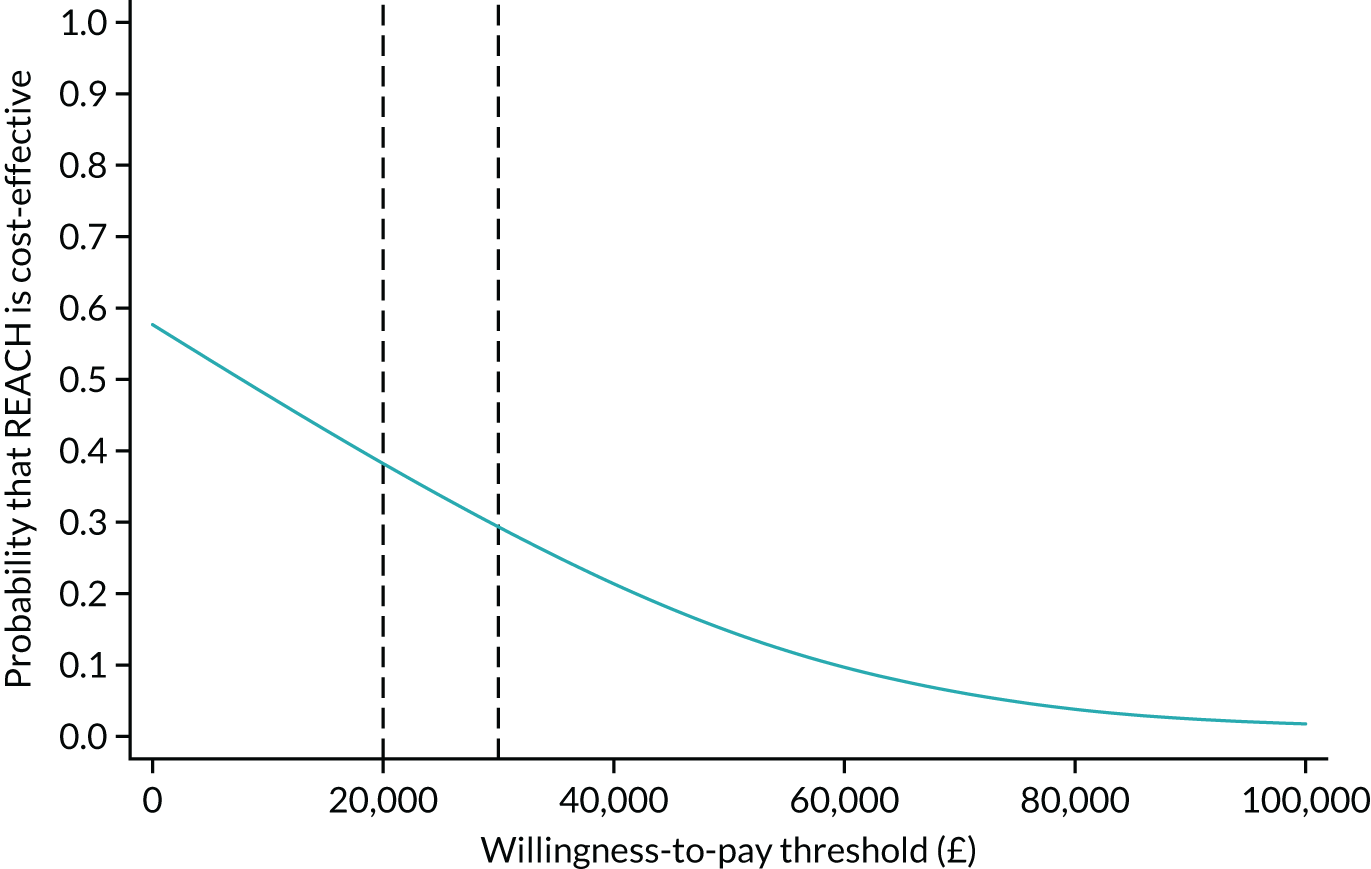
Sensitivity analysis
The cost-effectiveness results for each scenario explored in the sensitivity analyses are presented in Table 76. The results of the primary analysis are not robust to the sensitivity analyses conducted and a great deal of variation in the cost-effectiveness estimates is observed for each scenario explored.
| Treatment group | Cost (£), mean (SD) | Incremental cost (£) | QALY, mean (SD) | Incremental QALY | ICER (£/QALY) |
|---|---|---|---|---|---|
| ITT: unadjusted | |||||
| UC | 1082.08 (711.51) | 0.448 (0.045) | |||
| MoveMore | 1011.15 (561.42) | –70.93 | 0.393 (0.111) | –0.055 | 1290 |
| Complete case | |||||
| UC | 927.76 (824.9) | 0.424 (0.008) | |||
| MoveMore | 1069.67 (625.26) | 141.91 | 0.428 (0.009) | 0.005 | 28,382 |
| Self-reported EQ-5D-5L only: complete case | |||||
| UC | 1778.27 (2157.28) | 0.587 (0.025) | |||
| MoveMore | 1863.79 (1418.49) | 85.52 | 0.569 (0.009) | –0.018 | –4751 |
| Self-reported EQ-5D-5L only: imputed data | |||||
| UC | 1060.48 (710.27) | 0.564 (0.006) | |||
| MoveMore | 1010.81 (552.84) | –49.67 | 0.55 (0.005) | –0.014 | 3548 |
| Proxy-reported EQ-5D-5L only: complete case | |||||
| UC | 1085.9 (743.74) | 0.487 (0.004) | |||
| MoveMore | 1291.36 (666.13) | 205.46 | 0.465 (0.01) | –0.022 | –9339 |
| Proxy-reported EQ-5D-5L only: imputed data | |||||
| UC | 1053.8 (713.48) | 0.472 (0.005) | |||
| MoveMore | 1021.08 (560.73) | –32.72 | 0.453 (0.007) | –0.019 | 1722 |
| Map EQ-5D-5L to EQ-5D-3L: imputed data | |||||
| UC | 1066.75 (703.98) | 0.342 (0.006) | |||
| MoveMore | 1008.24 (552.98) | –58.51 | 0.338 (0.010) | –0.004 | 13,131 |
| Exclude non-implementing CH: imputed data | |||||
| UC | 1082.08 (711.51) | 0.450 (0.005) | |||
| MoveMore | 931.52 (610.44) | –150.57 | 0.430 (0.015) | –0.021 | 7291 |
Health economic model
The modelling framework was primarily informed by the broader policy context of an identified decision problem. In relation to the REACH feasibility study, it has been suggested that long-term care generally receives insufficient policy focus, specifically with respect to the provision of health and social care requirements. Additional complexities may exist regarding the financial arrangements with respect to ownership of CHs (private/public) and also the funding of care (state funded/CH budgets/out of pocket). Discussion among the wider members of the REACH team indicated that individuals could be relocated to long-term care by two main routes: on the basis of a needs assessment or following a hospital admission. It was felt that this was an important aspect to be included in the economic model.
Individuals are commonly placed into a CH in the later years of life (discussion with REACH team suggested, on average, in the last 2 years of life). However, anecdotal experience suggests that residents who survive beyond the average duration of residence may experience substantially longer life.
Interventions to enhance PA levels in CHs were considered economically justifiable, as greater PA may be associated with reduced risk of falls, lowered risk of chest infections, decreased risk of pressure ulcers and potential reductions in the need for wound care. With respect to improving residents’ quality of life, it was believed that increased physical functioning may correlate to improvements in moods, better mobility and, with certain groups, reduced agitation. With regard to potential cost offsets elsewhere in the health service, hospital admissions and transition from the CH to a nursing home were considered two potential risks associated with low levels of PA.
Model framework
The model schematic shown in Figure 21 is proposed to cover salient states requiring consideration to evaluate cost-effectiveness. This was informed by discussions with the wider REACH team.
FIGURE 21.
Exemplar model structure. A, active; D, death; I, inactive; N, nursing home.
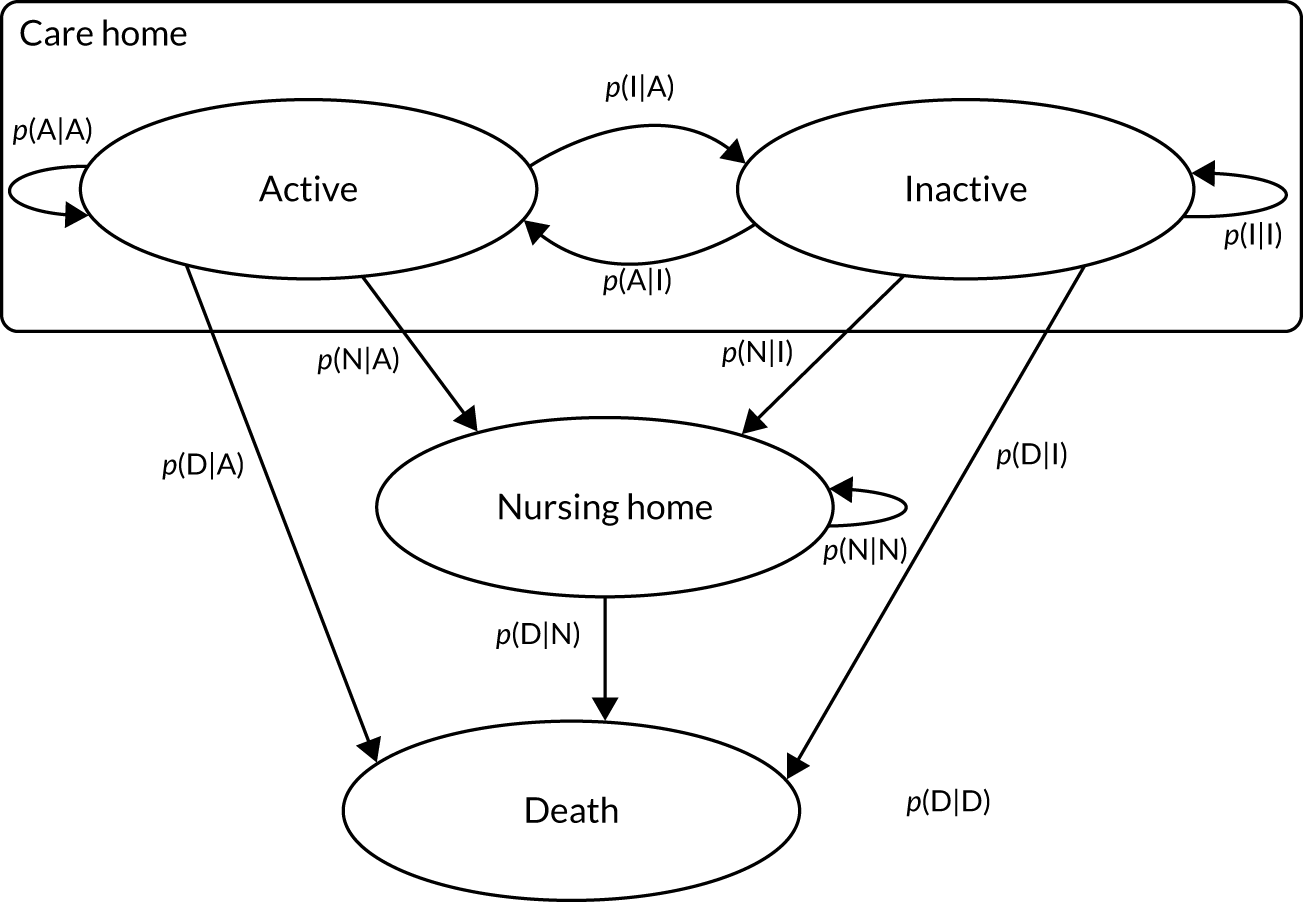
The model describes a simplified resident pathway. In the ‘CH’, proportions of the residents are described as being in either ‘active’ or ‘inactive’ health states. The terms ‘active’ and ‘inactive’ are broad classifications of activity levels to allow flexibility in extrapolating outcomes from existing and future primary RCTs. Residents move (transit) between health states according to transition probabilities (denoted by arrows). Residents can transit between ‘active’ and ‘inactive’ or they can transit to ‘nursing home’, which is a one-way sequence (tunnel state), as it is assumed that, once a resident transitions to nursing home care, they remain in nursing home care for the remainder of their life. Death is an absorptive state and the model requires estimates of the probability of death given current PA levels in CHs and nursing homes.
Each health state has costs and quality-of-life values associated with it, and residents accrue these as they transit through the health states.
Model parameters
The parameters required for the model are outlined in Table 77.
| Parameter | Value | Proposed source |
|---|---|---|
| Costs | ||
| Active | Resource use costs | Trial and relevant literature |
| Inactive | ||
| Nursing home | ||
| Dead | ||
| Quality of life | ||
| Active | Utility value associated with quality of life | Trial and relevant literature |
| Inactive | ||
| Nursing home | ||
| Dead | ||
| Probabilities | ||
| p[A|A] | Different probabilities depending on REACH intervention/UC | Trial and relevant literature |
| p[I|A] | ||
| p[N|A] | ||
| p[D|A] | ||
| p[A|I] | ||
| p[I|I] | ||
| p[N|I] | ||
| p[D|I] | ||
| p[N|N] | ||
| p[D|N] | ||
| p[D|D] | ||
It was anticipated that interventions that promote PA levels in long-term care will influence the probability of the inactive groups becoming active (i.e. p[A|I]) or reduce the probability of the active group becoming inactive (i.e. p[I|A]). Given that the anticipated life expectancy for living in long-term care facilities is low, the feasibility of estimating the probabilities required for the model was explored.
For residents in a nursing home, the health-state utility associated with being active may be assumed to be higher than for those who are inactive (assuming no adverse events occur from increased activity) and our expectation of overall health-state utility considered change in the likelihood of (1) risk of falls, (2) chest infections, (3) pressure ulcers and (4) wound care, conditional on activity level. Health-care costs associated with these four specific health risks were also considered, and the feasibility of obtaining relevant costs and utility estimates was explored.
Model feasibility
Parameterisation of the exemplar model outlined in Model framework was not feasible with the data obtained from the feasibility trial and the current wider evidence base.
Of particular importance was the lack of treatment effect for the MoveMore intervention, as there was little difference in quality of life reported on the EQ-5D-5L and there was also little difference in the activity levels of residents, compared with UC. This meant that parameterisation of the model in terms of a treatment effect would require heroic assumptions, as current evidence is inconclusive. The uncertainty around the treatment effect is also demonstrated in the level of variation observed in the within-trial sensitivity analyses.
A further limitation to the evidence base was the lack of a clear threshold to categorise active and inactive states that are relevant to this population group. The use of activity thresholds reported in the literature may not be sensitive to the changes observed in this older age group. Consequently, estimation of the relevant transition probabilities will not be feasible until a consensus is reached of how active/inactive is defined for this population group.
As it was not feasible to parameterise the model, we were unable to present estimates of long-term cost-effectiveness. However, we present an exemplar model that could be used as relevant data become available in the future and could be used to demonstrate the areas of further research that are required to make such a model feasible.
Discussion
Principal findings
The primary trial-based cost-effectiveness analysis indicated that the MoveMore intervention was not a cost-effective use of NHS resources, compared with UC. However, the results should be viewed with caution, given the small sample size in the feasibility trial, issues causes by the use of proxy-versus self-reported EQ-5D-5L questionnaires, and the number of missing data in the self-reported EQ-5D-5L questionnaire.
In both trial arms, EQ-5D-5L scores appeared to decrease over the trial period. Only for the last follow-up and only for self-reported EQ-5D-5L questionnaires did scores rise in the REACH arm. This small increase was not reflected in the proxy-reported EQ-5D-5L questionnaires. Overall, fewer QALYs were gained in the MoveMore arm than in the UC arm. The health-care associated costs were also lower in the MoveMore arm than in the UC arm. When the lower costs are analysed alongside the fewer QALYs, the MoveMore intervention does not appear to be cost-effective. However, the results were not robust to alternative assumptions explored in sensitivity analyses. There was considerable variation in the cost-effectiveness estimates, with each variation in assumptions indicating substantial uncertainty around the results.
Strengths and weaknesses of the economic analysis
One strength of this feasibility study lies in the randomised controlled design of the trial. This enabled the collection of good-quality data that were used in this analysis to explore the feasibility of a full trial and the feasibility of the analysis to be conducted. However, consideration of longer-term outcomes at this stage has not been feasible; this would be a valuable addition to future research.
A further limitation lies in the acceptability of using proxy and self-reported EQ-5D-5L scores. This was necessary given the frailty of the participants in this trial, but is problematic because of potential differences in self-reported and proxy-reported scores. Although self-reported and proxy-reported scores were significantly correlated, scores reported by proxy typically appeared lower than those that were self-reported. Previous work relating to the impact of the use of proxy-reported quality of life is relatively inconclusive, with some studies arguing that proxies provide an acceptable source of data83,84 whereas others suggest that there is too much variation between proxy- and self-reported scores. 85 The impact of using proxy- versus self-reported EQ-5D-5L scores was explored in sensitivity analyses, but should be explored further in a full trial analysis, as the relatively small sample size in this feasibility study means that it is not possible to draw firm conclusions.
Meaning of the feasibility trial
The analysis conducted for this feasibility trial has shown that a within-trial cost-effectiveness analysis would be feasible as part of a full trial. However, it is noted that, for both quality of life and resource use data, compliance decreased over the duration of the feasibility trial. Consequently, if a full trial was conducted, ways to maintain compliance should be explored, for example altering the frequency of questionnaires to address questionnaire fatigue.
A decision model to explore long-term impacts of the intervention was designed as part of this analysis. However, it was not feasible to parameterise the model with the current evidence base. Consequently, a full trial would need to build on the evidence base for a decision model to be feasible and useful.
Unanswered questions and further research
Although the analysis conducted here provides preliminary estimates of cost-effectiveness, the primary purpose was to assess the feasibility of conducting such analyses as part of a full trial. This feasibility trial was not powered to provide definitive answers; consequently, a full trial would need to be conducted to reduce the uncertainty around the cost-effectiveness estimates.
In addition, further research is required to enable the parameterisation of a decision-analytic model to explore the long-term impact of the MoveMore intervention. For example, further research to define what would reasonably count as active or inactive for this population group would be of value.
List of abbreviations
- 6-CIT
- Six-item Cognitive Impairment Test
- A&E
- accident and emergency
- ADL
- activities of daily living
- ANOVA
- analysis of variance
- AO
- activity organiser
- APAFOP
- Assessment of Physical Activity in Frail Older People
- BCT
- behaviour change technique
- BI
- Barthel Index
- CH
- care home
- CI
- confidence interval
- cpm
- counts per minute
- CQC
- Care Quality Commission
- DEMQOL
- Dementia Quality of Life
- EMS
- Elderly Mobility Scale
- ENRICH
- Enabling Research in Care Homes
- EQ-5D-3L
- EuroQol-5 Dimensions, three-level version
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- FAC
- Functional Ambulation Classification
- GDS
- Geriatric Depression Scale
- GP
- general practitioner
- ICC
- intracluster correlation coefficient
- ICER
- incremental cost-effectiveness ratio
- IM
- intervention mapping
- IQR
- interquartile range
- ITT
- intention to treat
- MET
- metabolic equivalent of task
- NC
- nominated consultee
- NICE
- National Institute for Health and Care Excellence
- NPT
- normalisation process theory
- NVQ
- National Vocational Qualification
- PA
- physical activity
- PAM-RC
- Physical Activity and Mobility in Residential Care Scale
- P-CAT
- Person-centred Care Assessment Tool
- PC
- personal consultee
- PDG
- Programme Development Grant
- PE
- process evaluation
- PPI
- patient and public involvement
- PV
- predictive value
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- REACH
- Research Exploring physical Activity in Care Homes
- SD
- standard deviation
- TUGT
- Timed Up and Go Test
- UC
- usual care
- WHOQOL-OLD
- World Health Organization Quality of Life-OLD
- WS
- workstream
Notes
-
Example of how concepts were presented to the Advisory Group
-
Intervention mapping process: performance objectives, behaviour change techniques and methods
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/pgfar09090).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
