Notes
Article history
The research reported in this issue of the journal was funded by PGfAR as project number RP-PG-0606-1071. The contractual start date was in August 2007. The final report began editorial review in August 2012 and was accepted for publication in February 2013. As the funder, the PGfAR programme agreed the research questions and study designs in advance with the investigators. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PGfAR editors and production house have tried to ensure the accuracy of the authors' report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Christopher Dowrick is a non-executive director of Mersey Care NHS Trust. Pete Bower has received funding from the British Association for Counselling and Psychotherapy for consultancy. Carolyn Chew-Graham was an advisory board member for Self Help Services, Manchester. Karina Lovell is a non-executive director of Manchester Mental Health and Social Care Trust.
Permissions
Copyright statement
© Queen's Printer and Controller of HMSO 2013. This work was produced by Dowrick et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Overview of the programme
In this chapter we describe the background to and rationale for our programme to increase equity of access to high-quality mental health services through primary care and provide a summary of what we proposed to do. We also provide a programme summary in Appendix 1. Throughout the text we refer to the the programme as ‘AMP’ or the ‘AMP programme’, in which AMP refers to Improving Access to Mental Health in Primary Care.
Background
According to the World Health Organization, in Western Europe over one-third of the population experience mental ill health at some time in their lives, with the majority coming into the diagnostic categories of anxiety and depression. 1 Mental health problems impose substantial emotional, social and economic burdens on those who experience them, their families and carers and society as a whole. 2 People suffering from depression and anxiety find it much more difficult to hold down a job, and those in work are likely to have high rates of sickness absence: > 900,000 adults in England claimed sickness and disability benefits for mental health conditions in 2003, with particularly high claimant rates in the north of England. 3,4 Layard5 has calculated the resulting loss of output within the UK as £17B or 1.5% of gross domestic product. Much of this cost falls on the Exchequer, which loses in consequence roughly £9B in benefit payments to people with mental health problems and reduced tax receipts. If problems related to impaired work efficiency (‘presenteeism’) as a result of mental ill health are included, the calculated loss of output is considerably higher. 6
A wide range of clinical interventions,7,8 collaborative care,9 self-management10 and social and community initiatives11 have been shown to be effective in trials in improving outcomes for people experiencing common but disabling mental health problems such as depression and anxiety.
Underserved groups
Many people with high levels of mental distress are disadvantaged, either because care is not available to them at the right place or at the right time or because when they do access care their interaction with caregivers deters help-seeking or diverts it into forms that do not address their needs. 12
Groups with inadequate access to primary care include people from black and minority ethnic (BME) communities, asylum seekers, homeless people and adolescents with eating disorders. For example, women of South Asian origin in the UK have a high prevalence of depression and self-harm, often in the context of severe and persistent social difficulties, which only become apparent when they are in a crisis. 13 Asylum seekers are at greatly increased risk of mental health problems:14 they are 10 times more likely to have post-traumatic stress disorder (PTSD) than age-matched general populations15 and face substantial political, institutional, cultural and language obstacles to accessing primary care. 16 Mental health problems are up to eight times more prevalent among homeless people than in the general population. 17 There is a ‘cycle of reluctance’ of homeless people to use primary care services and of general practitioners (GPs) to accept them, and homeless-focused primary care services may still not access rough sleepers, who are at greatest risk. 18 Although anorexia nervosa has the highest mortality rate of any mental disorder,19 young people with eating disorders rarely present on their own account to clinical services. 20
Groups who receive inadequate help when they do access primary care include elders, people with advanced cancer, those at risk of long-term sickness absence and people with medically unexplained symptoms. Depression is common in older people, particularly those with chronic physical illness, but tends to be underdiagnosed and inadequately managed. 21,22 Depression appears to be a significant and persistent symptom for about one-quarter of patients with advanced cancer23 and may be an independent predictor of mortality. 24 People with mental health problems are at risk of long-term sickness absence25 but primary care currently has few strategies to identify or help them. People considered to have unexplained physical symptoms often present with mental health needs,26 but clinicians tend to disregard these and assert somatic agendas; many of these patients are sceptical about doctors' ability to manage their health problems. 27
We focused on these eight groups as exemplars of those who are underserved by primary care because we were able to deploy the existing scientific and clinical expertise of our research group with regard to these groups. We considered that lessons learnt here may have wider implications for other groups of people whose mental health problems are managed within primary care.
The extent of commonality of issues across these groups meant that a combined approach was likely to be the most effective. The Social Exclusion Unit's report on mental health confirms that people from these groups face overlapping barriers to getting their mental health needs addressed. 3 Women from BME communities, homeless people, asylum seekers and elderly people living alone, for example, often experience severe and persistent social difficulties. Engagement and communication are inherently problematic in the cases of adolescents with eating disorders28 and women from ethnic minorities. 29
These groups also share a crucial set of problems with regard to health literacy, that is, the capacity to obtain, interpret and understand health information and services in ways that are health enhancing. 30 Health literacy is in part related to lack of educational attainment, but importantly it is also about the stigma associated with seeking help for mental health problems. Health literacy is critical for patients' confidence in themselves, and in the services they seek (or often do not seek) to access.
Health literacy needs to work both ways. Health services have an obligation to be literate about the needs of the patients they seek to serve. Empirical work on primary care provision for hard-to-reach groups has focused on how to physically structure services, that is, whether primary care trusts (PCTs) [or the forthcoming clinical commissioning groups or (CCGs)] should commission services that focus solely on provision for specific groups (e.g. elders or people from BME communities), or whether mainstream general practices should be encouraged to provide more flexible care through the enhanced services route. However, we considered that the key issue here is not how services are physically structured or funded, but how people from these underserved groups can be enabled to access high-quality mental health services in primary care. 31
Access to health care
In the UK, policy interest in access to mental health care has largely been restricted to two major issues. Understanding the delivery of mental health care has often been predicated on the influential ‘pathways to care’ model. 32 This model identifies several ‘filters’ that exist between patients with mental health needs in the community and different ‘levels’ of care, and has highlighted the importance of the recognition of mental health problems by primary care ‘gatekeepers’33 and the difficulties of training professionals to improve recognition and referral. 34,35
The second major policy concern is the provision of non-pharmacological treatments such as psychological therapies. Although such treatments are generally more acceptable to patients than medication,36 access is far more restricted because of limitations in the number of adequately trained therapists who can deliver these treatments, and because of problems with cultural congruity between therapists and many prospective clients. 37
Developing interventions to improve access to mental health care is a policy priority and has led to two major policy innovations in the UK. The first involves changes to the contract under which GPs are paid: one target in the Quality and Outcomes Framework (QOF)38 involves payments to GPs to use standardised screening instruments to detect cases of depression in populations such as patients with long-term conditions. 39 The second is the Improving Access to Psychological Therapies (IAPT) programme, which has involved the recruitment of psychological therapists,40 the introduction of ‘minimal’ psychological interventions such as guided self-help and computerised treatments41 and the adoption of the ‘stepped-care’ model to maximise patient access to care. 42
These access innovations are based on assumptions that are not always made explicit. Importantly, there is a focus on supply-side factors, such as the availability of treatments, and on structural and organisational changes required to reduce or remove instances in which pathway ‘filters’ become barriers to care. There is generally less explicit consideration of demand issues and the factors governing the journey of the patient in need. Within health sciences, there is increasing recognition of the need to base quality improvement activities on rigorous theories and models that describe core concepts of relevance, and outline the mechanisms and relationships that underlie service delivery problems. 43,44
Proxy measures of access, such as service use or supply of health professionals, have been used, but a full consideration must include multiple dimensions such as adequacy of supply, barriers to access, effectiveness and equity for different population groups. 45
If services are available and there is an adequate supply, then the opportunity to obtain health care exists. The extent to which a population gains access also depends on financial, organisational and social or cultural barriers that limit the utilisation of services. Available services must be relevant and effective if the population is to gain access to satisfactory health outcomes. Availability and barriers have to be considered in the context of the perspectives, health needs and settings of diverse groups in society. Equity of access may be measured in terms of the availability, utilisation or outcomes of services. Both horizontal (equal treatment for equal groups) and vertical (unequal treatment of unequal groups) equity require consideration.
Aim and objectives
We decided to undertake a research and development programme to determine how people from underserved groups can make better contact with primary care and to find out how to ensure that they receive the help that they really want and need for their mental health problems.
The aim of the AMP programme was to increase equity of access to high-quality primary care mental health services for underserved groups.
We had six principal objectives:
-
to clarify the mental health needs of people from underserved groups, who have been shown to receive inadequate primary care mental health services
-
to identify evidence-based primary care services that such people consider relevant to their needs
-
to identify barriers to, and facilitators of, access by such people to high-quality primary care mental health services
-
to develop and test a portfolio of interventions that are credible and acceptable for particular underserved groups
-
to establish effective strategies for the dissemination of evidence about interventions for members of underserved groups with mental health problems that have demonstrable efficacy and acceptability
-
to begin to integrate into primary care effective and acceptable interventions for people with mental health problems from underserved groups.
We considered it important to address the following key issues:
-
Complex problem presentation in primary care. The common mixture of physical and psychological symptoms makes assessment challenging, for example identifying depressive symptoms among older people or those with advanced cancers, or being aware of the frequency of primary presentation of physical symptoms among women from ethnic minorities.
-
Current diagnostic categories may be irrelevant, unhelpful or disabling,46 for example the concept of medically unexplained symptoms, the difference between depression and demoralisation for patients with advanced cancers, and depression in older people with chronic physical disease.
-
User-defined perspectives are crucial regarding definitions of unmet needs and how these needs are best understood. For example, qualitative work with patients with unexplained symptoms indicates that patients are unconvinced of the ability of doctors to treat psychosocial problems;47 and older people often view depression differently from health professionals. 48
-
Engagement and communication problems. With adolescents with eating disorders, lack of engagement is an inherent part of the disorder, including difficulty describing thoughts and emotions, embarrassment and negative attitudes to adults in authority. 28 Women from ethnic minorities tend to seek professional care only when in crisis. 29 Homeless people perceive reluctance to treat on the part of service providers.
-
Professional contexts. As currently configured, primary care services often do not meet the mental health needs of these patients. This may be because of the perceived stigma associated with attending mental health services, poor agreement between service and patient or client regarding treatment aims,49 poor outcomes of existing treatments or inaccessible or unclear pathways to care. In palliative care of advanced cancers, for example, professional training concentrates on physical care at the expense of psychological or spiritual dimensions. 50
We designed our programme to add value by combining clinical and methodological expertise. We built on Watters' three-dimensional model51 for exploring inter-relationships between macro-level institutional factors in the creation of mental health problems among these underserved groups and the interventions offered to them within or through primary care. We focused our efforts on targeting key clinical outcomes, exploring how to adapt service configurations to meet patients' needs, rather than changing patient presentation to fit in with existing services. We put patients' experiences and expressed needs at the centre of care, and addressed the practice and policy contexts in which these are located.
Programme plan
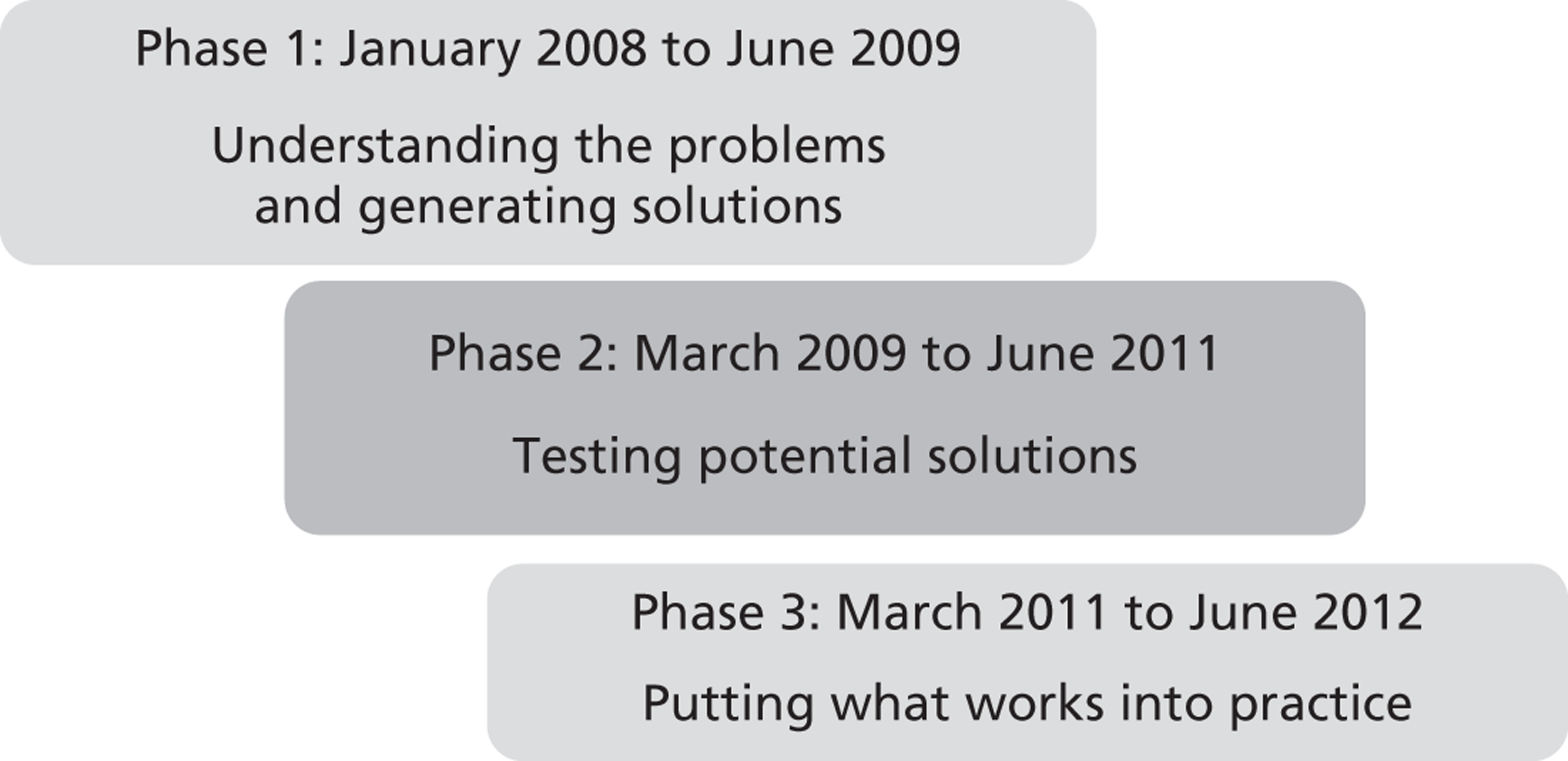
We designed the AMP programme to link knowledge about barriers to, and facilitators of, access for our exemplar groups with the perspectives of users, developing creative ways to meet the particular needs of these groups. We divided the programme into three overlapping phases (Figure 1).
FIGURE 1.
The AMP programme plan.
-
Phase 1 (months 1–18) – understanding the problems and generating potential solutions. We undertook a general review of barriers to, and facilitators of, access to care, and interventions to overcome barriers, using a combination of literature reviews and qualitative research methods. We focused on user perspectives of mental health issues in relation to each of the underserved groups to understand whether or not there were any access issues specific to each group and how different issues affect them all. We then considered the results of our reviews and used a consensus process to develop exemplar interventions that took account of known barriers and faciliators while remaining sensitive to the needs, preferences and priorities of our exemplar underserved groups and other stakeholders. We describe this process in Chapter 2.
-
Phase 2 (months 15–48) – testing potential solutions. We developed interventions designed to improve access, understanding and care by setting up a model of care, which we called the AMP Development Partnership. This model of care has three linked domains: increasing community stakeholder engagement, enhancing the quality of primary care and providing culturally sensitised well-being interventions. We developed interventions at the community, primary care and individual patient level. We used a quasi-experimental design to test the components of the AMP model, individually and jointly, in terms of their acceptability and credibility to service users and other stakeholders, their impact on the mental health of service users and their service implications. In Chapters 3–7 we describe how we implemented and evaluated the three components of the AMP model of care. We consider the implications of the combined AMP model of care for increasing access to appropriate primary care and well-being interventions and for reducing mental health stigma in the community.
-
Phase 3 (months 43–60) – putting what works into practice. We developed and evaluated methods to disseminate our findings across the broad economy of primary health care, including focused implementation experiments at both policy and practice levels in different PCTs, stakeholder meetings and the creation of a dedicated AMP website. We describe this phase in Chapter 8.
Finally, we draw the elements of the programme together. We make recommendations for future research and consider the implications of our evidence for clinical practice.
Chapter 2 Understanding the problems and generating solutions
In this chapter we set out our reasons for examining and synthesising multiple sources of evidence about inequities in access to high-quality mental health services. We describe how we collected this evidence and present our key findings from each of the sources. We then explain the methods that we used to draw the evidence together to plan our interventions.
Underlying perspectives
We began with the assumption that members of underserved groups are not passive sufferers of mental health problems but are people who interpret and respond to experiences and who are capable of mounting challenges to external forces bearing on them. 51 We considered the inter-relationships between macro-level societal and institutional factors in the creation of mental health problems among hard-to-reach groups and the ways of coping with and overcoming these problems, including interventions offered to them within or through primary care. We focused on key clinical outcomes, exploring how to adapt service configurations to meet patients' needs rather than changing patient presentation to fit in with existing services. We put patients' experiences and expressed needs at the centre of care and addressed the broader practice and policy contexts in which these are located.
We adopted a whole-system approach to identify the need for a range of credible and acceptable interventions, and the barriers to and facilitators of their development. This meant that we should examine diverse sources of evidence. 52 Quantitative evidence from randomised trials provides information about what works and for whom, but is of little help in explaining how or why. Grey literature, produced by service providers or advocacy groups, is a useful source of evidence for the current priorities of policy-makers and service providers, and for service innovations, although is sometimes lacking in rigorous evaluation. Qualitative sources of evidence are needed to find out why current practices may not work, and what might help to improve them. Published qualitative sources may not directly address key questions that we are concerned with here, namely problems with access; hence, there may be a need to turn to detailed interview transcripts, or to ask actual and potential service users and providers directly about specific issues. Stakeholders must be involved not only in answering research questions, but also in conceptualising the questions to be asked. It is then essential to find effective and valid ways of synthesising evidence to generate and test potential solutions.
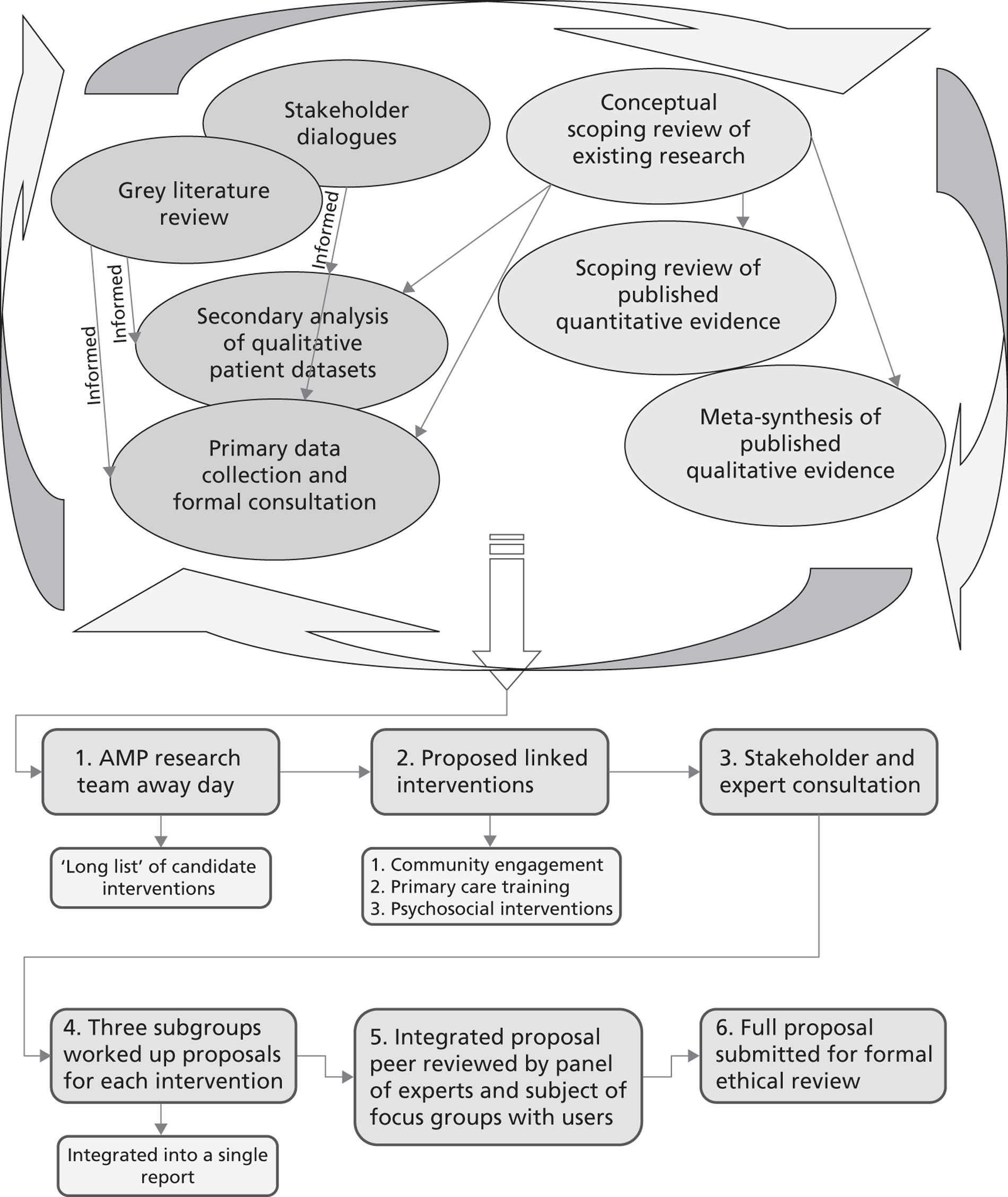
The approach we have taken is presented schematically in Figure 2, to which the rest of this chapter refers. We conducted seven linked studies. We began with a conceptual scoping review. We undertook a structured scoping review of published quantitative literature and a meta-synthesis of published qualitative literature. We reviewed relevant grey literature and undertook a secondary analysis of qualitative data sets generated with actual and potential users of primary mental health-care services. We also conducted two stakeholder consultation exercises, generating new qualitative data. We carried out the literature reviews and stakeholder exercises in parallel, rather than in series, to give stakeholders the opportunity to inform the literature reviews and analysis of available qualitative data.
FIGURE 2.
Methods of evidence generation and synthesis. 52 Reproduced with permission from Dowrick C, Gask L, Edwards S, Aseem S, Bower P, Burroughs H, et al. Researching the mental health needs of hard-to-reach groups: managing multiple sources of evidence. BMC Health Serv Res 2009;9:226.
Identifying key concepts
We began with a conceptual scoping review to develop a map of key concepts concerning access to primary care, and to identify the range of current interventions that have been used to improve access to care (see Structured scoping review of published quantitative literature). This review was generic and not restricted to mental health; the intention was to capture the full range of relevant concepts and definitions. Initially, members of the research team were asked to identify key papers and books relating to access. This database was augmented by a search of electronic databases using a range of terms relating to access, combined with a search filter developed at the National Primary Care Research and Development Centre in Manchester, to identify conceptual and theoretical literature. Candidate interventions around access were developed, starting with the list of interventions developed by the Effective Practice and Organisation of Care (EPOC) group of the Cochrane Collaboration,53 and refined through focused literature searches and reflection on the developing conceptual map.
The major components of our conceptual scoping review have been described in the paper by Dowrick et al. 52 and are presented in Figure 3.
FIGURE 3.
Key concepts in access to health care.
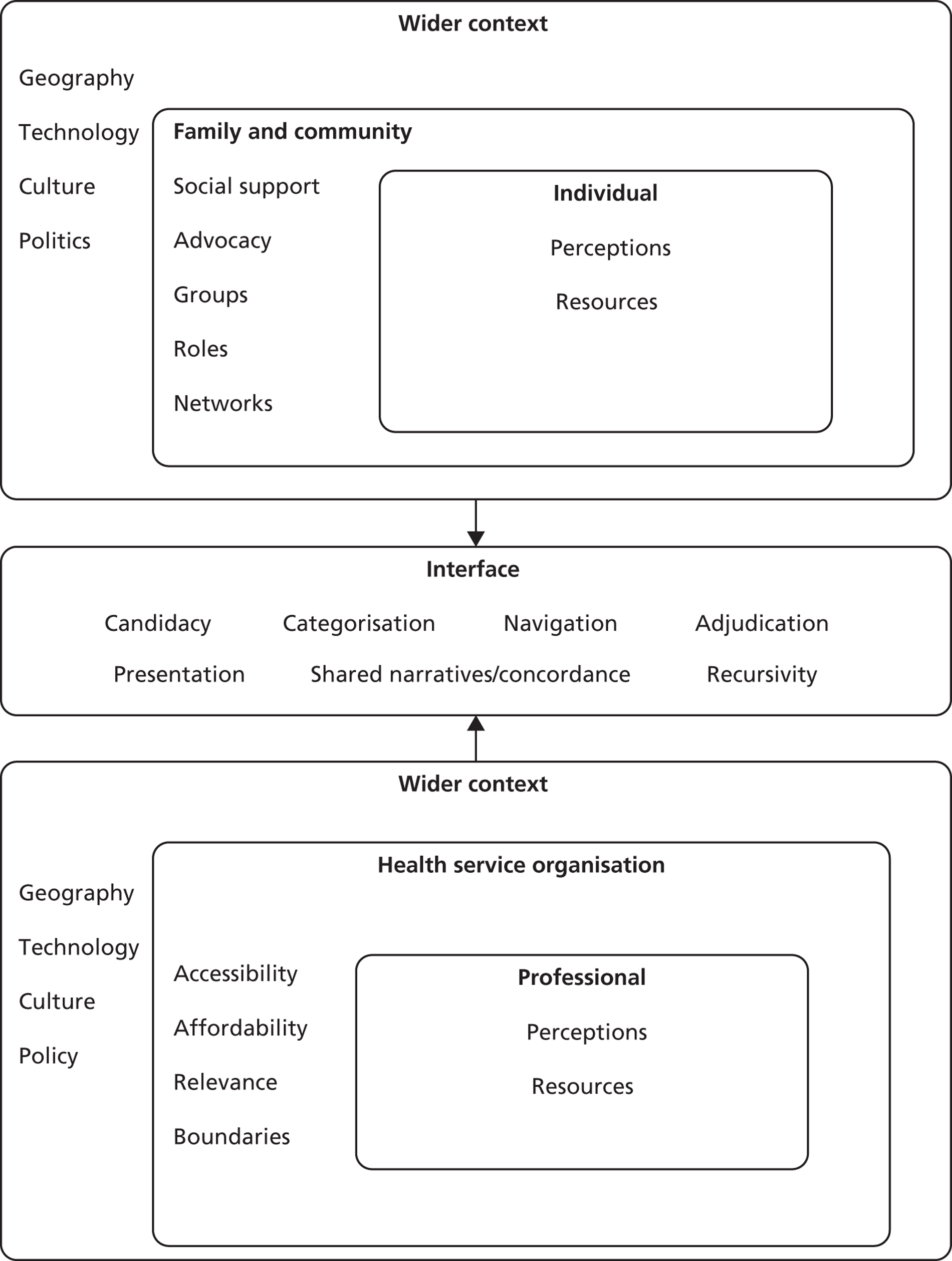
We draw attention to six key overlapping concepts emerging from this review: recursivity, candidacy, identity and morality, graduated access, adjudication and cultural competence.
Recursivity refers to the ways in which illness behaviour is both enabled and constrained by the interactions that take place between individuals and health professionals in health service settings. Illness behaviour and personal illness management strategies are modified by service contact, as people learn to ‘fit’ into what is required of them by health professionals and their beliefs about what is legitimate illness and service use. 54 The ability of health professionals to communicate effectively with patients may reinforce or discourage health action in the future. 55
Candidacy describes how people's eligibility for health care is determined between themselves and health services. 56 The reaction to each illness episode draws on past experience, cultural expectations, norms and self-definitions. This reservoir of candidacy, an understanding of a right to care, is then shaped towards resolving the individual illness episode. Candidacy in relation to an individual illness episode should be seen as a special case of the individual's ongoing perceptions of their right to care, balanced against a fear of socially inappropriate behaviour. Candidacy arises from ongoing negotiation, influenced by a wide number of factors. Health services are constantly defining and redefining the legitimate objects of health services. In response, people in the community are also trying to make sense of this process.
Following determination of candidacy, individuals undertake navigation to gain a point of entry to health services – an ‘appearance’. This involves a series of psychological and cognitive competencies and resources, which include self-efficacy57 and health literacy. 58 These capacities are partly patterned by individual characteristics, but also through the interaction of those individual capacities and the health-care system.
Appearances can involve a number of different approaches, including appearing before health services through patient-initiated actions, or through ‘invitations’ (where people respond to health services) or ‘grabs’ (where candidacy is not under patient control, such as compulsory hospital admission). Screening for depression during routine medical consultations reflects aspects of both of these types. 39 Other work has highlighted the role of more diffuse approaches (described as ‘muddling through’) in the presence of ambiguous symptoms, in which the effects of close social networks are emphasised. 59
With respect to identity and morality, an orientation to candidacy brings several aspects of the sociological discourse on identity into play. Identity refers to an individual's sense of self, and is maintained in interaction with others. People are motivated to seek confirmation of their identity in interactions with others, and there is some evidence that negative experiences with regard to health services reflect in part threats to identity. 60 This may involve perceived stereotyping by health professionals, feelings of disempowerment and feelings that their subjective experience is ignored.
Another strand of the identity discourse deals with roles. If illness threatens competence to perform social roles, it may involve a fundamental challenge to self. For example, in women presenting with depression in primary care, perceived failures of competence in primary social roles were interpreted as a sense of duty to seek care,61 but framing help-seeking as a moral action coloured women's experiences of care, which in turn came to be seen in terms of ‘self-sacrifice’ and the ‘moral dilemma’ of accepting medication.
In terms of graduated access, the concepts of recursivity and candidacy suggest that access to care is best seen as an interaction between organisational factors operating in health services combined with people's perceptions of those services and their individual social circumstances in seeking care. 62 One way of changing access is to modify service provision options at the point at which people want to access services. This may involve ‘graduated access’ to services, including services that people can access without requiring face-to-face contact with professionals and which maximise the use of new technologies such as the internet.
Adjudication refers to professional judgements about the presentation of an individual for an intervention or a service, influenced by categorisations made by professionals with reference to current services and relationships. Traditionally, this has been dominated by work on recognition and diagnosis and the application of standardised diagnostic systems. However, wider considerations are also at play. There have been concerns that psychological therapy services for mental health have been preferentially delivered to certain populations, threatening equity of access. 63 As services are generally oversubscribed, they may be withheld or rationed in ways that may not be made explicit, or inappropriate contact may be negotiated to preserve a relationship with a patient.
Adjudication leads to an offer (or non-offer) of a health service, which may be accepted or rejected. Current models of improving access, which focus on increasing throughput of patients and the efficiency of treatment delivery, have tended to assume that an offer will be sufficient, without necessarily giving enough attention to the likely response. The response of a patient will depend on the ‘fit’ between the offer and his or her identity. Primary care access can be seen as a distinctive field of activity and habitus,64 a set of dispositions that generate practices and perceptions of the way in which people encounter it. As primary care presents a set of technologies and relationships, past experience of illness and service contact coalesce with immediate decision-making about use. The concept of recursivity captures how the response of the system to patients may reinforce or discourage future health actions.
With regard to cultural competence, mental health services in the UK have been criticised for not being responsive to the needs of racial and ethnic minorities. 65 Improving the experiences of such patients requires measures such as hiring practitioners who speak relevant languages and understand the backgrounds of particular patient groups, and a willingness of clinicians to take cultural and ethnic issues into account during their management of patients. 66 One criticism of the notion of ‘cultural competence’ is that it often focuses on particular BME groups and ascribes characteristics to individuals based on a crude group membership. 67 An alternative conception is that cultural competence requires clinicians to take into account the individual values, beliefs and practices of the patient (which may or may not reflect his or her membership of a group). In this way, cultural competence can be seen as a specific form of patient-centredness,68 in which the clinician ‘tries to enter the patient's world, to see the illness through the patient's eyes’ (p. 35). 69 It is also important to pay careful attention to the ways in which cultural context affects our understanding of the nature of clinical evidence. Kirmayer70 has noted that Western diagnostic and conceptual frameworks may be culturally determined, and that cultural communities may have ‘ways of knowing’ that do not rely on the kinds of observational and experimental measures and methods that characterise evidence-based practice.
Gathering evidence
We used these concepts to inform our investigation into the mental health needs of people from underserved groups and how best to meet them, drawing evidence from six separate sources.
Structured scoping review of published quantitative literature
Aim
The purpose of our structured scoping review was to assess the extent and broad results of published quantitative evidence concerning the effectiveness of candidate interventions in improving access to care.
Methods
The population under review was patients with mental health problems in primary care. This included diagnosed disorders and non-specific problem categories such as ‘psychosocial problems’ and ‘stress’. Interventions included the range of candidate interventions that have been used to improve access to care identified in the scoping review. Comparisons included no treatment, usual care and other candidate access interventions. We expected that most published quantitative evaluations of the effectiveness of interventions would focus on effectiveness and cost-effectiveness outcomes and that benefits of access would be implied rather than stated. The focus was on identifying the amount of evidence for each group, the range of interventions that had been trialled and the broad pattern of the results.
The review began with a search of the Cochrane Database of Systematic Reviews (CDSR) and Database of Abstracts of Reviews of Effects (DARE) for previous reviews of candidate access interventions. This was followed by a search of MEDLINE, EMBASE, Cumulative Index to Nursing and Allied Health Literature (CINAHL) and PsycINFO using a range of terms relating to candidate access interventions, combined with a randomised controlled trial (RCT) and primary care filter. Searched were conducted between January and April 2008. The search strategy is provided in Appendix 2. The full texts of abstracts identified by the search were obtained and eligibility was judged by two reviewers. Papers for which eligibility was difficult to judge were assessed by other members of the research team and disagreements were resolved by discussion.
The resources available for the structured scoping review of published quantitative literature were insufficient to allow a full systematic review of all interventions in all populations groups (i.e. comprehensive searches, full assessment of quality and formal synthesis). Rather, the review was designed to identify the amount and type of quantitative evidence relating to access interventions in each of our exemplar groups and to summarise the broad magnitude, direction and consistency of effects.
Results
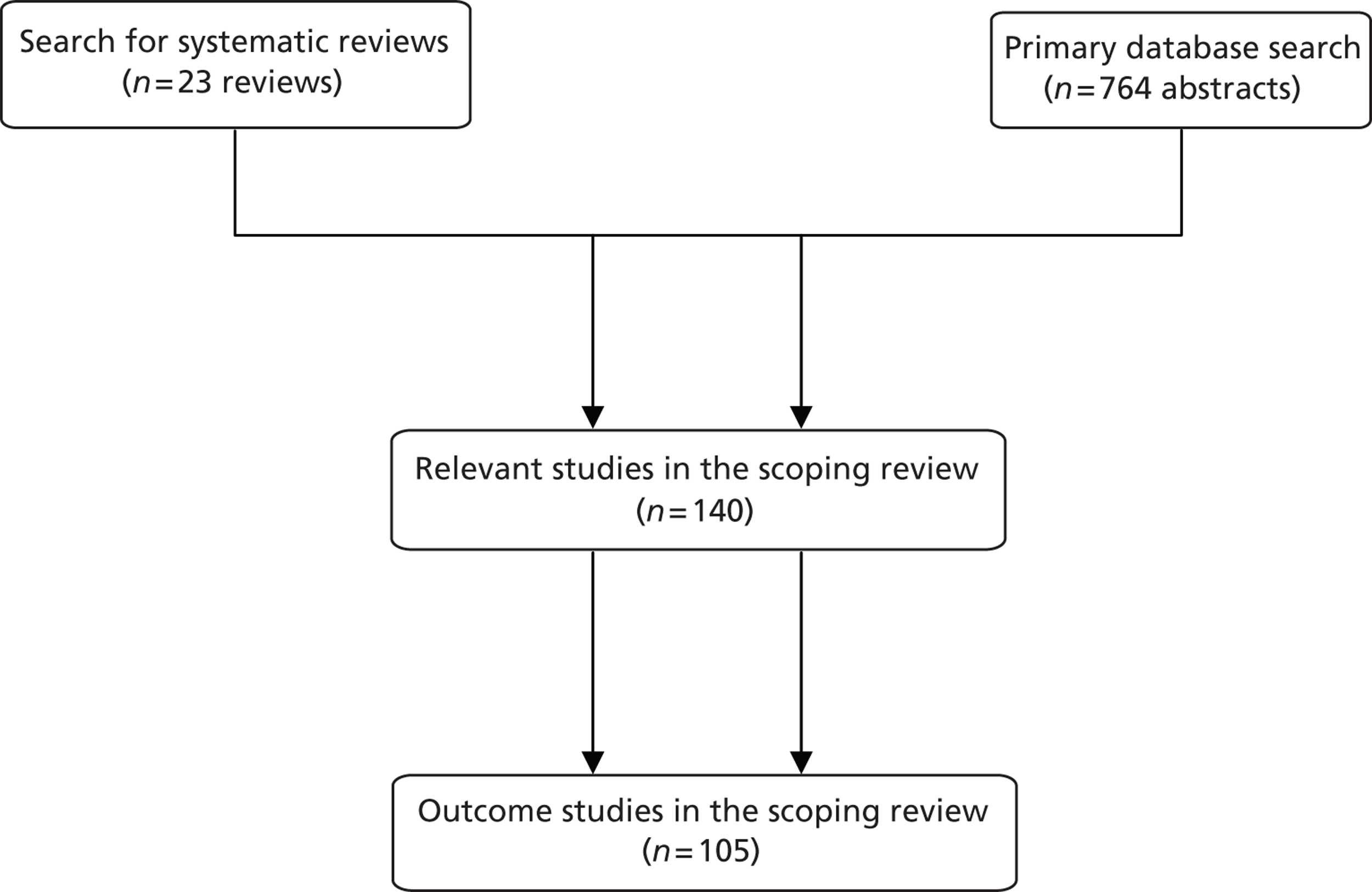
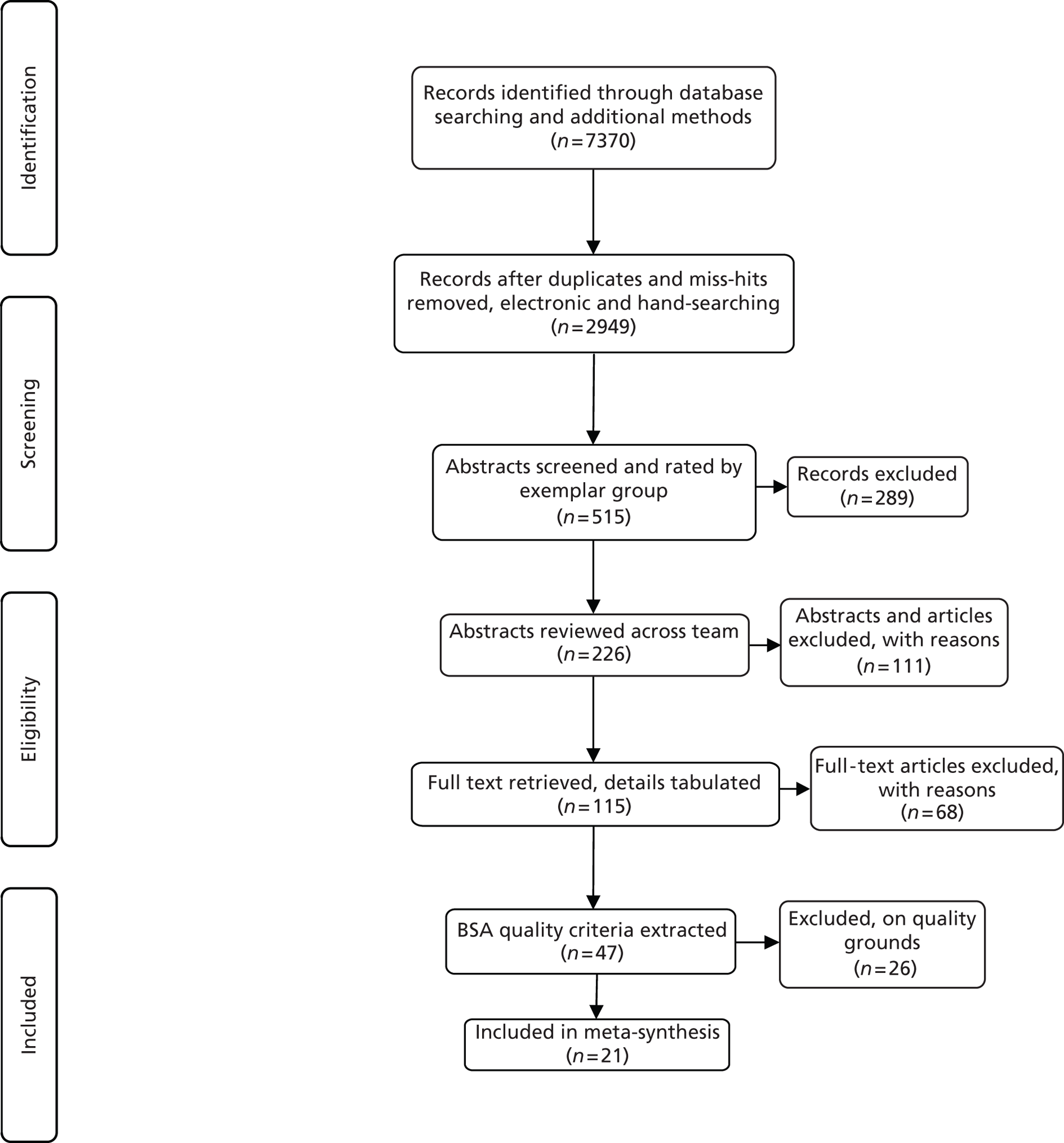
In the first search we identified 82 reviews and selected 23 as potentially relevant. 71–93 In the primary database search 764 abstracts were checked, which resulted in 105 quantitative outcome studies94–198 (some studies related to more than one exemplar group). Figure 4 shows the flow of studies through the review process.
FIGURE 4.
Flow of studies through the review process.
Interventions were categorised as:
-
application of existing mental health interventions in exemplar groups
-
modification of existing interventions to make them more acceptable to exemplar groups
-
access innovations, that is, interventions designed to increase the number of patients from exemplar groups receiving care.
Some interventions involved more than one category or more than one exemplar group, for example an intervention designed to deliver an existing psychological therapy, which was delivered using an innovative method, or an intervention delivered to elderly ethnic minorities. Examples of access interventions are provided in Table 1.
| Study | Intervention | Process intervention is designed to affect |
|---|---|---|
| Bhugra and Hicks105 | Educational pamphlet to influence help-seeking attitudes in South Asian women | Candidacy |
| Michael et al.156 | Community health workers (CHWs) used popular education to identify and address health disparities in Latino and African American communities in a metropolitan area in the USA. CHWs met regularly with community members to identify health needs and rank intervention priorities | Candidacy, navigation, receipts |
| Cornelius et al.122 | 24-hour crisis management hotline with a mobile support team and a residential care unit to reach indigent, urban African Americans. Service provides 24-hour crisis intervention and seeks to reduce the financial and social barriers to access | All |
| McCusker et al.153 | A two-stage (screening and nursing assessment) intervention for older patients in the emergency department (ED) who are at increased risk of functional decline. Patients aged ≥ 65 years expected to be released from the ED to the community with a score of ≥ 2 on the screening tool were identified. The intervention consisted of disclosure of results of the screen, a brief standardised nursing assessment in the ED, notification of the primary care physician and home-care providers, and other referrals as needed | Adjudication and offer |
| White et al.193 | Older adults were provided with internet access and received 9 hours of small-group training in six sessions over 2 weeks. Computers were available for continued use over 5 months and the trainer was available 2 hours per week for questions | Candidacy and navigation |
| Eisses et al.127 | Many people with depression in residential care homes for the elderly do not receive treatment because their depression remains undetected. The intervention consisted of a training programme for staff and collaborative evaluation by staff and a mental health specialist of residents with possible depression | Adjudication and offer |
| Slesnick et al.181 | Case management and individual therapy offered through a drop-in centre for homeless youth on substance use, mental health, housing, education, employment and medical care utilisation | Candidacy, navigation, receipts |
| Boiko et al.111 | Audiotaped survey developed for those with low literacy levels. Subjects from 11 migrant camps completed a self-administered audiotaped survey in Spanish to diagnose major depression, substance abuse, panic and generalised anxiety, and domestic violence. Primary care clinics assisted in finding camps and provided follow-up treatment | Candidacy, navigation, receipts |
Summary of evidence
Here we summarise the evidence from the scoping review, with reference to each of our eight exemplar groups.
Medically unexplained symptoms
There was inconsistent evidence concerning the effectiveness of training primary care providers to manage medically unexplained symptoms. Only one study showed a positive outcome184 and four reported no effect of training on patient outcomes. 99,145,162,173 Trials of collaborative care models reported benefits,150,188 as did trials of different types of psychological therapy [cognitive–behavioural therapy (CBT, reflecting interviews)]. 114,118,129,169
Advanced cancer
There was evidence that patients with advanced cancer could benefit from collaborative care models128,143 and from psychological therapy. 157,182
Ethnic minorities
There was reasonable evidence that ethnic minority patients could benefit from conventional psychological treatments and those modified for use with these groups. 94,101,104,112,116,117,131,132,142,157,158,161,170 There was limited evidence that training primary care providers in communication skills was effective in ethnic minority patients197 and that simple educational interventions were associated with benefits. 105,139 There was evidence that conventional collaborative care interventions were effective in improving mental health outcomes in ethnic minority patients. 125,128,159,160,192 There was some evidence that community outreach impacted on mental health outcomes. 103,156
Older people
There was reasonable evidence that a number of forms of psychological therapy (including CBT, reminiscence therapy, life review)96,102,119,134,157,195,198 and minimal psychological interventions (self-help, internet access, telemonitoring) could improve outcomes in older people. 106,135,140,143,144,175,176,185,193
Homeless people
There was some evidence that various forms of psychological treatment were effective in improving outcomes in homeless patients. CBT and supportive therapy were effective in reducing depression in women at a homeless shelter,131 whereas case management and individual therapy were effective in improving mental health, substance abuse and access to housing in homeless youths at an urban drop-in centre. 181 Other effective interventions were nursing interventions,186 psychiatric rehabilitation in street-dwelling individuals with psychiatric disorders177 and psychological therapy in cocaine-addicted homeless people. 146
Asylum seekers
There was some evidence that various forms of psychological treatment were effective in improving outcomes in asylum seekers. Training to improve primary care consultations about pain and health education and exercises improved outcomes in immigrant patients. 149,172 CBT and exposure were effective in the management of PTSD in refugees. 166 A group psychosocial intervention for mothers displaced by war was associated with gains in terms of mother and child mental health. 126 CBT and medication were effective in the management of PTSD in refugees165 and CBT was effective in the management of PTSD and panic among refugees. 137 Home visits by school nurses and bilingual teachers reduced depression in South East Asian refugees. 132 Family support and education groups were effective in improving social support and mental health in Kosovar refugees. 191
Sickness absence
There was limited evidence that various forms of psychological treatment were effective in improving outcomes in patients with sickness absence related to mental health. A social support intervention increased levels of satisfaction and attitudes towards employment for disabled African Americans and Latinos. 101 Solution-focused therapy was no more effective than routine care in the management of sick-listed employees. 163 A worksite stress reduction programme was related to improvements in depression and reductions in sick leave. 141 A CBT programme was more effective in reducing sick leave than usual care, but only in patients on short-term sick leave. 151
Adolescents with eating disorders
There was limited evidence that adolescents with eating disorders benefited from psychological interventions. Internet-delivered interventions for eating disorders in adolescents were associated with benefits. 123,133,136,167,196 Motivational enhancement therapy increased readiness to change in eating disorders in adolescents. 124,130 Self-help interventions98,190 and school-based programmes showed preliminary evidence of benefits in the management of eating disorders in adolescents. 171,189
Conclusions
Current evidence on interventions to improve access to care suggested that many patients in underserved groups can benefit from existing interventions, either provided as they are or modified to make them more acceptable. The evidence is particularly well developed for the elderly and ethnic minorities.
At present it is not know whether modifications to interventions to make them more acceptable are associated with increases in effectiveness or in overall levels of access. Although some quantitative research on innovations in access has been carried out, the current data are very limited. This may reflect the fact that evaluating the effect of a service innovation on overall levels of access is complex and not always amenable to a conventional RCT.
Meta-synthesis of published qualitative literature
Aims
By identifying commonalities across disparate published qualitative sources, meta-synthesis works in a similar way to meta-analysis of disparate published quantitative sources in generating a more powerful level of evidence in relation to a particular issue. This qualitative review examined the experiences of and attitudes to mental health treatment of identified hard-to-reach groups in their social contexts to shed light on participants' understandings of the processes of access and their experiences of the health system.
Methods
Search terms generated from known papers and previous research were combined with a previously developed qualitative research filter (see terms 89–115 in example search strategy for MEDLINE in Appendix 3), tested and adapted to run across MEDLINE, CINAHL, EMBASE, PsycINFO, Applied Social Sciences Index and Abstracts (ASSIA) and Web of Knowledge. Databases were searched on 15 May 2008. The resulting abstracts were assessed for relevance and a subset of papers was then extracted. The British Sociological Association's quality criteria199 were used to generate a definitive set of papers for the final synthesis. Key findings were extracted to a standardised proforma and were synthesised within and across groups using the classic lines-of-argument approach proposed by Noblit and Hare. 200
Results
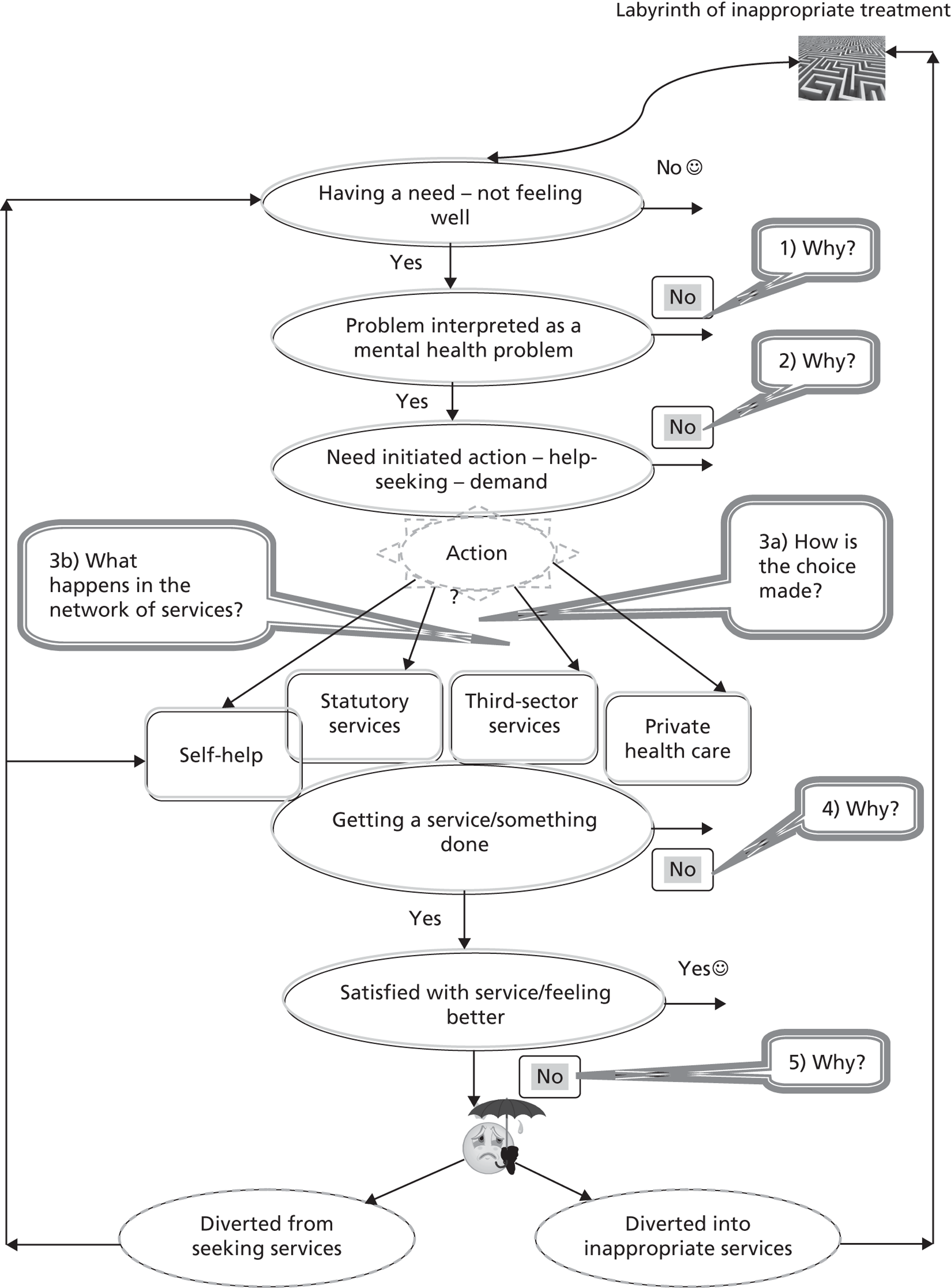
Twenty-one papers were identified as suitable for detailed analysis: two each for advanced cancer201,202 and adolescents with eating disorders,203,204 one each for homelessness205 and employment problems,206 two for older people with depression,48,207 six for medically unexplained symptoms,208–213 three for asylum seekers214–216 and four for BME communities. 29,217–219 Figure 5 shows the flow of studies through the review process.
FIGURE 5.
Flow of studies through the review process. BSA, British Sociological Association.
Summary of evidence
Details of our findings from this analysis have been published in the paper by Lamb et al. ,220 of which the key features are as follows.
Engagement in mental health treatment requires significant personal investment, including of time, material and emotional and social resources, and poses a threat to wider social identities with regard to friends, co-workers and neighbours. These investments in treatment are proportionally higher in deprived communities, where individual resources are low and the stigma attached to mental ill health is high. An understanding of these ‘costs’ by patients and GPs underlies decisions to seek and offer help, but is not explicit in the consultation.
A variety of self-management strategies are used across exemplar groups to maintain social function. These include denial, concealment, reframing and resilience. This could be functional or dysfunctional depending on circumstances. As the limits of self-management strategies are reached, patients withdraw from social networks, focusing their resources on primary roles (e.g. close family and work roles). Overinvestment in these strong bonds results in a sense of insecurity as peripheral roles in weaker networks are neglected. Withdrawal from social networks could be chosen, inflicted or circumstantial.
For example, one study illuminated how some homeless mothers had exhausted the capacity of their social networks, resulting in withdrawal and a lack of confidence in others. 205 The inevitable focus on their children and their role as mother clashed with shelter living, which deprived them of the space and resources for performing the maternal role. Women from South Asian communities could be cut off from their familial and social networks if they failed to conform to the rules and roles of those cultures or the expectations of their partner or family. 29,218
Decisions about whether or not to consult, and the appropriateness of treatment, are often based on attributions of aetiology: mind, body or social. Mind and body may be seen as secondary attributions, used when the inability to adequately perform social roles is legitimated by the sick role. Social problems relate to changes in, diminution of or incapacity to perform – or to be seen to perform – previous social roles that formed their identity.
Conclusions
The person providing the intervention has to demonstrate a willingness to achieve a comprehensive understanding of how the service user/patient views him- or herself in relation to his or her world and presenting problems to effectively engage him or her in care. However, the focus of treatment needs to be much broader, to include an emphasis on re-engagement with the wider social world and its inherent and often complex problems.
Self-help may be counterproductive in some groups as a focus on further investment within the narrow perspective of the primary role (which may be inherently dysfunctional, e.g. being an ‘anorexic’) may be unhelpful as it further isolates the person from reintegrating with the world.
People require interventions that can offer opportunities to fulfil new roles, which build on their existing strengths and help to increase confidence. A challenge of treatment is to address patients' and families' unrealistic expectations, sometimes brought about through their engagement with multiple value systems (especially in BME communities), while not posing a threat to their standing, position and safety within their community.
Depending on the nature of the problem in question, cultural and gender matching may or may not be the most appropriate option for presentation with mental health problems. The traditional ongoing GP relationship was reportedly valued. However, the ability to make informed choices and the diversity of available gatekeepers are paramount to increasing access for these groups. Respect for, and interest in, culture (wanting to find out, rather than knowing) appear to be more important than understanding, although some service users considered this to be important.
Pressure to consult in family pairs or units, and the use of family interpreters, limit opportunities for effective mental health treatment in orthodox settings such as the general practice consultation.
Dialogues with stakeholders
Aims
The aims of these dialogues were twofold. First, the intention was to establish relationships with stakeholders and enable the formation of a stakeholder steering group. Second, we wanted stakeholders to help us identify the mental health needs of our exemplar underserved groups and the extent to which primary care met these needs; and the barriers to and facilitators of, and critical components of, high-quality mental health services in primary care.
Methods
Dialogues were arranged with opinion-makers and key informants from relevant organisations, including health professionals, clinical academics, other service providers, commissioners, and service users and carers drawn from our exemplar underserved groups. Stakeholders were also invited to suggest relevant grey literature, inform the structured scoping review and suggest potential contacts for subsequent interviews with former, current and potential service users.
Potential stakeholders were identified using snowballing techniques. 221 Dialogues were conducted with individuals and groups, either by telephone or face to face. A dialogue analysis template was completed for each encounter. Each stakeholder was sent a draft copy of their dialogue analysis for any amendments and additions. Each completed document was then analysed using a thematic analysis template. Each analyst identified overarching and common themes within exemplar groups and noted synergies and differences between groups. Finally, we produced a parallel thematic analysis that portrayed the emerging themes identified by each analyst and developed a synthesis of findings with recommended interventions and approaches to improving access.
Results
We established a database of 327 stakeholders, including service commissioners, service providers, clinical academics and representatives of exemplar groups from key user and carer organisations.
We conducted 53 dialogues with stakeholders purposively sampled from across the range of exemplar groups, as indicated in Table 2.
| Exemplar group | Total |
|---|---|
| Adults with advanced cancer | 6 (7)a |
| Adolescents with eating disorders | 7 |
| Adult asylum seekers | 8 |
| Adults from BME communities | 11 |
| Elders with depression | 3 |
| Adults with employment problems | 2 |
| Homeless adults | 4 |
| Adults with medically unexplained symptoms | (1) |
| General | 12 |
| Total | 53 |
Summary of evidence
To increase equity of access to high-quality mental health services in primary care, stakeholders saw a need to make changes at both the systemic and service level.
They considered that systems, such as national and local policy and commissioning organisations, should be both dynamic and fair:
-
dynamic aspects included setting realistic targets, introducing incentives, for example through the QOF, requiring patient profiling to monitor progress, investing in more mental health primary care staff, and training and accrediting refugee GPs
-
fairness includes the provision of continuous funding for effective and valued services, ensuring that decisions on funding for services are transparent and justified; and paying for necessary services that health centres cannot provide.
They thought that services, especially primary care health centres, should be communicative, flexible, holistic, integral, positive, proactive and responsive:
-
Communication should involve a diverse range of communication methods; being approachable and demonstrating interest in patients by dropping – or at least lowering – professional boundaries; publicising to communities and potential patients that mental health services are available in and though primary care; demystifying the system for potential patients; informing patients about the mental health services available and how to access them; providing potential patients with information and education on mental health issues; increasing and improving links with other local services and resources, including employers, transport providers and community organisations; and seeking information and sharing information with patients on local and national mental health services and resources.
-
Flexibility could involve providing drop-in facilities for patients; radically overhauling appointment systems; the use of appointment reminders; and encouraging self-referral for therapeutic interventions.
-
Holism would be encouraged by responding appropriately to the complexity of people's lives; working with what service users think they need to do to improve their mental well-being; making services and interventions meaningful to potential patients; demedicalising distress; and recognising that diagnoses are not always helpful or relevant.
-
Integration would be enabled by identifying and working closely with local community groups and services; earning the trust of local communities; and encouraging the community to realise that it owns its health centre.
-
Positive attitudes would be fostered by providing welcoming settings; encouraging positive staff attitudes towards patients with emotional needs; recruiting staff who want to work with marginalised groups with emotional needs and providing them with extra support; ensuring that services are accepting of all, non-judgemental and antidiscriminatory; empowering patients and helping them to feel better about themselves when they leave – so that they return; increasing expectations of mental well-being among marginalised groups; and destigmatising distress through mental health promotion.
-
Proactivity would be enhanced by engaging in outreach work and ‘coaching’ and motivating patients; profiling patients and monitoring progress; and aiming to exceed targets.
-
Responsiveness involves offering creative and diverse interventions for service users that are effective and valued; learning from service users, specialist organisations and advisory bodies, and adapting and introducing services accordingly; facilitating user-led and -involved mutual support services; adapting systems around the needs and cultures of the local population; providing interpreters and translated information to patients; offering women-only services; and appointing more diverse staff.
Grey literature
Aim
The aim of the grey literature review was to find out what mental health services, of relevance to primary care, were currently available, planned or potentially accessible for members of underserved groups, primarily across the north-west of England, in the NHS and third-sector settings.
Methods
Material was sourced in light of the range of specialist expertise available in the research team, with active attempts to identify and address gaps in coverage. Documents were gathered in a pragmatic rather than a systematic fashion and did not constitute a comprehensive collection; they were mainly statutory health sector or voluntary sector reports. Individual summaries were prepared for each document, with a focus on recommendations relevant to the eight exemplar groups and their access to mental health services. We also looked for any guidance on the design of interventions to improve access and for examples of good practice and innovation.
Results
The 118 items in our grey literature database, when dated, covered the period 1985–2008, with half from 2005–8. 222–339
Much of the literature (40%)222–269 was of general relevance across the AMP groups, with a fair coverage of issues arising for BME groups,270–288 asylum seekers289–303 and homeless people. 304–311 Relatively little was found on the specific needs of five of the groups: adolescents with eating disorders,312–329 people on prolonged sickness absence from work,330–335 people with medically unexplained symptoms,336 people with advanced cancers and older people with depression. 287,288,337–339
These gaps may indicate a lack of shared understanding or recognition of the underlying problems to be addressed by the AMP project. Although they limit the potential for this literature to provide guidance on specific interventions for the groups concerned, we noted the overall relevance of findings from ‘general’ category documents. We also emphasise in this context that individuals can and do belong to more than one AMP exemplar group.
From an interventions perspective, there was considerable variation in the extent to which recommendations could be translated into concrete actions. The literature included hardly any innovative ‘ready-made’ solutions that could be straightforwardly rolled out in different settings. When examples of good practice were given, details of content and context were often lacking. There was a general focus on problems with services, with relatively little attention paid to cases in which existing services worked well.
With these cautions in mind, the grey literature was helpful in addressing questions about the likely acceptability of AMP interventions, rather than their impact or feasibility.
Summary of evidence
We have detailed our methods and evidence in Hibbert et al. 340 Here we summarise evidence from the grey literature within three domains: conceptualising services, the experience of services, and communicating information and values.
Service models should be based on care for the individual rather than the ‘condition’ and should promote possibilities for low-intensity health and social support. 238,269 The focus should be on early detection of problems and referral as appropriate. 267,335 Stepped care was proposed as a useful model. 265 A choice of therapeutic approaches and delivery modes is needed,234,286 including CBT, talking therapies, complementary and alternative therapies and group therapies (to combat isolation). Inequity of access to these is an issue for AMP groups. Dedicated services should be provided for asylum seekers,292 adolescents with eating disorders328 and women. 222 There is a need for culture change within mental health services to enable ‘bottom-up’ service development based on meaningful consultation with communities and users/carers. 258,273 Creative community-based approaches are required and methods of reaching out to communities should not rely solely on the written word. 270,274,291 There should be better collaborative working between statutory health care, social care and the voluntary sector. 267 The importance of social factors and social support for mental health underlines a case for integrated medical and social care. 227,304 Services should address mental health alongside physical health254 and should acknowledge spiritual and faith-related needs. 223,229,280,286 Services should include and support carers and families as appropriate. 242,244,270,304,312,326 Service providers also need support.
Racism informs a landscape of mutual mistrust between mental health services and service users from BME communities. 225,276,278,284,301 Culturally sensitive and responsive services are needed. They should accommodate different (including ‘non-Western’) perspectives on mental health, the individual and the family. 289,292,297 The stigma and shame associated with mental illness act as a barrier to access and should be addressed using ‘whole-community’ approaches. 238 Services should be welcoming286 and be presented in everyday, generic ‘non-clinical’ settings. 315 Barriers to access often concern practical issues such as GP registration,235,278,299,307,309,310 waiting times for appointments,267,279,314,329,338 booking systems,244,255,269,294 travel arrangements269,310,328 and lack of child-care provision. 222,275,276,315 Greater staff diversity of services is needed, including more community-based link/gateway workers and people from service users' communities. 235,240,270,284 Advocacy services, to help people navigate their way through the system, should be developed. 270,284,291,292
Users need information on the services available and how to access them. 229,248,291 Some potential users may not be familiar with the UK health-care system. Problems with translation and interpreting services include the availability,225,279,282,293 publicity,286 booking290 and consistency of services. 274 Improvements should be informed by audit of local population needs,290,291 alongside training for interpreters (on mental health issues)276 and health professionals (on working with interpreters). 289,295,297 Further training is advocated for primary care workers,229,242,254 employers335 and job centre staff267 on the recognition and awareness of mental health problems. Gaps in health professionals' knowledge are also identified in respect of the services available locally, the refugee/migration process, the health-care entitlements of asylum seekers, power relationships and cultural competencies. 275,292,297 The governance focus should include monitoring of waiting times for psychological therapies,235,243 ethnic equality and compliance with national guidelines (such as for the treatment of people with eating disorders). 312,326 Providers should define service content in concrete terms so that users know what to expect. 263,265
Conclusions
There were significant gaps in the grey literature coverage for five of the eight AMP exemplar groups. The literature was most helpful in indicating the likely acceptability of AMP interventions. The literature did not encourage a view of interventions as easy to identify or simple to apply in everyday practical situations. Interventions should promote access to individualised and culturally appropriate care. Interventions should work to normalise ‘mental health’ and to recalibrate the boundaries between mental health, physical health and social life.
Secondary analysis of qualitative data sets
Aim
The aim of this study was to gather evidence from service users about key issues arising from the scoping review in relation to access to primary care mental health services. This analysis was complementary to the meta-synthesis (see Meta-synthesis of published qualitative literature) in that it allowed access to existing qualitative data (the full text of interview transcripts) rather than the published findings of qualitative studies with only illustrative material presented.
Methods
Qualitative studies contributing data for secondary analysis were sampled by convenience and selected according to the team's judgement on their relevance to our research objectives.
Data comprised anonymised transcripts of semistructured and in-depth interviews with white British, black Caribbean and South Asian adult residents of north-west England. The interviews were conducted within seven different qualitative studies (one unpublished) during a period from 2001 to 2007 (Table 3). 47,48,219,341–343
| Study | Exemplar ‘hard-to-reach’ group | Year of data collection |
|---|---|---|
| Reeve et al.341 | People with advanced cancer | 2004–5 |
| Gask et al.342 | People from BME (South Asian) groups | 2007 |
| Edwards and Gabbay343 | People with risk of long-term unemployment | 2001–2 |
| Chew-Graham et al.48 | Older people with depression | 2005–6 |
| Chew-Graham et al. (unpublished data) | Older people with depression | 2007 |
| Edge and Rogers219 | People from BME (back Caribbean) groups | 2001–2 |
| Peters et al.47 | People with medically unexplained symptoms | 2004–5 |
As the original studies were designed to answer various research questions related to common mental health problems and mental well-being, transcripts that were judged by the primary researcher as irrelevant with regard to our interest in exploring access were discarded after discussion. The next step was a random selection of transcripts from each data set.
Out of the 111 transcripts of the original studies, 19 were discarded as they contained no relevant discussion and 92 were retained. Random selection of transcripts from each data set resulted in 33 transcripts being selected for initial comparative analysis with the remainder available for triangulation.
The process of secondary analysis was based on the methods described by May et al. 344 Initial analysis using a new conceptual framework345 (Figure 6) was conducted by the secondary researcher, who was naive to the original research findings. Initial findings were validated by reanalysis by or analytical comments from primary researchers. The next step was cumulative comparative analysis in which the initial findings could be complemented by additional theoretical sampling from the larger data set. Final summaries of findings for each study were sent to primary researchers for validation. Finally, a condition comparative analysis considered similarities and differences between findings for each study group. The overall approach to analysis was embedded in the interpretative research paradigm with orientation towards narrative and case study approaches.
FIGURE 6.
Analytical model: a heuristic for researching access to primary mental health care. 345 Reprinted from Social Science & Medicine, Vol. 72, by Kovandžić M, Chew-Graham C, Reeve J, Edwards S, Peters S, Edge D, et al. Access to primary mental health care for hard-to-reach groups: from ‘silent suffering’ to ‘making it work’, 763–72, 2011, with permission from Elsevier.
Summary of evidence
We have published the main findings on commonalities between groups in a paper by Kovandžić et al. 345 and some of the findings related to specific groups included in this study in a paper by Chew-Graham et al. 346 Here we outline the main findings, illustrated with some quotations from the data. Our analysis points to an extensive overlap in access-related issues across the observed groups, along with some particularities. The analysis confirms the hypothesised existence of five ways in which problems of access to primary mental health care are clustered across the analysed groups (see Figure 6). Reflecting the ‘taste of data’ we named these clusters as (1) ‘silent suffering’, (2) ‘in between suffering, coping and seeking help’, (3) ‘navigating networks of services’, (4) ‘negotiating acceptable treatment’ and (5) ‘making it work’.
-
‘Silent suffering’ is characterised by participants' descriptions of periods of psychological distress that were not formulated into mental health problems.
-
Even if suffering is formulated in ways that could lead to formal help-seeking in primary care, people may hesitate to do so. As one older person said:
Honestly GPs are hopeless. In my opinion GPs don't know mental health.
-
Once the attempt of placing demand is enacted, it is still not certain that the relevant health professional will be reached. Here is an example of the problems experienced by a patient with medically unexplained symptoms:
So I rang up after a fortnight and I asked the receptionist for an appointment to see Dr [. . .] regarding my knee, the results of my knee. She said ‘I can tell you Mr [. . .], there's nothing wrong with your knee’. So this is the receptionist. I said ‘Excuse me but have you become a doctor over night?’ I said ‘I know there's something wrong with my knee, you don't need to tell me, what do you think I'm coming to the doctors for’. So that was the time I decided to go private.
-
Access to effective and acceptable help is not guaranteed even if a person actually gains access to a relevant health professional. This domain of the problems of access relates mostly to the concept of concordance,347 but also to availability of choices.
-
Even if access to treatment is fully gained, the work of recursivity identified earlier implies the need to look at the factors influencing satisfaction with the quality and personal perceptions of the effectiveness of treatment to secure future access. A South Asian woman described this process as follows:
If you were here and I was depressed, severely depressed where I wasn't on medication and I was going completely mental I would be sitting here so quiet that you would have to do all the talking [. . .]. But now [after taking medication] I've come to a point where I'm getting my confidence back where I can approach people or talk to people freely and not hesitate so that would help [joining a therapy group].
Conclusions
Regardless of some particularities, there is an extensive overlap in access-related issues across the underserved groups. The main barriers to improving equity of access to primary mental health care could be formulated as multiplied stigma and related lack of effective information. Even if these barriers did not exist, access would remain problematic for underserved groups unless available services were more acceptable and ‘in tune’ with their needs and preferences. Our analysis indicates that developing acceptable services is the main facilitator of equitable access. To achieve this the services need to be pluralistic, adaptive, holistic, resonant with users' needs and socially conscious.
Interviews with (potential) service users
Aim
The aim of this study was to continue the process of gathering evidence from service users and carers about key issues in relation to access, focusing on members of underserved groups for whom adequate evidence was not available from the meta-synthesis of published qualitative literature or from the analysis of existing qualitative data sets. We have published the main findings from this study in a paper by Bristow et al. 348
Methods
This study therefore sought interviews with service users and carers from five BME communities (South Asian, Irish, Chinese, Somali and Polish) and with asylum seekers, homeless people and adolescents with eating disorders. Recruitment started with flyers (see example in Appendix 4) displayed at locations such as libraries and community organisations across Liverpool and Manchester, where members of our target groups would be likely to attend. The interviews were conducted at locations convenient to the participants; usually this was in office space provided by the recruiting organisation, but on occasion interviews took place in a participant's own home. Interpreting was facilitated by M-Four Translations, at Manchester City Council.
The interviews were semistructured, with a topic guide developed with reference to the scoping review and the heuristic of access presented in Figure 6. All of the interviews were audio recorded and transcribed verbatim.
Transcripts were analysed on a case-by-case basis, focusing on the ways in which the participants understood their emotional health and well-being; their attitudes towards help-seeking for emotional distress; and their experiences if they had tried to access mental health services. A comparative case analysis within the exemplary groups identified group-specific themes. A further comparative case analysis across the complete data set identified overarching themes. Ethical approval for this aspect of the programme was given by Wrightington, Wigan and Leigh Research Ethics Committee (reference 08/H1014/39).
Results
The number of participants for each exemplar group is presented in Table 4.
| Exemplar group | Target, n | Actual, n | Included in analysis, n |
|---|---|---|---|
| BME – South Asian | 5 | 5 | 2 |
| BME – Irish | 5 | 5 | 3 |
| BME – Polish | 5 | 1 | 1 |
| BME – Chinese | 5 | 6 | 6 |
| BME – Somali | 5 | 3 | 2 |
| Asylum seekers | 5 | 5 | 2 |
| Homeless people | 5 | 6 | 4 |
| Adolescents with eating disorders | 5 | 5 | 5 |
| Total | 40 | 36 | 25 |
Summary of evidence
Our findings supported those from the secondary analysis of qualitative data sets (see Secondary analysis of qualitative data sets) and provided some further elucidation of ways in which problems of access to primary mental health care are clustered.
This was reported in terms of sensations of isolation and loneliness, feeling abandoned and difficulties with communication. Self-help strategies to relieve distress or unhappiness included seeking company or social withdrawal. Symptoms of illness were understood in terms of pain and somatisation, life being sometimes up and sometimes down, and problems building up over time. We noted stigma in terms of emotional issues often being considered personal and private, and the impact of cultural and family values.
Respondents described crises as tipping points, with the person involved not always understanding what was happening. There was a lack of knowledge about available services, with the perception that GPs treat only the physical or that no one can help. We noted perceived stigma in terms of concerns about the consequences of a mental health diagnosis and treatment, and an assumed lack of compassion and understanding from health- and social-care professionals.
Respondents proposed wider, social models of care. They valued informal support networks. They were concerned about communication, reporting that GPs were often too busy to listen. They felt that there was a lack of trust and inadequate signposting about services.
Potential service users thought that GPs should have an interest and training in mental health issues. They said that GPs should be knowledgeable about services and willing to advocate for patients' access to them.
Respondents emphasised the importance of continuity of care and the need to educate people about how to deal with their emotions. They proposed more community groups, including drop-in centres where you have ‘time to speak, and be happy and enjoy’. They recommended more coherence and communication between health and social agencies. They also recommended a wide range of activities supportive of emotional health including gyms and health centres – ‘stress busting’; workshops in creative writing, photography, arts/crafts and gardening; educational support and skill development; confidence-building workshops; and complementary and alternative therapies.
Synthesising evidence
We synthesised the evidence gained from these multiple and diverse sources using a consensus process349 to develop candidate interventions that would take account of known barriers while remaining sensitive to the needs, preferences and priorities of our exemplar hard-to-access groups and other stakeholders. We focused on mental health-related services that have the potential to be commissioned by PCTs, including those delivered by non-statutory organisations.
Our synthesis of these sources of evidence produced key emergent findings, including:
-
ways in which (mental) health problems are formulated by people from underserved groups
-
risks attached to engaging with mental health interventions offered through primary care
-
limitations in access to existing psychosocial interventions and
-
better understanding of the dimensions of access.
Problem formulation
Problem formulation by people from hard-to reach groups is often very different from health professionals' perspectives. The concept of ‘embodied suffering’ is useful, because it encompasses both the close linkage between psychological symptoms and physical symptoms, and also the view that psychological symptoms cannot be dissociated from adverse lived experiences. The concept of ‘double stigma’ highlights the fact that members of marginalised groups who also have mental health problems may face compounding sources of stigma and discrimination. 340,346 People from these groups may view their problems through specific cultural or religious lenses, for example the need to be a ‘strong black woman’ or the belief that problems are a test of faith.
Risks and benefits of engagement
Interventions commonly regarded by health-care professionals as beneficial may involve risk for people from underserved groups. Emphasis on self-management may lead to concealment of symptoms, identification with dysfunctional peer groups or withdrawal into core social roles. Conversely, engagement with health services requires considerable personal investment of time and emotional and social resources, and poses threats to wider social identities including friends, co-workers and neighbours; these problems can be particularly salient in deprived communities where external resources are low and levels of stigma may be high. Engagement with services may also inhibit recovery if it reinforces responses that confirm illness identity. 220
Our evidence pointed towards a need for the development of resources for self-help, coping skills and resilience, designed to help members of underserved communities improve their mental well-being without direct primary care involvement. Initial consultations indicated that this was highly congruent with current priorities in both Liverpool and Manchester and in wider health policy. Once the limits of self-efficacy and self-management are reached, primary care should have the capability and capacity to deliver effective and appropriate treatment. However, members of underserved groups are less likely to recognise the need for treatment, or to identify primary care as the place to seek treatment. They are also less likely to perceive the treatment that they are offered or receive as appropriate to their needs. There is a need to reduce the stigma of mental ill health by allowing communities to reframe mental health problems in their own terms, and to influence the delivery of primary health care.
Psychosocial interventions
Evidence of efficacy for psychosocial interventions to alleviate common mental health problems was consistent for older people and reasonable for asylum seekers, homeless people and those from BME communities. However, evidence of efficacy was limited for adolescents with eating disorders, those with employment-related mental health problems and people with advanced cancers; and it was inconsistent for people with medically unexplained symptoms. Strategies aimed at increasing access to such interventions include enhancing candidacy, navigation, adjudication and technology, but evidence for their effectiveness is scanty.
We considered it unnecessary to reinvent the wheel with regard to the core content of effective psychosocial interventions, which are based on increasing involvement in positive or rewarding activities, learning to recognise and challenge exaggerated negative and self-critical thoughts and developing more effective problem-solving strategies. Nevertheless, there was a clear need to present the content in ways that are culturally acceptable, address physical difficulties and decrease social isolation. It was also important to incorporate users' own explanatory models, language and metaphors. Interventions needed to be available in a number of delivery modes, including individual and group, with support from health professionals using telephone, face-to-face or e-mail contact, and in both practice and community settings. Organisations and health professionals needed to promote antidiscriminatory attitudes and behaviours to increase access to interventions.
Dimensions of access
Access is a complex concept. As we noted in our conceptual scoping review (see Structured scoping review of published quantitative literature), help-seeking and access to care for mental health problems are often characterised by uncertainty. We have considered the key concepts of candidacy, identity and morality, graduated access, adjudication and cultural competence.
Intervening to improve access requires an understanding of the process by which access is achieved. Process-orientated models of access identify different stages of access (e.g. system entry, repeat use, adherence and outcome) and differentiate between ‘access entry’ (i.e. entering the care system) and ‘in-system access’ (i.e. access once in the system).
Generating solutions
Our procedures for generating the candidate interventions involved a series of interactions between the research team and local stakeholders, actual and potential service users from our exemplar groups and a panel of national and international academic experts in the field of primary care mental health (see Figure 2).
-
We began this process with a tightly structured day-long workshop for the entire AMP research team at which we considered the totality of evidence generated from the various sources indicated earlier and used facilitated small-group techniques to generate an initial ‘long list’ of candidate interventions.
-
We then produced a working document as a basis for consulting with the wider health-care community. This document proposed a set of linked interventions in three domains:
-
enhanced community engagement, to raise awareness of the potential benefits of interaction with primary care
-
increased sensitivity of primary care teams to the mental health needs of people from hard-to-reach groups
-
the design and implementation of a range of sensitised psychosocial interventions.
-
-
Members of our stakeholder group and our panel of experts were invited to comment on the working document, using an electronic proforma.
-
The research team then formed into three subgroups to work up detailed proposals for each of the proposed domains, taking account of service user, stakeholder and expert comments. We then integrated the working groups' reports into a single document.
-
We invited our panel of experts to subject the detailed integrated proposal to a formal peer-review process and, in parallel, held a series of consultations with service users and primary care teams to gather views on the utility and acceptability of the proposal.
-
Finally, we submitted the full proposal for formal ethical review.
To illustrate how these processes have worked, we describe how we focused our intervention strategy on specific hard-to-reach groups – older people and people from BME communities who are experiencing depression, anxiety or medically unexplained symptoms – and why we chose particular sorts of interventions.
Our starting point was to target groups who are least likely to access primary care (such as BME communities) and those who received suboptimal care if they do obtain access (such as older people). Our scoping review of psychosocial interventions identified the largest number of positive outcome studies in these two groups. Findings from our meta-synthesis and our secondary analysis highlighted differing ways in which mental health problems may be expressed, with a strong emphasis on physical manifestations of suffering; hence, we realised the importance of including physical symptoms. We received convergent advice from our local stakeholders, panel of experts and participating PCTs that older people and BME groups should be given highest priority.
As an example of the processes we employed, the rationale for our choice of the form and content of psychosocial interventions to be tested is derived from a synthesis of our multiple sources of evidence, including our programme team meetings. This is summarised in Table 5.
| Source of evidence | Findings |
|---|---|
| Scoping review | |
| How to make the intervention accessible? | People can benefit from existing interventions |
| Evidence base | Consistent evidence that older people could benefit from various psychological treatments, especially those with a CBT base; and evidence that modified psychological treatments may be effective for people from BME groups |
| Qualitative review: meta-synthesis | |
| How to make the intervention acceptable? | Re-engagement with the wider social world; use of diagnostic labels may be counterproductive; build on current strengths; respect and interest in culture |
| How to make the intervention accessible? | Information to make informed choices |
| Service considerations | Willingness by health professionals to understand service users' views of themselves |
| Stakeholder perspectives | |
| How to make the intervention acceptable? | Communicative, flexible, holistic, integral, positive, proactive, responsive |
| Grey literature | |
| How to make the intervention acceptable? | Focus on the individual not the condition; culturally appropriate; interventions should work to normalise mental health and recalibrate the boundaries between mental health, physical health and social life |
| How to make the intervention accessible? | Reaching out to the community; collaborative working; users need information on how to access services |
| Who should be involved in the delivery? | Advocacy to help people navigate their way through the service |
| Service considerations | Low intensity and social support; services should be bottom up |
| Secondary analysis of qualitative data | |
| How to make the intervention acceptable? | Pluralistic, adaptive, holistic, resonant and socially conscious; somatisation of mental suffering; cultural sensitivity; use of metaphors and individuals' explanatory models |
| How to make the intervention accessible? | Stigma prevents access and help-seeking |
| Service considerations | Social deprivation and isolation; improving availability and reachability; understanding and improving experiences and expectations of care |
| Service user perspectives | |
| How to make the intervention acceptable? | Isolation and loneliness; decreasing stigma |
| How to make the intervention accessible? | Lack of knowledge about available services |
| Service considerations | Lack of compassion and communication from health professionals |
| Conclusions drawn on synthesis day | |
| How to make the intervention acceptable? | Working with patients' explanatory models; focus on both psychological issues and social issues |
| How to make the intervention accessible? | Signposting to relevant services; culturally acceptable; variable site delivery; multidelivery system |
| Evidence base | Evidence-based psychological interventions |
| Who should be involved in the delivery? | Community ‘champions’; understanding of local services and referral criteria; peer led and professional led |
This summary of evidence shows how stakeholders, service users and the qualitative literature all emphasised the need for health-care organisations and health professionals to promote antidiscriminatory attitudes and behaviours. Reviewing the different sources of evidence about increasing access to interventions, we found that the content of psychosocial interventions needs to be presented in ways that are culturally acceptable, that adjust for physical difficulties and that decrease social isolation. It also became clear from the meta-synthesis, the secondary analysis and the stakeholder perspectives that there is a need to incorporate service users' own explanatory models, language and metaphors within the psychosocial interventions. Stakeholder and service user perspectives indicated that the interventions should be available in a number of delivery modes and in both health-care and community settings. 350 None of these sources on their own would have provided sufficient information to allow a credible range of psychosocial interventions to be developed.
Discussion
The AMP programme is designed to generate knowledge and capacity to increase equity of access to high-quality mental health services in primary care. The first steps to achieving this are to find out what high-quality services exist and what the barriers and facilitators are to their successful implementation for people from underserved groups. In this chapter we have explained how and why we gathered and then synthesised evidence from multiple sources to understand the problems and generate potential solutions.
Strengths and limitations
The major strength of our methodological approach was that it enabled us to answer a set of important questions that could not adequately be addressed by simpler or more conventional means. No single source of evidence would have been sufficient. The scoping review could tell us what psychosocial interventions worked for which groups of people, but not how or why they worked nor, importantly, how such interventions might be better accessed. The grey literature review and stakeholder interviews could tell us what services are available or planned, but not what potential service users thought about them. The meta-synthesis and secondary analysis could tell us about actual and potential service users' views on the formulation of mental health problems and on the services that might meet their needs, but were restricted by the issues that the original research sought to address. The interviews with actual and potential service users then enabled us to fill gaps in knowledge. Finally, our processes of evidence synthesis and refinement, involving several iterations between the AMP team, stakeholders, service users and external experts, were focused towards the development of an acceptable and credible intervention strategy.
Such a complex approach to evidence gathering and synthesis does also have its limitations. First, our aim to examine the needs of a wide range of hard-to-access groups, within and among which there is considerable diversity of demands and expectations, has an inherent tendency to generate solutions that are generic rather than specific. Second, it was not possible for all of the objectives of all of our evidence-gathering strands to be fully realised; our grey literature review, for example, was limited by the willingness of service providers to respond to our requests; and our access to interviews with Polish service users was more limited than anticipated. We are also aware that data collection methods such as snowballing (see Dialogues with stakeholders) may be prone to bias. Third, there remains the risk that, despite all of the external advice and review procedures built into this process, the perspectives and prejudices of the research team may have exerted undue influence on the conclusions and consequent outcomes.
Conclusions
We believe that our comprehensive approach to evidence gathering and synthesis is innovative in the field of health care. Although other research groups have successfully synthesised quantitative and qualitative research evidence,351 and incorporated consensus procedures to identify key interventions,352 we are not aware of previous examples of research teams including stakeholder and service user perspectives within the intervention development stage in the integrated, synergistic manner achieved here. Our experiences may, therefore, be of interest to others planning innovative, research-based complex interventions in health care.
We already have a good understanding of what works in primary care mental health services for the general population. The AMP programme has developed a set of methods which link that knowledge with what is known about barriers to access for underserved groups, integrating scientific understanding with the perspectives of stakeholders and service users and carers, to propose creative new ways to meet the needs of members of these groups.
Our programme brings together previously separate streams of research and development activity. In so doing it reduces duplication of effort and enables synergies. Lessons can thus more readily be learned about effective research and clinical methods and their dissemination into routine practice.
Access effects are not readily amenable to conventional trial designs because those designs generally take a population of patients accessing care and randomise them between different services, assessing average effectiveness and cost-effectiveness in those who have already agreed to receipt of services. Assessments of ‘minimal interventions’ (such as self-help and computerised self-help treatments) and suchlike, which demonstrate that less resource-intensive services can achieve equivalent clinical outcomes,353 imply potential benefits for access because more effective treatments can be provided from equivalent resources. However, the potential to achieve greater population access to care is not formally tested, and the cost per outcome benefits found in the population of patients accessing care may not scale up to those in the wider population.
A rigorous assessment of the effect of an access intervention would involve an assessment of mental health care in a population of patients before and after the introduction of an access intervention compared with a population who did not receive the intervention. Outcome assessment would involve calculation of the proportion of a target population who successfully negotiate the stages of access to receive appropriate high-quality care, the distribution of care according to need and the effectiveness of that care. Although there are examples in the literature that attempt to apply this design34,354,355 and methods that might be able to accommodate it,356 we did not locate any studies that provided a comprehensive assessment of access, equity and effectiveness. It is likely that exploration of these issues will require mixed-methods research combined with enhanced use of routinely collected data from public health and provider sources and creative use of comparators for intervention sites. 44,357 Such an approach should enable an adequate assessment of whether or not this comprehensive approach to service redesign improves access to primary care mental health services.
The next step for our team was to use this synthesis of multiple sources of existing information in planning the range of interventions that would be implemented and evaluated in phase II of the AMP programme. The following chapter explains how we did this.
Chapter 3 The AMP Development Partnership
Introduction
In response to our synthesis of evidence, linked to the findings from our methods for generating potential solutions – as described in the previous chapter – we considered it essential to address three distinct but overlapping domains:
-
the world beyond primary care, to address the processes that occur before service contact (candidacy and navigation)
-
the interface with primary care, to address the process by which services and patients agree on appropriate access to care (appearance, categorisation, adjudication, offer and recursivity)
-
the acceptability of interventions available in that setting and the likelihood that they will be attended and used as expected (receipt). 348
We therefore proposed a new multifaceted model, designed to improve access to primary care mental health services for people from underserved communities. The model is presented in Figure 7. The three core components of the model are:
-
Community engagement. Community engagement provides the opportunity to improve well-being and access for individuals and the resourcefulness of a system as a whole. It aims to meet local needs and presents an opportunity for reclamation of identity and agency, and includes the option of improved access to sensitised primary care services.
-
Primary care quality. To improve the quality of the patient experience when members of hard-to reach groups access primary care, primary care teams need to increase their competence in understanding and responding to the differing ways in which members of underserved groups present suffering and in encouraging them to access relevant services.
-
Psychosocial interventions. There is evidence for the effectiveness of psychosocial interventions for many underserved groups. Interventions must be tailored to meet the personal and communal needs of those who may benefit from them.
FIGURE 7.
Multifaceted model of care.

We deployed this model to create the AMP Development Partnership, within which the AMP team sought to work with community, practice and policy ‘champions’ to generate self-sustaining change at a neighbourhood level.
The three aims of the partnership were to:
-
increase equity of access to mental health services through primary care
-
improve the quality and responsiveness of those services
-
test the hypothesis that these changes can best be achieved by delivery of a new complex intervention.
As we explained in the previous chapter (see Generating solutions), in this phase of the AMP programme we decided to focus our attention on two underserved groups: elders and people from BME communities.
Intervention sites
In concordance with initiatives from our collaborating PCTs, we used a locality-based approach to deliver our interventions. We implemented and evaluated interventions in four localities, selected on the basis of the following criteria:
-
City: two localities in Liverpool and two in Manchester.
-
Population size: each locality had a population in the region of 25,000, currently considered as the optimum size for delivering the full range of integrated primary care services.
-
Range of exemplar groups: we needed to ensure access to as many of our exemplar groups as possible while working to promote existing PCT and Department of Health priorities in relation to the mental health of older people and BME communities.
-
The Index of Multiple Deprivation (IMD) 2007 (the Department for Communities and Local Government commissioned the Social Disadvantage Research Centre at the University of Oxford to produce the IMD): this is a local area-level measure of deprivation, with overall scores calculated from seven domain indices for income, employment, health, education, barriers to housing and services, crime, and living environment. Lower-layer super output areas (SOAs) are geographical entities introduced after the 2001 census. They contain an average of 1500 residents.
We focused on four specific localities. In each city one locality would enable involvement of ethnically diverse and economically deprived local communities. The other would involve more homogeneous communities in terms of people belonging to the ethnic majority, but they were equally disadvantaged in terms of higher than average employment insecurity and prevalence of chronic diseases.
The two Liverpool localities were Croxteth and Norris Green and Picton and Granby (Figure 8). Croxteth and Norris Green (wards 10 and 18 on Figure 8) are predominantly white British neighbourhoods, which in recent years have become synonymous in the public's view with gang violence. The PCT report that there are high levels of deprivation and worklessness in this area. According to standardised mortality rates (pooled by gender and age) for all wards in Liverpool, Croxteth is in the most deprived quintile for circulatory diseases and Norris Green is in the most deprived quintile for all cancers. 358 Henceforth, we refer to this locality as Croxteth.
FIGURE 8.
Liverpool intervention localities.
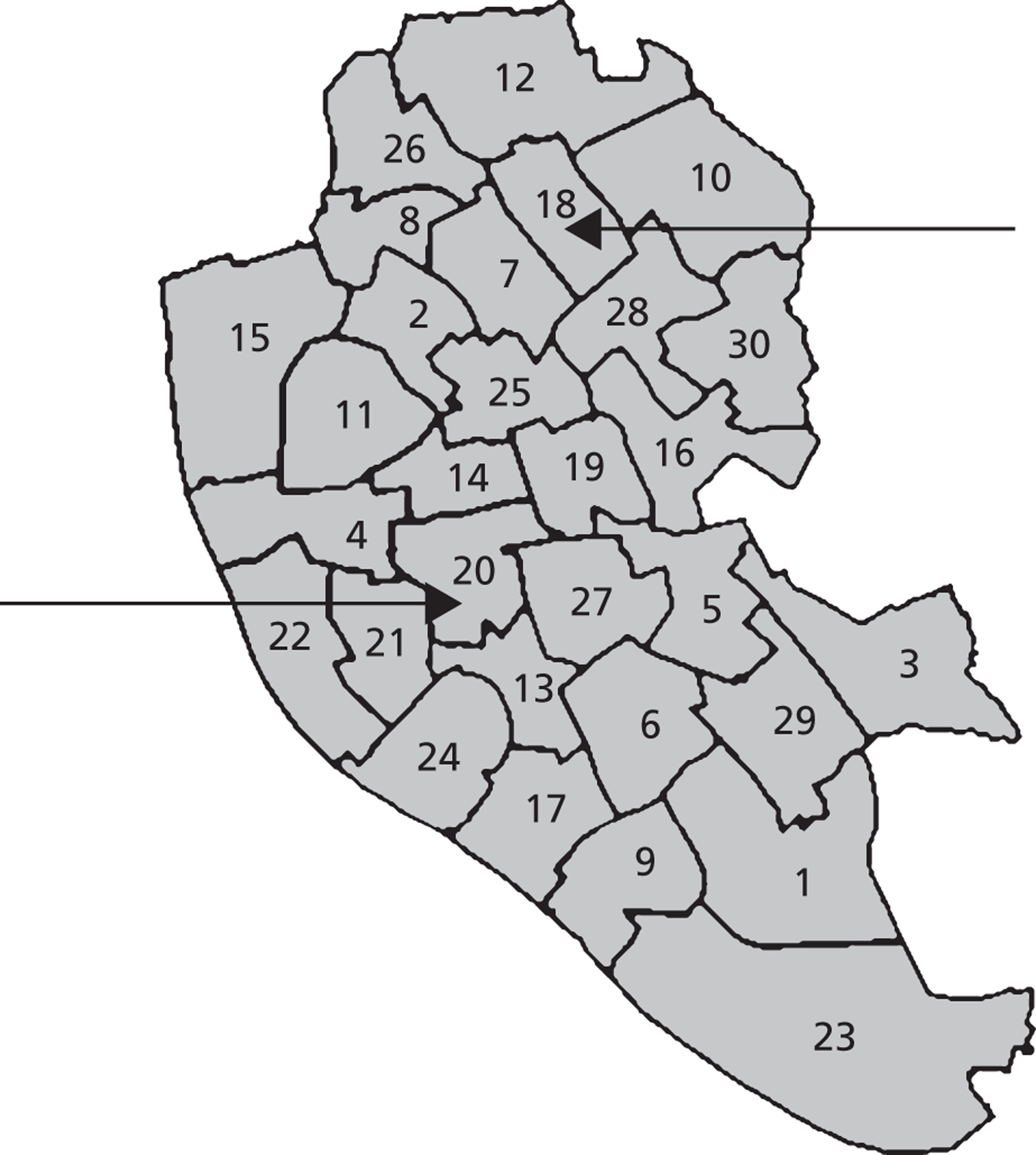
Picton and Granby (also known as Princes Park) are wards 20 and 21 in Figure 8. They are located in Liverpool's inner core and lie in close proximity to both the city centre and Wavertree Technology Park. The locality is characterised by ethnic diversity (> 40 languages in use), relative deprivation and extensive urban/housing reconfigurations within a number of urban regeneration projects. The majority of housing in the area is high-density pre-1919 terraces, and there is a large BME population (22.5% for Picton and 37.5% for Princes Park), including a substantial Somali community.
This locality includes the city's main centre for asylum seekers. Tenure patterns differ from national and local trends and are characterised by high levels of rented accommodation. Princes Park ward contains around 10 SOAs: seven of these are classified as belonging to the most deprived percentile of all SOAs in the country. Picton contains around 13 SOAs: three of these are in the most deprived percentile and seven are in the 2–5% most deprived. Approximately one-quarter of the population of each ward has some kind of long-term illness that limits their capacity to work. 359 Henceforth, we refer to this locality as Picton.
The two Manchester localities were Wythenshawe and Longsight (Figure 9). Wythenshawe is Manchester's largest district, a massive housing estate that was created in the 1920s as a garden city where an overspill population could be rehoused from industrial Manchester. It was originally divided into five local government wards: Baguley, Benchill, Northenden, Sharston and Woodhouse Park. In 2003, the ward of Benchill was abolished and its former territory was divided between the wards of Northenden, Sharston and Woodhouse Park.
FIGURE 9.
Manchester intervention localities.

The IMD 2007 score for Baguley ward was 46.82 and it was ranked 15 out of 32 across Manchester for deprivation. 360 In 2006, the Office for National Statistics (ONS) recorded that 9.3% of the population was from non-white ethnic groups. 360 According to the Manchester Residents' Survey of 2007, 21% of Baguley residents reported that they were not in good health,360 compared with 17% across Manchester as a whole and 7% across England. The unemployment rate in 2008 was 4.3%, higher than the average in both Manchester (3.9%) and England (2.5%). 360
Longsight is a residential suburb situated < 3 miles south of Manchester City Centre, which stretches from the City Centre through Ardwick. It has a very ethnically diverse population. According to the 2001 UK census, 52.7% of the population was from non-white ethnic groups. 360 This includes 36.1% who described themselves as Asian or Asian British (including 24.6% Pakistani and 7.2% Bangladeshi) and 9.1% who described themselves as black or black British. In 2006, the ONS recorded that 59% of the population was from non-white ethnic groups. 360 This included 40.9% who described themselves as Pakistani, Bangladeshi or Indian, 6.8% who described themselves as black Caribbean or black African and 3.9% who described themselves as being of mixed race. The remainder were from other ethnic groups, including 2.1% who described themselves as Chinese. The religious affiliation of its residents is one-third Muslim and around one-third Christian. Longsight is home to several mosques, some temples and a gurdwara, plus churches of varying denominations.
The IMD 2007 score for Longsight was 49 and it was ranked 13 out of 32 across Manchester for deprivation. 360 According to the Manchester Residents' Survey of 2007, 13% of residents reported that they were not in good health. 360 This compared with 17% across Manchester as a whole and 7% across England. The unemployment rate in 2008 was 4.5%. 360
Evaluation procedures
Evaluation was a crucial component of the AMP Development Partnership. It was conducted as a coherent process, interlinking the three intervention streams.
The partnership represents a complex, multilevel evaluation, based on the theoretical assumptions that intervening at three levels would be mutually reinforcing and thus more effective than intervening at one or two levels. However, we did not know whether or not this would actually be the case. We therefore allocated different degrees of intensity of intervention in order to have a no-intervention comparator for each of the three streams and hence the ability to explore the extent to which certain interventions reinforce others (Figure 10). This approach was designed to enable us to assess the extent to which access to – and quality of – services were affected by each intervention stream, considered separately and jointly.
FIGURE 10.
Scheme for allocating interventions. Reproduced with permission from Feld R, Woodside DB, Kaplan AS, Olmsted MP, Carter JC. Pretreatment motivational enhancement therapy for eating disorders: a pilot study. Int J Eat Disord 2001;29:393–400.
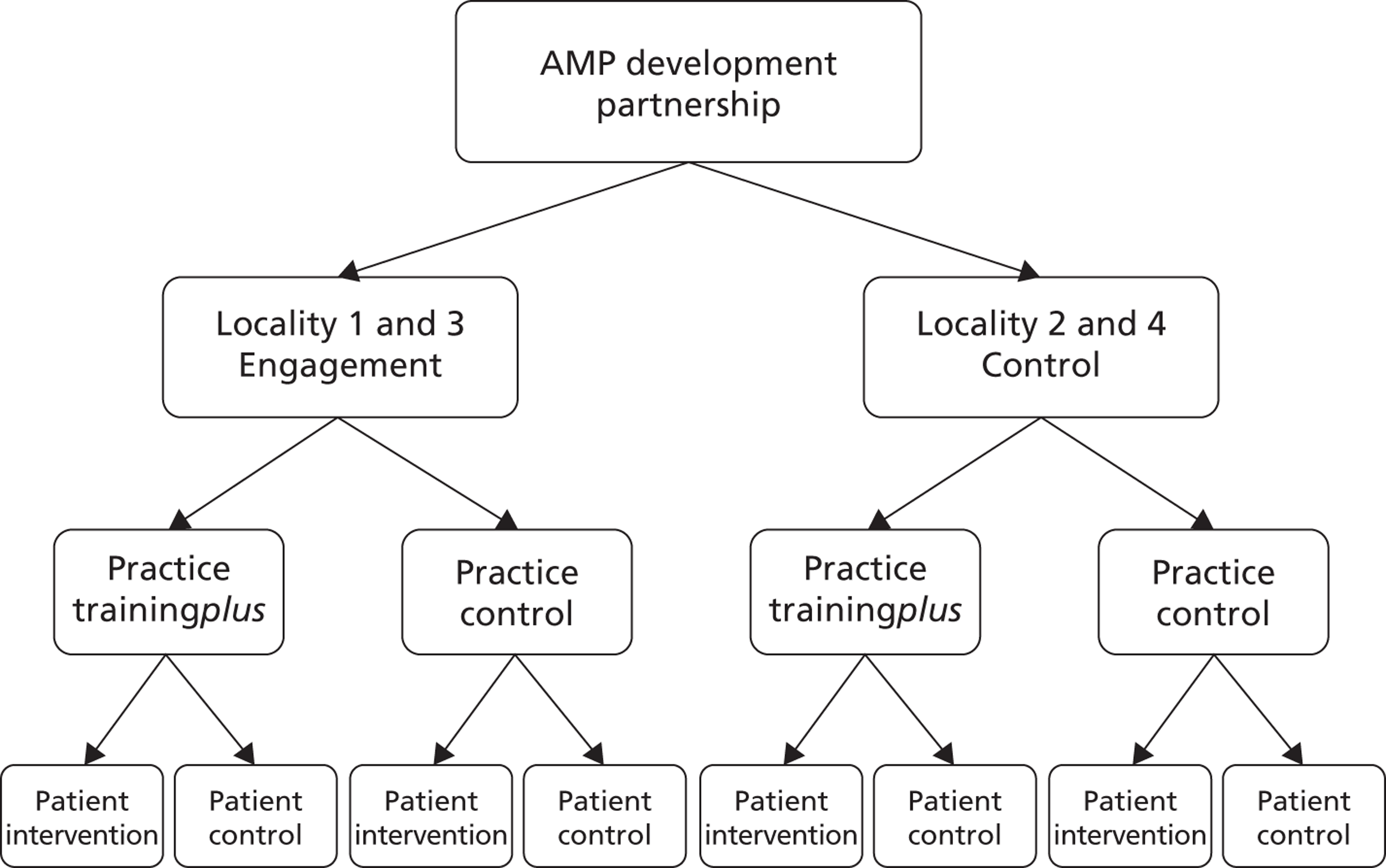
Within this allocation scheme we used mixed quantitative and qualitative methods to evaluate process and outcome, including:
-
the use of quantitative information including routine and project-specific data
-
interviews and focus groups with key actors
-
ethnographic observations and case comparisons.
We used a framework approach for analysis of qualitative data as this is well suited to an environment in which multiple researchers are gathering information from differing sites. 361,362 An initial coding framework was developed and transcripts were checked against the framework to ensure that there were no significant omissions. Using the qualitative software package MAXQDA (see www.maxqda.com; accessed 20 July 2012), codes in each interview were examined across individual transcripts as well as across the entire data set and allocated to the framework. Using the constant comparative method of analysis,363 broader categories were used for linking codes across interviews. Data were interpreted and analysed within the framework to distil, interpret and structure component statements about the intervention.
We provide further details of our evaluation methods within the descriptions of each of the three intervention streams in the following three chapters.
We received ethical approval to implement the AMP Development Partnership from the Salford and Trafford Research Ethics Committee (reference 09/H1004/67) with subsequent approval for the AMP well-being interventions being granted by the North West 8 Research Ethics Committee (reference 10/H1003/38).
To synthesise our findings and establish our key emergent conclusions, we organised a writing week for the whole of the AMP team, which took place in Warrington in January 2012.
Chapter 4 Community engagement
Aims and approaches
Our intention was to develop a simple reproducible community engagement model that could deliver on the aims of the intervention in a way that authentically engaged local stakeholders in the design and delivery of the community engagement interventions while providing for the wider needs of the programme.
Our scoping study (see Chapter 2, Identifying key concepts) stressed that access involves a dynamic and often protracted set of processes and decisions, involving not only patients and health practitioners but frequently also a wide range of stakeholders. For deprived communities the perceived personal ‘costs’ and ‘benefits’ for the patient or his or her family of engaging in treatment may involve different parameters from those in operation in more affluent communities. 220 Improving access for underserved groups could involve addressing any of the barriers in the pathway from patients recognising that they may need help to them seeking, negotiating and engaging in treatment. The nature, scale and impact of different barriers at the local level, as well as how we might best address them, could be understood only by engaging with the communities.
A community engagement approach needs to give communities a sense of collective ownership of the interventions, by involving them in both design and delivery. The role of the intervention team is to facilitate local action and local partnerships.
The community engagement strand of the AMP Development Partnership had four main aims:
-
to develop our knowledge of the range of understandings and attitudes about mental health and well-being in the community
-
to use this knowledge to tailor health literacy approaches to improve awareness of mental health issues in the community, including how, when and where to seek help
-
to address stigma and the acceptability of seeking help and identify the practical barriers to engaging in treatment
-
to develop local knowledge and networks required for primary care training and the psychosocial intervention.
In conceiving community engagement as an inductive problem-solving activity (see Figures 9 and 10), we expected these aims to be negotiated, augmented, refined and adapted to meet the needs of the local community.
We reviewed theory and practice in many different existing approaches to working with the community, which provided useful models and tools. 364,365 We drew pragmatically on a range of techniques that have previously been used in community engagement for addressing health issues. The University of Central Lancashire (UCLAN) model,366 built on participatory action research, is perhaps the best known in the UK. Although having a number of techniques and principles in common, developing a model for community engagement in a complex intervention context involved a different resolution of the principles underpinning participatory action research. A key difference between our approach and the approach of many others was the need to deliver tangible outcomes on a controlled range of issues at the local level within the intervention time frame. The community engagement element of the AMP model was then tailored specifically to meet the needs of community engagement in an intervention context. In doing so we turned to earlier precedents. Braithwaite et al. 367 developed a model for health promotion in minority communities that combined knowledge acquisition with organisation and development. Following Lewin,368 we conceptualised community engagement as a particular case of an inductive problem-solving process (Figure 11), taking place within the context of the research intervention.
FIGURE 11.
Community engagement as a problem-solving process.

Such cycles are routinely used in health service improvement and in policy development, for example in ‘plan–do–study–act’ cycles,12 in which they are conceived as an inductive spiral (Figure 12). 368
Community engagement model
Our community engagement model involved four components, implemented in sequence:
-
information gathering
-
community champions
-
consultative focus groups (CFGs)
-
community working groups (CWGs).
Our approach emphasised involving the community in reflecting on the problems and issues, and producing considered action at the local level in the relatively short time frame available. We also recognised the importance of gradually building trust when working with underserved communities with complex needs. We worked through participation, involving local people and service providers in both negotiating and delivering on the agreed aims. Drawing on the wider traditions of action research, this can be seen as empowerment through action and delivery.
We recognised that community engagement had certain predefined aims and parameters within the overall remit of the AMP programme. We therefore looked for an approach that would allow us to engage with the agendas of multiple community stakeholders, find common ground for action over the intervention period and help to foster partnerships and alliances that could lead to considered progress on more difficult issues in the longer term.
Because information gathering (step 1) was required to inform the AMP primary care and psychosocial interventions, this was carried out in all four localities.
In accordance with the wider intervention–control design, active community engagement (steps 1–4) was carried out in two of the four localities. The randomisation process involved stratification by city and by type of community. The Liverpool intervention site was randomly selected as Croxteth, with a focus on the mental health needs of elders. In Manchester, therefore, the intervention locality was Longsight, where we worked with the South Asian community. Within the timescale of the entire AMP programme, we were able to allow 2 years for implementation of our community engagement model.
Information gathering
Although our reviews conducted in phase 1 provided key findings, knowledge and best practice in working with underserved groups, they could not tell us about the specific issues for local people and wider stakeholders in the four intervention localities. The reviews did highlight that issues such as stigma and differential cultural understandings would bring additional challenges to engaging with communities.
Information gathering was also the first step in building the trust and networks necessary for successful engagement. It involves the intervention team getting to know the local area, communities and stakeholders by understanding the range of issues related to mental health and access from local people's own perspectives.
The aims of information gathering were to:
-
discover the range of understandings of mental health and well-being held by local people and communities
-
understand the wider issues that affect mental health and access to treatment at the local level
-
identify local community champions, partner organisations and wider community resources
-
develop a database of contacts and organisations to inform psychosocial interventions and primary care training
-
identify local stakeholders for CFGs (for active community engagement intervention localities only).
We developed a research strategy drawing on traditional ethnographic approaches369 and incorporating recent methodological innovations. 370
Information-gathering lasted for about 3 months and involved three overlapping approaches:
-
Entry to the field – getting to know the localities and people and the experience of life in these communities. We used internet searches and site visits to identify local service providers and events where we could meet local people. We invited local people and service providers to participate in ‘go-along’ interviews,370 which involved them showing us around the local neighbourhood, telling us about local people, communities, the area and how they live their everyday lives.
-
Key informant interviews using snowball sampling371 from distinct starting points located in the community (e.g. leaders, media, local businesses, education, police), with health- and social-care providers and within the voluntary sector. Accessing participants through local social networks allowed us to engage with people who would not be reached by sampling only from those in contact with formal services.
-
Mapping and collation of existing community data using a snowball approach with starting points in PCT community engagement teams, primary care, public health, social care, the voluntary sector, community media and local businesses.
These enabled the following outcomes:
-
the development of initial models of mental health understandings within the community
-
the development of key engagement messages
-
the development of a database of contacts, projects and resources across health, social, voluntary and community sectors
-
identification of local community nodes, information points, media and key actors.
Our information gathering was built on ethnographic principles that the interviewee is the expert and on the recognition that any knowledge that we gained about the community would always be contingent and incomplete.
Community champions
The community champion in each locality was to be the primary day-to-day contact for the community and was to facilitate the CFG and CWG. They were part-time appointments, funded by the AMP programme. Each community champion was supported by a member of the AMP research team. Whereas the researcher was responsible for safeguarding the needs of the intervention, the community champion needed to be seen as independent, representing the needs and agenda of the community as advanced through the work of the CFG and CWG.
Consultative focus groups
The CFGs were forums to negotiate the aims and agenda of the intervention with local people, agencies and wider stakeholders. They were expected to meet every 6 months or so over a period of 2 years. They were intended as a means of embedding the progress made in the intervention by involving local people and services in designing and implementing the community engagement programme. We expected the CFGs to play an important role in negotiating different agendas between local service providers; and to provide the strategic-level buy-in that is essential for many organisations if their workers are to dedicate time to participating in the working groups.
The main roles of the CFGs were to
-
bring together key local stakeholders
-
test and refine the findings of the information-gathering phase
-
clarify problems, resources and priorities for action across different areas of expertise
-
negotiate goals:
-
short term: what can be progressed now (including by the CWG)
-
mid-term: what needs to be achieved during the intervention life cycle
-
longer-term: issues requiring strategic action, advancing mental health and well-being in wider agendas at the local level and developing a shared vision to address problems and their treatment.
-
Membership of the CFGs was drawn from the contact list developed in the community mapping phase. Participants were chosen with an eye to the issues and resources identified through the mapping exercise. They included primary care and wider health sector workers (health professionals and policy-makers), members of voluntary or third-sector organisations, faith leaders, community police, local business representatives and local councillors. Although it was important to invite a broad cross-section of stakeholders, it was also important that the group be small enough that everybody had the opportunity to participate.
Community working group
Whereas the focus of the CFGs was on strategic issues and direction, the focus of the CWG was on implementing the action plan formulated by the CFG. It was intended that the CWG would involve local workers, strategic partners and community members in dividing the tasks needed to deliver a project, using locally available people and skills. Meeting monthly, it was expected to provide a regular opportunity for members from different sectors to develop knowledge, relationships and partnerships, and hence to improve access to care through local services in the mid- and longer term.
The CWG was created from nominated participants from the CFG. It could also involve other people with particular expertise or knowledge on a regular or occasional basis. We considered that splitting the ‘strategic’, agenda-setting function of the CFG from the ‘operational’ function of the CWG might be useful in maintaining focus on the agreed actions and a sense of shared ownership of the group's activities by the wider community.
Information-gathering findings
In Picton and Wythenshawe, the information-gathering phase was not followed by community interventions from the AMP team. We therefore present findings from this exercise in these two localities as discrete entities.
Picton
We began by walking around the area, visiting shops, markets and other publicly accessible spaces, making field notes and taking photographs. We conducted individual interviews with 22 people, of whom nine were white British and 13 were from BME communities (including three Somalis).
Perceptions of access
There was a shared perception among our respondents of an urgent need to do something about common mental health problems in the area. They thought that the general problems of living in the area adversely affect the mental health of local residents. These problems included racism, poverty and unemployment, poor living conditions and a lack of amenities. Respondents spoke of a lack of investment in vulnerable populations and orchestrated displacement of asylum seekers. They were also concerned about problems with communication, disconnectedness and isolation and loneliness. They did not feel sufficiently engaged in planning and decision-making about local services, and reported tensions with some voluntary sector providers. They were concerned about funding for voluntary services and a lack of collaboration between them and primary care.
When thinking about how to improve the well-being of people living in the locality, our respondents stressed the importance of informal and flexible facilities that are based locally and run by local people. They saw the importance of easily accessible funding for small community activities.
We combined these data with those gathered from the same locality during phase 1 and undertook a secondary analysis with the aim of understanding how access to primary mental health-care services was understood by those living and working in Picton. Our analysis generated a novel concept: the space of access. 372 We found the shape and dynamics of the space of access to be determined by at least four fields of tensions:
-
differing understandings of the area and of what was meant by ‘community’
-
differing understandings and definitions of mental well-being, illness and care
-
differing views on the position and importance of primary care services
-
the dynamics of resources beyond the ‘medical zone’ of care, especially in the third sector.
Community mapping
We developed a template of community resources with three overlapping domains:
-
health: mental health, general health or well-being
-
population: Somali, BME or general
-
site: local or city wide.
Wythenshawe
Both driving and walking through the area we identified events, facilities and organisations used by older people. We conducted 20 ‘go-along’ interviews,11 16 with older people (aged 52–91 years) and four with service providers, using snowball sampling from three different start points. Evaluation interviews were conducted with key informants from community organisations. Older people and service providers reflected on the personal and social meanings of the neighbourhoods in which they had lived or worked.
Importance of place and community
Wythenshawe held important memories for the service users. Some had lived there all their lives; others had been ‘bombed out’ of Liverpool and Manchester in the 1940s or came during the Manchester and Liverpool slum clearances of the 1950s. Wythenshawe provided abundant green spaces, new housing and modern facilities. A woman who moved to Wythenshawe in 1958 said: ‘I thought it was heaven on earth when I first moved here – 'cause I came from the backstreets of Manchester but coming up here was absolute heaven.’
The sense of community recalled from early days was contrasted with the present situation in which neighbours changed more frequently so that they no longer knew one another as they had done when they first moved in. Nevertheless, Wythenshawe was seen as a place where neighbours helped one another out.
Impact of change
From the 1960s onwards Wythenshawe underwent constant change and development. Shops and other services became more centralised and focused on the Civic Centre. The small neighbourhoods with their own local facilities declined. Service users were nostalgic for the communities that they remembered before the Civic Centre was developed. Changes to the built environment were referred to frequently. The sense of loss of amenities was aggravated by a feeling of powerlessness: an older man said, ‘they ask but they don't listen’. Service providers commented on the difficulties posed by short-term funding and the difficulties of providing continuity of services.
Support networks and barriers
There were many support networks operating in Wythenshawe, often associated with faith communities. They provided opportunities for older people to volunteer, as well as them being recipients of services. However, service users also highlighted losses associated with increasing age. They had a diminishing circle of friends, potentially leading to social isolation. A wheelchair user said: ‘There's no-one left to push.’ Participation in leisure activities was limited for financial and health reasons, and by fear of traffic and crime.
Community intervention findings
The community interventions in Longsight and Croxteth differed. In Croxteth the community champion worked through his existing organisation, rather than by adopting the CWG approach. Whereas the community champion and the CWG in Longsight addressed a wider range of issues, the focus of the community champion in Croxteth tended towards influencing local strategic issues. This may have reflected, in part, differences in needs and, in part, the differing styles of the two community champions. Although there were common themes between the localities (see Discussion), we report the work undertaken in each locality as a separate case study.
Longsight
Information gathering
Researchers initially immersed themselves in the local area, walking through the streets, local shops, parks and market, making field notes and taking photographs. The field notes, based on observations, conversations and naturalistic enquiry,361 provided an overview of local expertise and knowledge and gave us important insights into the motivations and needs of strategic stakeholders.
The first stage of observation focused on the activities and the ‘feel’ of the area:
I pass the Himmat Support Centre, which has a bouncy castle in the garden. There are several South Asian women standing near the front door. An Asian man in a wheelchair is being wheeled out of the gate, and a black man stands close to the gate, shuffling his feet; he appears to have learning difficulties and is talking to an Asian man that may have been his carer. The centre is busy and, on the basis of this afternoon's events, seems to be utilised by a varied cross section of the community.
Researcher notes
The second stage involved understanding these local activities through the eyes of the participants:
I sat and talked informally to [. . .] a member of the community mental health team [CMHT], about his work in Longsight and [. . .] a football team for people with enduring mental health issues which he organises. He talked about his belief in the effectiveness of a community centre based approach to supporting people with mental health issues, and this was his motivation to become involved with [local church] and bring some of the CMHT's work to the centre.
Researcher notes
Working through the contacts developed during the observation phase, the go-along interviews often elicited more nuanced, personal or emotive understandings of the local area and people:
One woman said to me, ‘We used to have servants but now we are servants.’ She was so ashamed that her son was a taxi driver when in Pakistan they had chauffeurs.
Researcher notes
The field notes from these exploratory site visits fed into team debriefings and the development of a database of local contacts and stakeholders.
Community champion
The Longsight community champion had lived in the area for a number of years. A British-born Muslim, with family in Pakistan, she had previous experience of working on cross-cultural health issues in other localities. As community champion she organised and ran the CWG meetings.
Consultative focus group
We held four CFGs during the programme. Timings were tailored to the availability of attendees and the progress made by the CWG. We held four CFGs throughout the programme (Table 6). Timings were adapted to the availability of attendees and the progress made by the CWG. Details of attendees at the CWG have not been fully collated. The imam and community police officer from group 1, for instance, continued to participate regularly in the working group although they did not attend further CFGs.
| Attendee | Group 1 | Group 2 | Group 3 | Group 4 |
|---|---|---|---|---|
| Third sector | 4 | 3 | 7 | 5 |
| Third sector (Bangladeshi) | 0 | 0 | 2 | 3 |
| Police | 2 | 0 | 0 | 0 |
| Faith leader | 1 | 0 | 0 | 0 |
| GPs | 2 | 0 | 1 | 0 |
| Practice managers | 2 | 1 | 1 | 1 |
| Public health | 0 | 1 | 1 | 1 |
| Mental health counsellors (GPs) | 0 | 1 | 2 | 1 |
| Domestic violence counsellors | 0 | 0 | 1 | 1 |
| Teacher (secondary) | 0 | 0 | 1 | 0 |
| AMP research team | 4 | 5 | 8 | 4 |
| Community champion | 0 | 1 | 1 | 1 |
| Total | 15 | 12 | 25 | 17 |
The agenda for each meeting tracked the problem-solving cycle (see Figure 11) and the emerging priorities and areas for action identified by the group are summarised in Figure 13. Researchers used field notes and recordings to produce a summary of the discussions and action points for the CWG.
FIGURE 13.
Longsight CFGs: evolving agendas.
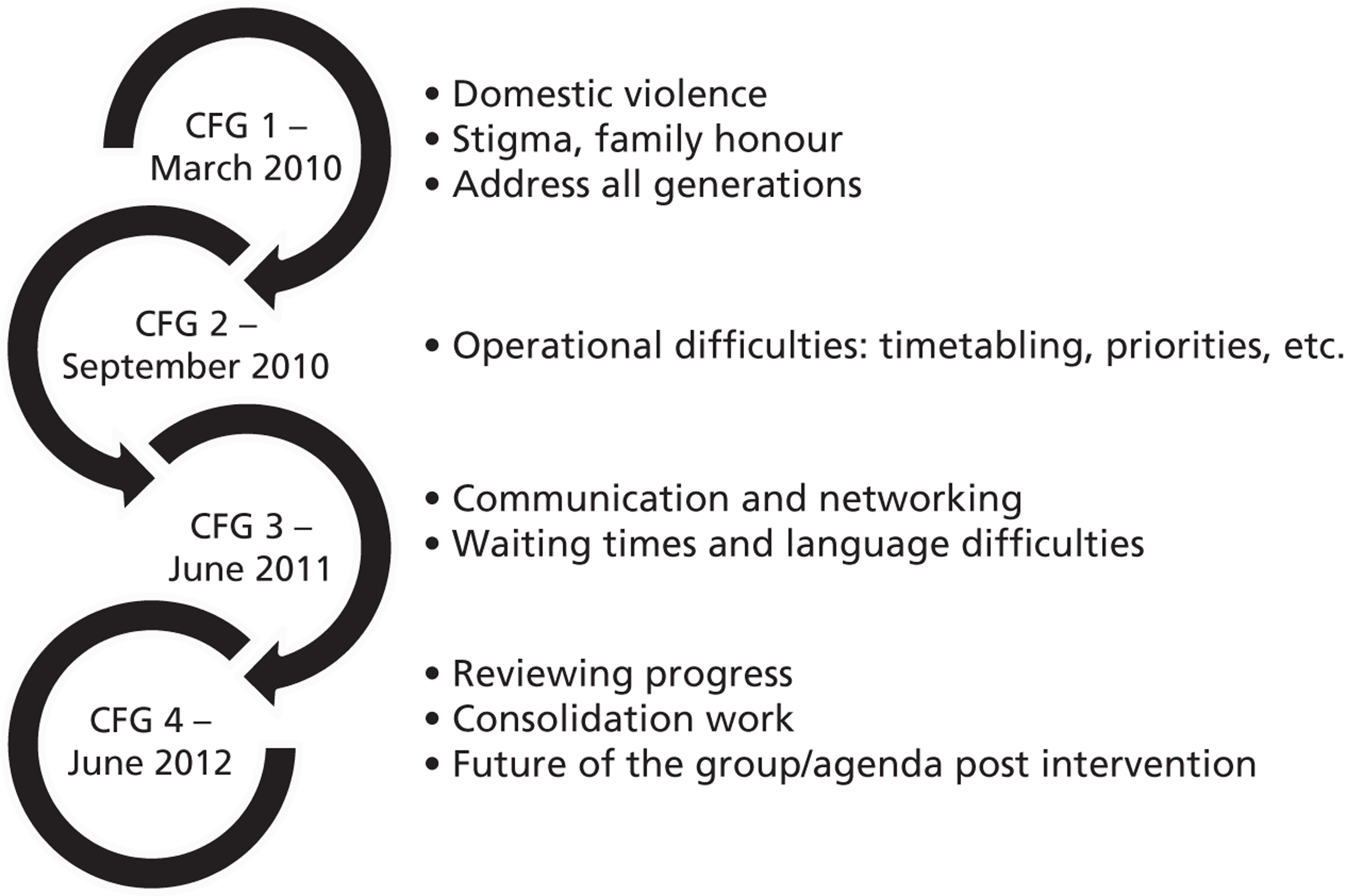
Community working group
The Longsight CWG began in July 2010. Led by the community champion the group included local service providers, a public health representative, a community police officer, a local imam and the practice manager of one of the intervention practices, as well as members of the AMP research team. The group had a high level of cultural knowledge and experience specific to working within the Asian community of Longsight. They met once a month, working towards the priorities identified in the first CFG of improving understanding of mental health issues and where to seek help, resulting in the following outputs.
Output 1: mental health calendar
The group decided that producing a mental health-themed calendar would have significant benefits over leaflets and posters as it might be displayed in the house, particularly in the kitchen, traditionally an area where women meet in the South Asian community. It could provide a talking point, potentially broadening its impact, as it might reach members of the community who would not be comfortable taking mental health information into their own homes.
To ensure that the calendar was relevant to the community, consultations were carried out with local Asian women's and men's groups as well as with local imams. These groups felt strongly about including three main areas: jinn and black magic, forced marriages and domestic abuse.
With one page per month, the calendar introduces different themes and issues in mental health and well-being matched to the seasons (see Appendix 5). Themes are illustrated through appropriate quotes from Quranic texts developed with local imams. The text runs in parallel columns in English, Urdu and Bengali. The final poster page reviews key messages and has contact details for local services.
The 2011 calendar was launched in late December 2010. The community champion appeared on Asian Sound Radio to promote the calendar and the work of the group. The calendar was distributed through local GP practices, third-sector partners, including mental health groups, Pakistani and Bangladeshi community groups and mosques. The calendar was refreshed and updated for 2012 and distributed through the same outlets and through new partners from the CFG.
Output 2: Facebook (and Twitter) group – ‘Mental Health in South Asian Communities’
A priority identified by the third CFG was a mechanism to share up-to-date information on changes in local services, events and resources for those working with the South Asian community. The concept behind the Facebook group was that members could update their own information as and when it changed. The Facebook page could also serve as a repository for good mental health materials available in South Asian languages. Facebook was chosen as a medium as it was widely used, enabled linkage with existing groups and was low cost and sustainable.
A member of the CWG proposed this idea and has been instrumental in setting up and administering the Facebook group. The group was launched in January 2012, drawing initially on the work carried out for the calendar. It has generated interest from practitioners in and beyond Longsight. At the end of June 2012 the Facebook page was generating up to 15 hits per day; the Twitter feed had 32 followers with an additional 3345 linked through LinkedIn accounts.
Output 3: relaxation CDs
Another issue identified by the CWG was the long waiting times for counselling and mental health services in South Asian languages, particularly Bangla. Many members of the group were looking for resources and materials that could help patients and clients while they were waiting for treatment. After reviewing all of the materials they could access they found little that they considered fully appropriate and freely available. Members of the group suggested a CD tailored to the South Asian community, including breathing exercises and muscle relaxation. The group has been working together on the content. They will consult through relevant community groups to ensure that the CD is culturally appropriate and addresses the community's needs. When complete, CDs will be manufactured and distributed through local health and third-sector services. The CD will also be freely available to download from the Facebook group.
Croxteth
Information gathering
We gathered information from walking and driving around the area, from visits to well-being resources and from local media and the internet. We undertook 19 individual interviews and one focus group with older people.
We witnessed a pride in the area and enthusiasm for making Croxteth a better place. There were concerns about the lack of public amenities, especially transport. Safety was an issue, related in part to danger from traffic and in part to fear of violent crime. We found that Croxteth has relatively few well-being facilities and that the majority of third-sector organisations appear to be economically vulnerable. However, we were impressed by the informal networks between various services and the presence of ‘human hubs’ who provide a sense of continuity and stability. There is a desire among community workers for greater contact with GP practices and recent initiatives have included a small local farm and health trainers.
Problems in accessing well-being services included a lack of knowledge of well-being, a lack of motivation for those who are depressed, a reluctance to engage with groups, inadequate transport services, safety concerns, financial difficulties, stigmatisation and sensory impairments. Proposed solutions to these problems included a web-based database of well-being resources, more health staff and community policing, improved public transport, and services made more physically accessible and provided free at the point of use.
Community champion
The community champion in Croxteth was an older man who had lived and worked in the locality all his life. As an active part-time employee with one of the third-sector organisations in the area, he was familiar with many of the problems facing local residents. Likewise, he was already aware of many of the local resources and had existing links with some of the key stakeholders.
Consultative focus group
Four CFG meetings were held in Croxteth between March 2010 and September 2011. Table 7 shows the background of the participants at each meeting. Apart from members of the AMP team, members of third-sector groups were the most likely to participate consistently in the CFGs. The participation of the police, community health workers, GPs and PCT staff (including commissioners) increased over time. Local councillors and housing and business leaders each took part in one CFG, whereas faith leaders did not participate in any of the meetings.
| Attendees | Group 1 | Group 2 | Group 3 | Group 4 |
|---|---|---|---|---|
| Third sector | 6 | 6 | 9 | 4 |
| Housing associations | 0 | 0 | 1 | 0 |
| Police | 0 | 0 | 1 | 1 |
| Local councillors | 0 | 0 | 2 | 0 |
| Business leaders | 0 | 0 | 1 | 0 |
| Faith leaders | 0 | 0 | 0 | 0 |
| GPs | 0 | 0 | 1 | 3 |
| Community health professionals | 0 | 1 | 4 | 1 |
| Primary care trust | 0 | 1 | 2 | 3 |
| AMP research team | 6 | 5 | 5 | 4 |
| Total | 12 | 13 | 26 | 16 |
The agendas of the four CFGs are summarised in Figure 14.
FIGURE 14.
Croxteth CFGs: evolving agendas.
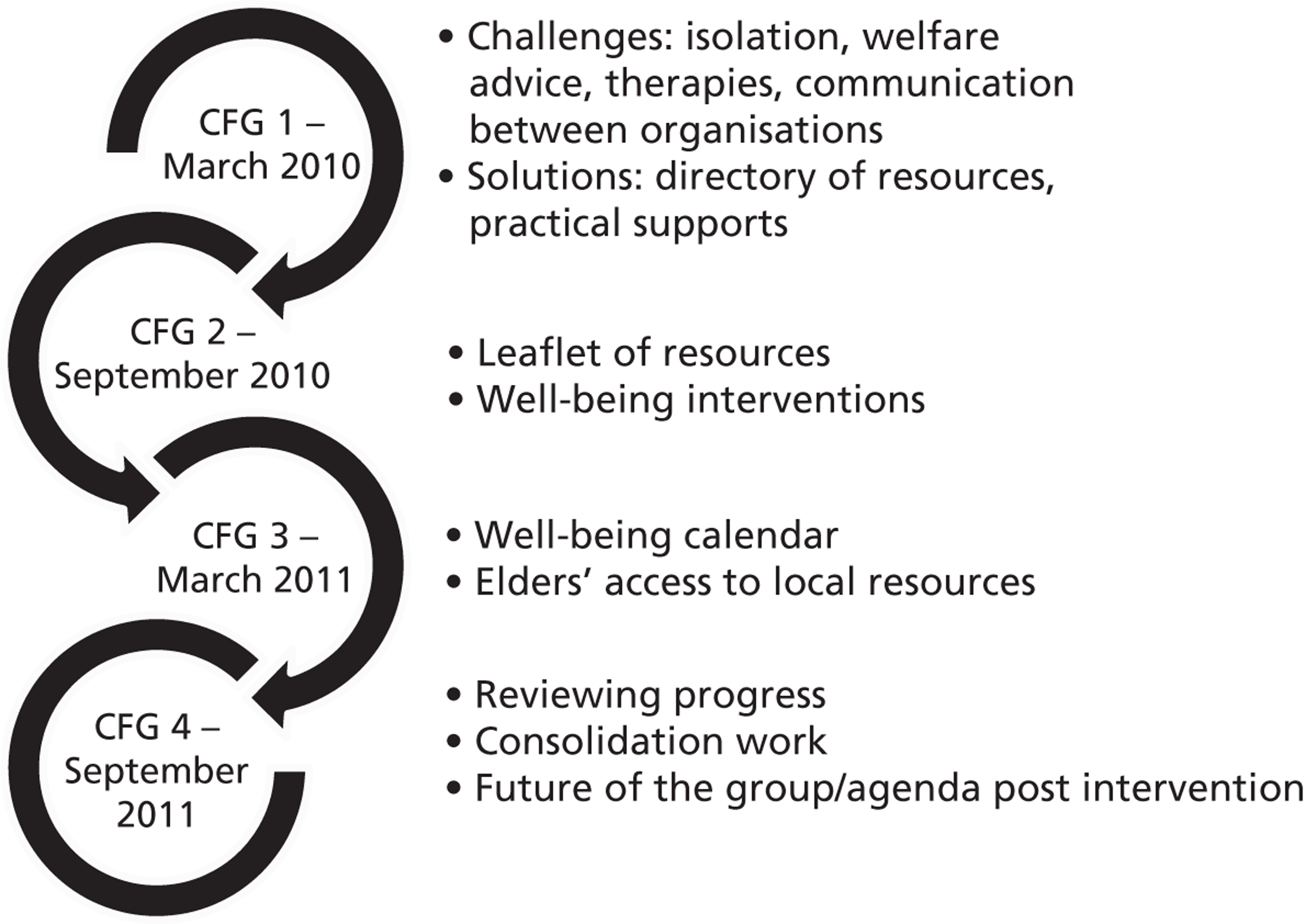
Outputs 1 and 2: ‘What's in L11’
Following extensive consultation with local third-sector organisations, and with the support of the AMP team and the CFG, the community champion produced two linked resource documents:
-
a ‘What's in L11’ leaflet
-
a well-being calendar for 2011 (see Appendix 6).
The leaflet and calendar both focused on the availability of, and access to, local third-sector and health resources of relevance to the mental health and well-being of older people in Croxteth and Norris Green.
These resources were distributed by the community champion, members of the research team, the local AMP well-being facilitator and the community police officer. Locations included primary care and community health centres, libraries, community centres, third-sector organisations and local pharmacies. Some 150 copies of the calendar and about 2000 copies of the leaflet were distributed.
The community champion also worked to engage the major local housing association and transport company in promoting the AMP agenda, the former through the inclusion of material in its regular resident newsletters and the latter through advertisements on local buses. Despite considerable effort, neither organisation was persuaded of the merits of pursuing these initiatives.
Strategic involvement
The community champion actively advocated the AMP community engagement agenda and promoted awareness of the mental health needs of older people through extensive networking with a variety of local and city-wide organisations. Local networking focused on fostering communication between the third-sector organisations represented in the ‘What's in L11’ literature. The city-wide organisations included the PCT's prevention and mental health group and Liverpool LINK Neighbourhood Open Space events. Here, his focus was on policy interventions. The strategic involvement of the community champion enhanced the opportunities for the AMP development agenda to influence PCT policy (see Chapter 8, Policy interventions).
Evaluation
Methods
Evaluating complex interventions requires attending not only to the expected trial outcomes but also to process evaluation, which details the background conditions that the ‘key ingredients’ require to operate and become embedded in the day-to-day routines and practices of the actors and stakeholders involved. We used an adaptation of framework analysis (see Chapter 3, Evaluation procedures) to synthesise findings across groups and locales, to understand their involvement and their perceptions of the interventions.
The locale, needs and access issues differed considerably between the four localities, as did the local service ecology. The first task in the community engagement evaluation was to understand the range of stakeholders – and for institutional stakeholders their operational background – involved during the intervention. There was a diverse range of process data available, from field notes of meetings to recordings of focus groups. These informed different aspects of the evaluation. The evaluation interviews carried out at the end of the programme were the primary source for the evaluation, with reference made to other sources as necessary.
Our evaluation consisted of four related dimensions, as shown in Table 8.
| Dimension | Data |
|---|---|
| 1. Stakeholder evaluations – understanding the aims, needs and objectives of local strategic stakeholders and the degree to which the intervention addressed or advanced these agendas | Go-along interviews, CFG and CWG field notes and recordings, community champion debriefing notes, evaluation interviews, wider process data (e.g. materials produced by CWG participants) |
| 2. Community engagement model – evaluating the efficacy of the model and processes of the community engagement approach that we adopted | As above plus evaluation data from the wider programme |
| 3. Population impact – evaluating the potential for impact on the local population and patient body | Go-along interviews, focus groups conducted by the community champion with local patient and community groups |
| 4. Evaluating the role of the community engagement intervention in the context of the wider programme | As above plus evaluation data from the wider programme |
The focus of the community engagement evaluation was the effectiveness of the community engagement model and how it related to the wider AMP programme. We explored the roles and experiences of the stakeholders who participated in the programme through semistructured one-to-one-interviews, using an agreed topic guide (see Appendix 7). We conducted 19 such interviews, 11 in Croxteth and eight in Longsight. We also undertook three focus groups with local community mental health and well-being groups to explore the efficacy and impact of materials produced by the CWG in Longsight.
Main findings
Uncertain context
Intervention sites were characterised by poverty, deprivation, high levels of need and demand on services. There was a common view that both need and demands on services increased during the intervention time frame (2009–12). Responding to these increases in demand was made more difficult by uncertainties over funding and organisational change, and consequent health and social service provision:
We've got a little bit of a reduction in services as well . . . people know we're still here which is good um but we're all on part-time hours at the moment so um all the workers' hours have been cut.
Mental health-care provider, Longsight
Despite a political commitment to intersectoral working and localised service provision,373 the realities for smaller third-sector organisations had been cuts and uncertainties over their future:
I think I think we have got huge structural difficulties when we think about the big society, because to my mind Liverpool has always had a big society, you know, with the history of philanthropy and volunteering and community activism. I think the localism agenda is . . . helpful to a point, but what I feel is that it . . . you know, if there are structures that are developed organically and naturally, and work, then we shouldn't be getting rid of them because of a new agenda that has been imposed.
Commissioner, Liverpool
Third-sector engagement
The third sector had come under pressure from funders to professionalise provision, adapt to performance metrics and focus on throughput. This led to focusing on services that attracted funding while cutting those that did not, despite ongoing demand. There was also a perceived tension between the funding available for smaller localised third-sector services and large-scale initiatives such as IAPT. Uncertainties over the services provided by the third sector, and their sustainability, were seen as core difficulties in building links and partnerships and in making referrals from GPs and statutory services. These difficulties initiating communication were seen as rooted in a lack of recognition of the pressures in a busy GP surgery:
On any given day I'll get twenty or thirty e-mails and then I'll get sort of three four types of leaflets in my in tray, ‘please put these in your surgery’, I'll get five or six posters, most of them are in English. And I'll phone the head office to find out if they do it in Bengali or do it in whatever and then its finding the space to put them up and then some patients don't even read the literature at all, they don't even look at it. Even the ones in Bengali.
Practice manager, Longsight
However, there was evidence of strong working relationships between third-sector and statutory services, for example between the police and domestic violence workers.
Croxteth
Views on the Croxteth community engagement intervention were mixed. AMP community engagement activity by the intervention team was valued, for example interactions between the AMP well-being facilitator and local health trainers. The CFGs were seen as good meetings and networking opportunities, but there were uncertainties over how productive they had been. There were perceptions that the meetings had not bridged divisions between primary care and the third-sector groups:
Primary care were at one side of the table and the voluntary, I was talking with the voluntary sector we were at the other side. So I didn't talk, well [. . .] I didn't, I didn't see . . . I mean that might have been happening, but in the little group I was in we were mainly voluntary.
Commissioner, Liverpool
The community champion was seen as committed and hard working, but there was a perception that he had limited success and needed more support to engage effectively:
I think ultimately, it was, possibly from, from our side maybe, you know, not, there wasn't enough support given by us maybe I don't know, to try and help him do more things . . . I mean, he had a struggle to, to, to make some relationships such as with [a local residents group], he'd mentioned a couple of times that he'd had trouble, getting them to support him.
Commissioner, Liverpool
There were uncertainties over what form this support should take. These difficulties in engagement may underlie a degree of replication between the AMP calendar and ‘What's on’ leaflet and some activities of community health workers.
Longsight
The CWG in Longsight allowed for closer working relationships and more regular contact and was valued as a place to develop new contacts and share news about services at a time of change:
It's like we're having to renetwork all over again because our previous networks that we had the majority of them have gone . . . It's literally now we've gone back to basics again, just go out there and network, publicise your services, find out what's out there . . . and then refer to agencies.
Domestic violence worker, Longsight
The opportunity for regular participation through the CWG may have influenced the perceived success of the CFG in Longsight, which was more positive with regard to making connections between sectors and different faith groups. Working together in the CWG on the Longsight calendar was perceived to have benefits for the content and its receipt. Passing on the calendar to clients, between members of the public and between health professionals was often discussed:
It's done awareness raising, it's kind of brought it out in the open, yeah, um it's given them a tool to go off, it's given them an arena for discussion about it because it kind of mentions quotes from the Quran as well so it's kind of got them to reflect that you know there is some of these or something that talks about mental health so it is something that happens in that community . . . I think when I spoke to people even though some there are some people that will not access our services because . . . they're a hard to reach community – but there've been people that have said oh I've passed my calendar onto somebody who needed it so indirectly that work was done for basically yeah.
CWG member, Longsight
There was a recognition that aspects of the cultural tailoring would be difficult to achieve in conventional settings:
I have to admit I was a bit I didn't like the bit about black magic the way it was described but I understood where people were coming from and sometimes you've just got to go OK well you're speaking from the community's experience so that's the way we need to go.
Public mental health specialist, Longsight
It was suggested that cuts to services may have limited engagement in the CFG and in referring to the well-being intervention. Among the third sector there was a sense of being seen as a ‘second-class’ service by clients and statutory services. The involvement of primary care in the Longsight CFG was considered crucial to its success:
Yeah the community ones they were really good, very good and I thought you just mentioned before about you know the GPs and I must say that was really really positive [. . .] to have the GPs all there together cause it's so difficult obviously cause they're so busy to get them together and that is something more that I know that this government that they want us to move towards is working a lot more closely with the GPs so it's an excellent thing to have in our community.
Family services, Longsight
Discussion
When reviewing our activity in light of the aims of our community engagement strategy (see Aims and approaches), we have evidence of a degree of success in all four domains:
-
Our information-gathering and community-mapping procedures enabled us to develop our knowledge of the range of understandings and attitudes about mental health and well-being in each of the four communities we were working with.
-
We used this knowledge to tailor health literacy approaches to improve awareness of mental health issues in the community. Working through community champions, CFGs and (in Longsight) a CWG we generated well-received outputs in the form of calendars and related material that addressed culturally relevant mental health issues and provided clear information on accessible resources.
-
Community members, clients and professionals considered that the materials and the processes of local engagement and partnership working developed through the programme could help address stigma among older people and members of BME communities, increase the acceptability of seeking help and identify (and overcome) practical barriers to engaging in treatment.
-
We were able to develop and utilise our local knowledge and networks to enhance the effectiveness of AMP trainingplus and our well-being intervention (see also Chapter 7).
The model that we adopted provides informative case studies of community engagement within the context of a complex intervention. The balance between community participation and working within the remit of the wider intervention differed between the two intervention localities. The strategic influence in Croxteth was successful in its own terms, but allowed for less active participation by local community organisations. The approach in Longsight relied on engaging with an active community, who recognised the value of the work and for whom the activities aligned with some of their own work.
Stakeholder engagement
We found clear evidence of engagement in both localities from third-sector organisations. There was also relatively strong engagement of primary care practitioners in Longsight and of health commissioners in Croxteth. However, we would not claim that the community champions or the engaged third-sector organisations were representative of their respective communities.
We consider that this engagement was predicated on the AMP community engagement model, providing opportunities for stakeholders, within a context of budgetary cuts and uncertainty, to share experiences, (re)build links between third-sector organisations and develop links between third-sector organisations and the statutory sector, especially primary care.
Overall, respondents appeared to consider the work of the CFGs and the CWG to be important and valuable. The facilitatory work and commitment of the community champions in maintaining contact and feeding back on meetings through e-mails and telephone calls appeared to be particularly important in this regard.
We found that the strategic focus of the CFGs was important in allowing practitioners with prescribed roles and workloads to devote their time to the groups' activities. For other staff with more autonomy this could be less of an issue, but the clear objectives produced by the groups and the freedom to contribute to agenda and set priorities were valued.
Communication
Communication was the biggest problem identified through the community engagement intervention. First, it was a question of finding the time to communicate. Second, was the timeliness of communication and having adequate appropriate information to hand. Third, there was a need to improve the quality or efficacy of communication between strategic stakeholders, establishing trust, value and a shared vision for developing a local service ecology that meets the needs of the whole population. There was often difficulty in bridging the different worlds of clinical practice and the third sector. The question for practitioners was essentially, ‘Is this a service I can refer patients to?’, bringing in secondary questions of suitability and reliability. Although third-sector organisations might be able to offer relevant skill sets, they experienced asymmetry in demand and funding sources.
The first two issues can potentially be improved through technology and systems improvements. The third is more complex. Our experiences and other research suggest that strategic-level partnerships, although essential, are insufficient,374 and that vehicles such as the CWG provide opportunities for local workers and practitioners to engage with one another.
Managing complex problems
An issue raised across the community engagement interventions was that those with the most complex problems were, on the one hand, those least capable of performing the ‘patient work’ required to engage in treatment and, on the other, those least likely to fit the ‘ideal patient’ model of services geared towards addressing discrete health or social problems. This situation was mirrored in the difficulties experienced in providing multiple points of access for the well-being interventions (see Chapter 6) and more generally in referrals across sectors.
In the case of complex problems it appeared that, without the ability to engage with multiple problems coherently, practitioners were concerned that patients would be unable either to engage with or to benefit from the treatment available. Second, practitioners were concerned about overstepping their role or of promising help that was not available. This confirms our review findings (see Chapter 2, Meta-synthesis of published qualitative literature) that service entry frequently occurs only at crisis points.
Community and university
Community engagement approaches are common in public health although there appears to be a tendency for public health approaches to have a broader remit rather than a single-issue focus. Given the breadth of public health targets and the limits of resources in deprived areas, it may be difficult to focus on one part of the population, potentially at the expense of others, particularly in diverse communities. Issues of how we should encourage, recognise and configure the role that universities play in their local communities are not isolated to this kind of programme, or to the UK. 375
The roles played by the community engagement teams can be understood as:
-
facilitation: providing space, structure, timetable and direction
-
translation between the different ‘worlds’ of practitioners across sectors
-
negotiation of a common agenda between different local actors
-
resourcing: small-scale financial inputs and university resources (graphic design, sound engineering) make a significant difference in communities with limited resources.
The esteem of the university can be an important element in securing access and trust with the community, as long as there is clarity and agreement about the role of the university in the local area.
Burdens and resources
Community engagement is critically dependent on the existence, and hence the funding, of a vibrant third sector. Our experiences have identified many hidden operational burdens on local services in areas of multiple deprivation. The cumulative impact of these additional burdens has not always been adequately reflected in resource allocation and organisational infrastructure.
At the time of writing local authorities and PCTs are the primary brokers of funding for services based in the third sector. The role of the new CCGs in this respect remains unclear (see Chapter 8). There is a risk that third-sector services fall beyond the conventional metrics that currently drive health-care systems.
The value of third-sector services often lies in their responsiveness to needs that are not met by conventional services. At a time of turbulence for health and welfare systems there is a danger that a patient's inability to engage with the health-care system, because of language or cultural issues, could be used as an unofficial proxy for health-care rationing, effectively removing the obligation to engage with those in greatest need.
Utility of the AMP community engagement model
The utility of our community engagement model was enhanced by its configuration as a discrete intervention with a phased approach, limited time frame and focused agenda. Our evaluation suggested that each component of the model had to be in place to effectively manage the multiple agendas and multiple stakeholders.
The successful application of our model depended on the careful management of its limitations. The phased approach gradually built trust with local people and organisations. This was evident, for example, in the increasing number and type of stakeholders attending the CFGs (see Tables 6 and 7). Establishing a focused agenda, achievable within the limited time frame of the AMP intervention, appeared to be valuable.
Paradoxically, the time frame of the AMP programme proved advantageous. Both information gathering and evaluation highlighted respondents who had previous experiences of community engagement as an extended ‘talking shop’ that did not result in tangible action. In working together to produce specific outputs, our groups gained confidence in their ability to act and in each other. The outputs appeared to be important in the intervention context and were well received both in the community and among health professionals and the research community. Members of the CFGs and the CWG had busy lives and finding time to attend, or to carry out wider work on outputs, could prove difficult, particularly at a time when services were stretched. The opportunity to engage in the programme appeared to offer an impetus to ‘do it now’.
Although all stakeholders valued working together and building therapeutic partnerships across statutory and third sectors, routine activities did not provide a framework to move this up their list of competing priorities. Many, particularly in the third sector, had attempted, with limited success, to build these relationships in the past. The opportunity to work together on a common project helped in getting to know new contacts better and developing the degree of trust required.
In Longsight, the separation of priority setting and addressing strategic issues in the CFG, and working on joint action on the resulting agenda through the CWG, appeared important in enabling effective working. It is worth noting, however, that although we explained this aspect of the community engagement model to stakeholders and participants on numerous occasions there appeared to be a limited understanding of its intended operation when discussed in evaluation interviews. The division of strategic and operational aspects between the CFG and the CWG was often unclear to those who were not routinely dealing with strategic issues. In retrospect, detailing the community engagement model and collecting relevant materials together on a project internet site may have provided a more accessible source of information than printed, distributed materials.
The involvement of a practice manager in the CWG in Longsight encouraged primary care to work directly with the third sector. Although we cannot directly attribute increases in intersectoral working to the community engagement intervention, developments among members of the CFG and the CWG suggest that it was influential. In the primary care evaluation, one GP reacted with considerable frustration at the prospect of a third-sector mental health group potentially closing because of funding problems. In the final CFG in Longsight, one third-sector participant announced that she would in future be offering training for GP practices in dealing with cases of domestic violence. This added to the overall sense that the AMP community engagement model had achieved measurable successes.
Chapter 5 Primary care quality
As part of the initiative to improve primary care quality, we developed a training intervention that we called AMP trainingplus. In addition to developing this training intervention, we conducted an ethnographic study within each of the practices that we worked with. In this chapter we begin by explaining what AMP trainingplus involved. Next, we describe how we sought to engage with primary care teams. We then present our ethnographic study and go on to describe and evaluate the training programme.
AMP trainingplus
The underlying rationale of the AMP model is the need to promote primary care services that recognise and accommodate the various ways that users and their communities ‘frame’ common mental health problems. This put the initiative broadly in line with ideas of ‘patient-centred’ and ‘culturally responsive’ services. However, for a successful outcome we needed to improve (where applicable) both patient and provider experiences of services. Simply offering training to GPs, even if this includes work on skills as well as knowledge, does not lead to improvement in outcomes for patients with mental health problems (apart from, possibly, newly diagnosed depression). 376 Improvement of primary care ‘quality’ and organisational change are both important. 377 Any initiative needs to be seen as relevant to practices' everyday work, and flexible enough to respond to the challenges posed by the needs of an individual practice. 378
As we explained in Chapter 2, the AMP programme assimilated evidence on the nature of access problems for underserved groups, and views of how access might be more equitable. We identified five key messages relevant for primary care (Box 1).
-
Engaging with services can require considerable personal investment of time and emotional and social resources from members of underserved groups.
-
People from underserved groups are less likely to consider the need for treatment, or to identify primary care as the place to seek treatment.
-
People from underserved groups are also less likely to perceive the treatment that they are offered/receive as appropriate to their needs. This has often been linked with differences in cultural understandings and perspectives.
-
Interventions commonly regarded by health-care professionals as beneficial may have negative consequences for people from underserved groups (threats to social identities, stigma, problems of illness identities).
-
‘Embodied suffering’ may be a useful concept for service providers. It highlights the close interplay of psychological and physical symptoms, and the relevance of adverse lived experiences for psychological symptoms.
These messages were incorporated into a syllabus checklist, which was the foundation of AMP trainingplus, designed to be a made-to-measure, flexible training package for primary care teams that would improve primary care quality, offering:
-
a training programme tailored to fit with local needs and priorities
-
practical support to review/address local organisational barriers to access, for example appointment booking, consultation times and interpreter services
-
links to a wide range of internal and external resources, including community-based psychosocial interventions within the AMP trial.
We developed AMP trainingplus with three interlinked strands:
-
Knowledge transfer, including a training component of up to six sessions, initially chosen from a menu of subject options. Our aim was to foster a space within which team members could reflect on practice and learn from colleagues.
-
Systems review: we offered practices intensive observation (up to 1 week) to identify organisational and structural features that may impede or promote access by underserved groups. This was centred on reception areas and appointment booking systems.
-
Active linking: we offered to raise awareness of other relevant organisations and resources that had been mapped and logged by the AMP team.
The knowledge transfer component was based on Grol's model,379 which emphasises the need to combine expertise from specialists with coproduction of ‘new’ knowledge within the practice. Grol noted that no single approach or focus is superior in all settings or for all problems, with different problems and settings needing individualised exploration of what would work to improve care. He does, however, offer guidance, including the need to bring expertise from specialists to the front line of care (e.g. to improve treatment of depression); promoting knowledge transfer through organisational changes and service integration; the importance of defining clear targets for change; the need for exploratory work to understand specific settings and target groups; and the importance of positive attitudes to change and a culture of learning and collaboration in target setting.
AMP trainingplus was developed for all practice staff, both those who have clinical contact with service users and those who have incidental contact with service users. We intended it to be practice-centred and responsive to the needs of each practice and to include topics such as consultation skills (detection of mental health problems, negotiating diagnoses, initial management, psychosocial skills, behavioural activation) and topics of broader relevance such as cultural competence, exploration of personal attitudes and values and working with interpreter services. The particular emphasis and specifics would depend on the local priorities determined by practices and primary care teams.
We identified the following intended outcomes:
-
increased staff awareness of, recognition of and respect for diversity
-
a change in consultation or encounter style and content, including communication, listening and negotiation, use of the evidence base, models of illness, use of interpreters and use of motivational techniques
-
a change in consultation or encounter outcomes, including referral, signposting, prescribing and satisfaction
-
a change in processes and systems, for example booking systems, use of interpreters, and referral to psychosocial interventions and social prescribing.
Engaging with practices
A vital part of AMP trainingplus was the need to embed the training in the locality within which each practice was situated. We needed to identify the scope and particularities of the issues to be addressed in each locality. We therefore undertook a process of gathering evidence and understanding its local relevance and identifying and logging third-sector resources, a procedure that we called community mapping. We have described this in Chapter 4 (see Information-gathering findings).
Working with our PCT partners, we identified four primary care teams (or practices) in two areas of each PCT based on mapping populations of underserved groups (see Chapter 3, Intervention sites). We needed to recruit practices to become involved in the AMP programme as either intervention or control practices. Our aim was to recruit two practices in each of the four localities selected to participate as intervention sites, with two others acting as control sites. We randomised the practices in each locality to the intervention arm or the control arm.
For the intervention practices, we sent letters of invitation to named senior GP partners and to practice managers along with written information explaining the purpose and nature of AMP trainingplus (see Appendix 8). Members of the research team then attempted to contact the named GP (and other GPs in the practice) and the practice manager to ascertain interest in the study.
When a practice expressed an interest in the programme, we arranged one or two pre-meetings to introduce the AMP staff and programme and answer questions about involvement in the study.
Topics covered in the initial meeting included summarising the results from phase 1 of the AMP programme; introducing community mapping (and community engagement for those localities where this was part of the intervention); negotiating the possibility of conducting ethnographic observations in the practice and arranging convenient slots for ethnography based in the reception area; and negotiating the possibility of an initial training session at which we would present the AMP model and the results of the community mapping and practice ethnographic observations, and explore local applicability and the practice's learning needs. We emphasised that there was no minimum commitment required on the part of the practice.
Practices were advised that the AMP team would facilitate practical arrangements for the first and any subsequent sessions (rooms, equipment, refreshments, etc.). We offered financial remuneration to cover the time that staff spent participating in AMP training and activities, which could include payment for locum cover or reimbursement for the use of the out-of-hours service.
At a later stage we also approached the two practices in each locality that had been randomised to act as control sites. We sought to meet with members of the practice team to introduce the programme of work and the aims of phase 2 of the AMP programme. In this meeting we aimed to negotiate the possibility of GPs and practice nurses using agreed computer codes to record the management of people with identified mental health problems; we also used this meeting to introduce the AMP well-being intervention and referral guidelines (see Chapter 6, Testing the intervention).
We also sought to discuss these two additional items with the eight intervention practices. We did this either as part of our knowledge transfer sessions or in separately arranged meetings.
Ethnographic observations
In this section we summarise the ethnographic observations that we conducted within the AMP intervention practices. The focus of the observations was on encounters between patients and receptionists at the front desk and encounters between staff within the practices. A more detailed account of this work may be found in the paper by Hammond et al. 380
Methods
We employed an ethnographic approach in the study as this allowed us to understand receptionists' work, as far as possible, in light of their own frames of reference.
Ethnography is a qualitative research approach, originating from cultural anthropology and becoming increasingly common in health services research. 381 It involves conducting fieldwork – spending time with people during their everyday activities and observing their actions and interactions to gain some insight into how they perceive their world – and closely considers issues relating to social norms, culture and power. 382 We carried out ethnographically orientated observations in general practices.
Of the eight practices approached, seven agreed to allow ethnographic observation in the reception area. All were situated in deprived urban areas but they varied in terms of other characteristics such as size, number of GPs and practice demographics, including ethnic mix.
Approximately 200 hours of observation were conducted during 2009–11 (Table 9). Researchers spent the majority of their time around the reception desk area. Our interest was particularly in those members of staff who spent part of their time working on a reception desk interacting with patients. We also familiarised ourselves with the ‘practice geography’, making observations in the waiting room as well as of encounters at the desk, staff interactions and patient flow.
| Practice | Time observed (hours) | No. of researchers conducting observations | No. of receptionists at practice |
|---|---|---|---|
| A | 38 | 3 | 7 |
| B | 22 | 2 | 8 |
| C | 7.25 | 2 | 5 |
| D | 26 | 1 | 5 |
| E | 36.25 | 3 | 7 |
| F | 37 | 1 | 7 |
| G | 34.50 | 3 | 6 |
Data analysis and management involved transcribing field notes to text files and importing these into a qualitative data analysis software package (MAXQDA). Individual incidents, considered meaningful to understanding the role of receptionists within a practice, were coded with descriptors that were then organised into clusters of related ideas by each researcher; this process was then conducted face to face as a group with all of the data combined to ensure that there was a high degree of agreement between researchers about the meanings ascribed to extracts.
Findings
Our findings focus on our observations of and conversations with receptionists with regard to a key element of their job, allocating and prioritising patient appointments, so allowing (or not) access for patients to GPs and practice nurses. We found that the context within which the practice operates impacts on the way that the receptionists' work is carried out. We identified three major themes:
-
complexity of the receptionists' role
-
allowing access
-
relationships within the practice.
Data presented are extracts from the field notes containing researchers' contemporaneous observations, reflections and annotations of the conversations with receptionists or between receptionists and patients or practice staff.
Complexity of the receptionists' role
Reception staff in all of the practices had multiple roles: answering the telephone, interacting with patients across the desk (to make appointments and book in for appointments, prescription requests), opening incoming mail, dealing with pharmacy staff and visitors and responding to queries from clinicians:
I was impressed by the range of activities carried out by R1 and her methodical approach to paperwork, e.g. papers were always tidied away into the correct piles or files, clerical jobs were fitted in between dealing with patients. R3 and R1 continued to deal with incoming calls, the second phone ringing, and patients at the window (often all three at once).
Practice D
Clinicians sometimes expected their needs to be met immediately, regardless of other demands on receptionists' time:
GP1 came in impatiently saying ‘I was ringing you’ to R3 who responded ‘I was busy’, which she was.
Practice D
Patients unable to speak or write in English added to the complexity, as their needs could not always be understood, nor could the rules of the practice be enforced.
Allowing access
The receptionists often had to negotiate a balance between granting patient access to GPs and practice nurses and restricting patient access to GPs and practice nurses. At busy times when the practice resources were seen to be under pressure, receptionists could struggle to find a way to avoid being ‘in the wrong’ with either the patient or the clinician.
The problem of ascertaining patient need in this context was complicated by the fact that receptionists sometimes made judgements on a clinical issue without sufficient information, time or training. 383 One receptionist explained some of the criteria that she used to determine a course of action for patient access based on clinical information that she obtained from the patient. These judgements were associated with feelings of responsibility for the clinical well-being of patients:
At the end of the day, I don't want someone leaving the practice without diabetic medication and have that be on my head. Or if it's an asthma attack or something.
Receptionist, Practice B
Receptionists' interactions with patients were shaped by their past and present experiences of those patients. For example, a patient's past history of aggressive behaviour was a contributing factor in how she was prioritised. Receptionists seemed to be trying to reconcile competing demands. Despite low status and a lack of technical knowledge, they had to make judgements about prioritising patients and allowing them access to clinicians.
Receptionists had to work within systems of rules and policies operating within practices, which they had little or no control over. In some cases rules were explicitly formalised; in others they were informal, internalised and implicit. Formal rules could sometimes have a detrimental impact on receptionists and were frequently subject to manipulation or circumnavigation. For example, in one of the practices, at the request of the senior GP, receptionists were required to ask all patients their presenting complaint and note it on the booking system. Following this rule positioned receptionists further into the clinical realm, which some patients were reported to be unhappy about.
In some cases rules were effectively unworkable in practice, for example asking patients to write down their own appointment time when they had poor literacy skills. In other circumstances, appealing to the legitimacy of a higher authority (usually a GP or the practice manager) was a useful tool for receptionists to employ to justify their position on a particular issue.
Relationships within practices
There was variety between, and within, practices in terms of the levels of interaction between receptionists and health professionals, the dynamics of these relationships and attitudes towards roles and responsibilities. It was particularly undermining for a receptionist if, when dealing with a patient, a health professional negotiated practice policy in a way that contradicted the receptionist's actions:
[Receptionists] became upset when they did not seem to be supported in their role by clinicians with regard to the rules of the practice – e.g. a patient expecting to be fitted in for a blood test that morning – receptionists explained it wasn't possible, but then nurse walked into reception and the patient asked them directly. Receptionists tried to explain to nurse what had been said but nurse cut them short and agreed to see the patient.
Practice C
We noted how the physical structure and organisation of the practice impacted on receptionists' work. In one practice there was a pronounced spatial differentiation between the reception, which was on the ground floor, and the consulting rooms and common room, which were on the first floor of a large building. There was little daily contact between receptionists and clinicians and the receptionists described how this distance left them feeling uninvolved. This contrasted with a practice that had a central meeting point around a ‘signing-in book’.
Discussion
We found that many of the difficulties that receptionists face in facilitating patient access to clinicians are compounded or alleviated by the actions of other members of the practice team and the organisation, structure and context of the practice. The danger is that socially constructed and mediated problems in practices are individualised and mapped onto receptionists, which exacerbates some of the inherent difficulties that they have to contend with. Constructing receptionists as powerful characters forecloses possibilities for questioning this dynamic. 384 The receptionists in this study did not feel powerful and, indeed, suggested that they were subject to rules and regulations that they did not understand and that they could not influence. This impacted on their ability to meet patient demand for access to clinical care.
Unpredictability and complexity are fundamental parts of general practice and it falls to the reception staff to deal with the consequences. To do this successfully necessitates flexibility and this should be taken into account when practice rules and systems are proposed and implemented. Of course, general practices vary in terms of staff numbers and roles, physical space, organisation, needs of the population served and culture. These specific qualities will inevitably shape attempts to improve the way that a practice functions for staff and patients. We suggest that rules are less useful when they constrain the ability of receptionists to deal dynamically with unpredictability, or repeatedly place them in situations that increase stress.
Eisner and Britten385 reported that the stress that receptionists experienced could be reduced when health professionals and other members of the practice team acknowledge the demanding nature of the role. Our findings support this position but expand on it: we suggest that, through reflection on the structural, social and spatial dynamics of a general practice, GPs and other members of the practice team have opportunities to identify patterns that may be shaping the experiences of receptionists in positive and negative ways. Swinglehurst et al. 386 describe the gap between formal protocols and real practice that is bridged through receptionists' creative ‘hidden’ work, of which clinicians are largely unaware. We observed and described such work and suggest that practices should reflect on work carried out at the front desk, identifying strategies (some of which may be straightforward to implement) that will help to ease the tensions that receptionists contend with daily. This has the potential to improve their job satisfaction and the performance of the general practice as a whole. Reducing the tensions experienced by, and impacting on the performance of, receptionists is likely to make the experience of patients attempting to make an appointment less problematic.
Delivering AMP trainingplus
First session
The outline and structure of the initial training session was the same for all practices and was based on our five main messages for primary care (see AMP trainingplus). It covered the following areas: aims of the AMP programme, feedback of results of phase 1, report of community mapping, report of ethnography if that had been completed prior to this initial session (which was the case in all practices except one), discussion of learning needs of individuals within the practice and the group itself, and discussion of the potential for further work or training based on issues arising from the meeting. The possibility of one person in the practice acting as a contact point (or ‘practice champion’) for the AMP team was also discussed.
After the initial training session we provided written feedback to each practice, summarising the issues discussed and suggesting possible areas where the AMP team could contribute in supporting the practice to meet some of the learning needs generated in the session. A designated member of the AMP team sought responses to our summary from the GPs and practice manager, through the ‘practice champion’ (where one was nominated), and ascertained the level of interest in further training sessions within the practice. We opened discussion with the practice contact about content, format, invited speakers and staff attending for future sessions. If appropriate, we offered the practice a menu of training options (see Appendix 9).
Subsequent sessions
The structure and content of subsequent training sessions differed between practices, depending on individual practice needs and negotiated aims. Table 10 summarises the topics covered in these sessions.
| Knowledge transfer (including skill development) | Systems review | Active linking |
|---|---|---|
|
|
|
Maintaining relationships with practices
One of the most important facets of the AMP programme was the developing relationship between the practice team (and specifically the named contact or ‘practice champion’) and a named member or members of the AMP research programme. We developed this relationship so that practices would feel that they were truly involved in the programme rather than ‘being researched’.
We decided to use the following strategies to develop and maintain this relationship:
-
presenting community mapping as a resource for the practice
-
maintaining contact with the practice and offering further support and training
-
offering referral options for the AMP well-being intervention (see Chapter 6)
-
providing reminders about linking with other community and third-sector resources
-
sustainability: exploring options for further development and continuing to work together.
Level of engagement
We engaged seven out of the eight practices invited to participate and delivered an initial session in all seven, during which the practice ethnography was presented and the learning needs of practice staff were identified through discussion. In two practices further training was not taken up, despite repeated attempts to contact the practices and offers of training sessions based on learning needs defined at the initial training session. The other five practices participated in between one and six further sessions (Table 11).
| Practice | No. of training sessions | Attending first session | Attending final session |
|---|---|---|---|
| A | 2 | GPs, practice managers, practice nurses, health practitioner, receptionists, administrative staff (19 in total) | GPs, practice manager, nurses (11 in total) |
| B | 5 | GPs (4), nurses (2), receptionist | Administrative staff (3) |
| C | 1 | GPs (7) | (One session) |
| D | 6 | GPs (2), practice manager, administrative staff (5) | GP, practice manager, practice nurse, medical students (2) |
| E | 1 | ‘Whole practice’ | (One session) |
| F | 5 | GPs (2), practice manager | GPs (3), practice manager |
| G | 7 | GPs (5), practice manager, practice nurse, receptionists (8) | GPs (3), practice manager, practice nurse, counsellor |
Evaluation
Methods
We undertook a process evaluation to illuminate the process of initiating and delivering the training and to identify where and why we succeeded against our aims and what lessons we should learn from the delivery of AMP trainingplus. We observed the delivery of training, making detailed field notes. After the training was completed, we arranged interviews with practice staff. Some staff agreed to one-to-one interviews, whereas others preferred to give feedback in focus groups. We conducted semistructured interviews using a topic guide (see Appendix 7) and subjected the resulting transcripts to a framework analysis (see Chapter 3, Evaluation procedures).
We also undertook quantitative data collection with the objective of assessing whether or not AMP trainingplus affected practice activity. We considered several options for collecting quantitative data from all 16 practices to measure any impact of AMP trainingplus. These included a prospective cohort study, a medical records study, a focus on patients with a diagnosis of depression and Patient Health Questionnaire (PHQ)-9 scores generated to meet criteria for the NHS QOF, and gathering data on the frequency and type of interpretation services. We decided to track referrals to mental health and well-being services (including the AMP psychosocial intervention) using Read Codes. We chose this option as it could be standardised across all practices, used a system that GPs are familiar with and left something in place that practices could use in the future.
We drafted a list of Read Codes used for patients referred to services for people with common mental health problems and tested the list with GPs in both Liverpool and Manchester. After refining the list we attempted to visit all practices to discuss setting up a template and collecting referral data every 3 months. We encouraged GPs to include this additional work in the Royal College of General Practitioners (RCGP) Credit-Based System for Continuing Professional Development. We also negotiated for reimbursement of service support costs in recognition of the administration time needed for collating Read Code data.
Why did practice engagement vary?
Engagement was a process rather than a single point of decision. It involved the development of mutual trust between a practice and the research team.
To gain access and maintain that engagement, the reputation of the researcher(s) and a history of working with one or more of the AMP research team in the past was important. Having a ‘practice champion’, a named contact within the practice, was vital in maintaining communication and momentum and facilitating repeat access for the research team.
The programme was usually introduced in the context of previous relationships at individual and organisational level, and clinicians may have had more awareness of this than researchers. Field notes for Practice G include the observation that the senior partner's conversation ‘focused very much on his/practice links with other clinicians/research and whether we knew them’. However, the academic nature of the AMP enterprise was sometimes seen by the AMP team as compromising in the practice setting; in those instances the presenter might emphasise shared GP status. Previous contacts did not always straightforwardly ‘enable’ engagement, for example in Practice C there was ambivalence among the GPs about previous academic contacts.
It seemed from initial ethnography and process evaluation that the management structure and style of the practice influenced engagement. Those practices with a more hierarchical structure seemed less receptive to continuing to work with us or delegated the learning and training to reception staff.
The work involved for the practice needed to be seen as coproduction – taking the practice forward – rather than practices ‘being researched’. In addition, the practice team needed to be in agreement with the underlying tenets of the AMP programme: that access to care for people with mental health problems needed attention, and that the practice team members had learning needs in this area. The AMP team thus had to maintain a balance between the core, explicit aims of the AMP programme and the flexibility demanded by practices. Some practice members did present some ideas about learning needs at the initial meeting, but there was still the need for negotiation around importance and priorities, allocating time and effort and encouraging the rest of the practice team to participate.
Reflections on the training process
We present results to illuminate the evaluation of the three interlinking strands of AMP trainingplus. Each illustrative data extract is identified by the source and the practice identifier.
Knowledge transfer
Respondents appreciated that training was organised at a time that was convenient to the practice. Reception staff particularly reported that they found the training to be valuable, both the opportunity to learn about mental health issues in patients they were coming into contact with across the desk and also as an opportunity to bring the team together:
I thought it was good, it got us involved and explain it went it explained more to us than we know as receptionists, we don't usually get involved in mental health and like anything like chronic diseases but with that it involved us as well so it was good . . . we got to listen and we were explained . . . Yeah so we got we were involved as well as the doctors which kind of makes us like say yeah, we understand more now cause otherwise we wouldn't have had as much understanding of mental health as we do now.
Receptionist, Practice D
GPs also suggested that including the receptionists in the training had had a positive impact on the practice:
Generally it was because it was for the patient, the reception staff as well because they have got a better understanding of how to deal with patients who are getting aggressive before . . . they think there might be something else going on. So rather than being just abrupt with they try to listen to the patients now more.
GP, Practice D
Receptionists were able to recollect particularly valuable individual training sessions:
[About asylum seeker training] We did ‘cause weren't we all quite shocked . . . It was quite interesting . . . Very upsetting as well wasn't it really.
Receptionists, Practice A
Some reception staff suggested that the training may have impacted on how they would deal with patients in the future:
If you see someone who's anxious and depressed you don't go in with all guns blazing now . . . : like no, you can't, it's like right how can I help . . . I'll try and do my best to help as long as you're polite with me I'll be polite with you.
Receptionist, Practice D
It was recognised that, in general practice, there are many topics that could be covered in training and that time was limited. The value of only one or two training sessions was thus questioned. Some reception and support staff felt that the training had not been relevant to non-clinicians:
Basically it was the clinicians who were more active in it because the clinicians were referring them. I don't think the staff, as in the reception staff or anyone else has had much input into the project.
Practice manager, Practice G
Some respondents had little recall of the training, whereas others suggested that it was not offering anything new:
Q: Since we did the research has anything changed in the way that you do things here as a result of it perhaps?
A: Well no because as far as the mental health referrals are concerned it's through the GP that they get referred anyway. I mean we still get patients who come in in a crisis or whatever, but we would get the doctor to deal with them do you know what I mean so it's not really.
Receptionist, Practice B
Respondents thus reflected on how training needs were agreed and how the training was delivered. The general view was that we had succeeded in fostering a space within which team members could reflect on their practice and practice systems, and learn from colleagues and the research team.
Systems review
We asked respondents to reflect on changes in the reception area and appointment booking systems, and the role played by receptionists in mediation between GPs and patients.
There was some evidence of changes in systems within practices, which staff attributed to participation in the AMP programme:
We used to do telephone triage and now the doctors do it, which is better for the receptionists cause me and [two other receptionists] always felt that we weren't trained clinically to triage.
Receptionist, Practice D
There was evidence that the training resulted in changes in attitudes or an improved understanding of patients and their presentation, and might impact on staff behaviour at the desk. The opportunity to work together seemed to have enabled a dialogue that had not been possible before, but which led to a better understanding of each other's roles in the practice:
Oh yes yes yes, we enjoyed, we loved that [patient journey] because it was very interactive, very very interactive. And they gave the staff the opportunity to because we don't all see what's happen outside, patient come in often extremely nice to us, but when you go out and the staff there ‘oh, he was horrible to me’. So we don't know what happens outside so we learnt about their side of stories as well.
GP, Practice D
An increased awareness of the contribution of the receptionist to the management of patients was also apparent:
Cause a lot of the time teams won't be involved in research it'll be you know maybe just the doctors so [. . .] for them it gave them kind of you know something to relate to you know sort of um you know they actually worked knowing that what you were involved in and what you what we were trying to get out of this.
Practice manager, Practice D
Active linking
We invited respondents to reflect on whether or not we had raised awareness of third-sector organisations and other resources as referral options for people with mental health problems. There was evidence that we did raise awareness about the voluntary sector, although it was not clear from these interviews how much this translated into changed behaviours:
They were very useful it made the practice team aware of existence of groups and services that we never thought they existed around us . . . . Also it gave us a clear way of tapping into these services whenever we need them so that is a great benefit . . . . I haven't personally referred because I probably haven't come across a patient.
GP, Practice B
Links with the AMP well-being intervention
Some respondents suggested that the reason why referrals were not made was because the well-being intervention was situated within a trial (which was a short-term initiative) and practitioners were concerned about the possibility of the patient receiving nothing. Others thought that it was because the focus on particular ethnic groups limited their options:
If it had been broader I think you would have been inundated and probably would be three foot high in paperwork and referrals.
Practice manager, Practice F
Some GPs reported barriers to accessing the intervention and tended to attribute these barriers to the patient. A GP in a practice that did not receive AMP trainingplus said:
Have I really got the energy, to spend 10 minutes explaining something that I think they're not going to do? Do you, does that make sense? [. . .] Talking therapies for certain, people coming from certain cultures is so alien to how they perceive what might help them, that it doesn't, that it's not gonna work, because they, they don't, they don't think it's going to be useful, so it . . . If they don't think it's going to be useful, chances are it won't be useful, you know.
GP, Practice J
The same GP described how it was possible to ‘forget’ to refer in the context of complex patient problems and competing organisational priorities:
Well because, you forget, you know. You know, today, I had a surgery running an hour late, by the time, you know, you might see somebody afterwards, you might think I should looked at that, but you already didn't do a loads of stuff the computer wanted you to do, you didn't do this and you . . . and they came in with five different things they wanted dealing with. It's like, ho[w] . . . their agenda, my agenda in terms of what my bosses tell me they want from me, and then, there's a sort of external thing that might work but they're sort of . . . they are further down the priority list.
Links with AMP community engagement
Those practices that had been involved in the community engagement strategy reported valuing this initiative and suggested that it had raised their awareness of local resources and possibly altered their behaviour:
I think that's important because I think um uh certainly at the focus group we said that we would like involvement with the local community members um and uh you know pillars of the community um local uh was it the police officer, etc. um and we actually identified that that was a really useful exercise.
Practice manager, Practice D
Having a concrete outcome from the community strategy that was perceived to be useful was commonly reported:
I thought they [well-being calendars] were a good cause. They went the calendars and [. . .] in demand and it had Islamic on and along with the English ones so I thought yeah I thought they were really good cause I took one home . . . Yeah I took one home so um and then people used to see them they used to say can we take one so they did go quite well.
Receptionist, Practice D
In Chapter 7 we discuss further the implications of links between AMP trainingplus and the other arms of the AMP Development Partnership.
Did AMP trainingplus affect referral patterns?
We collected Read Code data on mental health referral patterns from nine of the 16 AMP practices. Six of these practices were in the intervention arm (four from Manchester and two from Liverpool) and three were in the control arm (all from Liverpool).
Data were collected over 18 months, starting 6 months before AMP trainingplus was offered to intervention practices, and are summarised in Tables 12 and 13.
| Referral agency | 0–6 months (n) | 7–12 months (n) | 13–18 months (n) |
|---|---|---|---|
| Mental health workera | 29 | 36 | 34 |
| Voluntary services | 1 | 12 | 10 |
| Primary care mental health team | 83 | 58 | 35 |
| Counsellor | 157 | 164 | 115 |
| Psychologist | 3 | 6 | 10 |
| Community mental health teamb | 12 | 8 | 7 |
| Mental health information leaflet given | 5 | 9 | 3 |
| Exercise referral | 0 | 19 | 4 |
| Total | 290 | 312 | 218 |
| Referral agency | 0–6 months (n) | 7–12 months (n) | 13–18 months (n) |
|---|---|---|---|
| Mental health workera | 3 | 24 | 11 |
| Voluntary services | 0 | 0 | 0 |
| Primary care mental health team | 0 | 2 | 2 |
| Counsellor | 202 | 182 | 165 |
| Psychologist | 4 | 0 | 1 |
| Community mental health teamb | 30 | 26 | 20 |
| Mental health information leaflet given | 4 | 1 | 9 |
| Exercise referral | 7 | 5 | 8 |
| Total | 250 | 240 | 216 |
We found some evidence that the offer of or engagement of practices with AMP trainingplus was associated with altered patterns of referrals. Intervention practices were more likely than control practices to continue to refer to mental health workers including the AMP well-being facilitators and to refer to voluntary services. These differences did not reach conventional levels of statistical significance and without denominators it was not possible to comment on proportions of patients being referred from intervention and control practices.
Several factors affected our ability to gather useful comparative data. Despite discussion with practice staff in all practices, it proved impossible to create a common list of Read Codes that was appropriate for all practices that we engaged with. Some practices wanted to add additional codes (which they said that they used routinely) to our list. Capturing all referrals using a template was not acceptable to all practices, either because clinicians did not use templates or because they said that they had too many different templates already and were resistant to the introduction of another one, which they thought of as primarily for research.
There were differences between the four localities in the services that were available to practices. Thus, practices in Manchester had access to a primary care mental health team, whereas Liverpool practices had access to counselling and psychological therapy services. As they were known by different names (even though they offered similar interventions), GPs had different ways of coding them. Given that all control practices were in Liverpool, this skewed the referral patterns for community mental health and counselling between the intervention group and the control group.
It was not feasible for practices to identify members of underserved groups within their referral activity. This meant that we were gathering information on all patients registered with the practice.
Although we tried to ensure consistency of data recording between practices, it became apparent that Read Codes were applied by clinicians in the same practices in differing ways. Our data therefore reflect what clinicians remembered or chose to record as referrals, which may not always have reflected their actual referral activity.
Discussion
Achievements against objectives
Given that AMP trainingplus was delivered to a greater or lesser degree to seven of the eight intervention practices, it is relevant to consider the extent to which it enabled us to achieve our four intended outcomes.
1. Increased staff awareness of, recognition of and respect for diversity
Staff at all levels within primary care teams that had engaged with the training programme reported increasing awareness of, recognition of and respect for the needs of patients from underserved communities. Because we did not undertake any follow-on ethnographic work, we cannot be confident of the extent to which such reports were evidence of substantial changes in staff attitudes, or whether or not staff may have been influenced by other factors, such as a wish to convince the AMP team that its efforts had been worthwhile.
2. Change in consultation or encounter style and content
We received reports of changes in encounter style and content, particularly among receptionists. We are relying primarily on verbal evidence from practice respondents here, which may be subject to bias. The robustness of these findings would have been enhanced by before-and-after assessment of the style and content of practice encounters with patients (including GP consultations and other staff interactions with patients from underserved groups), using either detailed coding of observations or patient reports of practitioner behaviour. Although both methods have significant advantages methodologically, they are highly demanding logistically and dependent on the existence of reliable and validated coding schemes capturing the exact behaviours under consideration.
3. Change in consultation or encounter outcomes
We observed an increase in number of referrals to mental health workers, including the AMP well-being facilitators, and to voluntary organisations, but no other consistent change in referral behaviours, after the delivery of AMP trainingplus. We did not seek information on other relevant outcomes that might have been amenable to change as a result of the training, for example prescribing of antidepressants or anxiolytics. Nor did we attempt a formal analysis of medical records to investigate recording of consultations.
4. Change in processes and systems
Within several practices there were indications that reflecting back our ethnographic findings gave reception staff greater confidence in their role as mediator between GPs and underserved patients. There was also evidence in one practice of a system change, with doctors now taking responsibility for telephone triage, although it was not clear whether this was a result of – or coincidental with – engagement with the AMP training programme. It may be that the support staff were more confident after their training session on triage to suggest to their GP employers that they did not feel comfortable triaging calls (a view that was expressed in the training). There was no evidence of any changes in the systems for the use of interpreters.
We found evidence that the training programme increased awareness of – and encouraged signposting to – relevant voluntary and third-sector resources within the practice locality. This was particularly the case in the localities where AMP's community engagement was taking place, but it was also evident in the other two localities. However, we do not know whether or to what extent such signposting actually occurred.
Key learning points
-
We were not just ‘doing research’, we were offering things. Presentation of our community mapping was well received by practices, as they perceived the research team giving them useful information that they did not already have. Access to the AMP well-being intervention was also welcomed, although the referral process was seen as complicated and randomisation caused issues for some practices. Our offer of training was welcomed by most but not all of the practices; mental health is not necessarily prioritised by primary care teams and for some the AMP model appeared too complicated. Training appeared to be particularly successful when it addressed needs explicitly recognised by practices themselves, such as a lack of knowledge about the mental health needs of South Asian patients, or legal issues to do with asylum seeking.
-
It is valuable to have positive shared history with a practice, for example practices that have taken part in previous research, or members who have worked with principal investigators in other contexts. Thus, the reputation of the research team, or of key individuals within the team, is important. It is also useful for gaining acceptance if the members of the research and practice teams have shared clinical perspectives or a common cultural background.
-
Practice champions are important, acting as a link to the research team. Although it was not necessary for practice champions to ‘buy in’ to the full model of the AMP Development Partnership, they needed to have sufficient commitment and enthusiasm to encourage attendance at introductory sessions and promote the AMP agenda among other team members. In some less engaged practices we considered that there might be practice ‘antagonists’ who were not well disposed towards the AMP agenda. This was suggested by inactions (e.g. not responding to research team contacts) although it was not clear whether people acted invariably or consistently in this role. It was only as we began to work with practices that we were able to understand how the team ‘worked’ (in terms of communication, management styles, hierarchies, etc.) and could therefore identify whether key people could or would move things forward.
-
Flexibility and risk management are essential for both practice teams and the research team. We emphasised that practices could withdraw from our training programme at any stage and did not have to formally ‘sign up’ for a predetermined package. Engagement was a process, with continued involvement negotiated in a stepwise fashion. This was helpful for persuading practices to ‘opt in’ as it reduced their risk. However, it increased the risk for the AMP team insofar as it affected our ability to enact the full AMP agenda. It also called for high levels of energy from the AMP team: there was a continual need for us to work on maintaining our ‘investment’ when initial enthusiasm in a practice began to wane.
-
Practices are complex organisations, with a challenging variety of sizes, management styles and structures. Including all members of the practice team in training is beneficial but depends on a level of internal coherence and communication, which may not always exist. It takes time for a research team to understand how these dynamics work in any particular practice. Our policy of gradual engagement, linked with our ethnographic work, gave us the opportunity to develop such an understanding, although even then we were not always successful.
-
We therefore suggest that the effectiveness of AMP trainingplus was predicated on a trade-off between the needs of the primary care teams on one hand and the needs of the AMP team on the other. This is a dynamic process with a balance of investment and activity that varies not only between practices but also within practices over time.
-
When we come to consider the sustainability of AMP trainingplus, we need to remember that it represented only one arm of the AMP Development Partnership. We explain in Chapter 7 how the presence of the community engagement and well-being interventions arms offered primary care teams longer-term opportunities to meet the mental health needs of their underserved patients.
Chapter 6 Psychosocial intervention
Aim and objectives
In this arm of the AMP Development Partnership our aim was to develop and evaluate an evidence-based, feasible, acceptable and culturally sensitive psychosocial intervention for older people and people from BME communities.
To determine the content, delivery method, acceptability and cultural sensitivity of an intervention targeting older people and people from BME communities, we sought to synthesise data from previous work streams to design the intervention protocol; and to develop and deliver a training package for mental health workers to effectively deliver the intervention protocol.
We then conducted an exploratory trial in which we sought to:
-
test the intervention protocol, exploring the delivery of the intervention as well as adherence and acceptability
-
estimate key parameters for a definitive trial of the intervention protocol, through examination of recruitment rates and a comparison of outcomes in patients receiving the intervention and those receiving usual care.
Developing the intervention
The methods used to develop the intervention are summarised in Figure 15.
As noted in Chapter 2 (see Generating solutions), we held a 1-day synthesis workshop with the entire research team. The aim of the workshop was to synthesise the sources of evidence noted in Chapter 2 and produce key findings about the ways in which (mental) health problems are formulated by people from underserved groups; the costs attached to engaging with mental health interventions offered through primary care; and the limitations in access to existing psychosocial interventions.
We drew up a matrix of results, with each row of the matrix detailing one of the key intervention design issues that we wished to address, and the columns referring to the results from each individual data set (see Chapter 2, Generating solutions). This matrix was used as the platform to derive the key principles to be incorporated into the intervention. These included:
-
evidence-based psychosocial interventions
-
focused on both psychological issues and social issues
-
aimed to improve depression and anxiety
-
aimed to decrease social isolation
-
working with patients' explanatory models
-
destigmatising.
Following our synthesis, the intervention work-stream team drafted the details of the intervention and developed the training materials. The focus of the psychosocial intervention was on older people in Croxteth and Wythenshawe and people from BME communities in Longsight and Picton. Within the BME communities we focused on people from South Asian backgrounds in Longsight and people from Somali backgrounds in Picton. These groups were identified as being of high priority by both our stakeholder consensus exercise and the local PCTs. They include those less likely to access primary mental health care (BME communities) and those likely to receive substandard care when they do access primary care (older people). Our initial scoping review of psychosocial interventions (see Chapter 2, Structured scoping review of published quantitative literature) demonstrated the largest number of positive outcome studies in both of these groups.
Focus groups
To ensure that our intervention was acceptable and culturally sensitive, we undertook 11 focus groups with (potential) service users and service providers in each of our four localities (Table 14). South Asian and Somali service user groups were conducted either through interpreters or (in Manchester with two of the three groups) by a researcher who spoke Urdu, Hindi and Punjabi.
| Focus group | Location | n | Gender | Ethnicity | Age range (years) |
|---|---|---|---|---|---|
| Elders | Croxteth | 11 | Female 9, male 2 | All white British | 49–79 |
| Practitioners (older persons services) | Croxteth | 8 | Female 5, male 3 | All white British | 28–62 |
| Elders | Wythenshawe | 5 | Female 5 | All white British | 49–66 |
| Practitioners (older persons services) | Manchester University | 10 | Female 9, male 1 | White British 9, white (other) 1 | 30–59 |
| South Asian | Longsight | 17 | All female | Pakistani 14, Bangladeshi 1, Indian 2 | 24–65 |
| South Asian | Longsight | 14 | All female | Bangladeshi 14 | 22–55 |
| South Asian | Longsight | 9 | All male | Pakistani 7, Indian 2 | 35–65 |
| Practitioners (South Asian community) | Manchester University | 17 | Mixed | Mixed – majority South Asian | Not recorded |
| Somali | Granby | 10 | All female | Somali | 25–70 |
| Somali | Liverpool | 10 | All male | Somali | 61–80 |
| Practitioners (Somali community) | Liverpool community centre | 4 | Male 2, female 2 | Mixed | Not recorded |
We present the main emergent themes for older people and South Asian and Somali people.
Older people
Flexibility of provision
This included the need for longer sessions, more sessions, short waiting times, home visits, group sessions as well as individual sessions and the ability to respond to patient choice. Practitioners supported signposting for management of practical issues. They were also positive about group work for elders in community settings.
Stigma
The shame historically associated with mental health issues meant that elders were reluctant to talk about them outside the family. Therefore, deciding to access services relating to mental health might be difficult.
Overcoming barriers
When they needed to look for help beyond their immediate circle of contacts, elders identified methods of accessing the services that could help them, which supported multiple points of access, bypassing primary care if necessary. They did not always know what was available and what they were entitled to. Leaflets in community centres might help to inform elders of the existence and details of the services.
There was concern that GPs often fail to recognise psychological difficulties in their elderly patients or believe that there is nothing that they can do in the face of multiple problems. Elders identified receptionists as people who could obstruct access to their GP and were not always approachable. The perceived power wielded by receptionists was described vividly by one focus group participant who said, ‘Receptionists think they are God’, and added: ‘Before, it was like getting through Gestapo trying to get through a receptionist.’ This reinforced the importance of being able to bypass primary care.
South Asian people
Access
As with elders, stigma was a key issue. Participants recommended not naming interventions as ‘mental health’ programmes but rather as ‘well-being’ or ‘positive health’ programmes. There were barriers to access related to culture, religion, fears about confidentiality and difficulties with language. Use of interpreters could be problematic. Participants thought that accessing the psychosocial interventions should not be complex. Patients could be self-referred as well as being referred by friends, family or the health-care providers. Interventions should be provided by people who had expertise, good interpersonal and communication skills and the ability to develop trust and confidentiality. The place where the psychosocial intervention was delivered carried more significance. Professionals and service users both expressed preferences against home-based care. Service users preferred places that could be accessed without feeling self-conscious or embarrassed.
Social and practical elements
Participants thought that psychosocial interventions should empower people with skills and tools that they could take away and use in their daily life, including art therapy, jewellery-making, card-making, group-based exercise sessions, informative sessions on health and intergenerational conflicts, and leisure trips. There was also enthusiasm for exercise sessions.
Type of therapy
Some preferred individual therapy, whereas others seemed more positive about group therapy as a more effective method of destigmatising mental health. Few service users were aware of CBT and problem-solving. Most participants thought that patients should be able to start a new therapy or switch between therapies as appropriate.
Somali people
Content
Professionals thought that the design of interventions should be user-led, as professionals do not have enough understanding of the needs of the population. There was little concept of ‘mental health’ as an issue, or of counselling/talking therapies as a way of treating mental health, as these were generally considered to be the realm of the GP.
For talking therapies, Somali group members preferred a private weekly format to a group setting. They also thought that an effective intervention would be socially oriented, not focused on mental health, because of associated stigma.
Access
Professionals and members of the Somali groups both thought that the intervention should be community based. There were mixed views about how help would be accessed through doctors. A male group member said: ‘If we are sick, we go to the doctor. But, I don't know where to go with stress.’
FIGURE 15.
Developing the well-being intervention.
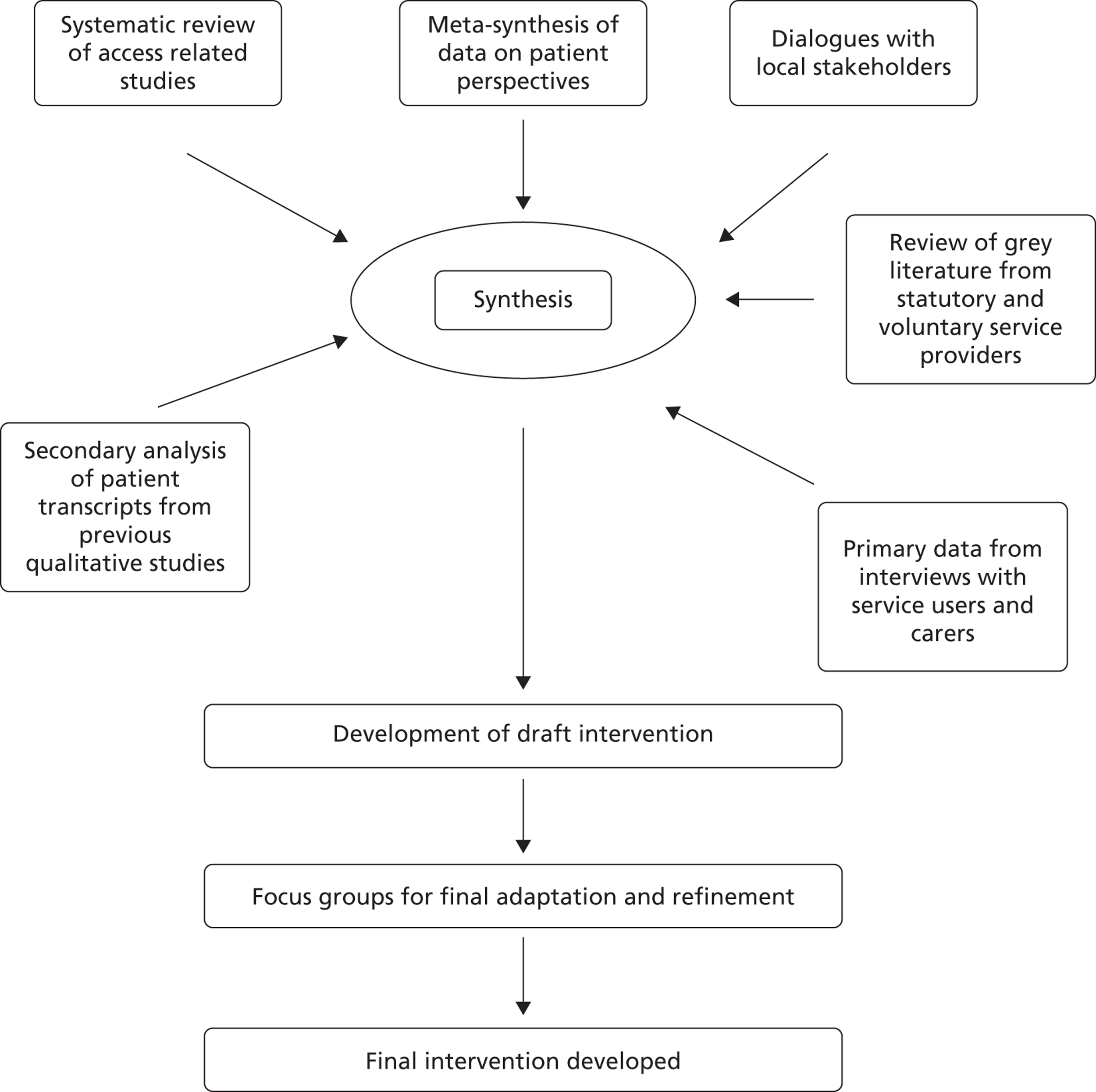
The well-being intervention
The well-being intervention focused on brief cognitive–behavioural strategies aimed at decreasing anxiety and depression and social isolation. The title ‘well-being’ was designed to maximise engagement and reduce stigma and to enhance linkage with our community engagement interventions. We incorporated a patient-centred interview and shared problem statements, goals and well-being plans. The intervention was delivered by well-being facilitators.
Participants were offered an initial patient-centred assessment session with a well-being facilitator and collaboratively devised a well-being plan. The well-being plan specified desired health- or social-care changes based on self-identified goals. Significant emphasis was placed on the patient as the ‘agent of change’, incorporating patients' previous experiences and coping strategies into the intervention and addressing stigma, expectations and illness trajectory to better engage patients. Once the goals had been identified, participants chose up to three ways to obtain support to achieve them: individual sessions with their well-being facilitator; group sessions with other participants; or direction (signposting) to appropriate public or third-sector services in their locality (Figure 16).
FIGURE 16.
The well-being intervention.
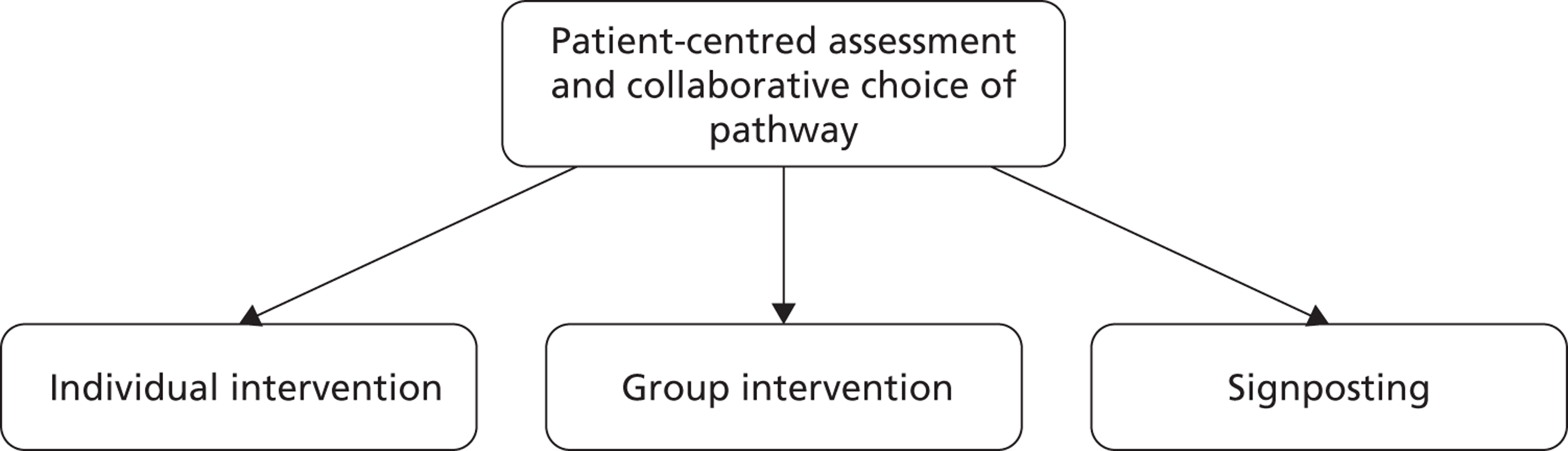
Individual intervention
-
The individual intervention used CBT, including behavioural activation, cognitive restructuring, applied relaxation and problem-solving, with an additional emphasis on decreasing social isolation by encouraging social activities.
-
The delivery mode (face-to-face, telephone or e-mail) was dependent on participant preference.
-
Individual interventions comprised up to eight sessions of approximately 30 minutes' duration over a 16-week period.
Group intervention
-
A well-being group, delivered by the well-being facilitator and third-sector volunteers, focused on improving mental health through group activities.
-
In the groups there was a strong emphasis on improving health and well-being and decreasing anxiety, depression and social isolation. Groups were delivered weekly for 1–2 hours over an 8- to 10-week period.
-
The content was specifically adapted by the group leaders to be culturally appropriate for the participants.
Signposting
-
This involved signposting to local mental health- or social-care services (support or drop-in centres) or activities, which included leisure and educational or employment opportunities. The aim of signposting was to decrease anxiety/depression, reduce social isolation and enhance health and well-being through mainstream, socially inclusive activities.
-
Participants for whom only signposting was indicated were seen three times over a 16-week period to ensure that they had accessed their preferred activities and overcome any barriers to attendance that they had faced.
Role of the well-being facilitator
The role of the well-being facilitator was to engage, support, advise and actively follow up participants. This included liaison with health- and social-care professionals who were, or needed to be, involved in their care, including GPs. When the participant was prescribed antidepressant or anxiolytic medication, the well-being facilitator would encourage guideline-concordant medication use, in liaison with the GP.
Training the well-being facilitators
The well-being facilitators attended a 3-day training programme. The training was accompanied by a training handbook that detailed session-by-session content (see www.amproject.org.uk, accessed 10 June 2013). A significant portion of the training focused on delivering the intervention (individual and group, using fictitious but typical cases of people with anxiety and depression). The research team developed an extensive directory of local services (see Chapter 4, Information-gathering findings) to ensure effective signposting.
Supervision
All well-being facilitators were supervised on a fortnightly basis, either face-to-face or by telephone (depending on location), by one of three members of the trial team (KL, LG or CD).
Testing the intervention
Our objectives were to test the acceptability of, adherence to and delivery of the intervention protocol and to estimate key parameters for a definitive trial of the intervention protocol, through examination of recruitment rates and comparison of outcomes between patients receiving the intervention and those in usual care.
Trial procedures
Design
This was an exploratory randomised trial of the effectiveness and acceptability of the well-being intervention for common mental health symptoms in (1) older patients and (2) patients from BME groups compared with treatment as usual.
Method
The exploratory study involved two trials. The core procedures (assessment, allocation, intervention and follow-up) were identical in both trials but the populations varied. We recruited older adults in Croxteth and Wythenshawe, South Asians in Longsight and Somalis in Picton.
Inclusion criteria
-
Age ≥ 50 years for Croxteth and Wythenshawe participants, in line with common inclusion criteria in published studies on psychological interventions for older people.
-
Age ≥ 18 years for Picton and Longsight participants.
-
Somali heritage in Picton and South Asian (Pakistani or Bangladeshi) heritage in Longsight.
-
Registered with one of the 16 primary care practices working with the AMP programme.
-
Scoring ≥ 10 on the PHQ-9 and/or the Generalised Anxiety Disorder 7-item (GAD-7) scale.
Exclusion criteria
-
Patients currently deemed to be at significant risk to themselves or others.
-
Patients with significant learning disabilities and cognitive impairment.
Recruitment
Recruitment was through multiple avenues, including through GPs, other health professionals, the voluntary sector or self-referral. Information was made available in relevant languages (Arabic, Bengali, English, Somali and Urdu) and in suitable locations in the community, for example surgeries, pharmacies, community centres, libraries, grocery stores and religious centres, including churches and mosques. We actively publicised the well-being interventions through our CFGs, regular newsletters and open community meetings. We made the psychological therapy teams in Liverpool and Manchester aware of our interventions and suggested them as a means to help reduce their waiting times. We also arranged meetings with AMP primary care teams to discuss the interventions and visited local community organisations.
Potential participants were given a patient booklet providing general information about the study (see Appendix 10). If they were interested in participating in the study, they or someone acting on their behalf (e.g. GP, other health professional or carer) provided their contact details to one of the AMP administrators. Following a referral, a researcher contacted potential participants and arranged to post or deliver further information. After a few days the researcher visited potential participants to answer any questions and obtain their informed consent. If consent was given, the researcher checked for eligibility using the PHQ-9387 and the GAD-7. 388 Participants scoring ≥ 10 on either or both of these measures completed the Work and Social Adjustment Scale (WSAS),389 the European Quality of life-5 dimensions (EQ-5D),390 the Clinical Outcomes in Routine Evaluation (CORE-OM)391 and a brief demographics form.
Participants who were ineligible were offered a list of appropriate local resources, generated from the community mapping element of the AMP Development Partnership (see Chapter 4, Information-gathering findings).
Randomisation
Randomisation was on a 2 (intervention) : 1 (control) basis. It was carried out by an administrator who did not have any formal connection to the study to ensure concealment of allocation from those assessing eligibility to the study. The recruiting researcher sent details to the administrator who randomised using random number tables. Separate randomisation schedules were used for BME and older patient samples.
Sample size
A formal sample size calculation was inappropriate to meet the aim of the exploratory study. To explore delivery and estimate key parameters for each trial, we aimed to recruit 50 patients to each.
Outcome measures
Outcome measures were CORE-OM, a 34-item self-report scale designed to measure global distress, including subjective well-being, life/social functioning and risk; PHQ-9 for depression; GAD-7 for anxiety; the WSAS for functioning; and the EQ-5D for quality of life (Table 15). These instruments are provided in Appendices 9–13 respectively.
| Outcome parameter | Measure |
|---|---|
| Well-being | CORE-OM |
| Depression | PHQ-9 |
| Anxiety | GAD-7 |
| Functioning | WSAS |
| Health state utilities | EQ-5D |
Analysis
Quantitative data were analysed on an intention-to-treat basis, with patients analysed in their allocated groups regardless of take-up of treatment. For analysis, we compared baseline demographic and clinical characteristics of the groups using descriptive statistics and calculated standardised mean differences to provide an estimate of the treatment effect (mean of intervention group at 20 weeks minus mean of the control group divided by the pooled standard deviation). Analyses were conducted in SPSS version 20 (SPSS Inc., Chicago, IL, USA) and Stata version 12 (StataCorp LP, College Station, TX, USA).
Adherence and delivery
To explore adherence to and delivery of the intervention we collected data on the interventions that participants chose, treatment uptake and attrition rates, and health professionals' field notes and reflections on delivering the intervention.
Well-being outcomes
The well-being quantitative analysis involved two feasibility trials in two populations with separate randomisation sequences, so the data were described and analysed separately. The small numbers in the feasibility studies mean that caution must be exercised when assessing differences between groups.
Recruitment and randomisation
In Croxteth and Picton we took referrals for 12 months from late September 2010. In Longsight and Wythenshawe we took referrals between late November 2010 and 31 December 2011.
In the elders group, 84 patients were referred. Fifty-two referrals were by GPs, seven by primary care mental health teams, four by voluntary organisations and 10 by others; 11 were self-referrals. Thirty-seven patients (44%) met the inclusion criteria and agreed to be randomised. At 20 weeks, 33 (89%) completed follow-up (96% in the intervention group and 71% in the control group).
In the BME group, 39 patients were referred. Of these, 20 were referred by GPs, two by primary care mental health teams, five by voluntary organisations and four by others; eight were self-referrals. Twenty (51%) met the inclusion criteria and agreed to be randomised. At 20 weeks, 16 (80%) completed follow-up (79% in the intervention group and 83% in the control group).
The Consolidated Standards of Reporting Trials (CONSORT) diagrams are shown in Figures 17 and 18.
FIGURE 17.
The CONSORT flow chart for the elders sample.
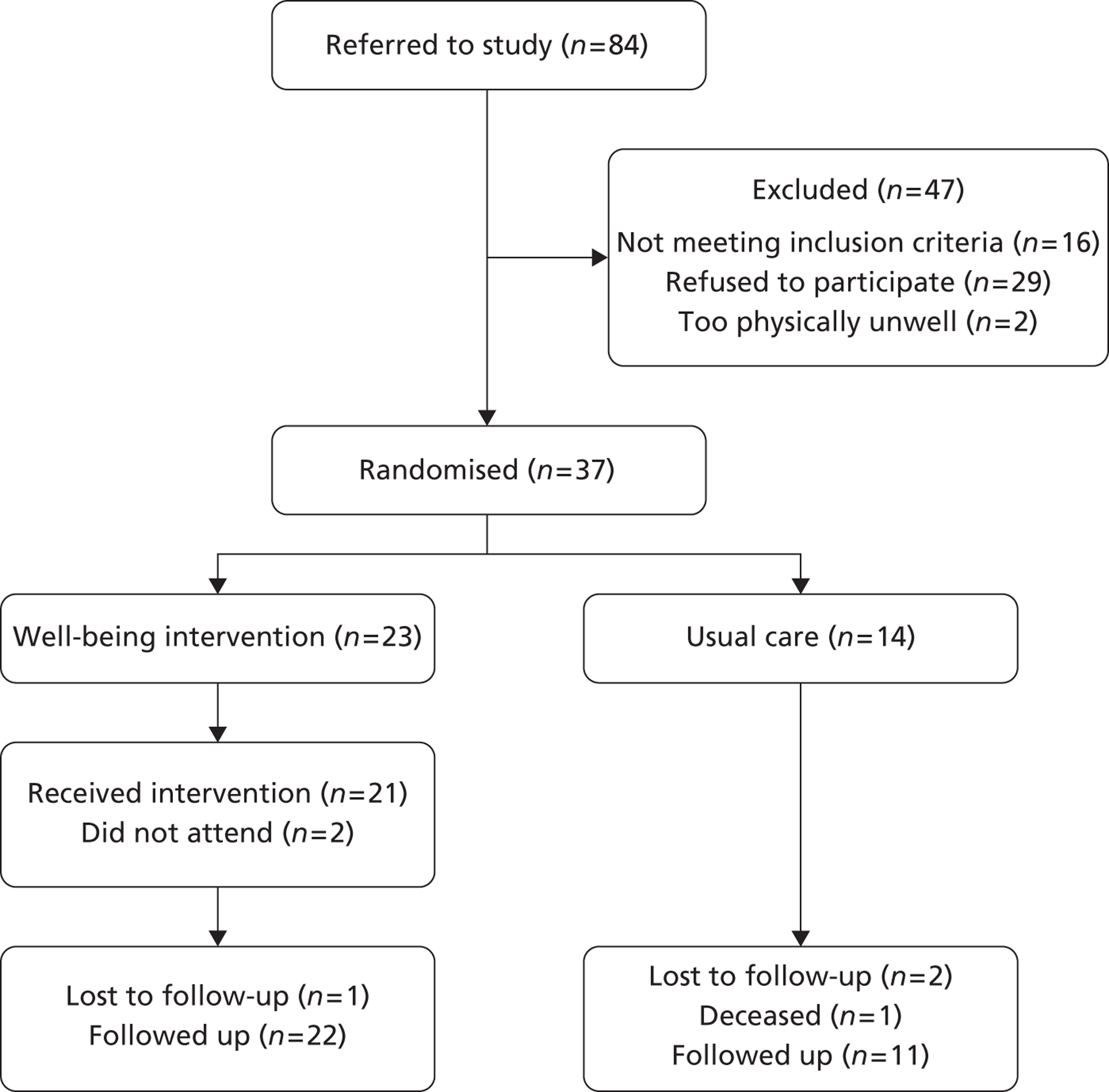
FIGURE 18.
The CONSORT flow chart for the BME sample.
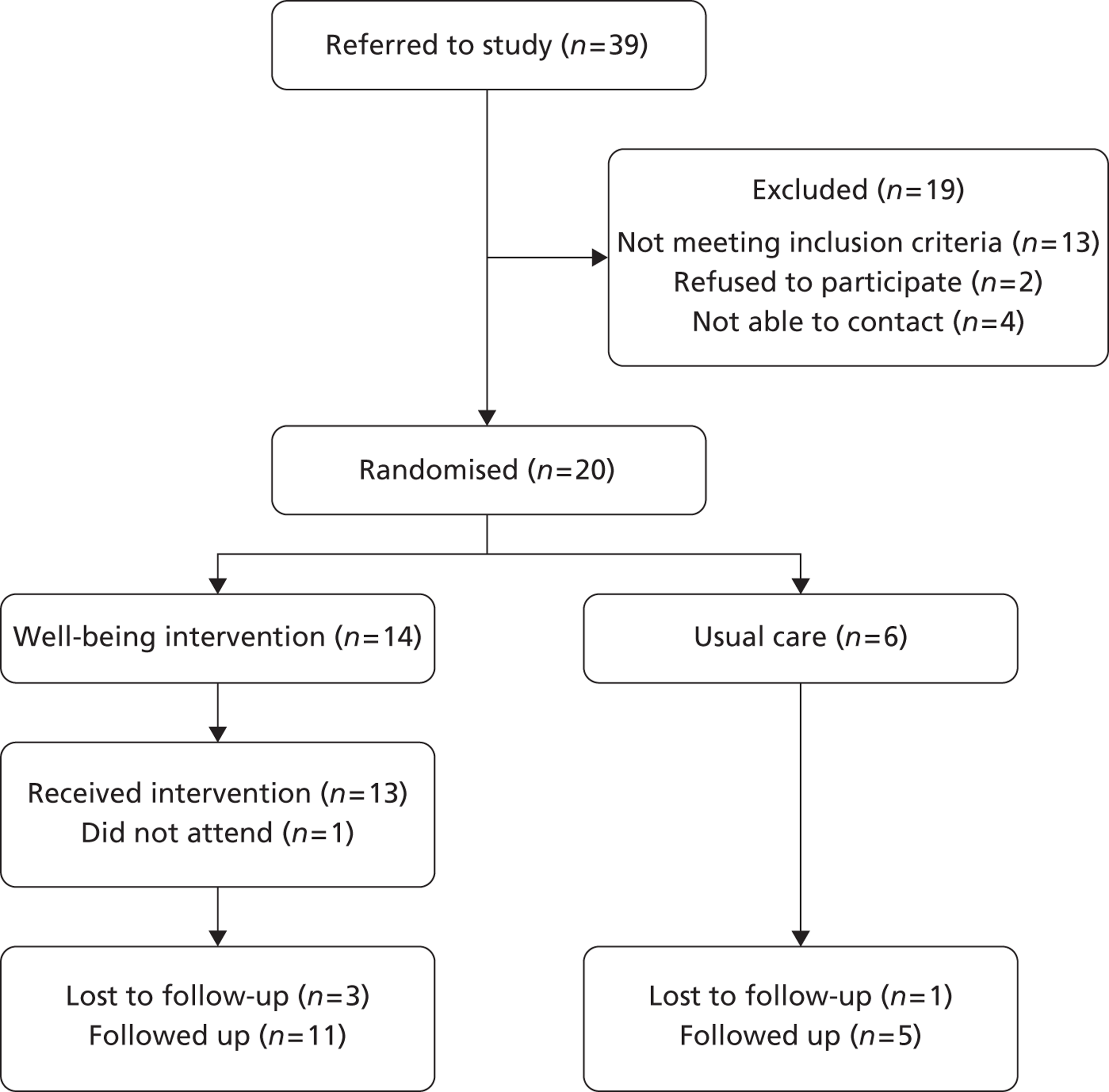
Baseline sociodemographic characteristics of the elders sample are shown in Table 16. As with most primary care mental health trials, most respondents were female, with a mean age around 64 years, nearly three-quarters were retired or otherwise not working and most were not involved in community activities. Levels of distress were relatively high, with a mean CORE-OM score of around 20 and a mean PHQ-9 score of 18.
Statistical significance testing of baseline differences is not recommended in trials generally and is inappropriate with small numbers when large differences between groups are likely to be not statistically significant because of limited power. Visual inspection of the data indicates reasonable comparability in terms of gender, age and ethnicity, but differences in employment and community engagement. Importantly, baseline levels of distress on the CORE-OM (primary outcome) and depression were comparable, although there were differences in other health measures.
| Characteristic | Well-being intervention (n = 23) | Usual care (n = 14) | Total (n = 37) |
|---|---|---|---|
| Sex, n (%) | |||
| Male | 6 (26.1) | 3 (21.4) | 9 (24.3) |
| Female | 17 (73.9) | 11 (78.6) | 28 (75.7) |
| Age (years), mean (SD) range | 65.64 (10.29) 50–84 | 60.70 (8.16) 53–78 | 63.77 (9.73) 50–84 |
| Ethnicity, n (%) | |||
| White British | 20 (87.0) | 13 (92.9) | 33 (89.2) |
| White other | 2 (8.7) | 1 (7.1) | 3 (8.1) |
| Mixed | 1 (4.3) | 1 (2.7) | |
| Employment, n (%) | |||
| Working full- or part-time | 5 (21.7) | 5 (35.7) | 10 (27.0) |
| Retired | 12 (52.2) | 3 (21.4) | 15 (40.5) |
| Not working or unemployed | 6 (26.1) | 6 (42.9) | 12 (32.4) |
| Engaged in community activities, n (%) | |||
| Yes | 3 (13.0) | 6 (42.9) | 9 (24.3) |
| No | 20 (87.0) | 8 (57.1) | 28 (75.7) |
| Baseline measures, mean (SD)a | |||
| PHQ-9b | 17.70 (5.14) | 19.00 (5.35) | 18.19 (5.19) |
| GAD-7 | 15.91 (4.31) | 13.20 (6.12) | 14.88 (5.16) |
| WSAS | 26.00 (9.48) | 22.86 (13.35) | 24.81 (11.03) |
| EQ-5D | 0.29 (0.36) | 0.31 (0.45) | 0.30 (0.39) |
| EQ-5D health state (0–100) | 44.65 (19.59) | 53.93 (25.81) | 48.16 (22.27) |
| CORE-OM (mean × 10)c | 19.85 (6.72) | 20.00 (6.90) | 19.91 (6.69) |
Baseline sociodemographic characteristics of the BME sample are shown in Table 17. All participants were female, with a mean age around 40 years, with most from Pakistani or Bangladeshi groups. In total, 20% had a degree and nearly one-third were involved in community activities. Levels of distress were relatively high, with a mean CORE-OM score of around 25 and a mean PHQ-9 score of 19.
Visual inspection of the data indicates reasonable comparability in terms of age and education, but differences in ethnicity and social engagement (although these are very sensitive to the small numbers in the groups). Importantly, baseline levels of distress on the CORE-OM (primary outcome) and depression and the other health measures were comparable. It is notable that the PHQ-9 scores in the BME and elder samples are comparable, but the CORE-OM scores were much higher in the BME sample.
| Characteristic | Well-being intervention (n = 14) | Usual care (n = 6) | Total (n = 20) |
|---|---|---|---|
| Sex, n (%) | |||
| Male | 0 (0) | 0 (0) | 0 (0) |
| Female | 14 (100.0) | 6 (100.0) | 20 (100.0) |
| Age (years), mean (SD) range | 38.92 (9.29) 25–56 | 43.02 (14.50) 21–58 | 40.15 (10.87) 21–58 |
| Ethnicity, n (%) | |||
| Pakistani | 6 (42.9) | 4 (66.7) | 10 (50.0) |
| Bangladeshi | 6 (42.9) | 2 (33.3) | 8 (40.0) |
| Punjabi Indian | 1 (7.1) | 0 (0) | 1 (5.0) |
| Somali | 1 (7.1) | 0 (0) | 1 (5.0) |
| Qualifications, n (%) | |||
| Degree or higher degree | 3 (21.4) | 1 (16.7) | 4 (20.0) |
| Eighth grade | 0 (0) | 1 (16.7) | 1 (5.0) |
| Sixth grade | 1 (7.1) | 0 (0) | 1 (5.0) |
| Fifth grade | 1 (7.1) | 1 (16.7) | 2 (10.0) |
| Third grade | 1 (7.1) | 0 (0) | 1 (5.0) |
| A levels | 0 (0) | 2 (33.3) | 2 (10.0) |
| O levels | 4 (28.6) | 0 (0) | 4 (20.0) |
| High school | 1 (7.1) | 0 (0) | 1 (5.0) |
| None | 2 (14.3) | 1 (16.7) | 3 (15.0) |
| Other | 1 (7.1) | 0 (0) | 1 (5.0) |
| Engaged in community activities, n (%) | |||
| Yes | 3 (21.4) | 3 (50.0) | 6 (30.0) |
| No | 11 (78.6) | 3 (50.0) | 14 (70.0) |
| Baseline measures, mean (SD)a | |||
| PHQ-9b | 19.36 (3.20) | 19.50 (1.76) | 19.40 (2.80) |
| GAD-7 | 18.07 (3.52) | 17.83 (1.17) | 18.00 (2.97) |
| WSAS | 28.85 (8.11) | 26.83 (8.35) | 28.21 (8.01) |
| EQ-5D | 0.21 (0.36) | 0.20 (0.49) | 0.20 (0.39) |
| EQ-5D health state (0–100) | 17.14 (12.51) | 17.50 (11.29) | 17.25 (11.86) |
| CORE-OM (mean × 10)c | 25.01 (5.86) | 24.92 (4.56) | 24.98 (5.38) |
Adherence and delivery
Of the 37 participants allocated to the well-being intervention, three did not attend any session: one participant moved and two were not contactable despite numerous attempts by the facilitators.
Sessions were offered face to face or by telephone, but all participants opted for face-to-face sessions. Of the 34 participants who received an intervention, 15 selected an individual-only pathway; 12 an individual and signposting pathway; five a group, individual and signposting pathway; one a group and signposting pathway; and one signposting only. The mean number of sessions attended was 6.3 (range 1–19). The mean total time of the sessions was 326 minutes (range 60–790 minutes).
In Appendices 14 and 15 we present two case studies (W030 and W019 respectively). We have chosen these to illustrate the flexibility and range of the AMP well-being interventions, including variability in ease of establishing contact between therapist and patient, intervention location and the importance of the social engagement dimensions of the intervention.
We offered group interventions in Longsight and Wythenshawe. In Longsight a group was established in partnership with a third-sector organisation that has run supportive groups for South Asian people with mental health problems for many years. In Wythenshawe a planned well-being group failed to recruit sufficient numbers during summer 2011 and so we ran a modified ‘Creative Activities’ group in early 2012. This involved partnership with a local third-sector organisation, with a focus on practical activities to reduce stigma associated with mental health.
The 20-week outcomes
Elders
The 20-week outcome data for the elders is shown in Table 18. Caution must be exercised in interpretation of outcome data in a feasibility study as the small numbers mean that baseline differences can occur through chance and power to detect differences is limited.
The results suggest that the group receiving the well-being intervention improved compared with the group receiving usual care.
The results are plotted in Figure 19 using a standardised mean difference (effect size) measure. The largest effects are seen for CORE-OM and PHQ-9. The small numbers mean that these results are not statistically significant, but the magnitude is fairly substantial compared with that seen for other psychosocial interventions in primary care. 392 These results are not adjusted for any potential baseline differences.
| Outcome | Well-being intervention, mean (SD), n | Usual care, mean (SD), n |
|---|---|---|
| CORE-OM | 14.32 (8.37), 22 | 19.71 (8.58,) 11 |
| GAD-7 | 11.41 (6.96), 22 | 12.27 (8.17), 11 |
| PHQ-9 | 11.82 (8.05), 22 | 16.55 (6.25), 11 |
| WSAS | 18.20 (11.84), 22 | 23.55 (14.30), 11 |
| EQ-5D | 0.40 (0.44), 22 | 0.27 (0.44), 11 |
FIGURE 19.
Forest plot of the effects of the well-being intervention on older patients. CI, confidence interval; SMD, standardised mean difference.
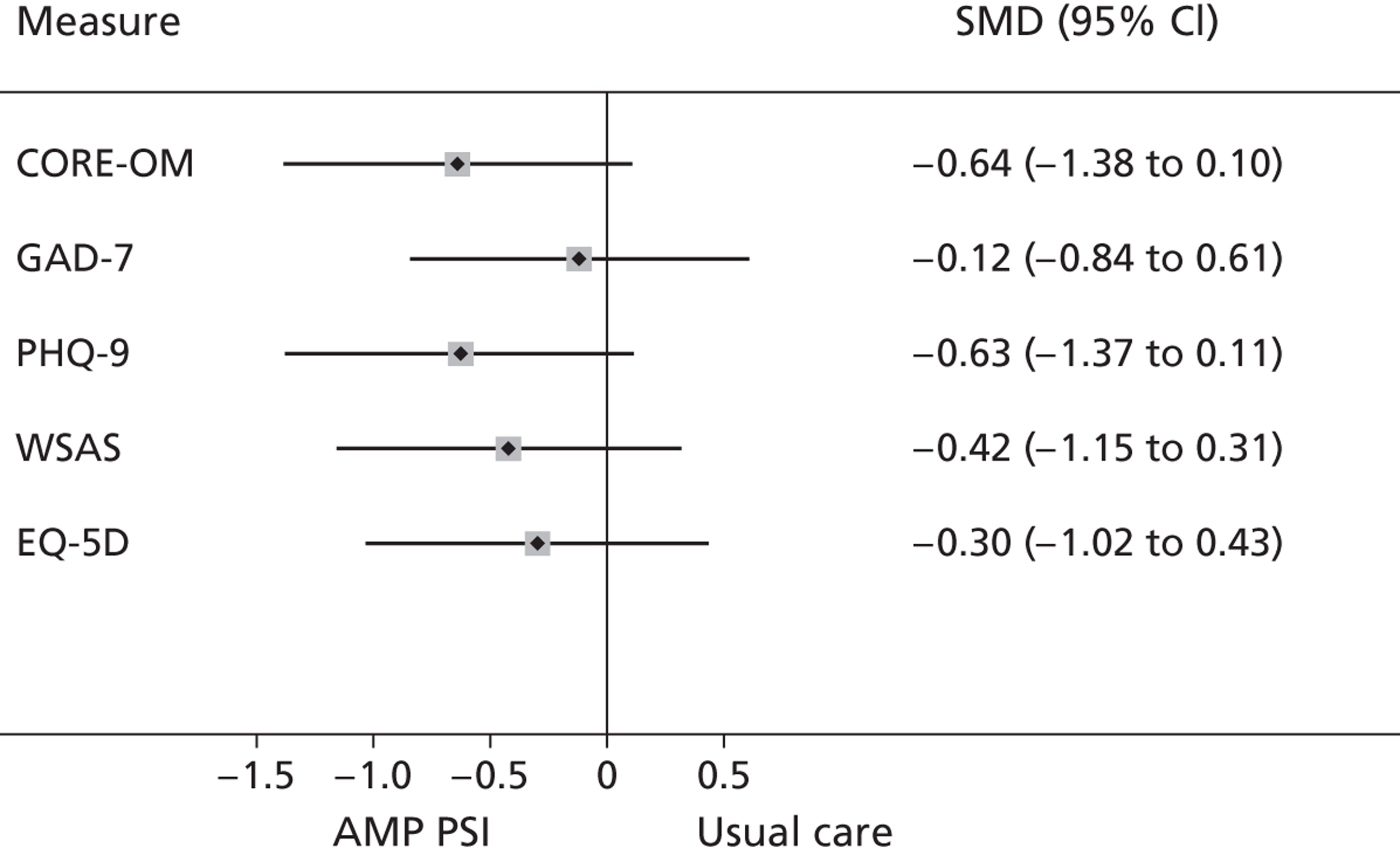
Black and minority ethnic groups
The 20-week outcome data for the BME sample is shown in Table 19. Again, caution must be exercised in the interpretation of these data as the small numbers mean that baseline differences can occur through chance and power to detect differences is limited.
The results are plotted in Figure 20 using a standardised mean difference (effect size) measure. The effects are smaller than those seen in the elders sample. The largest effects are seen for PHQ-9 and EQ-5D, for which the impact of the intervention was similar to that seen in comparative data from primary care. 390 These results are not adjusted for any potential baseline differences.
| Outcome | Well-being intervention, mean (SD), n | Usual care, mean (SD), n |
|---|---|---|
| CORE-OM | 20.98 (7.40), 11 | 20.32 (6.32), 5 |
| GAD-7 | 13.45 (4.53), 11 | 14.00 (4.64), 5 |
| PHQ-9 | 13.99 (4.91), 11 | 16.00 (6.44), 5 |
| WSAS | 22.30 (11.93), 10 | 24.40 (10.45), 5 |
| EQ-5D | 0.35 (0.46), 8 | 0.21 (0.38), 5 |
FIGURE 20.
Forest plot of the effects of the well being intervention on the BME sample. CI, confidence interval; SMD, standardised mean difference.
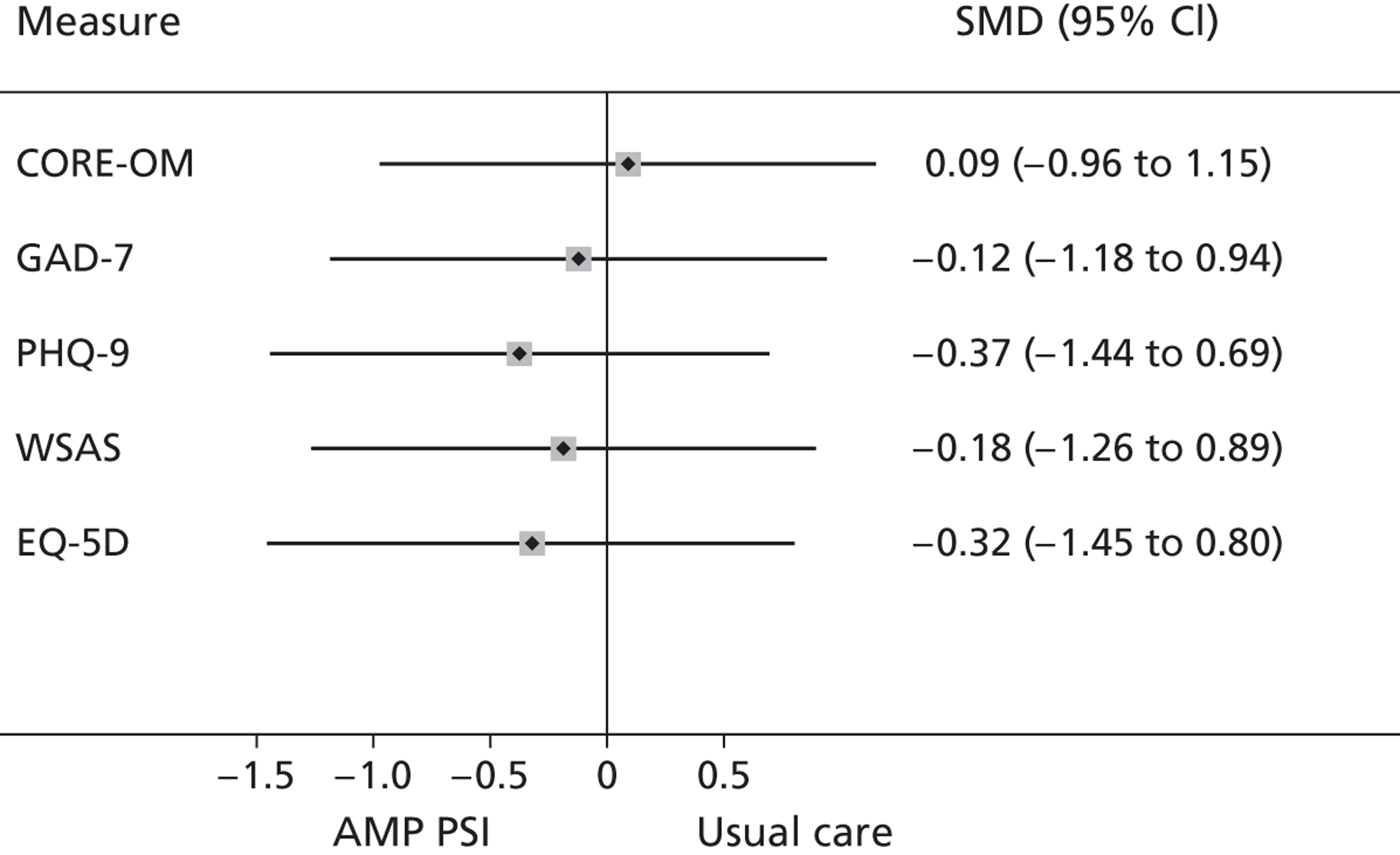
Evaluation
Referral and recruitment
The trial failed to meet the recruitment target. Only 57 eligible participants were recruited, 57% of our target.
We experienced different challenges in the two target groups and across the four sites. The evidence we present here is based in part on our own observations; we also draw on interview data from community and general practice participants (see Chapter 4, Evaluation and Chapter 5, Evaluation).
Wythenshawe
We almost met our randomisation target in Wythenshawe, with 24 randomisations from 34 referrals. Good relationships were built up with one AMP intervention practice, whose GPs made 17 referrals. In early November 2011 we were invited back to the practice to remind all of the GPs about the study, particularly as two partners had been recently appointed. Following this visit, GPs made six referrals in the remaining 2-month recruitment period. In one case a GP telephoned first to discuss a potential referral.
The existence of a long waiting list for the primary care mental health team helped, as GPs recognised that we would contact their patients straight away but that they could simultaneously refer to the primary care mental health team. Good relationships with members of the primary care mental health team brought in five early referrals and two at later points, one of whom was discussed first by telephone. We received nine self-referrals, mainly as a result of posters on medical practice notice boards in the Wythenshawe Forum.
However, there were no referrals from any third-sector organisations despite regular reminders and members of the team attending several meetings and large events in the Wythenshawe area. There was also little engagement with the other three AMP practices. One was an intervention practice where a manager commented:
Maybe you didn't do anything wrong, maybe we just forgot that you were there . . . maybe it probably needs to have been pushed a bit more, because it was a new service, and you know, it's like anything, it has to be at the forefront of their mind for them to use it.
There was no apparent impact of posters in pharmacies or outside the immediate area of the medical practices, or of our newsletters.
Of the 10 patients who were referred but not randomised, five were ineligible (one was too young, three scored below the threshold for eligibility on the PHQ-9 and/or GAD-7 and one was from a practice outside our recruitment area) and a further five did not consent.
Patients required up to an hour to talk about their situation, to understand the study and to ask questions before informed consent was given and eligibility assessed. Patients frequently required reassurance that they would not have to leave their home, that they would be able to have one-to-one rather than group sessions and that the intervention was for people like them, rather than those they perceived to be worse than they were.
Picton
We recruited only one participant in Picton from a total of nine people referred. The recruitment rate was limited by the size of the sampling frame. The Somali population in Picton is smaller than the South Asian population in Longsight. In addition, we found that many Somali patients were registered with another practice, on the border of our study locality.
Other factors that adversely influenced recruitment in Picton were noted in our evaluation interviews. Despite our efforts to meet with members of primary care teams, not all primary care staff were aware of the intervention:
I always sit in on the clinical side but not in the AMP because it was nothing to do with me.
Practice manager
Although many respondents considered the intervention to be welcome, it was seen as less attractive by some community members:
In terms of mental health in itself, people from my community do not trust simply at all, the professional side of it, you know, that is just a no, no.
Community organisation manager
Several GPs reported difficulty in identifying patients of specific Somali heritage, and some found this a frustrating problem. Some respondents were unable to identify the benefit or impact, whereas others saw the Somali focus as having a negative, stigmatising impact on the community:
Cause, you know, when you target something, you kind of like put the spotlight on it [. . .] so which increases the, not the, yeah, not to increase the stigma within the, you know, why are we targeting, say [. . .] is it because we are the most people, you know, prone to become mentally ill?
Community organisation manager
Working through interpreters and the lack of a Somali member of the AMP team were also seen as disadvantageous:
When you bring interpreters that thing kind of creates a barrier because that person does not want to disclose that information to that person, fear of they might go back to the community and they say: ‘You know so and so hiding on this and that’, and that kind of barrier that . . . . If the programme was [. . .] team of people who . . . from the Somali community I think they would have more impact you know than whereas if they employ there other people from the community.
Project worker
Longsight
In Longsight we randomised 19 from 30 referrals. Posters were distributed to practices, mosques, grocery shops, voluntary organisations and the library and the community engagement groups provided a focus for reminding people about the intervention. Many potential participants were not registered with the four AMP practices. One practice was very well engaged and referred 15 people into the study, but there were some communication problems with the other intervention practice with referrals not reaching the AMP team (faxes not received) and this practice referred only two people. As the lead GP said:
We thought that actually it's not right for the patient to refer somewhere where they're waiting for 3 months and not hearing something then they come here and then we have to chase it up and you say ‘oh the referral wasn't received’.
GP
Despite attempts to engage both control practices, no referrals were received directly from them, although their patients entered the study through other routes, including through self-referral, from the primary care mental health team waiting list and through referral from voluntary organisations. The organisation that offered its venue free to run well-being interventions also offered a staff member to co-facilitate the group and a volunteer to help during breaks.
Despite our frequent contacts with practices, including visits from the therapists, two of whom already took referrals from the GPs, and a regular newsletter, some staff still did not feel that they knew enough about the intervention. The randomised controlled design also proved to be problematic, as referral into the study was often assumed (by referrers and patients) to mean that therapy would be provided.
Croxteth
In Croxteth the CFGs were an effective forum for informing local stakeholders about the intervention. The two AMP control practices became engaged with the intervention following meetings with the study co-ordinator and the well-being facilitator, as did members of district nursing teams and third-sector organisations, including a housing trust. Self-referrals were encouraged by some GPs, who saw them as a motivating factor:
In some ways it's actually more likely for them to commit themselves, rather than us filling in the form, if they actually make the decision themselves to go.
GP
Although posters were widely displayed, some respondents thought that they did not adequately explain the intervention. Some GPs were unclear about the nature of the trial or the types of patients for whom it was relevant. This may in part explain the high proportion of inappropriate referrals from one GP, including several patients with severe cognitive problems. One GP expressed the view that some older people were frightened by all of the information (including the consent form) and that this deterred them from taking part in the study:
Some of these older people, I think they got a bit frightened by it [information] and I think it put them off a bit.
Croxteth 003, older patient
Participant perspectives
To explore acceptability from the patients' perspective and to ensure inclusion of patients with a range of baseline characteristics, almost all patients randomised into the trial were invited to participate in interviews. Semistructured interviews with consenting participants were conducted in patients' homes by members of the research team. An interview guide (see Appendix 18) was developed by the trial team to ensure exploration of key areas including experience of barriers to, and enablers of, the well-being intervention. Interviews were digitally recorded and usually lasted between 45 and 60 minutes. We carried out 39 interviews with trial participants as shown in Table 20.
| Group | Location | Gender | Ethnicity | Age range (years) |
|---|---|---|---|---|
| Elders | Croxteth | Female 7, male 1 | White British 7, white German 1 | 57–79 |
| Elders | Wythenshawe | Female 9, male 7 | White British 13, white British/Polish 1, Australian 1, Indian/Caribbean/English 1 | 51–85 |
| South Asian | Longsight | Female 14 | Bangladeshi 7, Pakistani 6, Indian 1 | 24–60 |
| Somali | Picton | Female 1 | Somali | – |
We also offered interviews to all of the well-being facilitators. Semistructured interviews explored key areas including referral to and experiences of the AMP well-being intervention, reservations or concerns about the intervention and whether or not the intervention fit with AMP trainingplus and community engagement.
Two of the supervisors were interviewed about their experiences of supervising the well-being facilitators, and the third provided reflective notes.
Audio tapes of interviews were transcribed verbatim and the transcripts were subjected to a framework analysis (see Chapter 3, Evaluation procedures). Direct quotations have respondent identifiers, with characteristics removed to ensure anonymity.
Accessing the intervention
As indicated by the focus groups (see Developing the intervention), what the intervention was called appeared to be important:
I said I don't know I will have to think about that because I had never heard of AMP so I didn't know what it stood for [. . .]. Whether it stood for someone who is going totally mental and sometimes I thought I was going totally mental.
Liv003, older patient
Recommendation from the GP was important in deciding to participate, and in the case of South Asian women so was discussion with family members:
I've spoken to my husband about it. He said if that is what your doctor has recommended then go and try it. If you speak about your problems maybe your mind will be ‘refreshed’ and you will feel better.
Long005, Bangladeshi patient
The lack of a long waiting list was helpful, as was the option for self-referral:
They never recommended it to us in the first place you know cause they were in one of the practices in included in the programme but they never recommended it to us uh you know so that's why I thought well I'd go and see if we were eligible to go on it.
W19, older patient
Promoting access
South Asian participants made several suggestions for promoting the intervention in their community. These included educating husbands in mental health, audio information for less literate people and use of Islam:
I think you need to advertise it in a way so that other people in the family do not have a problem with this type of programme. I think you can also get family support by using Islam to promote the issue/programme. Because a lot of people are very quick to dismiss something that is different or new, but if you say well in Islam or in the Quran this is what is written and this is how we must behave, they start to listen and think okay this is important for me too.
Long27, Bangladeshi patient
Location
For older people in particular, travelling to a venue was sometimes challenging and required planning. For both elders and BME patients, the flexibility of the AMP therapists in being able to see people at home was important. For the latter this was in contrast to what we expected from the focus group, at which participants had thought that there would be difficulties with home appointments.
Both elders and BME patients preferred face-to-face to telephone contact and almost all of the therapy in both groups was provided in this way. The atmosphere of the venue for therapy (both one-to-one and group) provided by voluntary organisations was very much appreciated:
A warm friendly feeling . . . you go some places you don't get that warm friendly feeling at all it is a friendly atmosphere there's I've not found anybody stabbing one another's back.
W004, older patient
Appropriateness of therapy
Cultural fit was a major issue for the South Asian women:
Our culture is very different to this English culture. The problems and issues I was going through was something very common . . . so if I talk about it with them I don't think they will realise my state of stress and depression and may think that I am exaggerating things. Men and women in Western societies think differently about issues we are very conservative about and I don't think they understand our family systems and issues. So it is better to talk to someone who can make out what you are going through.
Long006, Pakistani patient
Women who spoke Urdu, Punjabi or Hindi could be seen by a therapist who spoke their language, whereas Bangla, Sylheti and Somali speakers were seen with an interpreter. Not everyone found the interpreter to be a barrier. The Somali patient was comfortable with the interpreter, who also facilitated meetings with the researcher. However, the interpreter was a problem for some:
I would prefer someone from our own ethnicity and someone who knows the culture well. There are so many sensitive issues that they won't be able to understand and plus the way we talk in our own language you can't say things fluently if you don't know the language well.
Long006, Pakistani patient
Therapist fit
As in all psychological therapies, the fit between patient and therapist was an important factor in both satisfaction with the intervention and promoting recovery:
I think she is very supportive she is a very nice girl. Even though she is a white person I know that she sympathises with me and understands my illness. When I am uncomfortable you can tell that she feels my pain, she does not have to say it but you can just tell can't you?
Long008, Bangladeshi patient
Although most experiences were positive, this was not universal:
I think she was trying the best she could but I did find her overpowering [. . .] I just said I found it she was asking me to do things that I didn't really feel capable of doing . . . I didn't feel able to talk to her because I felt she was too young and she wouldn't understand.
W014, older patient
Intervention content
Participants generally perceived the choice and specific content of the well-being intervention to be appropriate, acceptable and helpful. The therapeutic model was acceptable to the Somali patient, and within South Asian culture in Longsight:
Yes definitely I would strongly recommend it. It has proved very beneficial to me and I think this is what people need in time of stress to come out of it and gain confidence. What I was going through I thought I will never come out of it but individual therapy helped me in gaining my confidence and becoming stable again.
Long006, Pakistani patient
It was possible to identify from the interviews the active elements of behavioural activation being used and sustained:
She sort of got me going doing things . . . balancing me day out and making a chart out of the week and doing that when I feel a bit down now I refer back to that and make a chart for myself just to get me moving.
W004, older patient
Therapeutic group interventions
The groups were popular with those who attended, although not everyone felt able to engage. We found evidence of benefit from groups being co-facilitated by an AMP therapist and a worker from a partner third-sector organisation, as this helped to overcome the perceived stigma associated with a ‘well-being’ group.
After the intervention
Most participants expressed the view that the well-being intervention was not long enough and that they would have preferred some kind of follow-up intervention or a ‘tailing off’ of contact with the therapists. However, some participants became actively involved in other activities and expressed a desire to volunteer with these groups:
I started the craft group and um been doing sort of things since AMP.
W005, older patient
Finally, there was concern about potential loss of funding for the organisations that provide language and culturally appropriate support for the community:
Please do something about the groups so that they keep on going I have been hearing that there is no funding, and soon such services will not be available for us. What will we do?
Long002, Pakistani patient
Reflections from therapists and supervisors
For those therapists who had previously received IAPT or similar training, the interventions used in the programme were similar; however, there was much more emphasis on case management, particularly in the elders group, and on visiting at home, which rarely happens in current step 2 IAPT services. For the therapists from the third sector, many of the interventions were novel, but they had greater experience in group work.
The levels of unmet need and the mental and physical multimorbidity and severity of mood symptoms were ‘eye-opening’ both for the therapists and for the supervisors. It was apparent that many people referred into the study would not have been able to access usual services and required a much more proactive approach to engage them. The therapists valued the flexibility of being able to provide longer sessions than they would usually do and the regular supervision that they received. The lack of psychological therapy for the population of Bangladeshi women in Longsight, many of whom were isolated, severely depressed and unable to speak English, was also a major unmet need identified, with very few signposting options for this group. However, the therapists involved in delivering the group interventions felt that these had been effective and well received, for both the elder population and the South Asian women.
Discussion
We developed and evaluated a psychosocial intervention tailored to older people and people from BME communities. We synthesised data from previous work streams to design the intervention protocol, refined this with help from focus groups and developed a training package for mental health workers. We then conducted an exploratory trial to test the intervention protocol.
We found that the well-being intervention could be delivered as planned. It was generally acceptable to patients and there was evidence of adherence. The majority of patients preferred one-to-one sessions, although the options for group work and signposting were valued.
We investigated parameters for a definitive trial of the intervention protocol through examination of recruitment rates and a comparison of outcomes between patients receiving the intervention and those in usual care. Evidence from our quantitative analyses indicated that patients offered the well-being intervention showed greater improvement than those offered usual care, with the largest effects seen for reduction in depressive symptoms. The magnitude of difference was comparable with that seen for other psychosocial interventions in primary care. 390 Our evidence of effect sizes will be helpful in estimating sample sizes for a future definitive trial.
Despite considerable effort on the part of the AMP research team, our recruitment rates were lower than anticipated. Recruitment to primary care trials in the UK is routinely problematic, and is particularly difficult for mental health trials. 393–395 Therefore, determining recruitment rates and the most effective recruitment strategies are critical steps in the development of a definitive trial. However, available evidence to support recruitment strategies is sparse. 396
In other mental health trials we have found that successful recruitment has been achieved by mass-screening lists of registered primary care patients,397 which results in a large numbers of recruits, although the overall response rate tends to be low. Although it might be possible to adopt this strategy for older people, who do tend to register in primary care, our knowledge of the barriers to recruitment identified in earlier stages of the AMP project made such an approach problematic. Mass screening would also be less likely to reach underserved members of BME communities who may not have registered as patients with primary care teams or, if they have, may not be readily identifiable from practice lists. Therefore, the current recruitment rates should be seen in a context in which one of the most effective strategies was not available.
The relatively high number of self-referrals was a positive finding, although many of these did not translate into randomised participants. In Chapter 7 we discuss the reasons for and implications of this finding.
Recruitment would have been enhanced if the design of the evaluation had allowed the inclusion of more practices, as we had numerous enquiries from potential participants who were not registered with one of our 16 practices. Recruitment would also have been enhanced by having a better knowledge of those practices that members of the Somali and South Asian communities tended to register with.
Many trials report initially poor levels of recruitment. Recruitment over a longer period (e.g. 18 months) would enable GPs to become used to the referral process and the service, and to receive positive feedback from their patients, potentially encouraging further referrals. It would also help to simplify the eligibility criteria. For example, in Croxteth and Picton, certain postcodes were initially specified. This caused problems and was soon changed so that a patient's postcode made no difference to his or her eligibility. Providing explicit information about the referral process during the AMP training sessions enabled receptionists and administrative staff to know exactly what was required (in one practice two referrals went astray and resulted in the GP losing confidence with AMP). Arranging for the GPs to meet the well-being facilitators at an early stage may also help – as, for example, in Croxteth – so that they know who will be working with their patients.
Cultural issues were of great relevance. On the one hand, it is important to ensure that well-being facilitators are seen as culturally appropriate by the local communities. This applies as much to older indigenous populations as to particular BME groups. On the other hand, our experiences may support an argument for reducing the cultural specificity of well-being interventions. There is a trade-off between specificity and potential sample size (most evident for the Somali community). Reducing specificity would also limit the risk of a particular community seeing itself as stigmatised, rather than prioritised, by the offer of an intervention. However, it is also clear that for the South Asian participants cultural specificity was valued and seen as important. Different strategies may therefore be needed to engage particular communities.
It should be noted that attrition rates at the first follow-up were not unusually high, despite the difficulties experienced in engaging these groups. Minimising attrition is essential to ensuring that baseline comparability provided through randomisation is maintained, and that the sample size achieved at recruitment is not significantly reduced in the main analysis. The study suggests that, although there is still work to be done in encouraging these groups into trials, their experience once recruited may not lead to particular problems of retention. However, it is possible that the low levels of recruitment reflect engagement of a very select group of patients in the trial and the low level of attrition might be a particular characteristic of that group; the low level of attrition might not generalise if wider participation is achieved.
Chapter 7 Integrating the AMP model
Introduction
We now consider the extent to which the different elements of the AMP Development Partnership may have impacted on each other to increase equity of access to mental health services through primary care and improve the quality and responsiveness of those services.
As we demonstrated in Chapter 2, two main barriers to equity of access are lack of information and multiple forms of stigma, whereas a major facilitator is the communicated availability of acceptable mental health services. 346 In Chapter 3 we provided our rationale for implementing a complex intervention model with three interlinked components (Figure 21).
FIGURE 21.
Multifaceted model of care.

In Chapters 4–6 we have explained how each component of the model was developed and assessed. The next challenge was to develop ways of evaluating this model, capturing both process and outcome and enabling the interactions between levels to be assessed.
If we take Figure 21 as a metaphor for the possible mechanisms of the AMP Development Partnership, we can see it as a set of interlinked cogs within a gearing system. A gear is a rotating machine part having cut teeth, or cogs, which mesh with another toothed part to transmit torque. Two or more gears working in tandem are called a transmission; they can produce a mechanical advantage through a gear ratio and thus may be considered a simple machine.
One way of looking at this model is to assume that the community engagement cog starts the process in motion, driving the primary care cog, which in turns drives the psychosocial intervention cog. However, because all cogs are interlinked, it is possible that activity in any one can influence the activity and speed of any others, and that concurrent activity in two could substantially affect the speed of the third. Conversely, lack of activity in one cog could reduce or stop the transmission of torque elsewhere in the system.
Improved responsiveness in a system like this can have several different outcomes, and hence can be viewed from several different perspectives. It would be possible to examine community-level outcomes, for example changes in the level and experience of mental health stigma within local communities, or changes in the extent of self-help activity at local community level. Given that the focus of our programme was on increasing equity of access to high-quality mental health services through primary care, we decided in this report to focus on the two most directly relevant outcomes: the extent to which the integration of the AMP model affected access to psychosocial interventions sensitive to the needs of underserved groups; and the extent to which the model impacted on the quality of mental health-care delivery within primary care overall.
Access to the well-being interventions
The assumption underlying the combined AMP model was that increased access to the well-being interventions would be related to the intensity of the other two AMP interventions. Therefore, we would expect access to the well-being interventions to be higher in the localities that were offered the AMP community engagement programme and for patients registered with practices that participated in AMP trainingplus; and highest for those who were in a position to benefit from both community engagement and practice training activities.
Consequently, we focus on patterns of referral and recruitment into the well-being interventions.
Referrals to the well-being interventions were more likely to come from the two localities that were offered the community engagement intervention. Figure 22 shows that there were a total of 80 referrals from these localities (50 in Croxteth and 30 in Longsight) compared with a total of 43 from the other two localities (nine in Picton and 34 in Wythenshawe). Not all referrals came through the practices. Referrals did not appear to be influenced by whether or not practice teams had been offered AMP trainingplus. There was no difference between the combined number of referrals from the practices offered AMP trainingplus and the combined number of referrals from the practices not offered the training intervention.
FIGURE 22.
Referrals to the AMP well-being intervention by locality and practice. Numbers in rows are of practice referrals. Numbers in columns are of locality referrals.
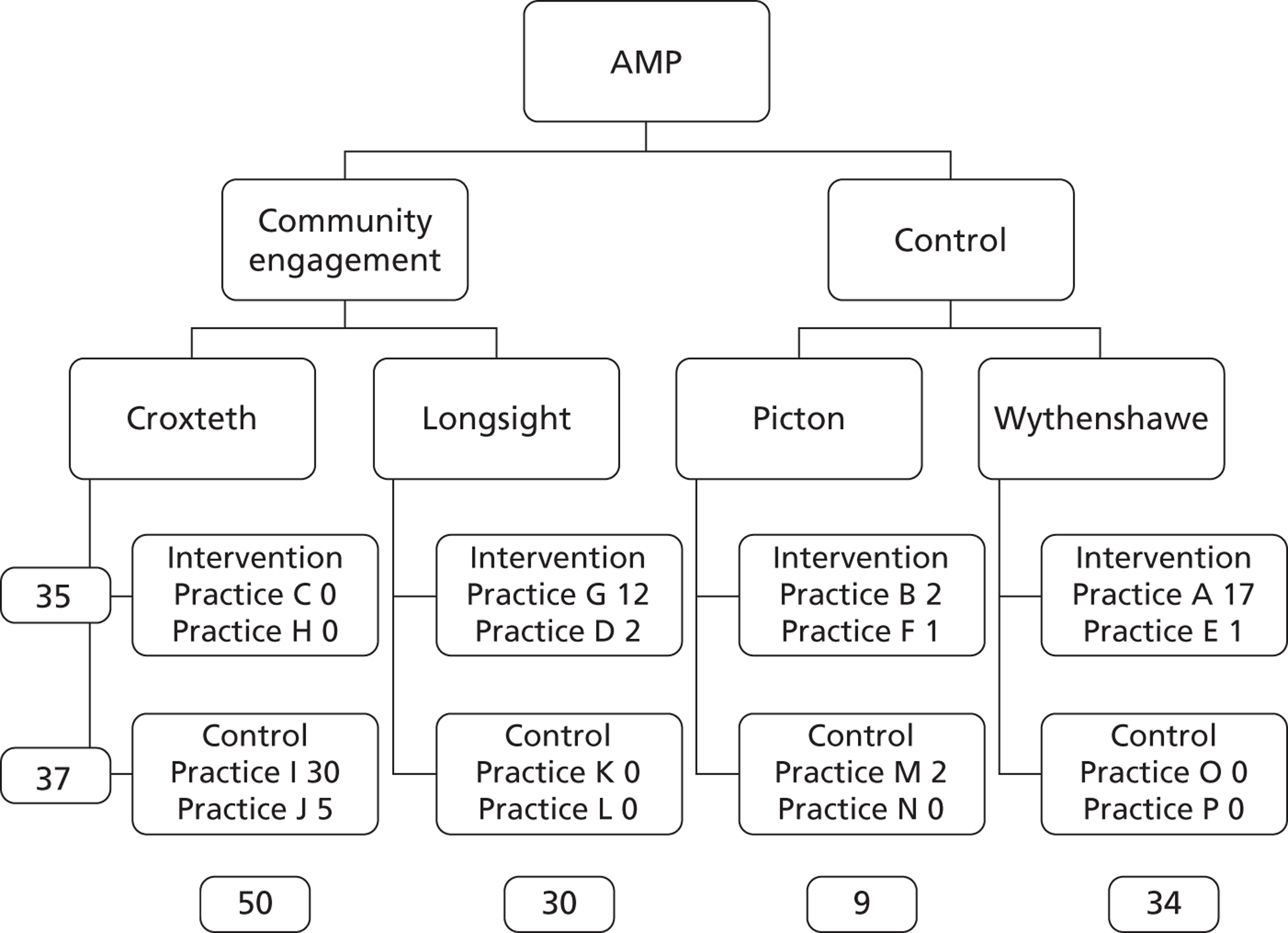
Recruitment to the well-being interventions, in contrast, was associated with the offer of AMP trainingplus, but not with community engagement. As we can see from Figure 23, 41 (72%) of the 57 participants recruited were registered with one of the practices offered the AMP training programme, whereas only 16 (28%) were registered with a practice not offered the training. Thirty-two (56%) of the recruited participants came from one of the two localities that had received the community engagement intervention, whereas 25 (44%) came from one of the other two localities.
FIGURE 23.
Recruitment to the AMP well-being intervention by locality and practice. Both column and rows numbers are of patients registered with practices.
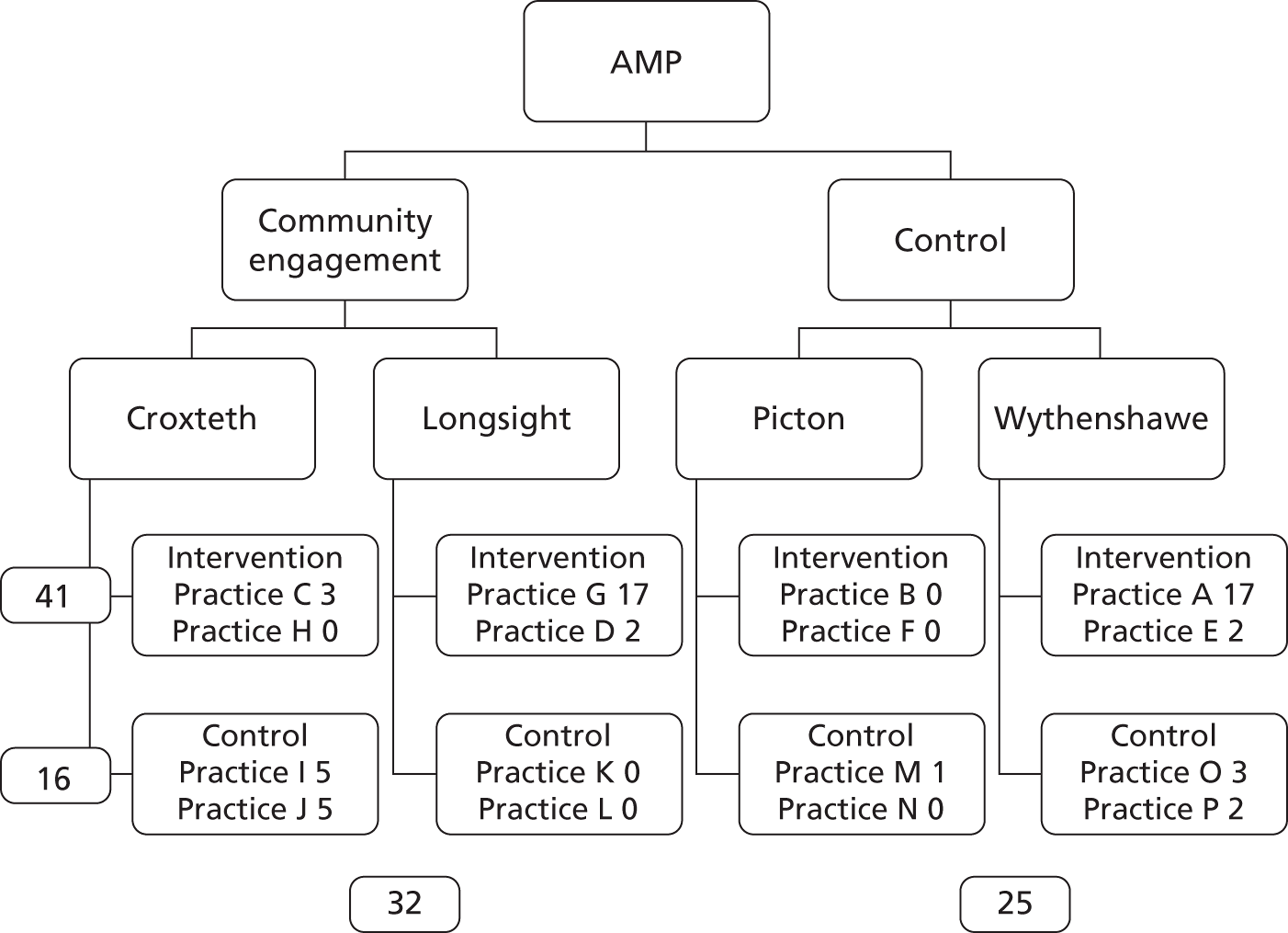
Synthesised analyses of our evaluation interviews provide a set of explanations for these divergent quantitative findings, which can be grouped under the headings of awareness, acceptability and authority.
Awareness of the existence of the AMP well-being intervention appeared to be more influenced by the community engagement intervention than by the practice training intervention. This may be partly because all of the 16 AMP practices were invited to refer patients to the well-being intervention, regardless of whether or not they were invited to participate in AMP trainingplus. The absence of a community engagement intervention in Picton, combined with the fact that many members of the Somali community gather information by word of mouth rather than through written materials, were likely to have contributed to low levels of awareness of the well-being intervention in that locality.
There appeared to be similar levels of acceptability at community and practice levels. There was evidence of considerable enthusiasm among many community organisations for the psychosocial intervention.
A participant with a community role with a housing trust in Wythenshawe told us:
The first problem [with depression] is people don't know that they've got it. They just think they're going through a low period in their life and they're just sad or . . . a turn of events: you lose your job . . . but I think the great thing that you're doing is you're trying to catch them before they go into that severe depression stage, and work on them mild to moderate before they're at that severe stage. You know, where they feel like they can't do anything. You're sort of hitting them mild to moderate where, you know, they're feeling low and it's about changing their mindset. And I work with other organisations with cognitive behavioural therapy and it's about making them aware of how they're feeling and changing that into a positive. So I think it's a great idea.
A service commissioner in Liverpool told us:
I think about the whole thing . . . so the AMP is improving access to mental health and primary care and then you have got the well-being facilitators . . . and . . . really exciting and well done for the bit that says in our, you know, here are the . . . facilities, here are the local things that we have in our local community . . . which for us in a practical world is really helpful. Really helpful for GPs, really good to say, listen here's, you know, here's what you've got . . . Then they have got the well-being facilitators . . . and the people who offer the therapy sessions – I think they are the same people.
Acceptability was enhanced by word-of-mouth reports from participants in the well-being intervention, who subsequently encouraged friends to self-refer.
However, other community stakeholders, particularly in Picton, were concerned about the potentially stigmatising effects of an intervention targeted at a specific ethnic minority. A Somali British woman told us:
Yes definitely you're making them very, very isolated because you're going after them as a group, I could see it now where this project would be like running after Somali, stop it's a well-being project here, don't you want to get involved, and they're like why do we need the well-being project, but if you stopped like ten people at the door who were a mix of people, multicultural people and you said to them this is this project is available I really think you should be interested, would you put your name down to just come and see, then you're more likely to get more people actually wanting to attend so I think that's a better way of doing it.
Concern was also expressed by potential service users that self-referral to the well-being intervention could result in a negative reaction from the primary care team, and the risk of being denied access to future primary health care.
Although practice teams were generally aware of the availability of the AMP well-being intervention, their views of its acceptability to the practice team varied. Variations in practice perspectives on its acceptability appeared to relate to three factors: workload prioritisation, which was usually dependent on the enthusiasm or otherwise of the practice manager; ease of navigation, which was particularly problematic in Picton where several GPs reported that their practice record systems made it difficult for them to readily identify patients from Somali backgrounds; and variable trust in the perceived efficacy of the intervention.
A sense of authority was stronger in primary care than among community organisations or potential self-referrers. GPs in particular are used to making decisions about whether or not and when to refer on to other agencies, whereas members of community organisations often do not feel sufficiently responsible or powerful to do so.
A community worker in Wythenshawe told us:
I suppose when it first started we thought the GPs were going to initially be doing that [referring].
A project worker in Liverpool said:
If there was anyone that I was sort of concerned about, I always discuss it with the vicar. And, you know, if there's anything we can do in that way then by all means, but I wouldn't be making decisions by myself; I don't think it would be part of my role.
General practitioners who had been offered AMP trainingplus were thus in a particularly strong position to make effective referrals insofar as their sense of authority was combined with a greater awareness of the types of patient who would be likely to need and benefit from a culturally sensitised psychosocial intervention.
Impact of the well-being intervention on community engagement
We found that participation in the well-being intervention had an impact on the community engagement arm of the AMP Development Partnership. Some well-being intervention participants felt sufficiently empowered by their experience to offer their time to work with local community organisations to raise awareness about mental health issues. Two Pakistani women said:
I can work as a volunteer I know what depression is what people go through and what can help to recover really have that experience after so many years. The AMP group and the Roby group are really good ones and I would suggest people to join them.
Long002
I can work as a role model for people and can voluntarily come to your group sessions and tell the participants how I overcame my depression naturally with the help of you people and you have made me strong honestly.
Long006
A well-being facilitator in Wythenshawe said:
I think for one particular client the fact that it was in the building was a really positive thing and I think if it hadn't if the sessions hadn't been held there I'm not sure the outcome would've been as positive [. . .] I think because the sessions were actually held there she got to meet some of the staff and she became quite involved with Age Concern and I think she felt quite empowered [. . .] It wasn't about being a recipient of an older person's service she could actually contribute to it.
Mental health care within primary care
When thinking of how the community engagement and psychosocial components of the AMP Development Partnership affected the primary care element, we should not use the metaphor of cogs and gears too rigidly, to imply that these were fixed entities. Rather they represent a dynamic set of processes. The components or strands did not routinely have set or rigid boundaries, much as threads are not always visible or separable within an overall fabric. They were defined rather by ongoing negotiation of boundaries between and within the three strands, so that they shaded into each other.
We should note that this complex interplay was to a large degree prescribed by the model itself and the underlying intention to promote opportunities for fruitful dialogue. Such interplay was effected in localities by (and depended on) individual research staff, health workers, etc., moving virtually, and sometimes physically, between community, primary care and well-being ‘spaces’. Movement in such cases was modulated by many factors, including assigned roles and priorities and perceived relevance in respect of the process and content of ‘other’ strands. It was also constrained by such roles and priorities: as a GP from Practice B noted, involvement in AMP-related meetings came ‘at the expense of time actually seeing patients’.
There were four main ways in which the primary care strand (AMP trainingplus) was affected by the other strands of the AMP model: community mapping, the well-being intervention, CFGs and understanding the AMP model.
Community mapping
Community mapping or information gathering was carried out in all four localities and in two of the localities it was a precursor to community engagement activities (see Chapter 4, Information-gathering findings). This proved very useful in the context of AMP trainingplus practices, where locality resources and service provision were chosen as the focus of training sessions by several teams. Discussion of local service provision sometimes arose or was prompted during the initial training session, accompanied by views of a rapidly changing landscape in which GPs were not necessarily informed when services were no longer available. The practices expressed clear needs for accessible, updated information on current service provision.
The AMP research staff who carried out locality mapping attended selected training sessions. Benefits were reported by primary care teams in terms of providing them with new information on local resources. The evidence of practical usefulness was additionally helpful in demonstrating some mutual benefit of study participation, thus challenging a view of practices and staff simply as ‘sites’ and ‘subjects’ of research.
The well-being intervention
The offer of the well-being intervention (see Chapter 6, Testing the intervention) was a useful means of initial engagement with primary care teams. As in the previous section, we were able to position the programme as offering a service to, not just conducting research on, the team.
However, as we have already seen in Chapter 5 (see Discussion), implementation of the well-being intervention was more problematic than the offer of information from our community mapping exercises. One obstacle was that primary care staff could not be certain that referred individuals would be eligible for the service (if entry criteria were not subsequently met) or would be offered the service (if patients were randomised to the control group). Some help was needed to guide practice staff through the documentation and to ensure and explain that programme staff would complete as much of this as possible.
Second, the well-being intervention was not embedded in the everyday practice of GPs and they saw it as requiring extra time and effort in an already busy environment and hence it was easily forgotten (see Chapter 6, Well-being outcomes). Some expressed the view that more time was required for the well-being referral system to be embedded, as well as seeing benefits of more direct and frequent contact with well-being facilitators.
Third, feedback suggested some difficulty in identifying suitable candidates for the well-being service and, specifically in Picton, those of Somali heritage. One of the practices considered that there would be benefits from a more inclusive approach in regard to nationality or ethnic target groups:
I think the problem is because it's just a specific group of patients . . . Although we have got Somali patients, they are not, we have also got a massive group of other patients from ethnic minorities . . . And I did think at the time it might have been, because I think when I first went into the first one I didn't realise it was going to be specifically for the Somali population . . . And that probably narrowed it really.
GP, Practice F
Some general reasons for the enhanced randomisation of patients from training practices to the well-being intervention have been identified (see Access to the well-being interventions). In addition, at the practice level, the service was probably better publicised in the training practices – through information provided with the initial invitation and through the first and any subsequent training presentations. We do not have direct evidence of an effect due to increased knowledge and skills of GPs as a result of participating in the training element of AMP trainingplus, although a general increase in awareness would perhaps constitute a desirable training outcome in itself.
Consultative focus groups
We found differing trends in respect of interaction between the CFG element of the AMP community engagement strategy and participation in AMP trainingplus and the well-being intervention.
In Longsight, the initial involvement of members of primary care teams in CFGs encouraged their later participation in AMP trainingplus. Senior staff in Practice G had initially expressed reservations about taking up our offer of training, but decided to accept the offer after some of them found direct benefit from taking part in the first Longsight CFG.
In Croxteth, by contrast, our active ‘selling’ of the well-being intervention to both training and control practices (see Chapter 5, Ethnographic observations) encouraged the later participation first of community nursing staff and later of GPs in CFG meetings. The evidence for this can be tracked through the attendance of community nurses and GPs at the Croxteth CFG meetings (see Table 7). In the case of the community nurses, this provided possibilities for engaging with members of the primary care team whom we had not managed to contact through direct approaches to the practice.
Understanding the AMP model
When thinking about the ways in which the three strands inter-related, we should also consider the complexities inherent in understanding and promoting the ‘complete’ model. This includes the extent to which we were able to put across the objectives of the model and its component parts. The presentation and ‘selling’ of the model in the primary care setting was sometimes challenging in respect of both its scope (potentially a broad remit that could encompass a wide range of activities) and also its specifics (which were deliberately left unfinished to allow tailoring to practice needs and context).
Implementing the AMP Development Partnership represented one extreme of a continuum in respect of the work entailed in marketing and implementation of – or normalising – new health-care interventions. 398 At the other end we might have a relatively finished and concrete example, such as a new prescription medicine, for which the uses and market niche are well defined and the prescriber can trial the product with relatively little disruption to everyday practice. Towards the centre of the continuum we might find instances such as telecare or educational packages that have more profound implications for changes in existing roles and workload, but which are nevertheless discrete and relatively specific. The AMP model takes this several stages further, with its ambition to promote change not only in terms of individual working practices, but also within organisational systems and relationships between practices and their local communities.
In some cases primary care teams did not have a full understanding of the model and its components. This was probably not helped by the variation in terminology used within the programme, for example the well-being intervention was also sometimes referred to as a psychosocial intervention. In practice, this was partly an ‘academic’ point, in that the decision whether or not to engage with the AMP programme was probably guided by factors other than the level of understanding of the model's underlying concepts. However, this did become a factor in the evaluation interviews, when teasing out views of impact necessarily involved exploring awareness and comprehension of the three model strands. Even when participants were confident that they had understood the AMP model, it is not clear that this was in fact the case:
Yes, yes it was absolutely fine and we got the whole concept of, you know it was more to try and get, particularly the elderly population out and the ones who got mental health issues and they weren't accessing the system. So we knew exactly what it was all for, yes.
GP, Practice E
Conclusions
Referrals to the well-being intervention appeared to be enhanced by our community engagement strategies, whereas recruitment was more likely for patients registered with practices that were offered AMP trainingplus. These differences were related in part to a greater sense of enthusiasm among community groups, in contrast to a greater sense of authority bestowed on and perceived by GPs.
The finding that receipt of a well-being intervention could have an impact on participation in community activities emphasises the potential fluidity of roles with the AMP model,372 especially beyond the medical zone of care. It also links to our findings from phase 1 (see Chapter 2) on the value of helping others as a way to support personal recovery.
With regard to the impact of the other elements of the AMP model on primary are, our analysis suggests that our community mapping activities were seen as strongly positive from a primary care perspective; the offer of the well-being intervention was initially welcomed but was seen by many GPs to contain various difficulties in terms of opportunities for recruitment; and there were clear, though varying, benefits from the interaction between practice training and participation in CFGs. It was not clear that GPs and other members of primary care teams fully grasped the implications of the overall AMP model; however, it was also unclear whether, or to what extent, that mattered in terms of their involvement and commitment.
Further analysis is needed on the impact of the primary care and well-being intervention elements on the community engagement element of the AMP Development Partnership. Further research is needed to clarify and extend the tentative conclusions that we have drawn in this chapter. These matters are discussed further in the next chapter.
Chapter 8 Putting what works into practice
Introduction
In phase 3 of our programme we moved from experimentation to implementation. We used evidence gained from phase 2, together with our knowledge of and experience in the diffusion of innovation377,399,400 to inform implementation strategies at three complementary levels:
-
we developed an educational intervention, a web-based resource pack on ‘how to do it’, linked to local stakeholder meetings
-
we undertook policy interventions at local and national levels
-
we initiated service interventions to implement key aspects of the AMP development model in differing clinical contexts.
In this chapter we describe these initiatives. We then make recommendations for future research in this field and reflect on the implications of the AMP programme for policy and practice.
Educational intervention
Our aim in creating a dedicated AMP website was to describe what we did within the AMP Development Partnership to inform and change professional attitudes and behaviour. Our intended audience was the range of specialist and non-specialist mental health staff working in primary care, and also academics and policy-makers in a position to influence practitioners.
Working with an information technology specialist, we describe the key elements of the interventions, which we have described in detail in the previous chapter of this report. The home page introduces the AMP model and explains how and why we developed it. The next pages present the three elements of the model and explain our evaluation procedures. We then give pictorial and verbal descriptions of the four intervention localities. We have included pages for study findings as they emerge and for further information, including AMP-related publications. There is also a members area and frequent opportunities for site visitors to print or comment on particular pages and topics. The website can be viewed at www.amproject.org.uk (accessed 10 June 2013).
The AMP website went live on 9 June 2012. We launched it through our national and international academic and policy networks. We highlighted it within our presentations of the AMP programme at two stakeholder events in Croxteth and Picton in mid-June. Both meetings were held in community venues relevant for the study target groups. These were attended by 25 members of third-sector organisations, three primary care practitioners, five primary care commissioners, two city councillors and others including housing association managers and study participants. We also linked it to the Facebook and Twitter groups set up by the Longsight CWG (see Chapter 4, Community intervention findings).
We also held two stakeholder events in Manchester in September 2012. We invited service users and providers, including patients recruited to the well-being intervention, local residents and service providers who participated in go-along interviews, all four practice teams in each area, participants in our focus groups and working group, people we met during the community mapping phase, and others representing organisations working with older people and the South Asian community. We presented key findings from all three strands of the AMP programme and two patients spoke at each meeting to share their experiences of receiving the well-being intervention. The meetings included questions and discussion.
Feedback on the website has been very positive. By 31 July 2012 there were 613 page views on the website, by 90 unique visitors. An international primary care leader commented: ‘Beautiful “human” stories. Impressive how you have found a consistent integrative line to make it possible to specify and diversify according to local conditions.’
We will keep track of web-related activity to identify where, when and how our AMP website influences attitudes and practice in the field of primary care mental health.
Policy interventions
In this section we describe the impact of the AMP programme on policy at both local and national levels.
Local policy impact
The AMP programme was set up from the start to encourage a close working relationship with local policy stakeholders. The funding for the programme was directed through Liverpool Primary Care Trust and we included senior clinical managers from both Liverpool Primary Care Trust and NHS Manchester as programme principal investigators. Our explicit intention was to maintain dialogue and interdependence, to enable rapid implementation of key findings as they began to emerge from the phase 2 experimentation stage of the AMP programme.
We now illustrate the impact of this relationship by describing how it enabled the AMP team to have a major influence on a review of primary care mental health policy in Liverpool.
Ongoing engagement
There was early and sustained engagement between the AMP team and representatives of Liverpool Primary Care Trust at different levels. At the managerial level, the programme was supported by the PCT's medical director and by its research and development (R&D) lead. During phase 1 and phase 2, we also had active liaison with the trust's director of stakeholder engagement, public health neighbourhood manager and community development workers, as well as members of its social prescribing group and its teams for integrated, mental health and public health commissioning and for delivering race equality.
We found the following benefits from this engagement as phase 2 of the AMP programme unfolded:
-
There were early synergies between the AMP development model and the trust's strategic direction, which is built on a neighbourhood management model. 401,402
-
Our community engagement activity in Croxteth, especially the CFG meetings and the active role of the AMP community champion (see Chapter 4, Community intervention findings), helped to strengthen relationships between the trust and third-sector organisations. In so doing it embedded key features and messages of the AMP development model, especially the active linking function.
-
AMP trainingplus activities raised awareness about the AMP well-being intervention and the important role of third-sector organisations in providing emotional, practical and social support for underserved groups in primary care settings.
Liverpool primary care mental health and well-being strategy
Our ongoing negotiations and discussions with PCT commissioners, as research findings emerged from the evaluation of the AMP development model, provided empirical evidence to support the trust's evolving strategy for primary mental health and well-being. This culminated in the active involvement of members of the AMP team in planning and delivering a series of three workshops between May and July 2011.
These workshops were designed to develop a coherent pathway for mental health service provision (both within and without primary and secondary care) with local buy-in from service providers. The workshops were well attended, with energetic participation from 99 third-sector organisations and specialist psychological and secondary care mental health providers.
The agreed pathway that emerged from these workshops closely followed the AMP development model (Figure 24). It includes multiple entry points and referral routes, an emphasis on collaborative care and the introduction of new mechanisms to encourage greater use of non-statutory service providers. Community resources are seen as central to the proposed model of care.
FIGURE 24.
Model of care proposed by the Liverpool primary care mental health and well-being strategy. CMHT, community mental health team; CW, community worker; EIT, early intervention team.
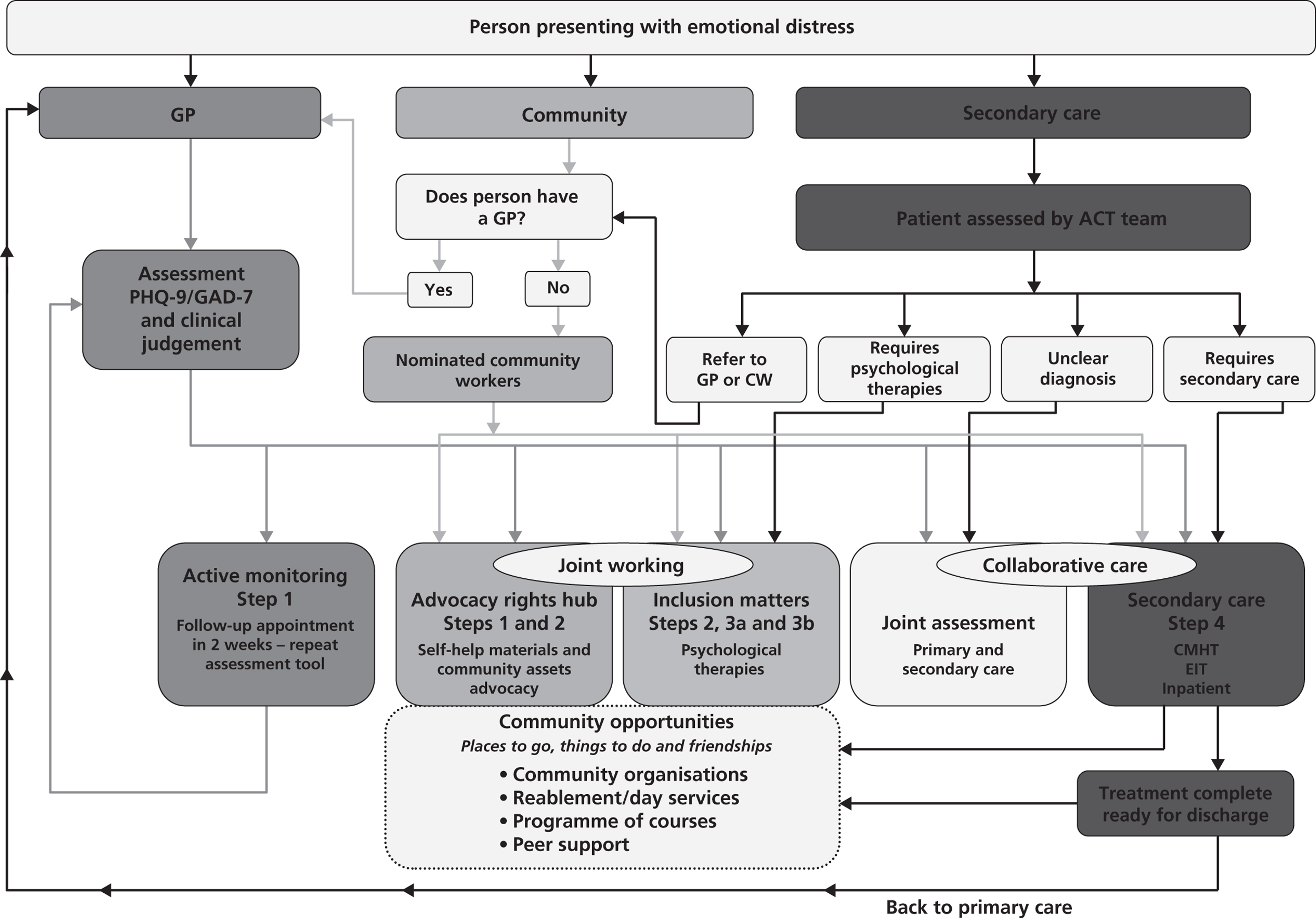
This pathway has subsequently been confirmed as being central to the primary care mental health strategy for Liverpool Primary Care Trust.
The aim of the strategy is to deliver a coherent and neighbourhood-based care pathway for primary mental health and well-being. Its core elements are:
-
a practical offer to reduce social exclusion
-
a social offer to reduce social isolation and promote health and well-being
-
a psychological offer to provide access to evidence-based psychological therapies
-
an integrated offer of primary and secondary care work together.
Changing contexts
It is important to be mindful of political, economic and organisational changes and their potential impact on the implementation of this agreed policy. Since the summer of 2011, major changes have occurred in the organisation of primary health care and in the amount of funding available to statutory and voluntary bodies. These have posed risks to the successful implementation of Liverpool Primary Care Trust's primary care mental health strategy:
-
Following the passage of the 2012 Health and Social Care Act, Liverpool Primary Care Trust ceased to exist on 30 March 2013. 403 Many of its functions will be taken over by the newly formed Liverpool CCG. It is not yet clear how the CCG will approach commissioning for primary care mental health.
-
A consortium of service improvement and development staff, service users and stakeholders, under the protectorate of the trust's Integrated Commissioning Team, currently act as a patient ‘watchdog’. The future of this group, including its stakeholder engagement function, is uncertain.
-
The city council has gone through major workforce reduction, based on the need to save over £140M between 2011 and 2013. This major reduction in costs has put third-sector, non-statutory services at risk, including many of those identified as crucial to the delivery of the primary mental health and well-being strategy.
National policy impact: National Institute for Health and Care Excellence guidance
During 2010–11, Linda Gask was a member of the guideline development group for the National Institute for Health and Care Excellence (NICE) guidance on common mental health disorders35 and led on the development of the section on access to health care. Outputs from the first phase of the AMP programme were available to inform this section and the conclusions from the AMP programme about the ways in which access might be improved were important in informing the background and scope of the reviews that were carried out for this guideline. The NICE guidance also provides important reciprocal support for the need to address issues of access to primary mental health care for underserved populations in the community, for which the developments in the intervention phase of the AMP programme offer us some potential solutions.
Service interventions
Embedding AMP interventions in partner localities
A key challenge for the AMP programme has been to work with our local partner organisations to deliver a legacy from the programme in the localities in which we have worked.
In Croxteth our partnership with the community centre where all of the CFGs and many of our one-to-one well-being sessions were held has encouraged local service providers to continue to refer potential clients to our well-being facilitator, now working there in a voluntary capacity.
In Longsight we have maintained the CFG into the final phase of the project and are seeking to ensure that its work in linking local organisations is continued through the development of the ‘Mental Health in South Asian Communities’ Facebook page (see Chapter 4, Community intervention findings).
Our partner third-sector organisation, which worked with us in delivering the group well-being intervention, has run two further AMP format groups since the end of the pilot trial and is also using elements of the model in other group interventions. Previously these groups were largely run as support groups; these are the first groups that have been informed by cognitive–behavioural principles.
The groups have not been formally evaluated, but common themes have been noted by the two facilitators. Participants speak of feeling unappreciated and guilty, feeling a sense of failure and a lack of self-worth, avoiding social contacts and having difficulty establishing goals for themselves. Helping participants to challenge these beliefs has been a key focus for the group, with emphasis on self-acceptance, sharing information and opening up to new experiences. The aim for future groups will be to extend the duration from eight to 12 sessions, following feedback from participants and facilitators that eight sessions are insufficient.
Service development informed by the AMP programme: Eis Ledaber
Six Degrees Social Enterprise has used the AMP model to inform the development of a service specifically tailored for the Jewish community in Salford. Greater Manchester is home to the UK's second-largest Jewish community, many of whom live in the Higher Broughton and Kersal localities of Salford, where they form the largest ethnic minority group in the city.
Historically it has not been easy to engage the community with mental health services. Stigma remains a major issue, and people with mental illness are often not referred until they are more severely ill. We facilitated a focus group with three members of the team, two of whom are directly involved in providing the service to the Jewish community, to try and capture the key learning points about the utility of this model for a completely different population.
Six Degrees, which provides the local step 2 IAPT service through its primary care mental health team in Salford, had previously worked with an orthodox former member of the team (who has trained as a cognitive–behavioural therapist) to set up a group intervention. He had adapted a generic self-development programme called STEPS to make it culturally acceptable within the Jewish community, but referrals were still low. Following a community stakeholder meeting at which barriers and potential solutions were identified, further support was obtained from NHS Salford, who funded the employment of a community engagement worker and encouraged the service to move forwards with the project.
The AMP model helped both to legitimise the approach that had been taken thus far in setting up the culturally adapted psychosocial intervention and to inform its further design, with the confidence of the local commissioners:
In terms of the overall orientation and how to go about doing things, that was a help – the [AMP] model – and just knowing you've got to look towards working with people from where they are at.
Chief executive, Six Degrees
The team working with the community now has four members, three of whom are training or have already qualified as psychological well-being practitioners (PWPs), and one of whom is a CBT therapist. They work closely with the local rabbis to gain their approval of the intervention.
Community engagement
The team links with GPs, third-sector organisations and other NHS providers to try to combat stigma and facilitate negotiation of culturally acceptable pathways to care for people with mental health problems. A newsletter is published every 6 weeks.
Working with primary care
This has recently started, with the aim of engaging the primary care staff working within the two main practices that serve the community. The senior doctors in these practices are embedded within the community and in the past have been reluctant to refer to third-sector services. But the population is growing, newer staff members are joining and it has become easier to engage staff and reassure them about what is on offer:
We want to have an open and transparent relationship with the GPs – we will let them know what we are doing, what they can get from the service and how they can refer . . . with the knowledge there is going to be a permanent qualified practitioner within the service . . . there will be four people who they know themselves – we are personally known to the GPs . . . so it's the feeling that I know these people I feel a bit more comfortable to refer.
Community engagement worker/trainee PWP
Psychosocial interventions
Individual and group sessions are available. One-to-one therapy is provided by one of the three orthodox Jewish PWPs working with the service and referrals can be made in a range of different ways, through GPs, the third sector, religious workers or self-referral, as recommended in the recent NICE guidance35 for promoting access in hard-to-reach populations (which itself was informed by the AMP project). Having more than one worker is important, as for some people the need for cultural understanding can be offset by fears about confidentiality. As one PWP who has previously worked as a practice manager for a local primary care team explained:
I am able to have that understanding of the cultural background without the patient feeling I know all their family and mixing on a social level . . . we've been able to provide choice.
Coming from a similar cultural background is seen as very important.
There are a lot of nuances, words, facial expressions which only people in that community might pick up. The best practitioner in the world won't be able to get those nuances because they are kind of so specific.
Community engagement worker/trainee PWP
The group intervention continues to be available for each gender. It is facilitated by the CBT therapist, who has specifically adapted it to this population using Jewish stories and perspectives to illustrate themes and ideas.
Six Degrees has published information about Eis Ledaber (see www.amproject.org.uk; accessed 10 June 2013). Further work is needed to formally evaluate this project, which has made considerable progress since its inception.
Recommendations for research
Our high-level conclusion from the AMP programme is that innovative and complex interventions aimed at service design need an innovative and complex combination of methods to enable robust assessment and evaluation. We consider that our combination of methods has been imaginative, original and fit for purpose.
Our work to understand the problems of increasing equity of access to primary care mental health services, described in Chapter 2, involved a combination of scoping reviews of published quantitative literature, a meta-synthesis of qualitative literature, a grey literature review, secondary comparative analyses of existing qualitative data sets and qualitative analysis of new interview and focus group material.
Our evaluation of the linked components of the AMP Development Partnership, described in Chapters 3–7, was based on a multilevel quasi-experimental design, which gave us the ability to test the component parts of the intervention separately and in differing combinations. It then involved the deployment and subsequent analytical fusion of comparative case studies, ethnographic investigations, qualitative analysis of new interview material (gathered from focus groups and individual respondents), descriptive quantitative analysis of routinely collected data and statistical evaluation of our pilot RCT.
Our evaluations have addressed the majority of the research objectives that we set for the AMP Development Partnership. They have also led to further questions, which, in combination, create a substantial agenda for future research into effective service redesign for primary care mental health services, with a focus on increasing equity of access for underserved groups.
Our community engagement model (see Chapter 4, Community engagement model) needs to be replicated and tested in other geographical areas, including rural as well as urban communities, and with a focus on differing underserved groups. It could also be usefully applied to other health priorities, for example cardiovascular disease or diabetes, for which inequities of access are known to exist.
Although we have argued that all four steps contained within our community engagement strategy were necessary to achieve maximum benefit, we cannot be certain that this was the case. Scaling up community intervention strategies across a considerably larger number of localities would allow for study designs that included some or all of the components, and would provide the opportunity to compare, for example, strategies with or without community mapping as a first step. It would also provide evidence to support or refute our assertion that a differentiation of function between CFGs and CWGs is the most effective means of delivering locally meaningful change.
Before AMP trainingplus (see Chapter 5, AMP trainingplus) can confidently be recommended as a template for quality improvement in primary care, it would benefit from replication with other primary care teams and across commissioning groups, perhaps with a focus on other underserved groups and different health priorities.
Although we consider that the initial ethnographic component was necessary to promote effective engagement, as we did not randomise at this level we do not know that this was the case. Similarly, although we found evidence of impact of – and synergies between – all three elements of the training programme, our study design did not allow for scrutiny of the independent effect of each element. Future large-scale studies should include quasi-experimental designs within similar primary care quality improvement initiatives to assess the separate and combined effects of these various elements.
Our quantitative measures of primary care outcomes were limited. Future studies should consider more detailed, systematic approaches to routine data collection than were possible in this programme.
Our design for a set of well-being interventions (see Chapter 6, The well-being intervention) with a focus on specific underserved groups had demonstrable validity and acceptability with most of the communities to which it was offered. Further qualitative investigation is needed to clarify the reasons why acceptability varied between different cultural groups, and to increase knowledge of cultural differences in understanding of mental health and attitudes towards help-seeking.
The apparent effectiveness of the well-being interventions, as assessed in our pilot trial, indicates that they are worthy of further investigation in larger RCTs. The results of the pilot trial will be helpful in determining sample sizes for future trials.
We are confident that psychosocial interventions can and should be revised to make them more relevant to the needs and expectations of differing cultural groups. However, further consideration needs to be given to two aspects. The first is whether or not the range of individual, group and signposting options is necessary for all populations, given that most participants opted for individual sessions with some signposting options. The second is how to deal with the need for cultural specificity of the psychosocial intervention without the perception of stigmatising of that population by publicly focusing on the nature of its difficulties. There are also difficulties in carrying out RCTs in populations with limited engagement in and understanding of research.
Our combined AMP model, with its simultaneous community, primary care and psychosocial interventions and its layered experimental design, is unique. We have demonstrated the internal added value of this combined approach in relation to its effects on increasing access to psychosocial interventions and enhancing the quality of primary care. Further analysis is needed to elucidate the impact on local communities in terms of increasing health literacy and reducing stigma, as well as to elucidate the optimal modes of ‘active linking’ between relevant local organisations. Work is also needed to estimate the economic impact of the AMP model in terms of direct costs and benefits of consequent changes in health-care use and indirect societal costs and benefits.
Although we have indicated the feasibility of the application of this model in related local contexts, before it can confidently be proposed as an effective method for increasing equity of access to high-quality primary mental health care it needs to be applied and rigorously tested in other settings. Our focus has been on underserved or marginalised groups in urban settings within a relatively prosperous country with a strong infrastructure of primary care services and a relatively well-developed range of existing psychological therapies. It is not clear how well our model would operate in countries where primary medical care is less developed or where there is little access to any psychological therapies. We have noted that third-sector organisations, crucial to the success of our community engagement strategies, are particularly vulnerable to change in economic circumstances; thus, their capacity is likely to vary depending on socioeconomic circumstances operating far beyond the control of research teams.
Our evaluation process was both necessary and useful, but it did carry risks and limitations. First, the inherent complexity of the process rendered analysis challenging. We needed to exercise careful judgement when drawing inferences across and between differing methodological perspectives, and to remain aware of the requirement to draw pragmatic conclusions of relevance to health-care planners and policy-makers. Second, it involved a perpetual balance or tension between achieving the core aim of the AMP programme – to increase equity of access to high-quality primary care mental health services – while maintaining sufficient flexibility to engage and maintain effective partnerships with our research stakeholders.
Although generalisation of our findings is permissible, it is essential to remain mindful of their contextual nature. The three elements of the AMP Development Partnership would have the same general structure if applied in other localities, or with a focus on other underserved groups, but the details of their content and processes, and hence their anticipated outcomes, would have been different. This would have been so within the confines of the AMP programme if our randomisation processes had led to the full community engagement strategy being offered in Wythenshawe and Picton instead of Croxteth and Longsight; if a different set of practices had been randomised to the offer of AMP trainingplus; or if our focus for the well-being intervention had been on other underserved groups. A fortiori, it will be the case for others planning to redesign primary mental health-care services and improve access for underserved groups elsewhere in the world.
Implications for policy and practice
Community engagement
The main implication of our findings concerning engagement within the AMP Development Partnership is that mental health expertise exists in communities, but needs to be nurtured. We found many examples of third-sector organisations with considerable and culturally relevant understandings of mental health problems experienced by their local communities. They also had practical experience in offering suitable help, even if it was not always couched in mental health terms. However, the volatile and precarious existence of many third-sector organisations means that they require nurturing if they are to flourish. Nurturing involves not only high-level encouragement but also the availability of resources. At a time when there are many uncertainties and organisational changes in health and social care, community interventions promoted by research groups provide an opportunity for local services to build and rebuild local contacts, and to develop knowledge, relationships and trust.
With regard to the model of community engagement that we have proposed and tested, we consider the following to be key elements for success:
-
The independence of the community champion from the research team is an important element in fostering and maintaining engagement and trust, and in confronting any conflicts, problems or disagreements that may arise.
-
It is helpful if the community champion is not allied with, and therefore seen as too closely identified with, the agenda of one particular local interest group.
-
By working closely with local organisations it is possible to harness their existing expertise and to ensure that the skills developed stay in the community for the future.
-
University research partners provide local organisations with access to new expertise, training and working methods, and with opportunities to build new relationships and partnerships with other agencies.
-
A focused strategy helps to raise the agenda of mental health and well-being among the many other priorities in areas of multiple deprivation.
Primary care quality
The main implication of our findings in relation to primary care is that primary care is necessary but not sufficient. Primary care retains a position of authority within underserved communities but it is not always the fulcrum of activity regarding common mental health problems. It may best be seen as one (albeit important) of a number of points of access to high-quality mental health care.
With regard to the implementation of training programmes based on AMP trainingplus, our experience leads us to propose the following steps:
-
Identify the scope and particularities of the issues to be addressed, including gathering and understanding evidence and its local relevance. This involves community mapping along the lines of the first step in our community engagement strategy.
-
Identify target practices based on mapping the population of underserved groups, in conjunction with local primary care commissioning groups or organisations.
-
Send letters of invitation to senior partners and practice managers along with written material explaining the purpose and nature of the training intervention. If the practice is in agreement, arrange one or two pre-meetings to introduce the research team and answer questions.
-
Negotiate the possibility of carrying out ethnographic observation before training starts.
-
Facilitate practical arrangements for this and any subsequent sessions (rooms, equipment, refreshments, etc.) and offer financial reimbursement to the practice for staff participating in training and related activities.
-
The initial training session should set out the research team's agenda, report on ethnographic observations, discuss learning needs and explore the potential for further training.
-
Feedback from and to the practice should be provided after each training session.
-
Arrange further training meetings as agreed, develop content and arrange guest speakers as required.
-
Maintain contact with the practice and offer further support and training, including options for further development after the formal training is completed.
If the training is part of a wider programme, based on the full AMP Development Partnership, then there are also important opportunities to encourage links with the other arms of the programme, by offering referrals to psychosocial interventions and linkages with local community resources.
Psychosocial interventions
The main implication of our findings in relation to psychosocial interventions is that they can – and should – be adapted to meet the needs of underserved groups. We have demonstrated that it is possible to create culturally appropriate versions of validated psychosocial interventions, and that doing so increases their acceptability among marginalised groups. Our pilot study also suggests that adapted psychosocial interventions may be effective in reducing common mental health symptoms and increasing well-being for members of these groups.
Our practical recommendations for the implementation of culturally sensitised psychosocial interventions include:
-
Use focus groups with members of relevant community groups to ensure that the content and form of the proposed interventions are culturally acceptable.
-
Use simple criteria for referral of patients so as not to create additional barriers and workload for GPs in identifying suitable patients.
-
Referral to the well-being intervention should be enabled through multiple routes, including self-referral.
-
An initial patient-centred assessment session should be held with a well-being facilitator, including a collaboratively devised well-being plan.
-
Incorporate flexibility in delivery in terms of the number and length of sessions, providing home visits as required and gradual phasing out of sessions if appropriate.
-
Ideally, an intervention should be provided by therapists who are able to speak the patient's language. (We were particularly concerned by the absence of NHS-funded therapists in Manchester with the ability to provide psychological therapy in the native language of Bangladeshi women, despite the considerable unmet mental health-care needs in this population.)
-
Incorporate a well-being plan that specifies desired health- or social-care changes, based on self-identified goals.
-
Significant emphasis should be placed on the patient as the agent of change, incorporating the patient's previous experiences and coping strategies into the designated interventions.
-
Stigma, expectations and illness trajectory should be addressed as this is important in engaging patients.
-
Once the goals have been identified allow participants to choose one or more ways to obtain support to achieve them.
-
If groups are to be an option, consider linking with suitable existing groups rather than setting them up de novo.
-
The role of the well-being facilitator is to engage, support, advise and actively follow-up patients.
-
A key function of the well-being facilitator is to liaise with other health- and social-care professionals who are, or need to be, involved in a participant's care. This usually includes the patient's GP.
-
Regular and timely communication with GPs helps build relationships of trust between well-being facilitators and practices and encourage further referrals.
-
If the patient is taking prescribed antidepressant or anxiolytic medication, the well-being facilitator encourages guideline-concordant medication used in liaison with the GP.
The AMP Development Partnership
Taking the AMP model as a whole, we have demonstrated that it is possible to intervene simultaneously at three different levels: community, primary care and psychosocial therapy. We have also shown that our multilevel intervention was greater than the sum of its parts, and that it increased equity of access to high-quality primary care mental health services. Primary care teams were sensitised to the needs and perspectives of underserved groups and gained a greater awareness of the availability and range of community-based resources. Access to culturally relevant psychosocial interventions was enhanced by engagement with community and primary care organisations.
The NHS in the UK is currently undergoing a period of rapid transformation, including the introduction of CCGs404 and the promotion of the policy of ‘any qualified provider’405 for the delivery of health care. This may therefore be a propitious time to propose a radical redesign of existing services. The AMP Development Partnership, with its emphasis on building partnerships between primary health care and community organisations, stands as an promising example for commissioners or providers wishing to fund or deliver innovative new service configurations designed to improve the mental health of members of underserved and marginalised groups.
In addition to the intrinsic value of our programme's content for advancing the priorities and needs of the NHS, we consider that it may be a useful model for co-operation between local communities and academic institutions. 406 The AMP programme provides supportive evidence of the prosecution of primary care research and development activities through partnership with health-care and third-sector providers. This can be seen as a ‘civic engagement’ role for the universities concerned, which often forms part of the overall university strategic objectives, including widening participation and partnership with local organisations. It is an example of the ways in which universities may engage ethically and effectively with their local communities.
Acknowledgements
We acknowledge the contributions of:
-
the AMP programme team (past and present), including Noreen Asghar, Najia Atif, Katie Bristow, Amy Catlin, Siobhan Connor, Anna Dowrick, Tom Dowrick, Louise Fisher, Emma Funnell, Maureen Glendinning, Margaret Goddard, Simon Gowers, Christina Ireland, Nicky Lidbetter, Claire McMyler, Kirsten McNicol, Rajan Madhok, Gabrielle Marr, Maxine Martin, Tim Millar, Rahena Mossabir, Bushra Nazir, Susan Newall, Faran-Ebi Pumude, Brian Spurgin, Naomi Wells and Alex Williams
-
the AMP advisory board, academic collaborators and external experts, including Ricardo Araya, Ann Casebeer, Linda Davies, Dawn Edge, Sandra Fortes, Jane Gunn, Gabriel Ivbijaro, Tony Kendrick, Sing Lee, Helen Lester, Carl May, David Morris, Elizabeth Murray, Don Nease, Sarah Peters, Joanne Reeve, Richard Riley, Anne Rogers, Peter Salmon, Greg Simon, Chris van Weel and Ken Wilson
-
the primary care teams and the many other stakeholders in the cities and localities where we undertook our research.
Finally, we are grateful for the support of Ksenia Orekhov and the National Institute for Health Research team supporting the Programme Grants for Applied Research programme.
Contribution of authors
All authors made a substantial contribution to the concept and design of the study or the acquisition of data or the analysis and interpretation of data, and drafted the manuscript or revised it critically for important intellectual content. All have given final approval of the version to be published.
Professor Christopher Dowrick (Primary Medical Care) coled the programme and the co-ordination of this report.
Professor Carolyn Chew-Graham (Primary Care) led the primary care element of the programme and the phase 1 secondary qualitative analysis and primary data collection.
Professor Karina Lovell (Mental Health Nursing) led the psychosocial intervention element of the programme.
Dr Jonathan Lamb (Research Associate) led the qualitative meta-synthesis, coled the framework analysis and took responsibility for drafting the community engagement element of the report.
Mrs Saadia Aseem (Research Assistant) contributed to the scoping quantitative review and the BME psychosocial evaluation.
Dr Susan Beatty (Research Associate) led the quantitative data gathering for the primary care evaluation and contributed to the other elements of the intervention.
Professor Pete Bower (Primary Care) led the scoping reviews and the quantitative analysis of the psychosocial intervention.
Dr Heather Burroughs (Research Fellow) coled the framework analysis and contributed to the community engagement interventions.
Ms Pam Clarke (Research Assistant) contributed to the initial stakeholder interviews, the community engagement intervention and the older people's psychosocial evaluation.
Dr Suzanne Edwards (Senior Research Fellow) supported the programme co-ordination and contributed to the community engagement and primary care interventions.
Professor Mark Gabbay (Primary Care) supported the development and management of the programme and critically reviewed the report.
Ms Katja Gravenhorst (Research Assistant) contributed to the primary care element of the intervention.
Mr Jon Hammond (Research Assistant) contributed to the primary care element of the intervention.
Dr Derek Hibbert (Research Associate) led the grey literature review and coled the primary care element of the intervention.
Dr Marija Kovandžić (Research Fellow) led the qualitative secondary analysis and contributed to the community engagement and primary care interventions.
Professor Mari Lloyd-Williams (Palliative Care) supported the development of the programme and critically reviewed the report.
Dr Waquas Waheed (Psychiatry) contributed to the community engagement and primary care elements of the programme.
Professor Linda Gask (Primary Care Psychiatry) coled the programme and the co-ordination of this report.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, CCF, NETSCC, PGfAR or the Department of Health.
References
- World Health Organization International Consortium in Psychiatric Epidemiology . Cross-national comparisons of the prevalences and correlates of mental disorders. Bull WHO 2000;78:413-26.
- Murray CJL, Lopez AD. The global burden of disease. Boston, MA: World Health Organization and Harvard University Press; 1996.
- Mental health and social exclusion. London: Office of the Deputy Prime Minister; 2004.
- Shiels C, Gabbay MB. Patient, clinician and general practice factors in long-term certified sickness. Scand J Public Health 2007;35:250-6. http://dx.doi.org/10.1080/14034940601072364.
- Layard R. The case for psychological treatment centres. BMJ 2006;332:1030-2. http://dx.doi.org/10.1136/bmj.332.7548.1030.
- Lelliott P, Tulloch S, Boardman J, Harvey S, Henderson M, Knapp M. Mental health and work. London: Royal College of Psychiatrists; 2008.
- Depression: management of depression in primary and secondary care (update). London: NICE; 2009.
- Generalised anxiety disorder and panic disorder (with or without agoraphobia) in adults. London: NICE; 2011.
- Gilbody S, Whitty P, Grimshaw J, Thomas R. Educational and organizational interventions to improve the management of depression in primary care: a systematic review. JAMA 2003;289:3145-51.
- Richards A, Barkham M, Jane C, Richards D, Williams C, Heywood P. PHASE: a randomised, controlled trial of supervised self-help cognitive behavioural therapy in primary care. Br J Gen Pract 2003;53:764-70.
- Araya R, Rojas G, Fritsch R, Gaete J, Rojas M, Simon G, et al. Treating depression in primary care in low-income women in Santiago, Chile: a randomised controlled trial. Lancet 2003;361:995-1000. http://dx.doi.org/10.1016/S0140-6736(03)12825-5.
- Salmon P, Dowrick CF, Ring A, Humphris GM. Voiced but unheard agendas: qualitative analysis of the psychosocial cues that patients with unexplained symptoms present to general practitioners. Br J Gen Pract 2004;54:171-6.
- Husain MI, Waheed W, Husain N. Self-harm in British South Asian women: psychosocial correlates and strategies for prevention. Ann Gen Psychiatry 2006;5.
- Carta M, Bernal M, Hardoy M, Haro-Abad J. Migration and mental health in Europe. Clin Pract Epidemiol Ment Health 2005;1.
- Fazel M, Wheeler J, Danesh J. Prevalence of serious mental disorder in 7000 refugees resettled in western countries: a systematic review. Lancet 2005;365:1309-14. http://dx.doi.org/10.1016/S0140-6736(05)61027-6.
- Caring for dispersed asylum seekers: a resource pack. London: Department of Health; 2003.
- Bhui K, Shanahan L, Harding G. Homelessness and mental illness: a literature review and a qualitative study of perceptions of the adequacy of care. Int J Soc Psychiatry 2006;52:152-65. http://dx.doi.org/10.1177/0020764006062096.
- Fisher K, Collins J. Homelessness, health care and welfare provision. London: Routledge; 1993.
- Gowers S, Bryant-Waugh R. Management of child and adolescent eating disorders: the current evidence base and future directions. J Child Psychol Psychiatry 2004;45:63-8. http://dx.doi.org/10.1046/j.0021-9630.2003.00309.x.
- Fairburn CG, Harrison PJ. Eating disorders. Lancet 2003;361:407-16. http://dx.doi.org/10.1016/S0140-6736(03)12378-1.
- Chew-Graham C, Baldwin R, Burns A. Treating depression in later life. BMJ 2004;329:181-2. http://dx.doi.org/10.1136/bmj.329.7459.181.
- Wilson K, Mottram P, Sixsmith A. Depressive symptoms in the very old living alone: prevalence, incidence and risk factors. Int J Geriatr Psychiatry 2007;22:974-9. http://dx.doi.org/10.1002/gps.1682.
- Lloyd-Williams M. Depression: the hidden symptom in advanced cancer. J R Soc Med 2003;96:577-81. http://dx.doi.org/10.1258/jrsm.96.12.577.
- Lloyd-Williams M, Shiels C, Dowrick C. The Brief Edinburgh Depression Scale (BEDS) as a screening tool in patients with advanced cancer. J Affect Disord 2009;113:127-34.
- Shiels C, Gabbay MB, Ford FM. Patient factors associated with duration of certified sickness absence and transition to long-term incapacity. Br J Gen Pract 2004;54:86-91.
- Ring A, Dowrick CF, Humphris GM, Davies J, Salmon P. The somatising effect of clinical consultation: what patients and doctors say and do not say when patients present medically unexplained physical symptoms. Soc Sci Med 2005;61:1505-15. http://dx.doi.org/10.1016/j.socscimed.2005.03.014.
- Peters S, Rogers A, Salmon P, Gask L, Dowrick C, Towey M, et al. What do patients choose to tell their doctors? Qualitative analysis of potential barriers to reattributing medically unexplained symptoms. J Gen Int Med 2009;24:443-9. http://dx.doi.org/10.1007/s11606-008-0872-x.
- Eating disorders: core interventions in the treatment and management of anorexia nervosa, bulimia nervosa and related eating disorders. London: NICE; 2004.
- Chew-Graham C, Bashir C, Chantler K, Burman E, Batsleer J. South Asian women, psychological distress and self-harm: lessons for primary care trusts. Health Soc Care Community 2002;10:339-47. http://dx.doi.org/10.1046/j.1365-2524.2002.00382.x.
- Sihota S, Linnard L. Health literacy: being able to make the most of health. London: National Consumer Council; 2004.
- Lester H, Bradley CP. Barriers to primary health care for homeless people – the general practitioner perspective. Eur J Gen Pract 2001;7:6-12.
- Goldberg D, Jenkins R, Griffiths S. Indicators for mental health in the population. London: HMSO; 1991.
- Goldberg D, Huxley P. Common mental disorders: a biosocial model. London: Routledge; 1992.
- Thompson C, Kinmonth A, Stevens L, Peveler R, Stevens A, Ostler K, et al. Effects of a clinical practice guideline and practice-based education on detection and outcome of depression in primary care: Hampshire Depression Project randomised controlled trial. Lancet 2000;355:185-91. http://dx.doi.org/10.1016/S0140-6736(99)03171-2.
- Common mental disorders: identification and pathways to care. London: NICE; 2011.
- Priest R, Vize C, Roberts A, Roberts M, Tylee A. Lay people’s attitudes to treatment of depression: results of opinion poll for Defeat Depression Campaign just before its launch. BMJ 1996;313:858-9. http://dx.doi.org/10.1136/bmj.313.7061.858.
- Lovell K, Richards D. Multiple access points and levels of entry (MAPLE): ensuring choice, accessibility and equity for CBT services. Behav Cogn Psychother 2000;28:379-91.
- Department of Health . Quality and Outcomes Framework n.d. www.dh.gov.uk/en/Healthcare/Primarycare/PMC/Quality/OutcomesFramework/index.htm (accessed July 2012).
- Dowrick C, Leydon G, McBride A, Howe A, Burgess H, Clarke P, et al. Patients’ and doctors’ views on depression severity questionnaires incentivised in UK Quality and Outcomes Framework: qualitative study. BMJ 2009;338. http://dx.doi.org/10.1136/bmj.b663.
- Clark D, Layard R, Smithies R, Richards D, Suckling R, Wright B. Improving access to psychological therapy: initial evaluation of two UK demonstration sites. Behav Res Ther 2009;4:910-20. http://dx.doi.org/10.1016/j.brat.2009.07.010.
- Kaltenthaler E, Parry G, Beverley C. Computerized cognitive behaviour therapy: a systematic review. Behav Cogn Psychother 2004;32:31-55. http://dx.doi.org/10.1017/S135246580400102X.
- Bower P, Gilbody S. Stepped care in psychological therapies: access, effectiveness and efficiency: narrative literature review. Br J Psychiatry 2005;186:11-7. http://dx.doi.org/10.1192/bjp.186.1.11.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. http://dx.doi.org/10.1136/bmj.a1655.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review – a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy 2005;10:S21-34. http://dx.doi.org/10.1258/1355819054308530.
- Gulliford M, Figueroa-Munoz J, Morgan M, Hughes D, Gibson B, Beech R, et al. What does ‘access to health care’ mean?. J Health Serv Res Policy 2007;7:186-8. http://dx.doi.org/10.1258/135581902760082517.
- Dowrick C. Beyond depression. Oxford: Oxford University Press; 2009.
- Peters S, Rogers A, Salmon P, Gask L, Dowrick C, Towey M, et al. What do patients choose to tell their doctors? Qualitative analysis of potential barriers to reattributing medically unexplained symptoms. J Gen Intern Med 2009;24:443-9. http://dx.doi.org/10.1007/s11606-008-0872-x.
- Burroughs H, Lovell K, Morley M, Baldwin R, Burns A, Chew-Graham C. ‘Justifiable depression’: how primary care professionals and patients view late-life depression? A qualitative study. Fam Pract 2006;23:369-77. http://dx.doi.org/10.1093/fampra/cmi115.
- Gabbay M, Shiels C, Bower P, Sibbald B, King M, Ward E. Patient-practitioner agreement: does it matter?. Psychol Med 2003;33:241-51. http://dx.doi.org/10.1017/S0033291702006992.
- Lloyd-Williams M, Payne S. Can multi-disciplinary guidelines improve the palliation of symptoms in the terminal phase of dementia. Int J Pall Med 2002;8:372-5.
- Watters C. Emerging paradigms in the mental health care of refugees. Soc Sci Med 2001;52:1709-18. http://dx.doi.org/10.1016/S0277-9536(00)00284-7.
- Dowrick C, Gask L, Edwards S, Aseem S, Bower P, Burroughs H, et al. Researching the mental health needs of hard-to-reach groups: managing multiple sources of evidence. BMC Health Serv Res 2009;9. http://dx.doi.org/10.1186/1472-6963-9-226.
- Alderson P, Bero L, Eccles M. Effective Practice and Organisation of Care group (Cochrane Collaborative Review Groups). London: John Wiley; 2005.
- Rogers A, Kennedy A, Nelson E, Robinson A. Uncovering the limits of patient-centeredness: implementing a self-management trial for chronic illness. Qual Health Res 2005;15:224-39. http://dx.doi.org/10.1177/1049732304272048.
- Biddle L, Donovan J, Gunnell D, Sharp D. Young adults’ perceptions of GPs as a help source for mental distress: a qualitative study. Br J Gen Pract 2006;56:924-31.
- Dixon-Woods M, Kirk D, Agarwal S. Vulnerable groups and access to health care: a critical interpretive synthesis. London: National Co-ordinating Centre for NHS Service Delivery and Organisation; 2005.
- Bandura A. Self-efficacy: the exercise of control. New York, NY: Freeman; 1997.
- Davis TC, Michielutte R, Askov E, Williams MV, Weiss BD. Practical assessment of adult literacy in health care. Health Educ Behav 1998;25:613-24. http://dx.doi.org/10.1177/109019819802500508.
- Pescosolido B, Gardner C, Lubell K. How people get into mental health services: stories of choice, coercion and ‘muddling through’ from ‘first-timers’. Soc Sci Med 1998;46:275-86. http://dx.doi.org/10.1016/S0277-9536(97)00160-3.
- Coyle J. Exploring the meaning of ‘dissatisfaction’ with health care: the importance of ‘personal identity threat’. Sociol Health Illn 1999;21:95-124. http://dx.doi.org/10.1111/1467-9566.t01-1-00144.
- Maxwell M. Women’s and doctors’ accounts of their experiences of depression in primary care: the influence of social and moral reasoning on patients’ and doctors’ decisions. Chronic Illn 2005;1:61-7. http://dx.doi.org/10.1179/174239505X19617.
- Rogers A, Hassell K, Nicolaas G. Demanding patients? Analysing the use of primary care. Milton Keynes: Open University Press; 1999.
- Clark D, Layard R, Smithies R, Richards D, Suckling R, Wright B. Improving access to psychological therapy: initial evaluation of two UK demonstration sites. Behav Res Ther 2009;47:910-20. http://dx.doi.org/10.1016/j.brat.2009.07.010.
- Bourdieu P. Outline of a theory of practice. Cambridge: Cambridge University Press; 1977.
- Fernando S, Keating F. Mental health in a multi-ethnic society: a multidisciplinary handbook. London: Routledge; 2008.
- Lakes K, Lopez S, Garro L. Cultural competence and psychotherapy: applying anthropologically informed conceptions of culture. Psychotherapy 2006;43:380-96. http://dx.doi.org/10.1037/0033-3204.43.4.380.
- Esmail A. Should Muslims have faith-based health services?. BMJ 2007;334. http://dx.doi.org/10.1136/bmj.39071.595301.94.
- Mead N, Bower P. Patient-centredness: a conceptual framework and review of the empirical literature. Soc Sci Med 2000;51:1087-110. http://dx.doi.org/10.1016/S0277-9536(00)00098-8.
- McWhinney I, Sheldon M, Brook J, Rector A. Decision making in general practice. London: Stockton; 1985.
- Kirmayer LJ. Cultural competence and evidence-based practice in mental health: epistemic communities and the politics of pluralism. Soc Sci Med 2012;75:249-56. http://dx.doi.org/10.1016/j.socscimed.2012.03.018.
- Badamgarav E, Weingarten S, Henning J, Knight K, Hasselblad V, Gano A, et al. Effectiveness of disease management programs in depression: a systematic review. Am J Psychiatry 2003;160:2080-90. http://dx.doi.org/10.1176/appi.ajp.160.12.2080.
- Barrett B, Byford S, Knapp M. Evidence of cost-effective treatments for depression: a systematic review. J Affect Disord 2005;84:1-13. http://dx.doi.org/10.1016/j.jad.2004.10.003.
- Bower P, Richards D, Lovell K. The clinical and cost-effectiveness of self-help treatments for anxiety and depressive disorders in primary care: a systematic review. Br J Gen Pract 2001;51:838-45.
- Bower P, Rowland N. Effectiveness and cost effectiveness of counselling in primary care. Cochrane Database Syst Rev 2006;3. http://dx.doi.org/10.1002/14651858.CD001025.
- Bower P, Rowland N, Hardy R. The clinical effectiveness of counselling in primary care: a systematic review and meta-analysis. Psychol Med 2003;33:203-15. http://dx.doi.org/10.1017/S0033291702006979.
- Bower P, Sibbald B. Systematic review of the effect of on-site mental health professionals on the clinical behaviour of general practitioners. BMJ 2000;320:614-17. http://dx.doi.org/10.1136/bmj.320.7235.614.
- Cabassa L, Hansen M. A systematic review of depression treatments in primary care for Latino adults. Res Soc Work Pract 2007;17:494-503. http://dx.doi.org/10.1177/1049731506297058.
- Chin M, Walters A, Cook S, Huang E. Interventions to reduce racial and ethnic disparities in health care. Med Care Res Rev 2007;64:7S-28S. http://dx.doi.org/10.1177/1077558707305413.
- Christensen H, Griffiths K, Gulliver A, Clack D, Kljakovic M, Wells L. Models in the delivery of depression care: a systematic review of randomised and controlled intervention trials. BMC Fam Pract 2008;9. http://dx.doi.org/10.1186/1471-2296-9-25.
- Cole M. Prognosis of depression in elderly community and primary care populations: a systematic review and meta-analysis. Am J Psychiatry 1999;156:1182-9.
- Druss B, von Esenwein S. Improving general medical care for persons with mental and addictive disorders: systematic review. Gen Hosp Psychiatry 2006;28:145-53. http://dx.doi.org/10.1016/j.genhosppsych.2005.10.006.
- Fellowes D, Wilkinson S, Moore P. Communication skills training for healthcare professionals working with cancer patients, their families and/or carers. Cochrane Database Syst Rev 2001;2.
- Gilbody S. Review: disease management programmes improve detection and care of people with depression. Evid Based Ment Health 2004;7. http://dx.doi.org/10.1136/ebmh.7.3.80.
- Gilbody S, Bower P, Fletcher J, Richards D, Sutton A. Collaborative care for depression: a cumulative meta-analysis and review of longer-term outcomes. Arch Intern Med 2006;166:2314-21. http://dx.doi.org/10.1001/archinte.166.21.2314.
- Gilbody S, Bower P, Whitty P. Costs and consequences of enhanced primary care for depression. Systematic review of randomised economic evaluations. Br J Psychiatry 2006;189:297-308. http://dx.doi.org/10.1192/bjp.bp.105.016006.
- Gilbody S, Whitty P, Grimshaw J, Thomas R. Educational and organizational interventions to improve the management of depression in primary care. JAMA 2003;289:3145-51. http://dx.doi.org/10.1001/jama.289.23.3145.
- Gunn J, Diggens J, Hegarty K, Blashki G. A systematic review of complex system interventions designed to increase recovery from depression in primary care. BMC Health Serv Res 2006;6.
- Heideman J, van Rijswijk E, van Lin N, de Loos S, Laurant M, Wensing M, et al. Interventions to improve management of anxiety disorders in general practice: a systematic review. Br J Gen Pract 2005;55:867-74.
- Neumeyer-Gromen A, Lampert T, Stark K, Kallischnigg G. Disease management programs for depression: a systematic review and meta-analysis of randomized controlled trials. Med Care 2004;42:1211-21. http://dx.doi.org/10.1097/00005650-200412000-00008.
- Raine R, Haines A, Sensky T, Hutchings A, Larkin K, Black N. Systematic review of mental health interventions for patients with common somatic symptoms: can research evidence from secondary care be extrapolated to primary care?. BMJ 2002;325. http://dx.doi.org/10.1136/bmj.325.7372.1082.
- Williams J, Gerrity M, Holsinger T, Dobscha S, Gaynes B, Dietrich A. Systematic review of multifaceted interventions to improve depression care. Gen Hosp Psychiatry 2007;29:91-116. http://dx.doi.org/10.1016/j.genhosppsych.2006.12.003.
- Wilson K, Mottram P, Vassilas C. Psychotherapeutic treatments for older depressed people. Cochrane Database Syst Rev 2008;1. http://dx.doi.org/10.1002/14651858.CD004853.pub2.
- van Boeijen C, van Balkom A, van Oppen P, Blankenstein N, Cherpanath A, van Dyck R. Efficacy of self-help manuals for anxiety disorders in primary care: a systematic review. Fam Pract 2005;22:192-6. http://dx.doi.org/10.1093/fampra/cmh708.
- Ali BS, Rahbar MH, Naeem S, Gul A, Mubein S, Iqbal A. The effectiveness of counseling on anxiety and depression by minimally trained counselors: a randomized controlled trial. Am J Psychother 2003;57:324-36.
- Antunes HKM, Stella SG, Santos RF, Bueno OFA, de Mello MT. Depression, anxiety and quality of life scores in seniors after an endurance exercise program. Rev Bras Psiquiatr 2005;27:266-71.
- Areán PA, Ayalon L, Hunkeler E, Lin EHB, Tang L, Harpole L, et al. Improving depression care for older, minority patients in primary care. Med Care 2005;43:381-90.
- Arthur AJ, Jagger C, Lindesay J, Matthews RJ. Evaluating a mental health assessment for older people with depressive symptoms in general practice: a randomised controlled trial. Br J Gen Pract 2002;52:202-7.
- Bailer U, de Zwaan M, Leisch F, Strnad A, Lennkh-Wolfsberg C, El-Giamal N, et al. Guided self-help versus cognitive-behavioral group therapy in the treatment of bulimia nervosa. Int J Eat Disord 2004;35:522-37. http://dx.doi.org/10.1002/eat.20003.
- Bakker IM, Terluin B, van Marwijk HWJ, van der Windt DAWM, Rijmen F, van Mechelen W, et al. A cluster-randomised trial evaluating an intervention for patients with stress-related mental disorders and sick leave in primary care. PLoS Hub Clin Trials 2007;2. http://dx.doi.org/10.1371/journal.pctr.0020026.
- Banerjee S, Shamash K, Macdonald AJ, Mann AH. Randomised controlled trial of effect of intervention by psychogeriatric team on depression in frail elderly people at home. BMJ 1996;313:1058-61. http://dx.doi.org/10.1136/bmj.313.7064.1058.
- Banks SR. The impact of social support and active coping on enhancing mental health and employability outcomes among African Americans and Latinos with disabilities: a community-based group intervention. Washington, DC: George Washington University; 1998.
- Barrowclough C, King P, Colville J, Russell E, Burns A, Tarrier N. A randomized trial of the effectiveness of cognitive-behavioral therapy and supportive counseling for anxiety symptoms in older adults. J Consult Clin Psychol 2001;69:756-62. http://dx.doi.org/10.1037//0022-006X.69.5.756.
- Beardslee WR. Outreach supported antidepressant treatment and cognitive behavioural therapy are effective for depression in low income minority women. Evid Based Ment Health 2004;7. http://dx.doi.org/10.1136/ebmh.7.1.21.
- Beeber L, Holditch-Davis D, Belyea M, Funk S, Canuso R. In-home intervention for depressive symptoms with low-income mothers of infants and toddlers in the United States. Health Care Women Int 2004;25:561-80. http://dx.doi.org/10.1080/07399330490444830.
- Bhugra D, Hicks MH-R. Effect of an educational pamphlet on help-seeking attitudes for depression among British South Asian women. Psychiatr Serv 2004;55:827-9. http://dx.doi.org/10.1176/appi.ps.55.7.827.
- Billipp SH. The psychosocial impact of interactive computer use within a vulnerable elderly population: a report on a randomized prospective trial in a home health care setting. Publ Health Nurs 2001;18:138-45. http://dx.doi.org/10.1046/j.1525-1446.2001.00138.x.
- Blanchard MR, Waterreus A, Mann AH. The effect of primary care nurse intervention upon older people screened as depressed. Int J Geriatr Psychiatry 1995;10:289-98. http://dx.doi.org/10.1002/gps.930100405.
- Blanchard MR, Waterreus A, Mann AH. Can a brief intervention have a longer-term benefit? The case of the research nurse and depressed older people in the community. Int J Geriatr Psychiatry 1999;14:733-8. http://dx.doi.org/10.1002/(SICI)1099-1166(199909)14:9<733::AID-GPS999>3.0.CO;2-G.
- Blumenthal JA, Emery CF, Madden DJ, Schniebolk S, Walsh-Riddle M, George LK, et al. Long-term effects of exercise on psychological functioning in older men and women. J Gerontol 1991;46:P352-61. http://dx.doi.org/10.1093/geronj/46.6.P352.
- Bogner HR, Morales KH, Post EP, Bruce ML. Diabetes, depression, and death: a randomized controlled trial of a depression treatment program for older adults based in primary care (PROSPECT). Diabetes Care 2007;30:3005-10. http://dx.doi.org/10.2337/dc07-0974.
- Boiko P, Katon W, Guerra JC, Mazzoni S. An audiotaped mental health evaluation tool for Hispanic immigrants with a range of literacy levels. J Immigr Health 2005;7:33-6. http://dx.doi.org/10.1007/s10903-005-1388-7.
- Brown C, Schulberg HC, Sacco D, Perel JM, Houck PR. Effectiveness of treatments for major depression in primary medical care practice: a post hoc analysis of outcomes for African American and white patients. J Affect Disord 1999;53:185-92. http://dx.doi.org/10.1016/S0165-0327(98)00120-7.
- Bruce ML, Ten Have TR, Reynolds CF, Katz II, Schulberg HC, Mulsant BH, et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients. JAMA 2004;291:1081-91. http://dx.doi.org/10.1001/jama.291.9.1081.
- Buwalda FM, Bouman TK, van Duijn MAJ. Psychoeducation for hypochondriasis: a comparison of a cognitive-behavioural approach and a problem-solving approach. Behav Res Ther 2007;45:887-9. http://dx.doi.org/10.1016/j.brat.2006.08.004.
- Callahan CM, Hendrie HC, Dittus RS, Brater DC. Improving treatment of late life depression in primary care: a randomized clinical trial. J Am Geriatr Soc 1994;42:839-46.
- Cardemil EV, Kim S, Pinedo TM, Miller IW. Developing a culturally appropriate depression prevention program: the Family Coping Skills Program. Cultur Divers Ethnic Minor Psychol 2005;11:99-112. http://dx.doi.org/10.1037/1099-9809.11.2.99.
- Cardemil EV, Reivich KJ, Beevers CG, Seligman MEP, James J. The prevention of depressive symptoms in low-income, minority children: two-year follow-up. Behav Res Ther 2007;45:313-27. http://dx.doi.org/10.1016/j.brat.2006.03.010.
- Catalan J, Gath DH, Anastasiades P, Bond SA, Day A, Hall L. Evaluation of a brief psychological treatment for emotional disorders in primary care. Psychol Med 1991;21:1013-18. http://dx.doi.org/10.1017/S0033291700030002.
- Chao S-Y, Liu H-Y, Wu C-Y, Jin S-F, Chu T-L, Huang T-S, et al. The effects of group reminiscence therapy on depression, self esteem, and life satisfaction of elderly nursing home residents. J Nurs Res 2006;14:36-45. http://dx.doi.org/10.1097/01.JNR.0000387560.03823.c7.
- Ciechanowski P, Wagner E, Schmaling K, Schwartz S, Williams B, Diehr P, et al. Community-integrated home-based depression treatment in older adults. JAMA 2004;291:1569-77. http://dx.doi.org/10.1001/jama.291.13.1569.
- Coleman EA, Grothaus LC, Sandhu N, Wagner EH. Chronic care clinics: a randomized controlled trial of a new model of primary care for frail older adults. J Am Geriatr Soc 1999;47:775-83.
- Cornelius LJ, Simpson GM, Ting L, Wiggins E, Lipford S. Reach out and I’ll be there: mental health crisis intervention and mobile outreach services to urban African Americans. Health Soc Work 2003;28:74-8. http://dx.doi.org/10.1093/hsw/28.1.74.
- Doyle AC, Goldschmidt A, Huang C, Winzelberg AJ, Taylor CB, Wilfley DE. Reduction of overweight and eating disorder symptoms via the Internet in adolescents: a randomized controlled trial. J Adolesc Health 2008;43:172-9. http://dx.doi.org/10.1016/j.jadohealth.2008.01.011.
- Dunn EC, Neighbors C, Larimer ME. Motivational enhancement therapy and self-help treatment for binge eaters. Psychol Addict Behav 2006;20:44-52. http://dx.doi.org/10.1037/0893-164X.20.1.44.
- Dwight-Johnson M, Ell K, Lee P-J. Can collaborative care address the needs of low-income Latinas with comorbid depression and cancer? Results from a randomized pilot study. Psychosomatics 2005;46:224-32. http://dx.doi.org/10.1176/appi.psy.46.3.224.
- Dybdahl R. Children and mothers in war: an outcome study of a psychosocial intervention program. Child Dev 2001;72:1214-30. http://dx.doi.org/10.1111/1467-8624.00343.
- Eisses AMH, Kluiter H, Jongenelis K, Pot AM, Beekman ATF, Ormel J. Care staff training in detection of depression in residential homes for the elderly: randomised trial. Br J Psychiatry 2005;186:404-9. http://dx.doi.org/10.1192/bjp.186.5.404.
- Ell K, Xie B, Quon B, Quinn DI, Dwight-Johnson M, Lee P-J. Randomized controlled trial of collaborative care management of depression among low-income patients with cancer. J Clin Oncol 2008;26:4488-96. http://dx.doi.org/10.1200/JCO.2008.16.6371.
- Escobar JI, Gara MA, Diaz-Martinez AM, Interian A, Warman M, Allen LA, et al. Effectiveness of a time-limited cognitive behavior therapy-type intervention among primary care patients with medically unexplained symptoms. Ann Fam Med 2007;5:328-35. http://dx.doi.org/10.1370/afm.702.
- Feld R, Woodside DB, Kaplan AS, Olmsted MP, Carter JC. Pretreatment motivational enhancement therapy for eating disorders: a pilot study. Int J Eat Disord 2001;29:393-400. http://dx.doi.org/10.1002/eat.1035.
- Foster RP. Treating depression in vulnerable urban women: a feasibility study of clinical outcomes in community service settings. Am J Orthopsychiatry 2007;77:443-53. http://dx.doi.org/10.1037/0002-9432.77.3.443.
- Fox PG, Cowell JM, Montgomery AC, Willgerodt MA. Southeast Asian refugee women and depression: a nursing intervention. Int J Psychiatr Nurs Res 1998;4:423-32.
- Gollings EK, Paxton SJ. Comparison of internet and face-to-face delivery of a group body image and disordered eating intervention for women: a pilot study. Eat Disord 2006;14:1-15. http://dx.doi.org/10.1080/10640260500403790.
- Haight BK, Michel Y, Hendrix S. Life review: preventing despair in newly relocated nursing home residents short-and long-term effects. Int J Aging Hum Dev 1998;47:119-42. http://dx.doi.org/10.2190/A011-BRXD-HAFV-5NJ6.
- Hanser SB, Thompson LW. Effects of a music therapy strategy on depressed older adults. J Gerontol 1994;49:P265-9. http://dx.doi.org/10.1093/geronj/49.6.P265.
- Heinicke BE, Paxton SJ, McLean SA, Wertheim EH. Internet-delivered targeted group intervention for body dissatisfaction and disordered eating in adolescent girls: a randomized controlled trial. J Abnormal Child Psychol 2007;35:379-91. http://dx.doi.org/10.1007/s10802-006-9097-9.
- Hinton DE, Chhean D, Pich V, Safren SA, Hofmann SG, Pollack MH. A randomized controlled trial of cognitive-behavior therapy for Cambodian refugees with treatment-resistant PTSD and panic attacks: a cross-over design. J Trauma Stress 2005;18:617-29. http://dx.doi.org/10.1002/jts.20070.
- Hunkeler EM, Katon W, Tang L, Williams JW, Kroenke K, Lin EHB, et al. Long term outcomes from the IMPACT randomised trial for depressed elderly patients in primary care. BMJ 2006;332:259-63. http://dx.doi.org/10.1136/bmj.38683.710255.BE.
- Jacob KS, Bhugra D, Mann AH. A randomised controlled trial of an educational intervention for depression among Asian women in primary care in the United Kingdom. Int J Soc Psychiatry 2002;48:39-148. http://dx.doi.org/10.1177/002076402128783190.
- Jonkers C, Lamers F, Bosma H, Metsemakers J, Kempen G, Van Eijk J. Process evaluation of a minimal psychological intervention to reduce depression in chronically ill elderly persons. Patient Educ Couns 2007;68:252-7. http://dx.doi.org/10.1016/j.pec.2007.06.010.
- Kawakami N, Araki S, Kawashima M, Masumoto T, Hayashi T. Effects of work-related stress reduction on depressive symptoms among Japanese blue-collar workers. Scand J Work Environ Health 1997;23:54-9. http://dx.doi.org/10.5271/sjweh.179.
- Kohn LP, Oden T, Muñoz RF, Robinson A, Leavitt D. Brief report: Adapted cognitive behavioral group therapy for depressed low-income African American women. Community Ment Health J 2002;38:497-504.
- Kornblith AB, Dowell JM, Herndon JE, Engelman BJ, Bauer-Wu S, Small EJ, et al. Telephone monitoring of distress in patients aged 65 years or older with advanced stage cancer. Cancer 2006;107:2706-14. http://dx.doi.org/10.1002/cncr.22296.
- Landreville P, Bissonnette L. Effects of cognitive bibliotherapy for depressed older adults with a disability. Clin Gerontol 1997;17:35-5. http://dx.doi.org/10.1300/J018v17n04_05.
- Larisch A, Schweickhardt A, Wirsching M, Fritzsche K. Psychosocial interventions for somatizing patients by the general practitioner: a randomized controlled trial. J Psychosom Res 2004;57:507-14.
- Lester KM, Milby JB, Schumacher JE, Vuchinich R, Person S, Clay OJ. Impact of behavioral contingency management intervention on coping behaviors and PTSD symptom reduction in cocaine-addicted homeless. J Trauma Stress 2007;20:565-75. http://dx.doi.org/10.1002/jts.20239.
- Levine S, Unützer J, Yip JY, Hoffing M, Leung M, Fan M-Y, et al. Physicians’ satisfaction with a collaborative disease management program for late-life depression in primary care. Gen Hosp Psychiatry 2005;27:383-91. http://dx.doi.org/10.1016/j.genhosppsych.2005.06.001.
- Llewellyn-Jones RH, Baikie KA, Smithers H, Cohen J, Snowdon J, Tennant CC. Multifaceted shared care intervention for late life depression in residential care: randomised controlled trial. BMJ 1999;319:676-82. http://dx.doi.org/10.1136/bmj.319.7211.676.
- Löfvander MB, Engström AW, Iglesias E. Do dialogues about concepts of pain reduce immigrant patients’ reported spread of pain? A comparison between two consultation methods in primary care. Eur J Pain 2006;10:335-41. http://dx.doi.org/10.1016/j.ejpain.2005.03.002.
- Lyles JS, Hodges A, Collins C, Lein C, Given CW, Given B, et al. Using nurse practitioners to implement an intervention in primary care for high-utilizing patients with medically unexplained symptoms. Gen Hosp Psychiatry 2003;25:63-7. http://dx.doi.org/10.1016/S0163-8343(02)00288-8.
- Marhold C, Linton SJ, Melin L. A cognitive-behavioral return-to-work program: effects on pain patients with a history of long-term versus short-term sick leave. Pain 2001;91:155-63. http://dx.doi.org/10.1016/S0304-3959(00)00431-0.
- McCurren C, Dowe D, Rattle D, Looney S. Depression among nursing home elders: testing an intervention strategy. Appl Nurs Res 1999;12:185-95. http://dx.doi.org/10.1016/S0897-1897(99)80249-3.
- McCusker J, Verdon J, Tousignant P, Courval D, Poulin L, Dendukuri N, et al. Rapid emergency department intervention for older people reduces risk of functional decline: results of a multicenter randomized trial. J Am Geriatr Soc 2001;49:1272-81. http://dx.doi.org/10.1046/j.1532-5415.2001.49254.x.
- McMurdo MET, Burnett L. Randomised controlled trial of exercise in the elderly. Gerontology 2009;38:292-8. http://dx.doi.org/10.1159/000213343.
- McNeil JK, LeBlanc EM, Joyner M. The effect of exercise on depressive symptoms in the moderately depressed elderly. Psychol Aging 1991;6:487-8. http://dx.doi.org/10.1037//0882-7974.6.3.487.
- Michael YL, Farquhar SA, Wiggins N, Green MK. Findings from a community-based participatory prevention research intervention designed to increase social capital in Latino and African American communities. J Immigr Minor Health 2008;10:281-9. http://dx.doi.org/10.1007/s10903-007-9078-2.
- Miller DK, Chibnall JT, Videen SD, Duckro PN. Supportive-affective group experience for persons with life-threatening illness: reducing spiritual, psychological, and death-related distress in dying patients. J Palliat Med 2005;8:333-43. http://dx.doi.org/10.1089/jpm.2005.8.333.
- Miranda J, Azocar F, Organista KC, Dwyer E, Areane P. Treatment of depression among impoverished primary care patients from ethnic minority groups. Psychiatr Serv 2003;54:219-25. http://dx.doi.org/10.1176/appi.ps.54.2.219.
- Miranda J, Chung JY, Green BL, Krupnick J, Siddique J, Revicki DA, et al. Treating depression in predominantly low-income young minority women. JAMA 2003;290:57-65. http://dx.doi.org/10.1001/jama.290.1.57.
- Miranda J, Duan N, Sherbourne C, Schoenbaum M, Lagomasino I, Jackson-Triche M, et al. Improving care for minorities: can quality improvement interventions improve care and outcomes for depressed minorities? Results of a randomized, controlled trial. Health Serv Res 2003;38:613-30. http://dx.doi.org/10.1111/1475-6773.00136.
- Miranda J, Green BL, Krupnick JL, Chung J, Siddique J, Belin T, et al. One-year outcomes of a randomized clinical trial treating depression in low-income minority women. J Consult Clin Psychol 2006;74:99-111. http://dx.doi.org/10.1037/0022-006X.74.1.99.
- Morriss R, Dowrick C, Salmon P, Peters S, Dunn G, Rogers A, et al. Cluster randomised controlled trial of training practices in reattribution for medically unexplained symptoms. Br J Psychiatry 2007;191:536-42. http://dx.doi.org/10.1192/bjp.bp.107.040683.
- Nystuen P, Hagen KB. Solution-focused intervention for sick listed employees with psychological problems or muscle skeletal pain: a randomised controlled trial [ISRCTN39140363]. BMC Publ Health 2006;6.
- Oslin DW, Sayers S, Ross J, Kane V, Ten Have T, Conigliaro J, et al. Disease management for depression and at-risk drinking via telephone in an older population of veterans. Psychosom Med 2003;65:931-7. http://dx.doi.org/10.1097/01.PSY.0000097335.35776.FB.
- Otto MW, Hinton D, Korbly NB, Chea A, Ba P, Gershuny BS, et al. Treatment of pharmacotherapy-refractory posttraumatic stress disorder among Cambodian refugees: a pilot study of combination treatment with cognitive-behavior therapy vs sertraline alone. Behav Res Ther 2003;41:1271-6. http://dx.doi.org/10.1016/S0005-7967(03)00032-9.
- Paunovic N, Öst L-G. Cognitive-behavior therapy vs exposure therapy in the treatment of PTSD in refugees. Behav Res Ther 2001;39:1183-97. http://dx.doi.org/10.1016/S0005-7967(00)00093-0.
- Paxton SJ, McLean SA, Gollings EK, Faulkner C, Wertheim EH. Comparison of face-to-face and internet interventions for body image and eating problems in adult women: an RCT. Int J Eat Disord 2007;40:692-704. http://dx.doi.org/10.1002/eat.20446.
- Quijano LM, Stanley MA, Petersen NJ, Casado BL, Steinberg EH, Cully JA, et al. Healthy IDEAS: a depression intervention delivered by community-based case managers serving older adults. J Appl Gerontol 2007;26:139-56. http://dx.doi.org/10.1177/0733464807299354.
- Rasmussen NH, Furst JW, Swenson-Dravis DM, Agerter DC, Smith AJ, Baird MA, et al. Innovative reflecting interview: effect on high-utilizing patients with medically unexplained symptoms. Dis Manag 2006;9:349-59. http://dx.doi.org/10.1089/dis.2006.9.349.
- Razali SM, Hasanah CI, Aminah K, Subramaniam M. Religious-sociocultural psychotherapy in patients with anxiety and depression. Aust N Z J Psychiatry 1998;32:867-72. http://dx.doi.org/10.3109/00048679809073877.
- Rees L, Clark-Stone S. Can collaboration between education and health professionals improve the identification and referral of young people with eating disorders in schools? A pilot study. J Adolesc 2006;29:137-51. http://dx.doi.org/10.1016/j.adolescence.2005.08.017.
- Reijneveld SA, Westhoff MH, Hopman-Rock M. Promotion of health and physical activity improves the mental health of elderly immigrants: results of a group randomised controlled trial among Turkish immigrants in the Netherlands aged 45 and over. J Epidemiol Community Health 2003;57:405-11. http://dx.doi.org/10.1136/jech.57.6.405.
- Rosendal M, Olesen F, Fink P, Toft T, Sokolowski I, Bro F. A randomized controlled trial of brief training in the assessment and treatment of somatization in primary care: effects on patient outcome. Gen Hosp Psychiatry 2007;29:364-73. http://dx.doi.org/10.1016/j.genhosppsych.2007.03.005.
- Rubenstein LZ, Alessi CA, Josephson KR, Trinidad Hoyl M, Harker JO, Pietruszka FM. A randomized trial of a screening, case finding, and referral system for older veterans in primary care. J Am Geriatr Soc 2007;55:166-74. http://dx.doi.org/10.1111/j.1532-5415.2007.01044.x.
- Scogin F, Hamblin D, Beutler L. Bibliotherapy for depressed older adults: a self-help alternative. Gerontologist 1987;27:383-7. http://dx.doi.org/10.1093/geront/27.3.383.
- Scogin F, Jamison C, Gochneaur K. Comparative efficacy of cognitive and behavioral bibliotherapy for mildly and moderately depressed older adults. J Consult Clin Psychol 1989;57:403-7. http://dx.doi.org/10.1037//0022-006X.57.3.403.
- Shern DL, Tsemberis S, Anthony W, Lovell AM, Richmond L, Felton CJ, et al. Serving street-dwelling individuals with psychiatric disabilities: outcomes of a psychiatric rehabilitation clinical trial. Am J Publ Health 2000;90:1873-8.
- Sims J, Hill K, Davidson S, Gunn J, Huang N. Exploring the feasibility of a community-based strength training program for older people with depressive symptoms and its impact on depressive symptoms. BMC Geriatr 2006;6.
- Singh NA, Clements KM, Fiatarone MA. A randomized controlled trial of progressive resistance training in depressed elders. J Gerontol Ser A Biol Sci Med Sci 1997;52:M27-35. http://dx.doi.org/10.1093/gerona/52A.1.M27.
- Singh NA, Stavrinos TM, Scarbek Y, Galambos G, Liber C, Singh MAF. A randomized controlled trial of high versus low intensity weight training versus general practitioner care for clinical depression in older adults. J Gerontol Ser A Biol Sci Med Sci 2005;60:768-76. http://dx.doi.org/10.1093/gerona/60.6.768.
- Slesnick N, Kang MJ, Bonomi AE, Prestopnik JL. Six- and twelve-month outcomes among homeless youth accessing therapy and case management services through an urban drop-in center. Health Serv Res 2008;43:211-29. http://dx.doi.org/10.1111/j.1475-6773.2007.00755.x.
- Sloman R. Relaxation and imagery for anxiety and depression control in community patients with advanced cancer. Cancer Nurs 2002;25:432-5. http://dx.doi.org/10.1097/00002820-200212000-00005.
- Smith RC, Lein C, Collins C, Lyles JS, Given B, Dwamena FC, et al. Treating patients with medically unexplained symptoms in primary care. J Gen Intern Med 2003;18:478-89. http://dx.doi.org/10.1046/j.1525-1497.2003.20815.x.
- Smith RC, Lyles JS, Gardiner JC, Sirbu C, Hodges A, Collins C, et al. Primary care clinicians treat patients with medically unexplained symptoms: a randomized controlled trial. J Gen Intern Med 2006;21:671-7. http://dx.doi.org/10.1111/j.1525-1497.2006.00460.x.
- Stasi MF, Amati D, Costa C, Resta D, Senepa G, Scarafioiti C, et al. Pet-therapy: a trial for institutionalized frail elderly patients. Arch Gerontol Geriatr Suppl 2004;9:407-12. http://dx.doi.org/10.1016/j.archger.2004.04.052.
- Tollett JH, Thomas SP. A theory-based nursing intervention to instill hope in homeless veterans. Adv Nurs Sci 1995;18:76-90.
- Unützer J, Katon W, Callahan CM, Williams JW, Hunkeler E, Harpole L, et al. Collaborative care management of late-life depression in the primary care setting. JAMA 2002;288:2836-45. http://dx.doi.org/10.1001/jama.288.22.2836.
- van der Feltz-Cornelis CM, van Oppen P, Adèr HJ, van Dyck R. Randomised controlled trial of a collaborative care model with psychiatric consultation for persistent medically unexplained symptoms in general practice. Psychother Psychosom 2006;75:282-9. http://dx.doi.org/10.1159/000093949.
- Wade TD, Davidson S, O’Dea JA. A preliminary controlled evaluation of a school-based media literacy program and self-esteem program for reducing eating disorder risk factors. Int J Eat Disord 2003;33:371-83. http://dx.doi.org/10.1002/eat.10136.
- Waller D, Fairburn CG, McPherson A, Kay R, Lee A, Nowell T. Treating bulimia nervosa in primary care: A pilot study. Int J Eat Disord 1996;19:99-103. http://dx.doi.org/10.1002/(SICI)1098-108X(199601)19:1<99::AID-EAT12>3.3.CO;2-6.
- Weine SM, Raina D, Zhubi M, Delesi M, Huseni D, Feetham S, et al. The TAFES multi-family group intervention for Kosovar refugees: a feasibility study. J Nervous Ment Dis 2003;191:100-7. http://dx.doi.org/10.1097/01.NMD.0000050938.06620.D2.
- Wells KB, Sherbourne CD, Miranda J, Tang L, Benjamin B, Duan N. The cumulative effects of quality improvement for depression on outcome disparities over 9 years: results from a randomized, controlled group-level trial. Med Care 2007;45:1052-9. http://dx.doi.org/10.1097/MLR.0b013e31813797e5.
- White H, McConnell E, Clipp E, Branch LG, Sloane R, Pieper C, et al. A randomized controlled trial of the psychosocial impact of providing internet training and access to older adults. Aging Ment Health 2002;6:213-21. http://dx.doi.org/10.1080/13607860220142422.
- Whooley MA, Stone B, Soghikian K. Randomized trial of case-finding for depression in elderly primary care patients. J Gen Intern Med 2000;15:293-300. http://dx.doi.org/10.1046/j.1525-1497.2000.04319.x.
- Williams JW, Barrett J, Oxman T, Frank E, Katon W, Sullivan M, et al. Treatment of dysthymia and minor depression in primary care. JAMA 2000;284:1519-26. http://dx.doi.org/10.1001/jama.284.12.1519.
- Winzelberg AJ, Taylor CB, Sharpe T, Eldredge KL, Dev P, Constantinou PS. Evaluation of a computer-mediated eating disorder intervention program. Int J Eat Disord 1998;24:339-49. http://dx.doi.org/10.1002/(SICI)1098-108X(199812)24:4<339::AID-EAT1>3.0.CO;2-J.
- Wissow LS, Gadomski A, Roter D, Larson S, Brown J, Zachary C, et al. Improving child and parent mental health in primary care: a cluster-randomized trial of communication skills training. Pediatrics 2008;121:266-75. http://dx.doi.org/10.1542/peds.2007-0418.
- Zauszniewski JA. Teaching resourcefulness skills to older adults. J Gerontol Nurs 1997;23:14-20.
- Blaxter M. Criteria for the evaluation of qualitative research papers. Med Sociol News 1996;22:68-71.
- Noblit GW, Hare DR. Meta-ethnography: synthesizing qualitative studies. London: Sage; 1988.
- Luoma M-L, Hakamies-Blomqvist L. The meaning of quality of life in patients being treated for advanced breast cancer: a qualitative study. Psychooncology 2004;13:729-39. http://dx.doi.org/10.1002/pon.788.
- Koffman J, Morgan M, Edmonds P, Speck P, Higginson I. Cultural meanings of pain: a qualitative study of black Caribbean and white British patients with advanced cancer. Palliat Med 2008;22:350-9. http://dx.doi.org/10.1177/0269216308090168.
- Rother S, Buckroyd J. Experience of service provision for adolescents with eating disorders. Prim Health Care Res Dev 2006;5:153-61. http://dx.doi.org/10.1191/1463423604pc192oa.
- Tierney S. The individual within a condition: a qualitative study of young people’s reflections on being treated for anorexia nervosa. J Am Psychiatr Nurse Assoc 2008;13:368-75. http://dx.doi.org/10.1177/1078390307309215.
- Tischler VA, Rademeyer A, Vostanis P. Mothers experiencing homelessness: mental health, support and social care needs. Health Soc Care Community 2007;15:246-53. http://dx.doi.org/10.1111/j.1365-2524.2006.00678.x.
- Millward L, Lutte A, Purvis R. Depression and the perpetuation of an incapacitated identity as an inhibitor of return to work. J Psychiatr Ment Health Nurs 2005;12:565-73. http://dx.doi.org/10.1111/j.1365-2850.2005.00875.x.
- Lawrence V, Banerjee S, Bhugra D, Sangha K, Turner S, Murray J. Coping with depression in later life: a qualitative study of help-seeking in three ethnic groups. Psychol Med 2006;36:1375-83. http://dx.doi.org/10.1017/S0033291706008117.
- Peters S, Stanley I, Rose M, Salmon P. Patients with medically unexplained symptoms: sources of patients’ authority and implications for demands on medical care. Soc Sci Med 1998;46:559-65. http://dx.doi.org/10.1016/S0277-9536(97)00200-1.
- Nettleton S, Watt I, O’Malley L, Duffey P. Understanding the narratives of people who live with medically unexplained illness. Patient Educ Couns 2005;56:205-10. http://dx.doi.org/10.1016/j.pec.2004.02.010.
- Perron J, Hudelson P. Somatisation: illness perspectives of asylum seeker and refugee patients from the former country of Yugoslavia. BMC Fam Pract 2006;7.
- Rogers A, Allison T. What if my back breaks? Making sense of musculoskeletal pain among South Asian and African-Caribbean people in the North West of England. J Psychosom Res 2004;57:79-87. http://dx.doi.org/10.1016/S0022-3999(03)00570-1.
- Chew C, May CR. The benefits of back pain. Fam Pract 1997;14:461-5. http://dx.doi.org/10.1093/fampra/14.6.461.
- Hodgson P, Smith P, Brown T, Dowrick C. Stories from frequent attenders: a qualitative study in primary care. Ann Fam Med 2005;3:318-23. http://dx.doi.org/10.1370/afm.311.
- Warfa N, Bhui K, Craig T, Curtis S, Mohamud S, Stansfeld S, et al. Post-migration geographical mobility, mental health and health service utilisation among Somali refugees in the UK: a qualitative study. Health Place 2006;12:503-15. http://dx.doi.org/10.1016/j.healthplace.2005.08.016.
- Whittaker S, Hardy G, Lewis K, Buchan L. An exploration of psychological well-being with young Somali refugee and asylum-seeker women. Clin Child Psychol Psychiatry 2005;10:177-96. http://dx.doi.org/10.1177/1359104505051210.
- Palmer D, Ward K. ‘Lost’: listening to the voices and mental health needs of forced migrants in London. Med Confl Surviv 2007;23:198-212. http://dx.doi.org/10.1080/13623690701417345.
- Green G, Bradby H, Chan A, Lee M, Eldridge K. Is the English National Health Service meeting the needs of mentally distressed Chinese women?. J Health Serv Res Policy 2002;7:216-21. http://dx.doi.org/10.1258/135581902320432741.
- Burr J, Chapman T. Contextualising experiences of depression in women from South Asian communities: a discursive approach. Sociol Health Illn 2004;26:433-52. http://dx.doi.org/10.1111/j.0141-9889.2004.00398.x.
- Edge D, Rogers A. Dealing with it: black Caribbean women’s response to adversity and psychological distress associated with pregnancy, childbirth, and early motherhood. Soc Sci Med 2005;61:15-2. http://dx.doi.org/10.1016/j.socscimed.2004.11.047.
- Lamb J, Bower P, Rogers A, Dowrick C, Gask L. Access to mental health in primary care: a qualitative meta-synthesis of evidence from the experience of people from ‘hard to reach’ groups. Health 2012;16:76-104. http://dx.doi.org/10.1177/1363459311403945.
- Faugier J, Sargeant M. Sampling hard to reach populations. J Adv Nurs 1997;26:790-7. http://dx.doi.org/10.1046/j.1365-2648.1997.00371.x.
- Patiniotis J. Who’s listening? Gender sensitive mental health service provision: key issues from the perspectives of service users. Liverpool: PPI Forum for Mersey Care; 2005.
- Cornah D. The impact of spirituality on mental health: a review of the literature. London: Mental Health Foundation; 2006.
- Survey of Pennine Care Mental Health NHS Trust service user/carer involvement policy. Ashton-under-Lyne: Pennine Care Mental Health Trust; n.d.
- Chew-Graham CA, Bashir C, Firth M, Saltmore S. Mental health needs assessment of under-represented groups in Central Manchester Primary Care Trust. Manchester: Central Manchester Primary Care Trust; 2001.
- Miah N. A Mental Health Survey. How Are You Being Looked After? n.d.
- Barker I. Thematic analysis of responses to consultation on proposals outlined in: Change in mind: proposals for the future of Manchester’s mental health services. Manchester: Manchester Mental Health Community; 2006.
- The Manchester mental health needs report – developing the service to meet the needs. Manchester: Manchester Mental Health and Social Care Trust; 2003.
- Mental health needs in Manchester: working group report. Manchester: Manchester Mental Health and Social Care Trust; 2003.
- Mersey Care NHS Trust . Mersey Cares 2008.
- A review of mental health services in the North West – consultation flyer. Manchester: NHS North West; 2008.
- Involving service users and carers - the Mersey Care way. Liverpool: Mersey Care NHS Trust; n.d.
- Mental health at work: developing the business case. London: Sainsbury Centre for Mental Health; 2007.
- Primary care services for depression: a guide to best practice. London: Department of Health; 2006.
- Mental health and social exclusion. London: Office of the Deputy Prime Minister; 2004.
- Fox D, Scott-Samuel A. Human rights, equity and health. London: Nuffield Trust; 2004.
- Mental health and social exclusion: consultation document. London: Office of the Deputy Prime Minister; 2003.
- Improving access to psychological therapies: stakeholder engagement process. Liverpool: Liverpool Primary Care Trust; 2007.
- A vision for commissioning and planning for health services in Wigan Borough (draft). Wigan: Ashton, Leigh and Wigan PCT; 2007.
- Commissioning for primary care mental health services – improving access to psychological therapies for people living with alcohol and common mental health problems. Liverpool: Liverpool Mental Health Consortium; 2007.
- Commissioning for primary care mental health services – improving access to psychological therapies. Liverpool: Liverpool Mental Health Consortium; 2007.
- Right from the start. Kingston upon Thames: Rethink; 2003.
- Bird A. We need to talk: the case for psychological therapy on the NHS. London: Mental Health Foundation; 2006.
- Who cares? The experiences of mental health carers accessing services and information. Kingston upon Thames: Rethink; 2003.
- A question of choice. London: NSF; 2000.
- Hughes R. Manchester mental health community: mental health services reconfiguration - patient and public involvement review. Manchester; 2005.
- Do helplines help? Summary report. Kingston upon Thames: Rethink; 2003.
- Mental health services in North Mersey – the configuration opportunity: a discussion paper on the future for mental health services in Knowsley, Liverpool and Sefton. Liverpool: North Mersey Mental Health Trust; 1999.
- Mental health services review: report on progress towards the development of comprehensive mental health services in the North West. Manchester: NHS Executive North West; 1996.
- Mental health services in the North West: a review of progress towards the development of comprehensive mental health services. Manchester: NHS Executive North West; 1998.
- A joint agency agreement for mental health services and a joint draft strategy for mental health in Liverpool. Liverpool: Liverpool Health Authority; 1995.
- A joint agency agreement for mental health services and a joint strategy for mental health in Liverpool. Liverpool: Liverpool Health Authority; 1996.
- Doing it for real: a guide to setting up and undertaking a User Focused Monitoring project. London: Sainsbury Centre for Mental Health; 2003.
- Creating a stronger voice for mental health: a service users event hosted by Commission for Patient and Public Involvement in Health. London: Commission for Patient and Public Involvement; 2007.
- Directed enhanced services – access to primary care. Liverpool: Liverpool PCT; 2007.
- Watt A. Social Exclusion Task Force . Adults Facing Chronic Exclusion (ACE) Pilots 2007.
- Innovations for anxiety. Kingston upon Thames: Rethink; 2006.
- Rose SM, Black BL. Advocacy and empowerment: mental health care in the community. London: Routledge & Kegan Paul; 1985.
- Naylor C, Wallcraft J, Samele C, Greatley A. Research priorities for service user and carer-centred mental health services: consultation report. London: National Co-ordinating Centre for NHS Service Delivery and Organisation; 2007.
- Keating F, Samele C, Furnish K, Greatley A. Research priorities for service user and carer-centred mental health services: a synthesis of the literature and policy documents. London: National Co-ordinating Centre for NHS Service Delivery and Organisation; 2006.
- Samele C, Wallcraft J, Naylor C, Keating F, Greatley A. Research priorities for service user and carer-centred mental health services: overview report. London: National Co-ordinating Centre for NHS Service Delivery and Organisation; 2007.
- Mental Health in Higher Education Project . Mental Health in Higher Education Project E-Bulletin Mhhenews 2007. www.mhhe.heacademy.ac.uk/news-and-events/ebulletin/ (accessed 26 June 2013).
- Clark J. Understanding mental health systems in the North West phase 1: survey of operational documents. Hyde: NW CSIP; 2008.
- CSIP survey: next phase. Hyde: NW CSIP; n.d.
- Our NHS our future: clinical pathway group reports. Manchester: NHS North West; 2008.
- Mental well-being summit summary findings. Hyde: NW CSIP; 2008.
- Mahoney C, Rippon S. Final report of the NHS North West Mental Health Commission listening events held October to February 2008. Hyde: NW CSIP; 2008.
- Developing a new health service for Liverpool: update on Big Health Debate Live! – one year on. Liverpool: Liverpool PCT; 2007.
- The Big Health Debate and next steps. Liverpool: Liverpool PCT; 2007.
- Mir G. Better Health Briefing 2: effective communication with service users. London: Race Equality Foundation; 2007.
- Thorlby R, Curry N. PCTs and race equality schemes. London: King’s Fund; 2007.
- Bennett J, Kalathil J, Keating F. Race equality training in mental health services in England: does one size fit all?. London: Sainsbury Centre for Mental Health; 2007.
- Begum N. Doing it for themselves: participation and black and minority ethnic service users. London: Social Care Institute for Excellence and the Race Equality Unit; 2006.
- Review of equality and diversity research carried out with communities in Liverpool. Liverpool: Liverpool Mental Health Consortium; 2006.
- Waheed W, Gask L, Lester H, Kendrick T, Peveler R. Primary care mental health. London: Gaskell/Royal College of Psychiatrists; 2009.
- Caught between stigma and inequality: black & minority ethnic communities and mental well-being in Kensington & Chelsea and Westminster. London: BME Health Forum/Migrant and Refugee Communities’ Forum; 2005.
- Seabrooke V, Milne A. Culture and care in dementia: a study of the Asian community in North West Kent. Northfleet, Kent: Alzheimer’s and Dementia Support Services; 2004.
- Fedigan D. Gypsy and traveller health. Wigan: Ashton, Leigh and Wigan PCT; 2005.
- Street C, Stapelkamp C, Taylor E, Malek M, Kurtz Z. Minority voices: research into the access and acceptability of services for the mental health of young people from black and minority ethnic groups. London: Young Minds; 2005.
- Sooch R, Kalyan G, Rai J. Oppressed voices: understanding the effects of domestic violence for South Asian women. Kingston upon Thames: Rethink; 2006.
- Our voice: the Pakistani community’s view of mental health and mental health services in Birmingham. Kingston upon Thames: Rethink; 2007.
- Knight L. Carers’ experiences and satisfaction with mental health services in Liverpool. Liverpool: Mersey Care NHS Trust; 2002.
- Seebohm P, Henderson P, Munn-Giddings C, Thomas P, Yasmeen S. Together we will change – community development, mental health and diversity. London: Sainsbury Centre for Mental Health; 2005.
- Keating F, Robertson D, McCulloch A, Francis E. Breaking the circles of fear. London: Sainsbury Centre for Mental Health; 2002.
- Communications for all: handy hints manual. Liverpool: North, Central and South Liverpool PCTs; 2004.
- Howard P, Buffin J, Bashford J, Heginbotham C. Engaging local communities: reaching seldom heard groups. Preston: University of Central Lancashire; 2008.
- Lane P, Hearsum S. The mental health and well being of black and minority ethnic elders: a foundational report on the research literature and a mapping of national resources. Part four: a national mapping of projects for BME elders to support their mental health and well-being. Birmingham: CSIP West Midlands; 2007.
- Lane P, Hearsum S. The mental health and well being of black and minority ethnic elders: a foundational report on the research literature and a mapping of national resources. Birmingham: CSIP West Midlands; 2007.
- Asylum seekers: meeting their healthcare needs. London: British Medical Association; 2002.
- Lambeth PCT. ‘I like the way we are talking now’. Refugees, asylum seekers, health services and involvement. London: Lambeth PCT; 2004.
- Palmer D, Ward K. ‘Unheard voices’: listening to refugees and asylum seekers in the planning and delivery of mental health service provision in London. London: Commission for Patient and Public Involvement in Health; 2006.
- Ward K, Palmer D. Mapping the provision of mental health services for asylum seekers and refugees in London: a report. London: Commission for Public Patient Involvement in Health; 2005.
- Cutler C. Fit to be detained? Challenging the detention of asylum seekers and migrants with health needs. London: BID; 2005.
- Newbold E. A Case Study Looking at Depression in the Asylum Seeker Community 2007. www.healthy-inclusion.org.uk/asylum-speaker-health/ (accessed 26 June 2013).
- Access to healthcare for asylum seekers: guidance from the ethics department. London: British Medical Association; 2001.
- Sixsmith J, Lawthom R, Whittle N, Mountian I. Health experiences of access to health: understanding the case of Manchester’s Somali and Iraqi asylum seekers and refugees: interim report (February). Manchester: Manchester Metropolitan University; 2008.
- Adhana L. The health and well-being of women and child asylum seekers and refugees in Wigan. MSc dissertation. Liverpool: Liverpool John Moores University; 2006.
- Fit for purpose yet? The Independent Asylum Commission’s interim findings. London: Independent Asylum Commission; 2008.
- Hutchinson H. Health impact assessment needs evaluation of asylum seekers in Liverpool (draft). Liverpool: Liverpool PCT; 2008.
- O’Neill J. Asylum Health UK Education Audit and Research Lead . Merseyside Asylum Seeker Health: Health Impact Needs Assessment – towards the Development of Liverpool Asylum Seeker Rapid Assessment Centre 2008.
- Leggatt V, Burnett A. Medical Foundation for the Care of Victims of Torture . Brief Interventions With Survivors of Torture 2007.
- McClusky G, Shelmerdine K. NE Leeds PCT . FLASH (Focus, Learning &Amp; Self-Help) Clinics 2007.
- Burnett A. Medical Foundation for the Care of Victims of Torture . Tackling Inequalities in the Health of Refugees in Host Countries: A Challenge for Researchers and Policy Makers 2006.
- Vasiliou C. Making the link between mental health and youth homelessness: a pan-London study. London: Mental Health Foundation; 2006.
- Anderson I, Baptista I, Wolf J, Edgar B, Benjaminsen L, Sapounakis A, et al. The changing role of service provision: barriers to access of health services for homeless people. Brussels: FEANTSA European Observatory on Homelessness; 2006.
- Stephens J. The mental health needs of homeless children and young people. London: Mental Health Foundation; 2002.
- Somers M. Homeless and vulnerable persons team annual report 2006–2007. Wigan: Ashton, Leigh and Wigan PCT; 2007.
- Fairclough J, Somers M, Reid A, Greenall P, Gavaghan J. From prison to the streets and back. Wigan: Wigan and Leigh Community Safety Partnership; 2003.
- Somers M. Homeless and vulnerable persons team annual report 2005–2006. Wigan: Ashton, Leigh and Wigan PCT; 2006.
- Somers M. Specialist health visitor for homeless and vulnerable people annual report 2003–2004. Wigan: Ashton, Leigh and Wigan PCT; 2004.
- Provision of health and mental health services for homeless people in Derby. Derby: Mental Health Services; n.d.
- Failing families. Norwich: Beat; 2008.
- Youth Access . Access to Counselling Key Findings; An Evaluation of the Relationship Between YIACS and CAMHS n.d. http://youthaccess.org.uk (accessed 19 June 2008).
- Wilson C. Youth Access . Breaking down the Barriers (a Strategy in Development, Case Studies and Key Findings on Young people’s Mental Health needs): Youth Access; 2001–2 n.d. http://youthaccess.org.uk/publications/counselling-publications/ (accessed 22 June 2013).
- Smith K, Leon L. Turned upside down: developing community-based crisis services for 16–25-year-olds experiencing a mental health crisis. London: Mental Health Foundation; 2001.
- Laws S. Hear me! Consulting with young people on mental health issues. London: Mental Health Foundation; 1998.
- Knight L. Young carers’ experiences and satisfaction with mental health services in Liverpool. Liverpool: Mersey Care NHS Trust; 2002.
- NHS Health Advisory Service . A Review of the Adolescent Forensic Psychiatry Service Based on the Gardener Unit, Prestwich Hospital 1994.
- Do you ever feel depressed?. London: YoungMinds; 2003.
- Children and young people get depressed too. Leaflet. London: YoungMinds; 2003.
- Young minds: thoughts allowed. London: YoungMinds; n.d.
- What are child and adolescent mental health services. Leaflet. London: YoungMinds; 2002.
- YoungMinds . Bulimia and Anorexia 2007. www.youngminds.org.uk/parents/im-concerned-about/bulimia-and-anorexia (accessed 19 June 2008).
- Worried about eating problems and disorders?. London: YoungMinds; 2003.
- Time to tell. Norwich: Eating Disorders Association; 2006.
- Something’s got to change. Norwich: Beat; 2006.
- ‘Getting better?’ Is the quality of treatment for eating disorders in the UK getting better?. Norwich: Eating Disorders Association; 2005.
- The hidden cost of eating disorders. Norwich: Eating Disorders Association; 2003.
- Eating disorders: the need for action in 2000 and beyond. Norwich: Eating Disorders Association; 2000.
- Kemp PA, Davidson J. Routes onto incapacity benefit: findings from a survey of recent claimants. London: Department for Work and Pensions; 2008.
- Health@Work . Strategic Plan 2005–8 2007. www.healthatworkcentre.org.uk/ (accessed 26 June 2013).
- Taylor R, Lewis J. Understanding the impact of JRRP for people with mental health conditions. London: Department for Work and Pensions; 2008.
- Tackling social exclusion: achievements, lessons learned and the way forward. London: Office of the Deputy Prime Minister; 2003.
- Hasluck C, Green AE. What works for whom? A review of evidence and meta-analysis for the Department for Work and Pensions. London: Department for Work and Pensions; 2007.
- Bilsker D, Gilbert M, Myette TL, Stewart-Patterson C. Depression & work function: bridging the gap between mental health care & the workplace. Vancouver: Mental Health Evaluation and Community Consultation Unit, University of British Columbia; 2005.
- South West Regional Development Centre . The Role of Referral Management Centres in Managing Medically Unexplained Symptoms 2008.
- Basildon PCT PPI Forum . A Framework for Elderly Mental Health Care Facilities in GP Surgeries (draft) 2005.
- Access to older people’s mental health services: patient survey report. High Wycombe: Patient Dynamics; 2007.
- Profile of the over 55’s in Knowsley. Liverpool: Knowsley Council/Knowsley PCT; 2008.
- Hibbert D, Catlin A, Chew-Graham C, Clarke P, Edwards S, Kovandžić M. Access to High Quality Mental Health Services by Hard-to-Reach Groups: A Grey Literature Review 2008. www.liv.ac.uk/amp (accessed 13 June 2013).
- Reeve J, Lloyd-Williams M, Payne S, Dowrick C. Revisiting biographical disruption: exploring individual embodied illness experience in people with terminal cancer. Health (London) 2010;14:178-95. http://dx.doi.org/10.1177/1363459309353298.
- Gask L, Aseem S, Waquas A, Waheed W. Isolation, feeling ‘stuck’ and loss of control: understanding persistence of depression in British Pakistani women. J Affect Disord 2011;128:49-55. http://dx.doi.org/10.1016/j.jad.2010.06.023.
- Edwards S, Gabbay M. Living and working with sickness: a qualitative study. Chronic Illn 2007;3:155-66. http://dx.doi.org/10.1177/1742395307082124.
- May C, Allison G, Chapple A, Chew-Graham C, Dixon C, Gask L, et al. Framing the doctor–patient relationship in chronic illness: a comparative study of general practitioners’ accounts. Sociol Health Illn 2004;26:135-58. http://dx.doi.org/10.1111/j.1467-9566.2004.00384.x.
- Kovandžić M, Chew-Graham C, Reeve J, Edwards S, Peters S, Edge D, et al. Access to primary mental health care for hard-to-reach groups: from ‘silent suffering’ to ‘making it work’. Soc Sci Med 2011;72:763-72. http://dx.doi.org/10.1016/j.socscimed.2010.11.027.
- Chew-Graham C, Kovandžić M, Gask L, Burroughs H, Clarke P, Sanderson H, et al. Why may older people with depression not present to primary care? Messages from secondary analysis of qualitative data. Health Soc Care Community 2012;20:52-60. http://dx.doi.org/10.1111/j.1365-2524.2011.01015.x.
- Stevenson F, Scambler G. The relationship between medicine and the public: the challenge of concordance. Health 2005;9:5-21. http://dx.doi.org/10.1177/1363459305048091.
- Bristow K, Edwards S, Funnel E, Fisher L, Gask L, Dowrick C, et al. Help seeking and access to primary care for people from ‘hard-to-reach’ groups with common mental health problems [published online ahead of print 6 July 2011]. Int J Family Med 2011. http://dx.doi.org/10.1155/2011/490634.
- Murphy M, Black N, Lamping D, McKee C, Sanderson S, Askham A, et al. Consensus development methods, and their use in clinical guideline development. Health Technol Assess 1998;2.
- Bower P, Gask L, Lamb J, Burroughs H, Chew-Graham C, Edwards S, et al. Improving access to psychosocial interventions for common mental health problems in the United Kingdom: narrative review and development of a conceptual model for complex interventions. BMC Health Serv Res 2012;12.
- Dixon-Woods M, Agarwal S, Jones D, Young B, Sutton A. Synthesising qualitative and quantitative evidence: a review of possible methods. J Health Serv Res Policy 2005;10:45-53. http://dx.doi.org/10.1258/1355819052801804.
- Lovell K, Bower P, Richards D, Barkham M, Sibbald B, Roberts C, et al. Developing guided self-help for depression using the Medical Research Council complex interventions framework: a description of the modelling phase and results of an exploratory randomised controlled trial. BMC Psychiatry 2008;8. http://dx.doi.org/10.1186/1471-244X-8-91.
- Rahman A. Challenges and opportunities in developing a psychological intervention for perinatal depression in rural Pakistan – a multi-method study. Arch Womens Ment Health 2007;10:211-19. http://dx.doi.org/10.1007/s00737-007-0193-9.
- Pyne J, Rost K, Farahati F, Tripathi S, Smith J, Williams D, et al. One size fits all: the impact of patient treatment attitudes on the cost-effectiveness of a depression primary care intervention. Psychol Med 2004;35:839-54.
- King M, Nazareth I, Lampe F, Bower P, Chandler M, Morou M, et al. Impact of participant and physician intervention preferences on randomized trials: a systematic review. JAMA 2005;293:1089-99. http://dx.doi.org/10.1001/jama.293.9.1089.
- Pawson R, Tilley N. Realistic evaluation. London: Sage; 2011.
- Bodenheimer T, Wagner E, Grumbach K. Improving primary care for patients with chronic illness: the Chronic Care Model, part 2. JAMA 2002;288:1909-14. http://dx.doi.org/10.1001/jama.288.15.1909.
- Understanding Liverpool better: the Joint Director of Public Health report for 2008–9. Liverpool: Liverpool Primary Care Trust; 2009.
- Liverpool Primary Care Trust . Ward Profiles 2005–7 n.d. www.liverpoolpct.nhs.uk/Library/. . ./Princes%20Park.pdf (accessed August 2012).
- Picture of progress: compendium of statistics. Manchester: Manchester Primary Care Trust; 2007.
- Patton MQ. Qualitative research and evaluation methods. Thousand Oaks, CA: Sage; 2002.
- Ritchie J, Lewis J. Qualitative research practice. London: Sage; 2003.
- Corbin J, Strauss A. Basics of qualitative research: grounded theory procedures and techniques. London: Sage; 2008.
- Blake G. Community engagement and community cohesion. London: Joseph Rowntree Foundation; 2008.
- Wells KB, Miranda J, Bruce ML, Alegria M, Wallerstein N. Bridging community intervention and mental health services research. Am J Psychiatry 2004;161:955-63. http://dx.doi.org/10.1176/appi.ajp.161.6.955.
- Downe S, McKeown M, Johnson E, Koloczek L, Grunwald A, Malihi-Shoja L. The UCLAN community engagement and service user support (Comensus) project: valuing authenticity, making space for emergence. Health Expect 2007;10:392-406. http://dx.doi.org/10.1111/j.1369-7625.2007.00463.x.
- Braithwaite RL, Bianchi C, Taylor SE. Ethnographic approach to community organization and health empowerment. Health Educ Behav 1994;21:407-16. http://dx.doi.org/10.1177/109019819402100311.
- Lewin K. Action research and minority problems. J Soc Issues 1946;2:34-46. http://dx.doi.org/10.1111/j.1540-4560.1946.tb02295.x.
- Gold RL. The ethnographic method in sociology. Qual Inq 1997;3:388-402. http://dx.doi.org/10.1177/107780049700300402.
- Carpiano RM. Come take a walk with me: the ‘go-along’ interview as a novel method for studying the implications of place for health and well-being. Health Place 2009;15:263-72. http://dx.doi.org/10.1016/j.healthplace.2008.05.003.
- Biernacki P, Waldorf D. Snowball sampling: problems and techniques of chain referral sampling. Sociol Methods Res 1981;10:141-63.
- Kovandžić M, Funnell E, Hammond J, Ahmed A, Edwards S, Clarke P, et al. The space of access to primary mental health care: a qualitative case study. Health Place 2012;18:536-51. http://dx.doi.org/10.1016/j.healthplace.2012.01.011.
- Prime Minister’s Office . Government Launches Big Society Programme n.d. www.number10.gov.uk/news/topstorynews/2010/05/big-society-50248 (accessed August 2012).
- Dooris M. Joining up settings for health: a valuable investment for strategic partnerships?. Crit Public Health 2004;14:49-61. http://dx.doi.org/10.1080/09581590310001647506.
- Rubin V. Evaluating university–community partnerships: an examination of the evolution of questions and approaches. Cityscape 2000;5:219-30.
- Sikorski C, Luppa M, König HH, van den Bussche H, Riedel-Heller SG. Does GP training in depression care affect patient outcome? Systematic review and meta-analysis. BMC Health Serv Res 2012;12. http://dx.doi.org/10.1186/1472-6963-12-10.
- Gunn JM, Palmer VJ, Dowrick CF, Herrman HE, Griffiths FE, Kokanovic R, et al. Embedding effective depression care: using theory for primary care organisational and systems change. Implement Sci 2010;5. http://dx.doi.org/10.1186/1748-5908-5-62.
- Kennedy A, Chew-Graham C, Blakeman T, Bowen A, Gardner C, Protheroe J, et al. Delivering the WISE (Whole Systems Informing Self-Management Engagement) training package in primary care: learning from formative evaluation. Implement Sci 2010;5. http://dx.doi.org/10.1186/1748-5908-5-7.
- Grol R. Knowledge transfer in mental health care: how do we bring evidence into day-to-day practice?. Can J Psychiatry 2008;53:275-6.
- Hammond J, Gravenhorst K, Funnell E, Beatty S, Hibbert D, Lamb J, et al. Slaying the dragon myth: a qualitative study of receptionists in UK general practice. Br J Gen Pract 2013;63:e177-84.
- Savage J. Ethnography and health care. BMJ 2000;321:1400-2. http://dx.doi.org/10.1136/bmj.321.7273.1400.
- Emerson RM. Writing ethnographic fieldnotes. Chicago, IL: Chicago University Press; 1995.
- Arber S, Sawyer L. The role of the receptionist in general practice: a ‘dragon behind the desk’?. Soc Sci Med 1985;20:911-21. http://dx.doi.org/10.1016/0277-9536(85)90347-8.
- Offredy M. Access to primary care: decision making by GP receptionists. Br J Community Nurs 2002;7:480-5.
- Eisner M, Britten N. What do general practice receptionists think and feel about their work?. Br J Gen Pract 1999;49:103-6.
- Swinglehurst D, Greenhalgh T, Russell J, Myall M. Receptionist input to quality and safety in repeat prescribing in UK general practice: ethnographic case study. BMJ 2001;343. http://dx.doi.org/10.1136/bmj.d6788.
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606-13. http://dx.doi.org/10.1046/j.1525-1497.2001.016009606.x.
- Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166:1092-7. http://dx.doi.org/10.1001/archinte.166.10.1092.
- Mundt JC, Marks IM, Shear MK, Greist JH. The Work and Social Adjustment Scale: a simple measure of impairment in functioning. Br J Psychiatry 2002;180:461-4. http://dx.doi.org/10.1192/bjp.180.5.461.
- EuroQol Group . EuroQol: a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208.
- Evans C, Connell J, Barkham M, Margison F, McGrath G, Mellor-Clark J, et al. Towards a standardised brief outcome measure: psychometric properties and utility of the CORE-OM. Br J Psychiatry 2002;180:51-60. http://dx.doi.org/10.1192/bjp.180.1.51.
- Bower P, Knowles S, Coventry PA, Rowland N. Counselling for mental health and psychosocial problems in primary care. Cochrane Database Syst Rev 2011;9. http://dx.doi.org/10.1002/14651858.CD001025.pub3.
- Hunt CJ, Shepherd LM, Andrews G. Do doctors know best? Comments on a failed trial. Med J Aust 2001;174:144-9.
- Tognoni G, Alli C, Aranzini F, Bettelli G, Colombo F. Randomised clinical trials in general practice: lessons from a failure. BMJ 1991;303:969-71. http://dx.doi.org/10.1136/bmj.303.6808.969.
- Hetherton J, Matheson A, Robson M. Recruitment by GPs during consultations in a primary care randomized controlled trial comparing computerized psychological therapy with clinical psychology and routine GP care: problems and possible solutions. Prim Health Care Res Dev 2004;5:5-10. http://dx.doi.org/10.1191/1463423604pc168oa.
- Treweek S, Pitkethly M, Cook J, Kjeldstrøm M, Taskila T, Johansen M, et al. Strategies to improve recruitment to randomised controlled trials. Cochrane Database Syst Rev 2010;4. http://dx.doi.org/10.1002/14651858.MR000013.pub4.
- Richards D, Hughes-Morley A, Hayes R, Barkham M, Bland M, Bower P, et al. Collaborative Depression Trial (CADET): multi-centre randomised controlled trial of collaborative care for depression – study protocol. BMC Health Serv Res 2009;9. http://dx.doi.org/10.1186/1472-6963-9-188.
- Murray E, Treweek S, Pope C, MacFarlane A, Ballini L, Dowrick C, et al. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Med 2010;8. http://dx.doi.org/10.1186/1741-7015-8-63.
- Fletcher J, Gavin M, Harkness E, Gask L. A collaborative approach to embedding graduate primary care mental health workers in the UK National Health Service. Health Soc Care Community 2008;6:451-9. http://dx.doi.org/10.1111/j.1365-2524.2007.00754.x.
- Gask L, Lever-Green G, Hays R. Dissemination and implementation of suicide prevention training in one Scottish region. BMC Health Serv Res 2008;8. http://dx.doi.org/10.1186/1472-6963-8-246.
- Joint strategic needs assessment, statement of need. Liverpool: Liverpool City Council and Liverpool Primary Care Trust; 2011.
- The joint strategic framework for public mental health 2009–2012. Liverpool: Department of Public Health, Liverpool Primary Care Trust; 2009.
- Equity and excellence: liberating the NHS. London: Department of Health; 2010.
- Department of Health . Function of Clinical Commissioning Groups n.d. www.dh.gov.uk/health/2012/06/ccg-functions/ (accessed August 2012).
- Department of Health . Any Qualified Provider n.d. www.healthandcare.dh.gov.uk/any-qualified-provider-2/ (accessed August 2012).
- Garlick S, Palmer V. Toward an ideal relational ethic: rethinking university community engagement. Gateway 2008;1:73-89.
Appendix 1 Programme summary
National Institute for Health Research Programme Grants for Applied Research
Programme Summary
Aims and Objectives: To increase equity of access to high quality primary care mental health services for hard to reach groups. Objectives: to clarify mental health needs in these groups, identify relevant services and their barriers and facilitators, develop and test credible interventions, establish dissemination strategies and integrate new services into primary care.
Background and Rationale: Mental health problems impose substantial burdens patients, carers, and health-care systems. A wide range of interventions have demonstrable efficacy in improving the lives of people experiencing common but disabling mental health problems. However many people with high levels of mental distress are disadvantaged either because they are unable to access care (e.g. black and ethnic minorities, homeless, asylum seekers, adolescents with eating disorders), or because access does not lead to adequate care (e.g. people with unexplained symptoms, prolonged sickness absence, advanced cancers or older people with depression). Key research issues needing to be addressed include complex problem presentation and diagnostics in primary care, user defined perspectives on problem formulation, management and outcome, engagement and communication, and the professional context of mental health encounters.
Research Environment: Our team is strongly represented within the new National School for Primary Care, and key NHS bodies including the Mental Health Research Network and North West Primary Care Research Network.
Research Plans: The programme will link knowledge about barriers to access for our exemplar groups with the perspectives of users, and developing creative ways to meet the particular needs of these groups. Phase 1 (months 1 to 24): Understanding the Problems and Generating Potential Solutions. We will undertake a narrative review of barriers to access to care, and interventions to overcome these barriers, using a combination of systematic review, qualitative meta-synthesis techniques and interviews with service users and providers. We will focus on user perspectives on mental health issues in relation to each of the hard-to-reach groups, in order to understand whether there are any access issues specific to each group, and how different issues affect them all. We will then consider the results of our reviews, and use a consensus process to develop exemplar interventions which take account of known barriers while remaining sensitive to the needs, preferences and priorities of our exemplar hard-to-reach groups and other stakeholders. Phase 2 (months 19–48): Testing Potential Solutions. We will develop interventions in three domains: improving access (e.g. outreach, transport, accessibility, internet use), improving understanding (e.g. knowledge and attitudes of care providers, public understanding) and improving care (e.g. skills training, psychological interventions, self management, role of voluntary sector). We will test interventions in terms of acceptability and credibility to service users and other stakeholders, their impact on the mental health of service users, and their service implications and cost effectiveness. Phase 3 (months 43–60): Putting what Works into Practice. We will develop and evaluate methods to disseminate our findings across the broad economy of primary health care, including a focused implementation experiment in two PCT sites.
Projected Outputs and Dissemination Plan: Outputs will include resource packs with associated educational interventions. Outcomes: Improved knowledge, skills and case identification by care providers; new services sensitised to needs of hard to reach groups, with evidence of better access and outcomes; increased R&D capability of NHS staff. Impact: Increased equity of access to high-quality primary care mental health services.
Expertise of Research Team: We bring together internationally recognised mental health researchers from Universities of Liverpool and Manchester, with policy makers and managers from two Primary Care Trusts. We have substantial expertise in the range of methodologies necessary for applied health research, in service and diagnostic issues, and in the design and prosecution of trials and related interventions for our exemplar hard to reach groups.
Justification of Costs: We will integrate existing resource from our academic and NHS institutions with the resource directly associated with this programme, to provide an efficient and cost-effective mechanism for delivering on our aims and objectives. In order to achieve our objectives we expect to appoint a programme coordinator, two senior research fellows, four research assistants and a senior technician. Statistical and health economic expertise are important but not central to our objectives, and will be provided as required through consultancy arrangements.
Management and Governance: Our programme will direct by two chief investigators, with support from a Programme Management Group (meeting 6–8 times a year), an Advisory Group (meeting twice yearly) and an international group of experts. All aspects of the programme involving direct contact with NHS service users or providers will be the subject of applications for aproval to relevant Research Ethics Committees. The applicants include two Trust clinical directors and the lead of a service user organisation.
Patient and Public Involvement: Our programme ensures primary care user involvement at all stages, and hence will build strong academic–community partnerships. This includes:
-
(a) consultation with service users and their supporters to enable effective service redesign;
-
(b) collaboration with a service user as co-applicant, and others to be deployed to deliver interventions; and
-
(c) control: service user led self help clinics may be tested during the programme.
Appendix 2 Search strategy for the scoping review
Databases searched: CINAHL (nursing), EMBASE (emef), Ovid MEDLINE(R) (medf), PsycINFO (psya).
-
Models, theoretical/
-
what is.m_titl.
-
the meaning of.m_titl.
-
taxonomy.tw.
-
typology.tw.
-
conceptuali?ation.tw.
-
conceptually.tw.
-
(theor$ adj1 map$).tw.
-
(theor$ adj1 model$).tw.
-
(theor$ adj1 framework$).tw.
-
(theor$ adj1 meaning$).tw.
-
(theor$ adj1 approach$).tw.
-
(theor$ adj1 overview$).tw.
-
(theor$ adj1 feature$).tw.
-
(theor$ adj1 (mode or modes)).tw.
-
(theor$ adj1 characteristic$).tw.
-
(theor$ adj1 form?).tw.
-
(conceptual$ adj1 map$).tw.
-
(conceptual$ adj1 model$).tw.
-
(conceptual$ adj1 framework$).tw.
-
(conceptual$ adj1 meaning$).tw.
-
(conceptual$ adj1 approach$).tw.
-
(conceptual$ adj1 overview$).tw.
-
(conceptual$ adj1 feature$).tw.
-
(conceptual$ adj1 (mode or modes)).tw.
-
(conceptual$ adj1 characteristic$).tw.
-
(conceptual$ adj1 form?).tw.
-
(defin$ adj1 map$).tw.
-
(defin$ adj1 model$).tw.
-
(defin$ adj1 framework$).tw.
-
(defin$ adj1 meaning$).tw.
-
(defin$ adj1 approach$).tw.
-
(defin$ adj1 overview$).tw.
-
(defin$ adj1 feature$).tw.
-
(defin$ adj1 (mode or modes)).tw.
-
(defin$ adj1 characteristic$).tw.
-
(defin$ adj1 form?).tw.
-
((theor$ or conceptual$ or defin$) adj1 (scheme or schema)).tw.
-
(literature adj1 analys?s).tw.
-
1 or 2…or 38 or 39
-
(access adj5 care).mp. [mp=ti, hw, ab, it, sh, tn, ot, dm, mf, nm, tc, id]
-
40 and 41
Appendix 3 Search strategy for the meta-synthesis of published qualitative literature
Databases searched: MEDLINE, CINAHL, PsycINFO, EMBASE, ASSIA and Web of Knowledge.
-
exp continental population groups/
-
exp ethnic groups/
-
prejudice/
-
exp culture/
-
transcultural nursing/
-
arab$.ti,ab.
-
bangla$.ti,ab.
-
bengali.ti,ab.
-
cantonese.ti,ab.
-
creole.ti,ab.
-
farsi.ti,ab.
-
french.ti,ab.
-
gaelic.ti,ab.
-
guj?rati.ti,ab.
-
hakka.ti,ab.
-
hindi.ti,ab.
-
kashmiri.ti,ab.
-
korean.ti,ab.
-
kurdish.ti,ab.
-
mandarin.ti,ab.
-
mirpur$.ti,ab.
-
nepali.ti,ab.
-
pashto.ti,ab.
-
patois.ti,ab.
-
polish.ti,ab.
-
p?njabi.ti,ab.
-
somali.ti,ab.
-
spanish.ti,ab.
-
sylheti.ti,ab.
-
tamil.ti,ab.
-
turkish.ti,ab.
-
urdu.ti,ab.
-
vietnamese.ti,ab.
-
welsh.ti,ab.
-
yoruba$.ti,ab.
-
africa$.ti,ab.
-
african-american.ti,ab.
-
afro-caribbean.ti,ab.
-
african-carribean.ti,ab.
-
anti-racist.ti,ab.
-
anti-racism.ti,ab.
-
asian.ti,ab.
-
asylum.ab,ti.
-
carribean$.ti,ab.
-
blacks.ti,ab.
-
crosscultural.ti,ab.
-
cross cultural.ti,ab.
-
diversity.ti,ab.
-
equal opportunit$.ti,ab.
-
equality.ti,ab.
-
(ethnic$ adj3 minorit$).ab,ti.
-
ethnic$.ti,ab.
-
ethnographic$.ti,ab.
-
ethnology.ti,ab.
-
gypsy.ti,ab.
-
gypsies.ti,ab.
-
immigration.ti,ab.
-
immigrant$.ab,ti.
-
indian.ti,ab.
-
jamaica$.ti,ab.
-
minorit$3.ti,ab.
-
migrant$.ab,ti.
-
mixed race.ti,ab.
-
multi racial.ti,ab.
-
multiracial.ti,ab.
-
multi cultural.ti,ab.
-
multicultural.ti,ab.
-
multi ethnic.ti,ab.
-
multiethnic.ti,ab.
-
multi lingual.ti,ab.
-
multilingual.ti,ab.
-
pakistan$.ti,ab.
-
race.ti,ab.
-
racial$.ti,ab.
-
racism.ti,ab.
-
racist.ti,ab.
-
refugee$.ti,ab.
-
(religion or religious).ti,ab.
-
romany.ti,ab.
-
(social adj (inclusion or exclusion)).ti,ab.
-
social$ excluded.ti,ab.
-
social$ inclu$.ti,ab.
-
transcultural.ti,ab.
-
trans cultural.ti,ab.
-
trans racial.ti,ab.
-
transracial.ti,ab.
-
traveller.ti,ab.
-
or/1-87
-
Qualitative Research/
-
Focus Groups/
-
Nursing Methodology Research/
-
qualitative.tw.
-
((ethnographic or ethnological or ethnology) adj2 (research or study)).tw.
-
(grounded adj2 (theor$ or study or studies or research or analysis)).tw.
-
((theme or thematic or themes) adj2 analysis).tw.
-
content analysis.tw.
-
constant comparative method$.tw.
-
field notes.tw.
-
participant observation.tw.
-
narrative analysis.tw.
-
(naturalistic adj2 field study).tw.
-
(audiorecording or audio recording).tw.
-
focus group$.tw.
-
(conversation analysis or discourse analysis).tw.
-
hermeneutic.tw.
-
((phenomenology or phenomenological) adj2 research).tw.
-
(semi-structured adj2 (question$ or interview$)).tw.
-
(key informant adj2 (question$ or interview$)).tw.
-
((unstructured or un-structured) adj2 (question$ or interview$)).tw.
-
(tape recorded or tape recording).tw.
-
ethnonursing.tw.
-
lived experience.tw.
-
((life or womens) adj2 (story or stories)).tw.
-
Life world$.tw.
-
((theoretical or purposive) adj1 (sample or sampling)).tw.
-
or/89-115
-
exp mental Health/
-
exp depression/
-
117 or 118
-
88 and 116 and 119
Appendix 4 Flyer for stakeholder perspectives
Appendix 5 Longsight 2011 calendar
Appendix 6 Calendar 20(L)11
Appendix 7 Topic guide for phase 2 evaluation interviews
The objective of these interviews is to gather information on the impact of AMP interventions at community and primary care levels. Data will be gathered between Easter and December 2011, using focus group or individual interviews as appropriate. Telephone interviews are acceptable.
Community engagement
About 30 participants will be recruited (i.e. about seven or eight in each locality). Purposive sampling to include CFG invitees in Longsight and Croxteth. In Picton/Granby and Wythenshawe, sample from those stakeholders who would have been invited to CFGs if we had organised them: include primary care and third sector; and local residents as well as non-residents.
1. Prompts for Longsight and Croxteth
-
How do you think priorities for mental health care differ between the voluntary sector and primary care?
-
Do you have a clearer understanding of [voluntary sector] [primary care] than you did before the CFG was set up?
-
Have links/relationships/contacts between the voluntary sector and primary care changed?
-
If yes, in what ways?
-
Role (if any) of CFG?
-
-
If yes, what impact have these changes had, or could they have?
-
Do you think any changes will last?
-
If yes, what would that depend on?
-
-
-
What other factors have influenced/may influence relationships between the voluntary sector and primary care
-
E.g. other local initiatives, policies on big society, cuts in funding.
-
-
Have you heard about the AMP programme's well-being intervention?
-
If yes, have you referred anyone to it?
-
Are there any particular reasons why you did or didn't refer anyone to the well-being intervention? Are there any particular barriers to making a referral?
-
2. Prompts for Picton/Granby and Wythenshawe
-
How do you think priorities for mental health care differ between the voluntary sector and primary care?
-
Do you have a clearer understanding of [voluntary sector] [primary care] than you did 2 years ago?
-
Have links/relationships/contacts between the voluntary sector and primary care changed?
-
If yes, in what ways?
-
If yes, what impact have these changes had, or could they have?
-
Do you think any changes will last?
-
If yes, what would that depend on?
-
-
-
What factors have influenced/may influence relationships between the voluntary sector and primary care
-
E.g. local initiatives, policies on big society, cuts in funding.
-
-
Have you heard about the AMP programme's well-being intervention?
-
If yes, have you referred anyone to it?
-
Are there any particular reasons why you did or didn't refer anyone to the well-being intervention? Are there any particular barriers to making a referral?
-
Primary care
Aim for two key informants from each practice including controls. Key informants could be a GP, practice manager, staff who've experienced the training, e.g. receptionists and/or practice nurses.
1. Prompts for intervention practices that engaged with AMP trainingplus
-
What (if anything) do you know about AMP?
-
Getting involved:
-
What encouraged you to get involved (what was the selling point)?
-
What encouraged you to stay involved?
-
Provide a brief summary of the AMP trainingplus experience for that particular practice, with reference to the ethnographic exercise and each of the three training strands (knowledge transfer, systems review, active linking):
-
What worked, what didn't/‘how was our driving?’
-
Were the aims/intentions clear?
-
Did training content/scope meet needs?
-
Level of intrusiveness/flexibility
-
Was it as you expected?
-
Has anything changed in the practice as a result?
-
If so, how did this happen?
-
Has the change had any effects (e.g. on access/patient care)?
-
-
-
Staying involved:
-
Do you intend to continue with this change?
-
Are you more or less likely to do similar things in future?
-
-
More generally:
-
About AMP trainingplus:
-
Was anything missing from AMP trainingplus?
-
What could have been done differently?
-
How could we improve our approach/content if we were to roll this out more widely?
-
-
About community engagement (Longsight and Croxteth only):
-
What did you understand by AMP's ‘community engagement’?
-
(How) did it impact on your practice?
-
-
About the well-being interventions:
-
Have you had any experience of the AMP well-being interventions?
-
Did you refer patients? Did any patients talk about their experiences?
-
Do you have any particular reservations or concerns about referring patients to the AMP well-being intervention?
-
Did the well-being intervention fit with the AMP training (and community engagement)?
-
-
(Apart from any AMP-related changes), what has changed in the practice in the past 2 years, with regard to mental health care?
-
What were any changes related to, e.g. practice initiatives, PCT initiatives, changes in mental health services?
-
-
2. Prompts for intervention practices that did not engage
-
What (if anything) do you know about AMP?
-
What discouraged/hindered you from getting involved with AMP trainingplus?
-
Compare with another initiative you did get involved with.
-
What could we have done differently?
-
-
Do you think you missed out on anything because you didn't get involved?
-
About community engagement (Longsight and Croxteth only):
-
What did you understand by AMP's ‘community engagement’?
-
(How) did it impact on your practice?
-
-
About the well-being interventions:
-
Have you had any experience of the AMP well-being interventions?
-
Did you refer patients? Did any patients talk about their experiences?
-
Do you have any particular reservations or concerns about referring patients to the AMP well-being intervention?
-
Did the well-being intervention fit with the AMP training (and community engagement)?
-
-
What (if anything) has changed in the practice in the past 2 years, with regard to mental health care?
-
What were any changes related to, e.g. practice initiatives, PCT initiatives, changes in mental health services?
-
3. Prompts for control practices
-
What (if anything) do you know about AMP?
-
What (if anything) have you learnt about AMP trainingplus?
-
Would you be interested in getting involved in such an initiative in the future?
-
What would encourage/discourage you from doing so?
-
If you did get involved, what do you think would be the benefits, and for whom?
-
-
About community engagement (Longsight and Croxteth only):
-
What (if anything) did you understand by AMP's ‘community engagement’?
-
(How) did it impact on your practice?
-
-
About the well-being interventions:
-
Have you had any experience of the AMP well-being interventions?
-
Did you refer patients? Did any patients talk about their experiences?
-
Do you have any particular reservations or concerns about referring patients to the AMP well-being intervention?
-
Did the well-being intervention fit with the AMP training (and community engagement)?
-
-
What (if anything) has changed in the practice in the past 2 years, with regard to mental health care?
-
What were any changes related to, e.g. practice initiatives, PCT initiatives, changes in mental health services?
-
Appendix 8 Information sheet for practices
Appendix 9 Menu of training options for practices
Appendix 10 Well-being intervention: information booklet for patients
Well-being intervention: information booklet for patients (PDF download)
Appendix 11 First page of Clinical Outcomes in Routine Evaluation
First page of Clinical Outcomes in Routine Evaluation (PDF download)
Appendix 12 Patient Health Questionnaire
Appendix 13 Generalised Anxiety Disorder 7-item scale
| Over the last 2 weeks, how often have you been bothered by the following problems? | Not at all sure | Several days | Over half the days | Nearly every day |
|---|---|---|---|---|
| Feeling nervous, anxious or on edge | 0 | 1 | 2 | 3 |
| Not being able to stop or control worrying | 0 | 1 | 2 | 3 |
| Worrying too much about different things | 0 | 1 | 2 | 3 |
| Trouble relaxing | 0 | 1 | 2 | 3 |
| Being so restless that it's hard to sit still | 0 | 1 | 2 | 3 |
| Becoming easily annoyed or irritable | 0 | 1 | 2 | 3 |
| Feeling afraid as if something awful might happen | 0 | 1 | 2 | 3 |
| Add the score for each column | ||||
| Total score (add your column scores) |
If you checked off any problems, how difficult have these problems made it for you to do your work, take care of things at home or get along with other people?
Not difficult at all ___
Somewhat difficult ___
Very difficult ___
Extremely difficult ___
Appendix 14 Work and Social Adjustment Scale
Rate each of the following questions on a 0–8 scale (0 indicates no impairment at all and 8 indicates very severe impairment):
Because of my [disorder], my ability to work is impaired. 0 means not at all impaired and 8 means very severely impaired to the point I can't work.
| 0 means not at all impaired | 8 means very severely impaired | |||||||
|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
Because of my [disorder], my home management (cleaning, tidying, shopping, cooking, looking after home or children, paying bills) is impaired. 0 means not at all impaired and 8 means very severely impaired.
| 0 means not at all impaired | 8 means very severely impaired | |||||||
|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
Because of my [disorder], my social leisure activities (with other people, such as parties, bars, clubs, outings, visits, dating, home entertainment) are impaired. 0 means not at all impaired and 8 means very severely impaired.
| 0 means not at all impaired | 8 means very severely impaired | |||||||
|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
Because of my [disorder], my private leisure activities (done alone, such as reading, gardening, collecting, sewing, walking alone) are impaired. 0 means not at all impaired and 8 means very severely impaired.
| 0 means not at all impaired | 8 means very severely impaired | |||||||
|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
Because of my [disorder], my ability to form and maintain close relationships with others, including those I live with, is impaired. 0 means not at all impaired and 8 means very severely impaired.
| 0 means not at all impaired | 8 means very severely impaired | |||||||
|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
Appendix 15 European Quality of life-5 dimensions
Reproduced with permission from the EuroQoL Group.
Appendix 16 Case study W030
Contact
-
One initial assessment.
-
Eight face-to-face sessions over 9 weeks.
Method of referral
W030 was referred to the AMP programme through her GP. She stated that she found it hard to ask for help and so waited until she felt that was the only option. She would not normally have spoken to her GP about mental well-being concerns as she felt that the GP did not provide enough time for her and it was not something that should be spoken about to a GP. Since being involved with the AMP programme, W030 has discussed her concerns with her GP and is currently awaiting contact from the psychologist.
Initial contact
W030 was easily contactable by telephone and was willing to engage.
On-going contact
W030 expressed a wish to be seen at home. This worked well and she never missed or cancelled a session. Later she stated that if she had had to come to an external location she would not have come to the appointments. This was for a number of reasons relating to anxiety about going out, finding it hard to keep appointments and getting motivated to go out. For the final session we agreed that she would come to an external location as part of her therapeutic process. She kept to this appointment and this was a big part of her therapeutic process.
I believe that the flexibility afforded to her in being able to see her in her home was crucial to W030 continuing with the therapy.
Social engagement
W030 showed no interest in group work or organised social activities at first. By the third session she was keen to join the AMP group and felt that it would be good for her. She did not attend because of anxiety about new group situations but has since made moves to attend local community groups and feels that this will help her continue the work that we did in the sessions. For the final one-to-one session she came to the resource centre and took away information about the activities there; she had also been out more and discovered some other activities in the community that she wanted to engage in such as a coffee morning and IT lessons.
Other
W030 was stunned at her own progress during the therapy. She stated that her relationship with her husband had improved. He also reported this to me after the final session.
W030 said that she had made an appointment to see the smoking cessation nurse as she felt that she ‘had the strength’ to give up smoking now. She also reported a decrease in obsessive–compulsive disorder-type behaviours, tearfulness and panic.
Appendix 17 Case study W019
Contact
-
One initial assessment.
-
Nine face-to-face sessions over 11 weeks.
-
Eight group sessions over 8 weeks.
Method of referral
W019 was referred to the AMP programme through her GP.
Initial contact
W019 was initially difficult to contact. At the third attempt to contact her by telephone I managed to get hold of her and she seemed reluctant to engage, putting obstacles in the way of possible appointments. She agreed to a date 2 weeks from that telephone call but then cancelled on the day and said that she would call me back the following week. After not hearing from her for 2 weeks I recontacted her and asked her if she was still interested and she agreed to a date the following week.
In total, from the first attempt at contact it took 8 weeks and eight contacts/attempts at contact to complete the initial assessment.
W019 stated that this difficulty was because she was anxious about the unknown regarding the sessions and so found it hard to commit to attending. She felt panicky and was visibly shaking and nervous at her first session. She also thought that perhaps others needed the service more than her and wasn't sure if she was really suitable (i.e. not ‘in need’ enough). However, she decided to attend as she did want to speak to someone about her ‘troubles’.
It was clear from the beginning that W019 would benefit from this service and by the final few sessions she stated as much. I believe that she would never have attended had she received only one/two telephone calls or a letter.
Ongoing contact
One of the reasons why W019 stated that she had cancelled the first appointment was because she didn't want to go to the area in which I was located because of unpleasant memories of her past associated with that area. Therefore, I arranged to see her at her GP surgery, which she felt more comfortable with, and she subsequently committed to the sessions and attended each one.
Note: the extra work from my perspective of booking a room at the GP surgery was significant as the room could not be booked in advance and, therefore, I was required to telephone each week (sometimes more than once as I had to speak to the practice manager). I got the general impression that the practice was uncomfortable with me using its rooms. However, when W019 spoke to her GP, the GP was pleased to have the service on site.
Because W019 had decided to attend the group at the resource centre she agreed that we would transfer our sessions there so that she could have them straight after the group. This worked well and she attended every group and one-to-one session. This worked so well in fact that she has gone on to be a volunteer there and feels very safe and comfortable. The resource centre has become a safe haven-like environment for her.
In total, she received four sessions at the GP surgery and six sessions at the resource centre.
Social engagement
W019 engaged well in the group and, although feeling sceptical to begin with, states that she has gained a lot from the group. She has signed up to be a volunteer and would like to continue using Wednesday mornings to come to the resource centre to receive the social activity and engagement that has boosted her confidence, self-esteem and self-worth. Although relatively active generally, she has realised the importance to her well-being of getting out and engaging socially and so places great importance on continuing with this. I believe this is a result of the group work as well as the one-to-one sessions with AMP.
Appendix 18 Interview schedule guide for participant evaluation of the well-being intervention
1. Opening
Clarify ethical implications, confidentiality and consent
Ensure that participants have read and signed the consent form. Emphasise that the data from the interview will be treated in a confidential manner and that they can stop at any point without negative consequences, and ask them if they have any questions.
Explain the AMP programme and the aims of the research
The aim of the AMP programme is to find ways that will make it easier for people to get help for common mental health problems. We want to understand what problems people face in accessing mental health care when they need it. We also want to find the ways to solve and prevent these problems. In other words, we are looking at how to make available the right type of help in the right way, right time and right place. The well-being programme, which you (or someone you know) has completed, has been part of our attempt to do this.
Explain the purpose of the interview
We are interested in getting some feedback about people's experiences of the well-being programme that they have either completed personally, or experienced indirectly through a friend, family member or someone they care for. We want to know about what has and what hasn't worked for people, and try and understand the reasons for this.
Highlight the areas to be covered
I'd like to find out your views on how you found out about the well-being programme, why you decided to take part in it, what it was like and what effects (if any) it has had on you. I'd also like to find out how you have been since you saw [insert name of person who did baseline assessment]. I'd like to know what's happened since, whether you've received any help, if things have improved and whether you're satisfied with what's happened.
Invite and answer any questions
I. Discovery
How did you first find out about the programme? Who told you about it?
Were you given a choice about the content of your well-being programme?
If so, were you given enough information to help you make your choice?
II. Engagement
What was it that made you decide to try the programme? (Try and find out about background/personal circumstances of participant)
Did you have any reservations about taking part? (How were these overcome?)
Was there anything in particular that made it easier to take part? Did anyone help you?
2. Views on reasons for accessing the intervention
Examine case notes in advance to establish what particular intervention the participant was offered, and whether they accepted it.
Aim: Participants will have been randomised to either the control or the intervention arm. The latter involves a variety of possible options, such as group sessions, individual sessions or signposting. Explore their opinions about what they were offered.
Those randomised to the intervention arm:
I think you went to see [insert name of well-being facilitator] who did an assessment. How did you find that assessment? Was it easy or difficult to talk about your problem(s)? Did you feel that [insert name of well-being facilitator] was interested in you and understood your problem?
After your assessment/after you saw [insert name of person who did the baseline interview]:
Did he/she give you any ideas about help that might be available? What kind of things were you offered?
Did any of them put you off straight away? Why? Did you find anything particularly appealing? Why?
What was it that influenced your decision to choose what you did? Did the facilitator persuade you to try something that you might not have thought of?
Can you talk a bit about [insert name of well-being facilitator] the well-being facilitator? (How much contact did you have with them? What did you think about their approach? Did you get on with them? Were they friendly? Did you feel that they listened to you properly? And understood what you needed? Did you look forward to seeing them? Do you think seeing the facilitator made you feel better?)
3. Experiences of receiving the intervention
Aim: Encourage the participant to provide a descriptive overview of the programme that they received. Encourage the participant to explore their opinions about the strengths and weaknesses of the programme. Primary areas of questioning: format, delivery, time and location.
I. Format
How many people were there?
What did you do?
Did the sessions change over time or was each one much the same as the rest?
II. Delivery
Who led the sessions?
What did you think of their approach?
III. Time
How did you find the length of each session?
How often were they? (Was that frequent enough/not frequent enough?)
Were you happy with the number of sessions overall?
IV. Location
Where did the sessions take place?
Was it easy to get to?
Did you require any special travel arrangements?
4. Views on outcomes
Aim: Investigate the perceived impacts the intervention has had on those who have taken part.
How do you think that taking part in the well-being programme has had an effect on you personally (positive/negative)? Has it helped you? In what ways?
Can you give some examples of this? (Try and relate questions on outcomes to the specific circumstances and well-being issues of the individual in question)
Did you enjoy the sessions? Did you look forward to them? Were they better than you anticipated?
Are you satisfied with what you were offered? Would you recommend it to other people?
Was there anything you didn't like or would change?
5. Closing
Aim: Summarise some of the participant's main thoughts for clarity.
Ask if there is anything else that hasn't been covered; particularly other suggestions for how the programme could be improved.
Explain the next stages of the programme and how the interview data will be used in relation to them.
Is there anything that you'd have liked me to ask about but I didn't?
Do you have any further suggestions for how the well-being programme could be improved in the future?
List of abbreviations
- AMP
- Improving Access to Mental Health in Primary Care
- BME
- black and minority ethnic
- CBT
- cognitive–behavioural therapy
- CC
- Community Champion
- CCG
- clinical commissioning group
- CFG
- consultative focus group
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CONSORT
- Consolidated Standards of Reporting Trials
- CORE-OM
- Clinical Outcomes in Routine Evaluation
- CWG
- community working group
- DARE
- Database of Abstracts of Reviews of Effects
- EQ-5D
- European Quality of life-5 dimensions
- GAD-7
- Generalised Anxiety Disorder 7-item scale
- GP
- general practitioner
- IAPT
- Improving Access to Psychological Therapies
- IMD
- Index of Multiple Deprivation
- NICE
- National Institute for Health and Care Excellence
- ONS
- Office for National Statistics
- PHQ-9
- Patient Health Questionnaire
- PCT
- primary care trust
- PTSD
- post-traumatic stress disorder
- PWP
- psychological well-being practitioner
- QOF
- Quality and Outcomes Framework
- R&D
- research and development
- RCT
- randomised controlled trial
- SOA
- super output area
- WSAS
- Work and Social Adjustment Scale
