Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 17/149/19. The contractual start date was in April 2019. The final report began editorial review in July 2021 and was accepted for publication in March 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2022 Jepson et al. This work was produced by Jepson et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Jepson et al.
Chapter 1 Introduction
Background to the study
The origins of this study are in a master’s in Public Health project; it was developed by students who were taking a module on ‘Developing and Evaluating Complex Interventions’. This module was developed and delivered by Ruth Jepson and members of the Scottish Collaboration for Public Health Research and Policy for the Master’s in Public Health at The University of Edinburgh, Scotland. As part of the module assessment, all students were to submit a team proposal for an intervention based on the 6 Steps in Quality Intervention Development (6SQuID) framework (this framework was developed by Ruth Jepson, Danny Wight, Erica Wimbush and Lawrence Doi). The students presented their proposal to a mock grant panel and a winning project was selected. Stand Up for Health (SUH) was the winning project in 2016. The module team believed that SUH had great potential and so decided to further develop and pilot it with members of the student team.
Ruth Jepson worked with the students to reach out to contact centres (also known as call centres) in the Edinburgh area. One contact centre, Ipsos MORI (Edinburgh, UK), responded positively and the team was able to start piloting work and developing both a theory of change and a theory of action (see Figures 2 and 4). Following this pilot, the team was able to develop this larger feasibility study. Although none of the original students is still involved directly in the project, several of them still have close links with the Scottish Collaboration for Public Health Research and Policy.
Evidence supporting the study
Sedentary behaviour as a public health problem
Sedentary behaviour is a serious occupational health hazard, which is linked with an increased risk of type 2 diabetes, cardiovascular disease, musculoskeletal issues and poor mental well-being. 1–6 Earlier research studies proposed that these risks are independent of physical activity7,8 given that, conceptually, sedentary behaviour and physical activity are different,9 with each thought to pose health risks independent of each other. 5,10–12 However, more recent research shows that, although physical activity can modify the associations between health risks and sedentary behaviour,13,14 health effects of sedentary behaviour are still evident even after controlling for physical activity. 4,5,12,15 A review16 of behaviour change strategies that are used for the reduction of sedentary behaviour among adults reported that interventions that showed the most promise in reducing sitting time were those that aimed to changed sedentary behaviour rather than increase physical activity. The reduction of sedentary behaviour is, therefore, not a consequence of effectively promoting physical activity and should be recognised independently when developing interventions, guidelines and legislation.
Workplace sedentary behaviour is placing a large burden on employers and the health-care system. In office-based roles, many employees have prolonged periods of sitting, which are enforced by workplace culture and ergonomic set-up. 17 This sitting behaviour can impact on the health of office-based workers. For example, musculoskeletal issues are a leading cause of disability worldwide and one of the most common health problems for desk-based workers. 18–20 Estimates of the prevalence of musculoskeletal symptoms in computer users are as high as 50%. 21 Lower back pain in particular is associated with prolonged sitting. 22
Factors associated with sedentary behaviour in workplaces
A cross-sectional study conducted among Australian adults23 found that the following were associated with higher levels of occupational sitting: being male; being younger; having higher education and income; both part-time and full-time employment; sedentary job tasks; white-collar or professional occupations; and higher body mass index (BMI). Some of these findings were corroborated by a systematic review of occupational correlates for sedentary behaviour. 24 The review identified full-time employment, working in a call centre, high level of leisure sitting time, high body weight, being older, high education and high income levels as positive correlates, and blue-collar occupations and smoking as negative correlates. 24 Political correlates (described as incentivisation, coercion and job description) that were identified included repetitive work, handling heavy loads and forceful exertion, which were found to be negatively associated with occupational sedentary behaviour. Low control or autonomy was found to have a positive association.
Qualitative studies conducted with employees and managers in a UK-based software engineering company25 and non-academic office staff at a university in Singapore26 have identified several barriers to reducing sedentary behaviour in workplaces, including workplace social and cultural norms (sitting is perceived to be a reflection of productivity by themselves and others, whereas standing is seen as disturbing others), work pressures (pressure to deliver work), the nature of the job requiring more sitting (e.g. working with computers) and physical environment and office infrastructure (small office spaces, no adjustable workstations and lack of facilities).
Contact centres as a setting for public health interventions
There are over 6200 contact centres in the UK, employing 734,000 agents,27 which is roughly 1 in 25 of the UK workforce. Scotland and the North East of England are home to some of the largest contact centres in Europe. Workplaces are often considered as homogeneous, but there are wide variations in worker demographics, the amount of worker autonomy, salaries, the environment and culture.
The call handlers (the highest proportion of contact centre staff) earn an average salary of £16,319 per year, compared with the national average of £26,500, which puts them in the bottom third of earners. 28 An industry report that collected data from 208 contact centre managers and directors using a structured questionnaire reported that turnover rates are high in UK contact centres, with an average attrition rate of 20% reported in 2020. 29 Short-term absence rates are also high, with 5.7% of agent workdays being lost to short-term sickness and unauthorised absences. 29 Career progression is limited, and a lack of promotion and development opportunities has been reported as the second greatest cause of employee attrition. 29
Contact centres and health
Contact centres are currently one of the most sedentary working environments, with higher levels of sedentary behaviour than other office-based work. 24,30 Studies have reported that contact centre staff spend 75–83% of their workday sitting. 30,31 The technology in contact centres prevents staff from regularly leaving their desk and many call handlers often report that work environments are stressful owing to low workplace autonomy, strict supervision of individual performance and commission-based salary systems. 32 Several international studies33,34 show that as many as 60–65% of contact centre employees experience musculoskeletal issues, and a study in the UK35 noted that one in four employees at a contact centre experienced upper body musculoskeletal issues.
A recent study32 found that a common factor for sedentary behaviour shared by contact centre agents, team leaders and senior staff was a considerable lack of knowledge and awareness of sedentary behaviour as a risk factor for poor health. In addition, there was a low level of knowledge among staff of guidelines and recommendations relating to sedentary behaviour and physical activity in the workplace, and therefore there is often no reflection of these guidelines and recommendations in organisational policies. 32,36
Contact centres and organisational drivers
Many organisations representing the contact centre industry are highly constrained by profit-based drivers, cost minimisation and economic outcomes based on productivity and high-quantity customer enquiry resolution. 37 Several contact centres adopt ‘mass production models’ to minimise cost and maximise output, resulting in mechanisation and standardisation of work methods, and reduced employee training and autonomy. 37 The work is such that employees do not engage with other team members and can be isolating, and employees may view themselves as replaceable. 37 These factors can also often influence organisational investment into workplace health initiatives; fears of cost-ineffective programmes and reduced productivity rates are commonly presented by senior team leaders within private contact centres. 32
Contact centre agents have voiced concerns over job security and performance monitoring, and a desire for increased autonomy over their working practices, as influential factors for their motivation to participate in strategies to reduce sedentary behaviour in the workplace. 32 However, organisational pressures to maintain high levels of productivity and meet targets frequently work against organisational investment into health and physical activity programmes within some contact centres. This is often due to perceptions that these activities will reduce the agents’ call-making time and lead to productivity losses. 38 One study reported that leaders and senior staff had ‘identified a conflict between promoting productivity and targets to call agents, while encouraging them to move more and sit less’. 32
Workplace intervention research to reduce sedentary behaviour
Over the last 5–10 years, there have been several systematic reviews of workplace interventions to increase physical activity and reduce sedentary behaviour. 24,39–41 Most recently, a systematic review of environmental interventions in workplaces (e.g. sit-to-stand desks)40 found evidence of significant reductions in sedentary behaviour in 14 out of 15 studies. This review found that multicomponent interventions that targeted more than one level of the socioecological framework, were most effective. In 2016, another systematic review41 assessed the effectiveness of white-collar workplace interventions to reduce sedentary time; it similarly found that multicomponent interventions had the greatest effect. Both reviews40,41 identified a need to assess whether policy-based measures or organisational change could further increase effectiveness. One study42 assessed the effect of sit–stand desks and ergonomic awareness on reducing sedentary behaviour in 15 Swedish contact centres and found that working at a sit–stand desk was associated with a slightly greater reduction in sitting time than sitting at a non-sit–stand desk. Regular interruptions to sitting time during the workday have previously been found to significantly reduce discomfort in the lower back and fatigue levels in overweight and obese office workers, without affecting productivity. 43 Another study44 found that the use of standing desks led to significant reductions in upper back and neck pain in office workers. A recent study45 exploring barriers to participation suggested that ‘barriers occurred at multiple levels of influence, and support the use of ecological or multilevel models to help guide future programme design/delivery’. 45
Multicomponent workplace interventions
Given the specified need to address cultural and organisational factors affecting workplace behaviour, we developed and piloted SUH (the intervention in this report). There are a limited number of other similar interventions and the evidence is still sparse, with only one UK-based study, which is ongoing. This UK-based study is funded by the National Institute for Health and Care Research (NIHR) Public Health Research (PHR) programme46 and is currently examining the effectiveness of the Stand More AT Work (SMArT Work) and life intervention aimed at reducing sitting time of office workers. Although this intervention is similar to our intervention in some respects, SUH specifically considers aspects of organisational change, targets contact centres and takes a systems-based approach. 47 This takes into account the complexity of the context, resources and assets of specific contact centres. The Stand Up Victoria study in Australia48,49 also had a multicomponent intervention. However, height-adjustable workstations were a main part of the intervention. Although we envisaged that some contact centres would take up this option, we recognised that not all contact centres have the resources, or desire, to implement them. A third study in Perth, Australia,50 used a similar participatory approach to SUH but had no theoretical basis and was assessed at only a 12-week time point.
Sedentary behaviour research in contact centres in the UK
Research on sedentary behaviour in contact centres is sparse and no reviews were identified on this topic. Two relevant primary studies are discussed here. 32,51 The first study32 is a qualitative study exploring factors that influence contact centre agents’ physical activity and sedentary behaviour in the workplace. The study conducted interviews with contact centre agents, team leaders and senior staff, and reported that agents said that several factors influenced their motivation to increase physical activity and reduce sitting time, including continuous performance monitoring, concerns over job security and a desire for increased autonomy in the workplace. As mentioned in Contact centres and organisational drivers, the study noted the conflict reported by team leaders and senior staff relating to productivity and promoting more movement and sitting less.
Another study51 used a mixed-methods approach to explore the acceptability and feasibility of a multicomponent intervention that targeted physical activity and prolonged sitting in contact centres. The study reported that contact centre agents perceived that the study assessments were acceptable and education sessions, height-adjustable workstations and e-mails were seen to be the most effective components. This intervention is also based on the socioecological model and is similar to the SUH programme. Although the intervention51 has several merits, SUH has a greater emphasis on organisational factors and takes an adaptive and flexible approach, taking into account the contexts and systems of each contact centre.
Relevant policy and practice
Policy regarding sedentary behaviour is insufficient considering the evidence of its associated risks. A recent study reviewed current national and international occupational safety and health policy documents (e.g. guidelines, legislation and codes of practice) for their relevance to occupational sedentary behaviour. 36 The review found that many workplaces and jurisdictions had legal frameworks that established a duty of care for occupational health, but discovered that no occupational health and safety authority had a policy specifically targeting occupational sedentary behaviour. Although some existing policies have aspects relevant to sedentary behaviour in the workplace, the authors identified a need to address the emergent hazard of excessive occupational sedentary behaviour by developing specific policies for this issue. They also highlight a need to support workplace-based initiatives that aim to minimise sedentary behaviour and the associated risks.
A number of awards exist across the UK that are designed to recognise and encourage efforts made by organisations to improve health and well-being in the workplace. These include the North East Better Health at Work Award52 in England and the Healthy Working Lives award53 in Scotland. Although these awards have several categories for health promotion that can mitigate some of the negative outcomes of excessive sitting time, reducing sedentary behaviour as a specific outcome is not acknowledged.
Importance of this research
Current UK workplace legislation means that many members of staff in contact centres receive remedial ergonomic support as a mitigation measure to reduce existing musculoskeletal issues only after a chronic or musculoskeletal condition has been diagnosed. 54 However, current practices, compounded by workplace culture, inhibit initiatives that encourage contact centre staff to reduce sitting time. 55 Taking into account the lack of policies from authoritative bodies that are specific to sedentary behaviour, mean that it is important for workplaces to proactively develop their own organisational policies that include, and promote, opportunities for reducing occupational sitting time. 36 Given that contact centres are among the most sedentary workplaces,30 and that employees report higher levels of stress and depression than other desk-based work,56 it is key that preventative approaches are implemented in contact centres.
This work is currently needed to ensure that healthier working policies are distributed equitably across all workplaces, not just those that have more worker autonomy and better working conditions. Creating healthier contact centre environments may be more difficult than in other workplace settings, which is why such an intervention is necessary. In addition, building the capacity to develop and measure workplace-based interventions for health in contact centres is vital for developing a stronger business case to encourage and enhance organisational uptake and buy-in.
Overall research aims and objectives
Aim 1: to test the acceptability and feasibility of implementing the SUH intervention in contact centres.
The research questions for aim 1 were:
-
What is the acceptability, feasibility and utilisation of the various components of the intervention in a range of contact centres?
-
Does the programme theory and process of implementing the intervention work as intended?
-
Does the programme theory/intervention need to be adapted and if so, in what ways?
-
Are there differences in delivery of the intervention between different contact centres? If so, what are the reasons for these?
Aim 2: to assess the feasibility of using a cluster randomised controlled trial (RCT) study design.
The research questions for aim 2 were:
-
Is the study design (cluster RCT) feasible for a confirmatory trial of an intervention to reduce sedentary behaviour in staff working in contact centres?
-
How many clusters and participants per cluster are required for a confirmatory trial?
-
What is the recruitment rate of participants in each cluster and how many are lost to follow-up (e.g. owing to staff turnover)?
-
Are the range of study procedures (e.g. recruitment strategies and outcome measurement tools) feasible for a future confirmatory trial?
-
Are there differences in aspects of study procedures (e.g. uptake) between different contact centres? If so, what are the reasons for these?
-
What are the preliminary estimates of the variability of primary (reduction of sedentary behaviour in the workplace) and secondary outcomes within and between contact centres?
Aim 3: to scope the feasibility of a future health economic evaluation of SUH.
The research question for aim 3 was:
-
Is it feasible to provide estimates of the cost-efficiency of SUH from (1) an NHS and Personal Social Services (PSS) perspective and (2) an employer’s perspective?
Development of the Stand Up for Health programme theory
This study used a theory-based approach to evaluation. Programme theory is ‘an explicit theory or model of how an intervention, such as a project, a program, a strategy, an initiative, or a policy, contributes to a chain of intermediate results and finally to the intended or observed outcomes’. 57 Proponents of this approach argue that evaluation should not be driven by methods (as all have their strengths and weaknesses) but instead, that theories should be made explicit and the evaluation steps (and design) be built around them by elaborating on assumptions, revealing causal chains and engaging all concerned stakeholders. To develop the programme theory, we also had to consider the systems in which the SUH intervention was being implemented. The 6SQuID framework was used to develop the SUH intervention with members of staff at a contact centre using co-production methods supplemented by other data. The programme theory was developed through a comprehensive literature review and qualitative work in a pilot contact centre using the six steps in quality intervention development (6SQuID) framework. 58 The adoption of an intervention development framework is critical to understand and address the causal factors and to ensure that the programme is tailored to the needs of the centres. 6SQuID is an innovative and collaborative framework, which allows for the development of interventions that are acceptable and sustainable to the target population. It has, to date, been used to develop a range of interventions, including a family-based intervention to facilitate HIV (human immunodeficiency virus) testing,59 a kinship care intervention60 and an alcohol brief intervention in symptomatic breast clinics. 61 The framework consists of six steps:
-
step 1 – defining the problem
-
step 2 – identifying modifiable and non-modifiable causal factors
-
step 3 – defining the theory of change
-
step 4 – defining the theory of action
-
step 5 – testing and refining the intervention
-
step 6 – collecting evidence of effectiveness to justify evaluation and implementation.
In addition to these six steps, the 6SQuID process incorporates three key points to consider when following the framework. The first is to maintain stakeholder involvement throughout the entire process to encourage ownership of the problem and the solution. This is recognised as being crucial to developing acceptable and sustainable interventions. 58 The second key point is to acknowledge the system within which the intervention is being developed. All interventions take place within a system that operates in a certain way, which can impact on the success of the intervention. 58 In this study, the overarching system is the workplace, which has complex layers of written and unwritten rules and policies, fixed resources and often rigid cultures. Contact centres have particularly rigid policies, and failure to develop an intervention to take account of the systems will probably result in inadequate implementation, leading to failure of the intervention. The third key point is the consideration of the evaluation phase from the outset of development. The means by which an intervention will be evaluated should be considered during early phases of intervention development to ensure that the process and intended outcomes are measured accurately and robustly.
As an adaptive intervention, the fidelity of the SUH intervention is to the theories of change rather than being prescriptive about activities that catalyse change. 62 To ensure transferability, it takes into account the specific system (the contact centre, how it organises its work and how SUH will fit into the organisational and cultural systems) and context (e.g. layout of the centre, work-time flexibility, budget and resources available). In addition, it includes all employees from the start of development, with the aim of creating a social norm of standing more at work. By gaining insight from contact centre staff about their specific needs, this approach is more likely to lead to a sustainable and effective intervention. 58
6SQuID step 1: defining and understanding the problem and its causes
The first step of developing an intervention is to understand the problems and their causes. Step 1 creates the foundation for a successful intervention and involves fully understanding the problem that an intervention is trying to address and developing an understanding of the contributing factors to the problem. From the literature review and the stakeholder consultations (with the pilot centre, Ipsos MORI) we collectively defined the problem as the high level of sedentary behaviour (sitting time) during working hours in contact centres.
Through the literature review and focus groups with 34 participants, four themes emerged and were grouped into four levels by the researchers: individual, social/community, structural environment and organisational (Table 1). 62
| Level | Factors contributing to sedentary behaviour |
|---|---|
| Individual |
|
| Social |
|
| Environmental |
|
| Organisational |
|
6SQuID step 2: identifying which factors can be modified
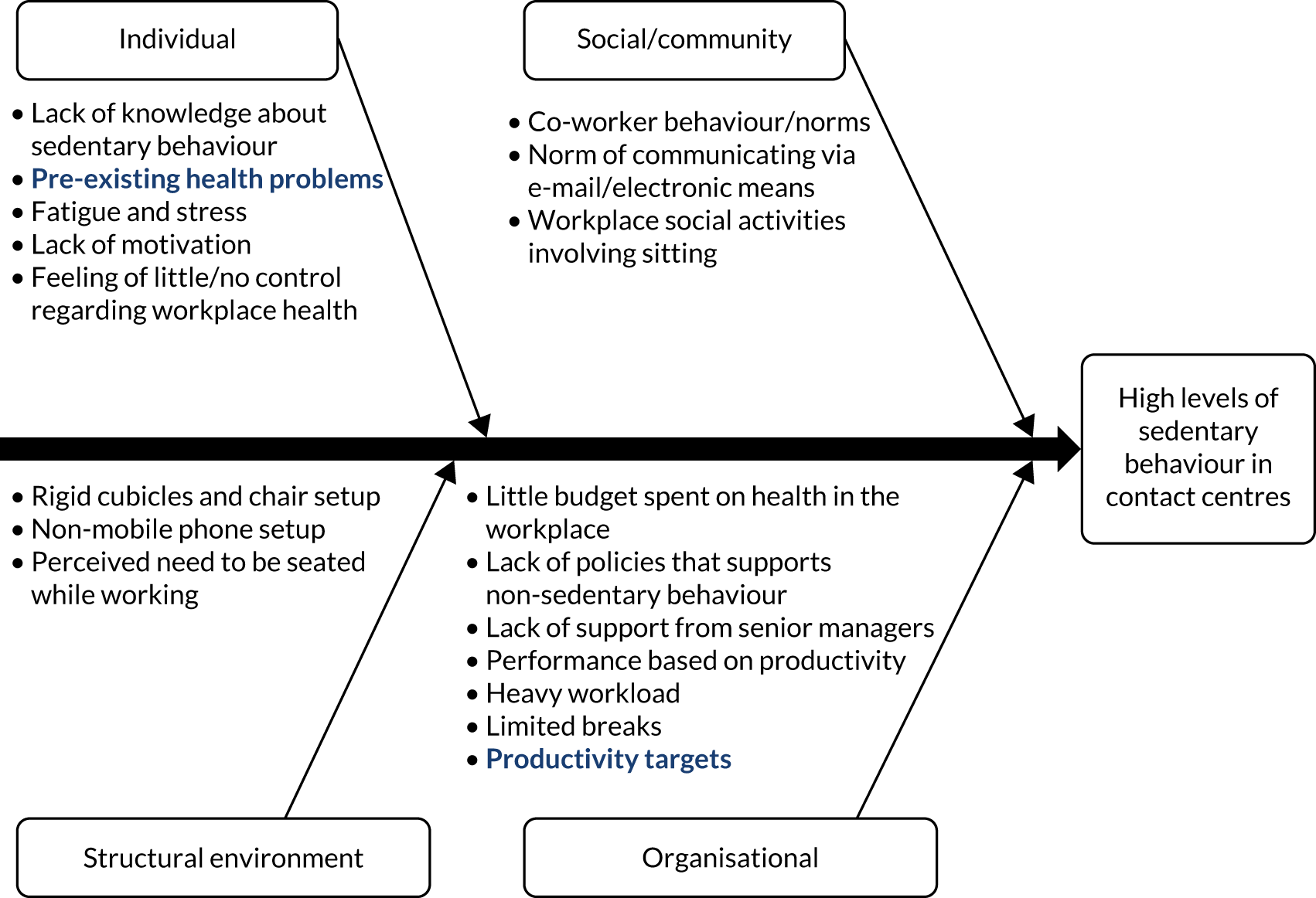
Modifiable factors with the greatest scope for change were considered to identify which specific factors should be targeted through intervention activities. These are described in the fishbone diagram (Figure 1).
FIGURE 1.
Fishbone diagram identifying the modifiable and non-modifiable factors. Black text, potentially modifiable factors; navy text, non-modifiable/hard-to-modify factors.
6SQuID step 3: deciding on the mechanisms of change (theory of change)
The intervention was based on two main theories: social cognitive theory63 and the social ecological model. 64 The intervention also aimed to create a sense of ownership to increase the likelihood of longer-term sustainability. 58 Although social cognitive theory addresses many personal determinants and socioenvironmental factors, the social ecological model takes the proposed multifaceted approach one step further to consider the intervention at not only the individual and interpersonal levels, but also the organisational, environmental and group levels, and takes into account the interactions between each of these. 65 By targeting multiple levels of the workplace, SUH aimed to foster an atmosphere that creates a social norm within the office community of sitting and standing within the workplace. The social ecological model justifies and predicts that SUH’s multifaceted approach will be effective, acceptable, feasible and sustainable. We also took a systems-based approach, by recognising that the implementation and sustainability of the intervention is dependent on how adaptive the contact centre system is to change.
Developing a theory of change involved developing intervention activities to target each modifiable factor leading to sedentary behaviour. This step details how each modifiable factor identified in step 2 could be addressed at each level of the contact centre by designing specific activities informed by the focus groups, literature review and workshop data. The literature review identified a number of systematic reviews of workplace interventions to increase physical activity and reduce sedentary behaviour. 17,24,39,40 Most recently, a systematic review of environmental interventions in workplaces (e.g. sit-to-stand desks)40 found evidence of significant reductions in sedentary behaviour in 14 out of 15 studies. This review found that multicomponent interventions that targeted more than one level of the socioecological framework were most effective. In 2016, another systematic review assessed the effectiveness of white-collar workplace interventions to reduce sedentary time. 41 It also found that multicomponent interventions had the greatest effect. Both reviews identified a need to assess whether policy-based measures or organisational changes could further increase effectiveness. SUH is designed to have organisational change as a key component of the intervention. A recent UK study funded by the NIHR PHR programme found that the SMArT Work intervention was effective in reducing sitting time of office workers within an NHS workforce using height-adjustable workstations, self-monitoring tools and behaviour change techniques. 46,66
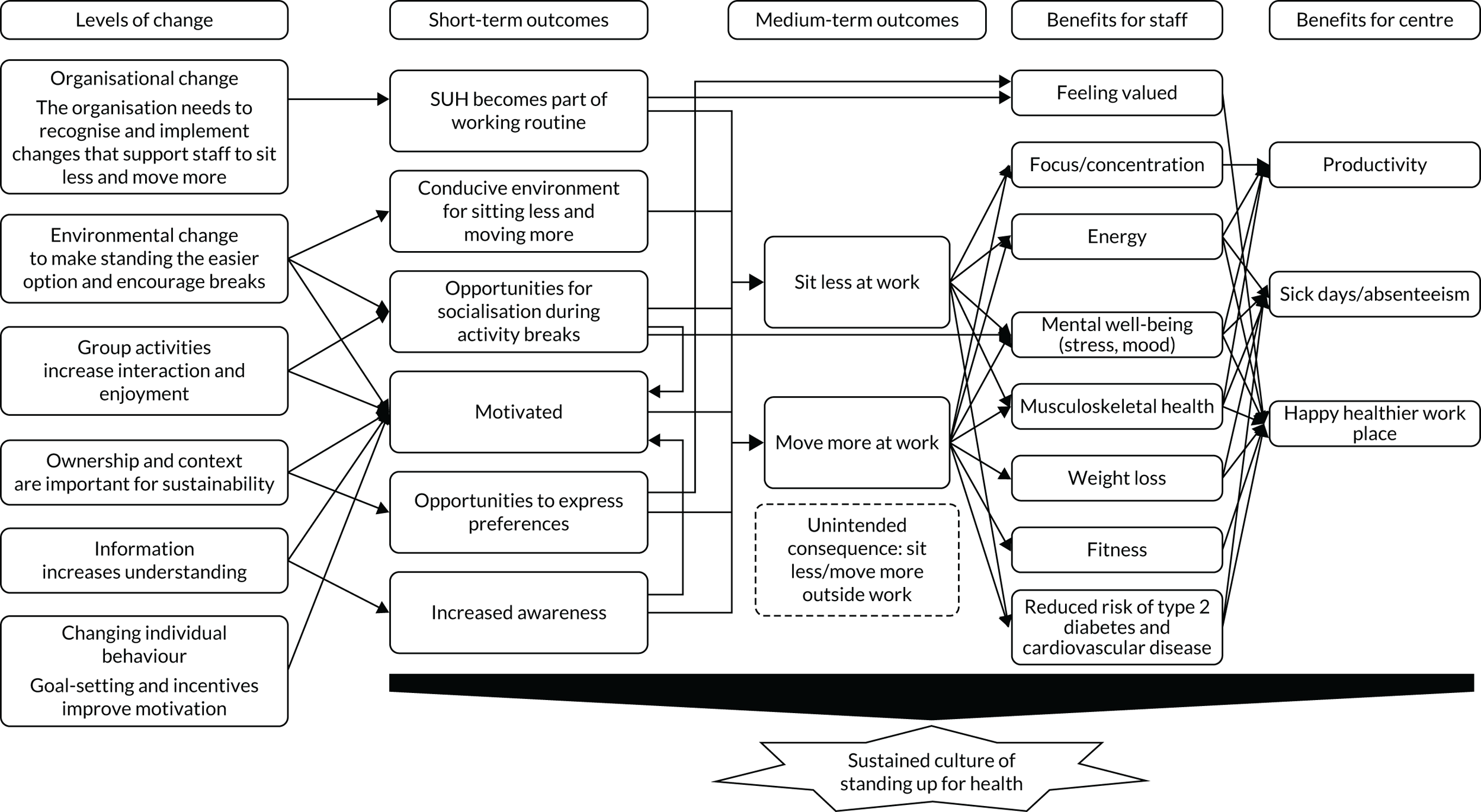
We found no reviews of interventions to reduce sedentary behaviour specifically in contact centres. The use of sit–stand desks and ergonomic awareness, as well as multicomponent workplace interventions, are effective in increasing physical activity and decreasing sedentary behaviour in contact centres. 42,51 The programme theory that we developed is outlined in Figure 2.
FIGURE 2.
The SUH programme: theory of change.
6SQuID step 4: clarifying how the mechanisms of change will be delivered (theory of action)
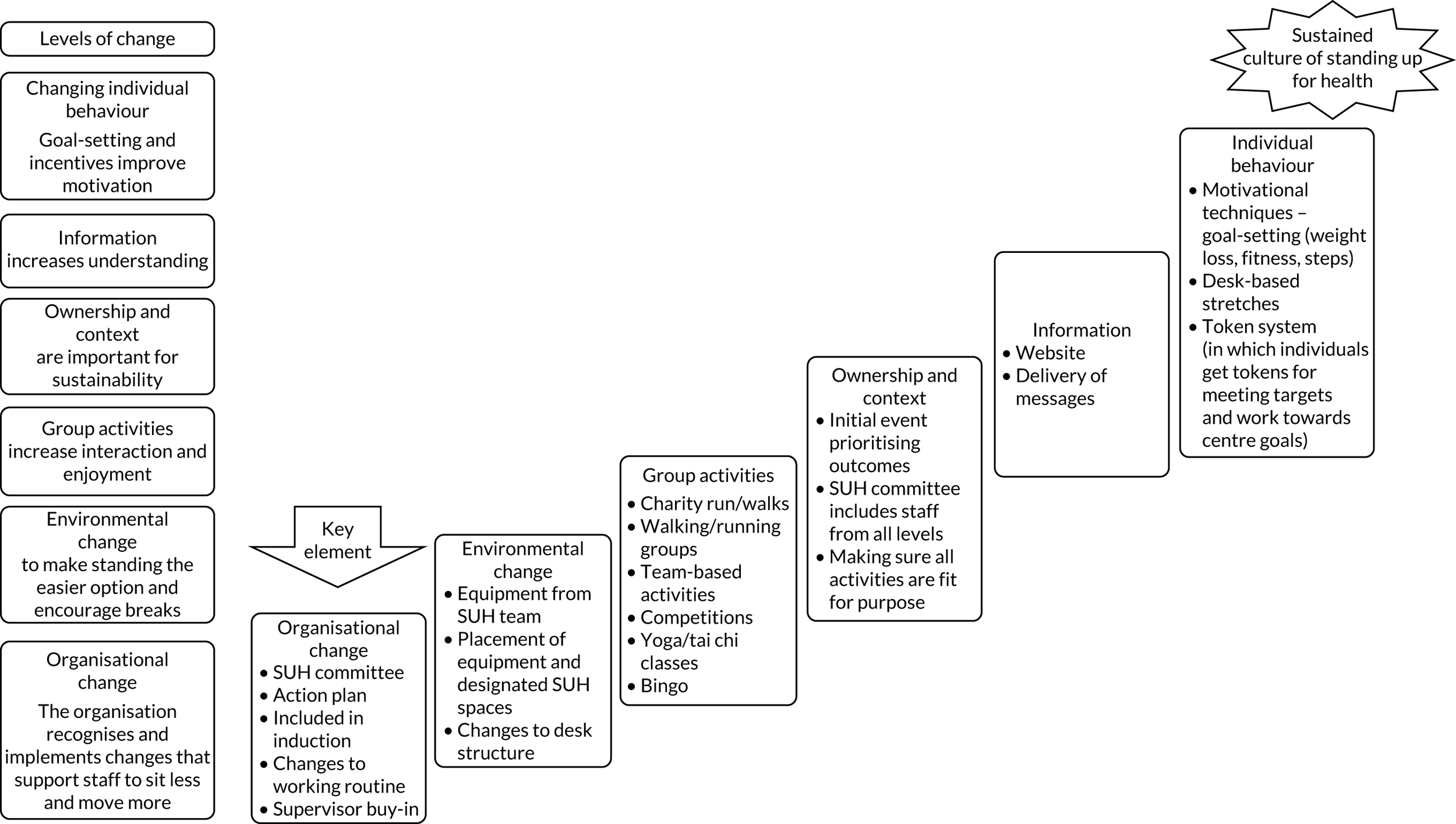
After defining the theories of change, the researchers identified the necessary resources available for implementation of the activities (Figure 3) and illustrated the programme theory in a logic model to demonstrate how intervention activities would lead to intended outcomes (Figure 4). Inputs and resources were identified through focus groups and informal discussions with management. During this phase, a workshop was held at the test contact centre to introduce staff to examples of intervention activities and equipment for the workplace. The workshop activities were developed based on feedback from staff in the focus groups. Staff were asked to contribute their own ideas and prioritise the ideas for intervention activities/workplace equipment that they wanted to try out. The research team fed back the results to the SUH implementation group; the SUH implementation group then decided on the final intervention activities to be implemented. There was at least one activity from each theory of change and the activity took account of the resources, assets (e.g. local spaces, existing equipment and spare spaces) and budget available. Once the specific intervention activities were chosen, the team worked with the contact centres to decide on an action plan for delivery and implementation of the activities (who, what, when and where).
FIGURE 3.
The SUH programme: resource assessment.
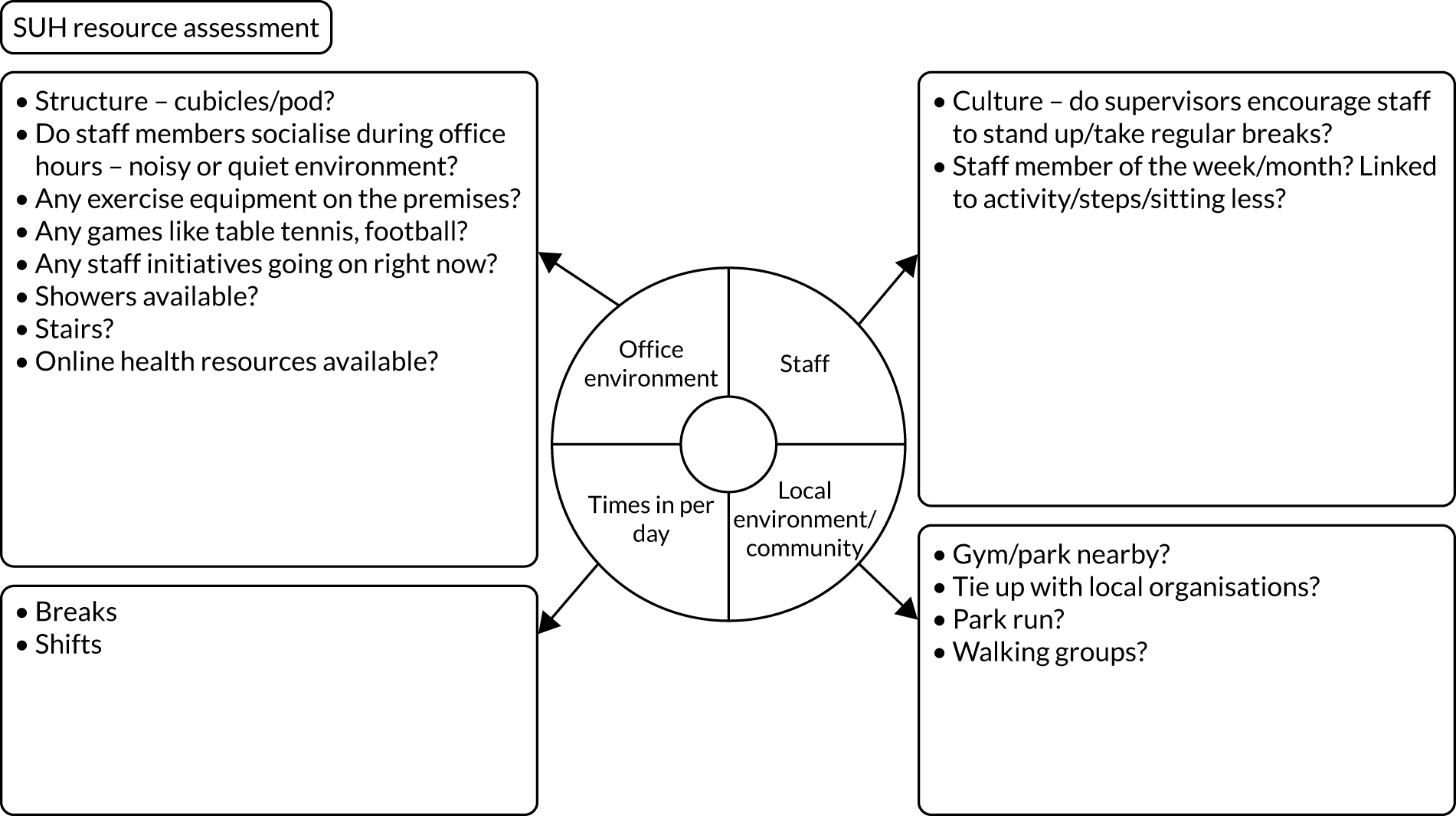
FIGURE 4.
The SUH programme: theory of action.
6SQuID step 5: testing and adapting the intervention
Contact centre staff in the pilot centre were assisted and guided by the researchers during two wellness committee meetings to establish and set goals for the programme. Continuous feedback was gathered from staff throughout the duration of the intervention so that the delivery of activities could be adapted as necessary. The intervention that was initially developed in Ipsos MORI continues to be implemented (although with a reduced emphasis owing to COVID-19) nearly 3 years after it started. The contact centre has reported that 25% of staff now use standing desks (an increase from almost none). There are a number of different activities going on at any one time and the call centre staff are constantly thinking of new activities to implement. The contact centre also asked to ‘bolt on’ a mental health component: the research team worked with them to implement mindful activities that either were standing up interventions (e.g. jigsaw puzzles on a stand-up desk) or encouraged them to leave their desk and be mindful [e.g. Lego® (Billund, Denmark) and knitting].
The final step of 6SQuID is to collect sufficient evidence of effectiveness to justify rigorous evaluation and implementation. This is the evaluation that is described in this report. However, as mentioned previously in Development of the Stand Up for Health programme theory, although the theory of change remains constant, an adaptive intervention needs to respond to contextual issues. Therefore, each centre was aided in developing a section of activities to meet its needs. Table 2 outlines which of the steps were undertaken prior to, and as part of, this study.
| Step | Pre-evaluation developmental steps | Steps undertaken in this study |
|---|---|---|
| Step 1: defining the problem | Yes | No |
| Step 2: identifying modifiable and non-modifiable causal factors | Yes | No |
| Step 3: defining the theory of change | Yes | No |
| Step 4: defining the theory of action | Yes, for the Ipsos MORI site | Yes, each centre developed its own theory of action |
| Step 5: testing and refining the intervention | Yes, for the Ipsos MORI site | Yes, some centres needed to test and refine some activities |
| Step 6: collecting evidence of effectiveness to justify evaluation and implementation | No | Yes |
Developing theories of action for the contact centres in this study
6SQUiD steps 4 and 5 formed the basis of the tailored intervention for each contact centre. The hypothesised theories of change (step 3) remain constant, but the theories of action are specific to each contact centre. The first step of the intervention included a ‘workshop’ that took place at a contact centre in which staff could test, suggest and vote for various activities that they wanted to try. The staff also described the environment, location, existing equipment and other assets that were then used to plan the activities. The SUH research team provided some small pieces of equipment for centres to try out before any investment was made. Although the number of activities was not limited, we worked with the contact centres to implement at least one activity from each theory of change (see Figure 2). These activities were used to create an action plan to be implemented over several weeks. A SUH committee, made up of all levels of contact centre staff, was created to support activity implementation. At the end of the intervention period, the researchers ran a second workshop to understand which activities had worked (step 4 of 6SQuID). Further prioritisation and choosing of future activities was then undertaken. All equipment and activities were risk assessed and details of how to use the equipment/undertake the activities were provided. A website was developed with useful resources, and opportunities for the contact centres to blog/share their experiences and create a community of SUH contact centres.
Developing the programme activities: pre lockdown
To enable the activities to fit within the systemic, cultural and environmental constraints of individual contact centres, we used the following methods to develop and implement activities for the SUH programmes during the pre-lockdown period.
Workshops to co-produce the list of activities to be delivered
The SUH team conducted two workshops as part of the programme. In the initial workshop, staff tried out various equipment and activities. The staff also participated in the prioritisation exercise, in which they used stickers to express their preferences for individual, social and environmental activities. The SUH team also lent several pieces of equipment (e.g. exercise bike, stepper, twisting disks, mini table tennis and mini golf) to the centres, keeping in mind environmental factors and staff preferences. In addition, an office wellness company (Sit–Stand.Com®; Coalville, UK) provided desk risers to centres at no cost. The SUH team had a discussion with centre stakeholders regarding the best style of desk riser for their contact centre, and the following were then shipped to the centres by Sit–Stand.Com:
-
centre 2 – Yo-Yo Desk Slim 80 cm (× 2) and Yo-Yo Desk Mini (× 1)
-
centre 3 – Yo-Yo Desk 90 cm (× 2) and Yo-Yo Desk 120 cm (× 2)
-
centre 7 – Yo-Yo Desk Slim 80 cm (× 3)
-
centre 9 – Yo-Yo Desk Slim 80 cm (× 2) and Yo-Yo Desk Mini (× 1)
-
centre 10 – Yo-Yo Desk Slim 80 cm (× 2) and Yo-Yo Mat Medium (× 2)
-
centre 11 – Yo-Yo Desk Slim 80 cm (× 2).
The SUH team worked with contact centre managers to understand context (e.g. centre layout, work-time flexibility and shift patterns) and resource availability (budget, space, online material, equipment and staff members with physical activity or other expertise). They used a resource assessment template to map out the assets and resources for the centre.
The team came back to the centre for workshop 2 after 3 months, at which they spoke to the staff about activities that had been implemented, likes and dislikes, and suggestions to ensure staff involvement and ownership.
Stand Up for Health committee
It was recommended that a SUH committee, consisting of staff members from teams across the participating centre, be set up. The committee was an important element of the programme and was responsible for procuring and generating ideas for activities from staff and aiding implementation of the intervention.
Action plan
After the initial workshop, the SUH team worked with the centre stakeholder to develop an action plan specific to the centre (for an example action plan, see Report Supplementary Material 1). The SUH team encouraged the adoption of at least one activity from each level of the theory of change (Table 3). A ‘SMART’ (specific, measurable, achievable, relevant and time-bound) approach was adopted to enhance success of implementation. The second workshop helped to refine the action plan.
| Theory of change | Example of activitiesa |
|---|---|
| Organisational | SUH implementation group (made up of all levels of staff; this is the only obligatory activity); management-led action plans; inclusion of non-sedentary behaviour as part of organisational strategies and goals; inclusion of non-sedentary behaviour activities for staff into roles and responsibilities (e.g. for supervisors); inclusion of ‘standing’ time into the working day |
| Environmental | Equipment: standing desks or a standing desk team area, bicycle desks, other equipment in communal places. Repurposing or changing the environment: standing communal areas with mindful/enjoyable activities, such as jigsaws or knitting, or a darts board; moving printers further away; exercise spaces; boards on walls to draw on |
| Social/cultural | Group activities in work time, such as 5 minutes of stretching per hour; group goal-setting; exercise classes before or after shifts; competitions between workspaces or teams; workplace challenges; rewards for standing more/being more physically active; educational prompts |
| Individual behaviour | Individual goal-setting, active travel to and from work, lunchtime walks; apps; links to local groups and activities |
Duration of the intervention
The duration of the intervention was defined as the period that the centres took to develop their preferred activities for each theory of change, prepare an action plan for sustained engagement and test out some of the activities. This process took around 3 months but was dependent on the contact centres and COVID-19.
Scalability and translation
This intervention is designed to be scalable and transferable into other contact centre settings in the UK and internationally. It is also transferable to other workplace settings. The reason why we have not specified activities (or fidelity to particular activities) is to allow for flexibility, scalability and transferability to different contexts. We recognise that some contact centres will have more resources and assets than others, which is why we have suggested a range of activities that can all activate the theory of change. Given that the theories of change are the most adaptive aspects of the intervention, the intervention is adaptive to all contact centres, and it is designed so that contact centres can implement it at little or no cost.
Protocol amendments in the context of COVID-19
Study aims and research questions
All of the original aims remained the same (see Overall research aims and objectives), but we added an additional aim: aim 4 – consider previous aims under the context of COVID-19.
All of the research questions also remained the same, but we included some additional ones to take account of the impact of COVID-19.
The research questions for aim 1 were:
-
Can SUH be adapted for those working remotely?
-
What is the acceptability and feasibility of this mode of delivery?
The research questions for aim 2 were:
-
Is it feasible to adopt an online format and does this affect the use of a stepped-wedge study design?
-
Does the mode of delivery impact on the feasibility of the study design (online vs. face-to-face delivery)?
Impact of COVID-19: changes to data collection
All scheduled workshops and data collection until January 2020 were completed as planned. The research team did not make any in-person visits after this time. The SUH team had planned 13 additional visits from March 2020 to June 2020, all of which were cancelled. The team shifted to remote collection of data, including interviews, focus groups and questionnaires.
It is important to note that the normal routine in centres was disrupted and, hence, any follow-up data collected may have been biased. Outcomes such as mental health, work engagement and sitting behaviour are likely to have been influenced by the COVID-19 pandemic and may not accurately capture intervention effects. Given this, we still administered the questionnaire when it was easy to do so and endeavoured not to increase burden for centres.
Posting activPAL™ devices (PAL Technologies Ltd, Glasgow, UK) to the centres was considered as an option. However, this was not feasible because researchers needed to be present to explain attachment and filling of logbooks. There would also be high risk of loss of the devices.
Impact of COVID-19: changes to intervention activities and delivery
From workshops to personalised activity plans
We were not able to go to the centres during lockdown to conduct the workshops. Instead, we conducted one-on-one virtual consults with up to 30 staff per centre to capture the varied working arrangements and unique barriers. We spent approximately 20 minutes with each staff member and asked specific questions about barriers to and facilitators of sedentary behaviour and physical activity at the various levels (environmental, social and individual). We reviewed the information and got back to them individually with tailored recommendations for their specific situation. We developed a personalised activity plan with recommendations and resources for each staff member. We then pulled all of the recommendations and resources generated from the consults and created a document(s), which was shared with all staff members at the centre.
Social activities
The SUH team organised a step count challenge to encourage staff to sit less, move more and generate social interaction. The challenge was conducted over 6 weeks, and staff made a virtual trip from Land’s End to John O’Groats. Staff formed teams of five and submitted the weekly steps for their team on the SUH website.
Equipment
The SUH team sent some pieces of equipment (e.g. balance board, balance ball chair, mini table tennis and twisting discs) to centre 7 for the benefit of staff who were working onsite.
Chapter 2 Methods
Study design
This was a feasibility study with a cluster RCT design (to address aim 2), combined with a process evaluation (to address aim 1) and an economic component (to address aim 3). Given that the intervention was implemented in a workplace, it was not possible to randomise at the individual level; therefore, a cluster RCT was the only option. We explored the relative advantages and disadvantages of the stepped-wedge and the cluster parallel-group designs as the two most appropriate options. After much discussion, we decided on a staircase stepped-wedge trial design (Figure 5). Full details of the methods and rationale for the design are provided in the paper published by our team. 67
FIGURE 5.
The SUH programme cluster trial design: planned and actual. B, baseline data collection; 3F, 3-month follow-up; 6F, 6-month follow-up; Q, qualitative data collection; W, workshop.
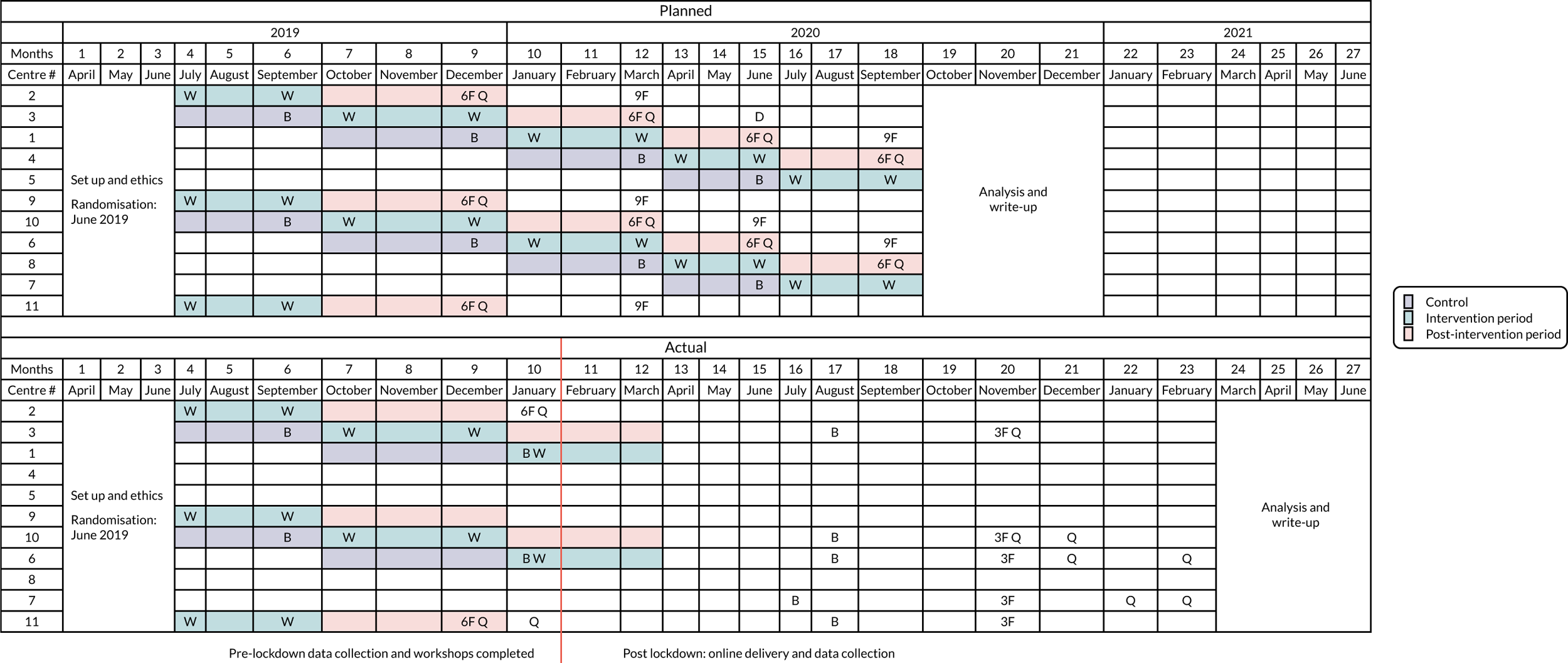
Our study design is unusual because it is not a standard stepped-wedge design (it has lots of incomplete sections), but it is also not a standard waiting list control design because there are many cross-sectional comparisons, which may not always be present in a waiting list control design. Similar designs are increasingly being used in evaluation research and involve random and sequential crossover of clusters from control to intervention until all clusters are exposed. 68 It can be considered as an extension of the parallel-cluster trial with a baseline period. Such a design makes it possible to achieve a phased introduction of the intervention. It combines pragmatism with a robust design, and the way that the study is conducted has much in common with the parallel-cluster trial. Such designs are likely to be appropriate (1) when evaluating an intervention that will be implemented irrespective of evidence for effectiveness and (2) when it will be logistically implausible to roll out the intervention simultaneously to all clusters. 69 This is an important consideration, given the significant cost of loaning equipment to a large number of individuals; we also would not be able to collect activPAL data on half of the anticipated sample at one time point. This design allows us to have a smaller number of individuals at each baseline assessment point, in turn meaning that a smaller number of activPAL devices, equipment and other resources would be required.
Although there continues to be debate over the design and its limitations (e.g. Kotz et al. 70), some of which are valid, evaluations of public health interventions often have to be pragmatic and consider the stakeholders and context of the intervention involved (in this instance, the contact centres). We argue that we need a pragmatic option for a number of reasons. First, it could potentially cause delays in the evaluation process if we waited until all contact centres were at the same stage of readiness for implementation. A structural/location/organisation change in one contact centre could delay the process. Second, it would be more costly and resource intensive to implement the intervention and collect baseline data in all the contact centres at a single time point. We have hired two researchers, but the spread of locations in Scotland and the North East of England would make implementation and data collection difficult and increase the potential for failure. Last, we have observed that contact centres want to implement the intervention when they hear about it and it is unlikely to cause any harm. It has been implemented in one contact centre for over 1 year and only positive benefits have been reported. Journals, such as Trials71 and Lancet Global Health,72 are publishing the results of such designs.
Setting
The trial took place in contact (or call) centres run by the public sector (e.g. the NHS), private sector (e.g. banks or businesses) or third sector organisations (charities and not-for-profit organisations).
Study population
Given that this was a cluster RCT, contact centres rather than the staff employed in the contact centres (e.g. managers, supervisors and call handlers) were recruited. All staff in those contact centres had the opportunity to participate in the intervention. For the evaluation components, staff had the option of taking part on an opt-in basis.
Recruitment
Our original aim was to recruit 10 contact centres with more than 100 employees in Scotland and/or the North East of England. The target was to recruit 10 contact centres by month 3 of the project. A total of 11 contact centres were recruited by this time, two of which had under 100 employees (72 and 33 employees, respectively). We decided to include these two smaller centres in the place of one larger centre because both were very enthusiastic and we wanted to start randomisation as soon as possible.
All staff who had been working in the contact centres were invited (via e-mail through their contact centre, posters within the centre and in-person visits to the centre by the SUH research team) to be involved in the evaluation of the intervention. Staff who were interested in participating were sent an information sheet and consent form. It was made clear that participation or non-participation would not affect terms of their employment.
Retention
The average annual turnover (attrition) of contact centre staff is around 24%, compared with 15% in other industries. This high rate of attrition has implications for the retention and follow-up of participants. The high turnover is partly because of contact centres employing a large number of students and people looking for short-term work. Although this is a problem for the evaluation, it may be conducive to the overall success of the intervention, which has the potential to impact on a range of people, enabling them to engage with health-promoting activities that may encourage the development of lifelong habits. One of the aims of this study was to determine the retention rates for a future study. We intended to use a number of strategies to increase retention into the evaluation (as opposed to the intervention):
-
Staff were incentivised (with a £5–10 gift voucher) to complete baseline and outcome data assessments.
-
If staff left the contact centre, we would explore what methods were possible for follow-up (e.g. post, e-mail and telephone) and evaluate the most effective method.
-
We were to record data on the length of time employed in the contact centres. These data would help us determine whether or not turnover is higher at the beginning of the employment period (which could impact on retention rates).
Randomisation
Randomisation occurred in month 3 of the study. The unit of randomisation was contact centres. A computer-generated block randomisation algorithm was used to randomly allocate each contact centre to start the intervention at one of five time points, 3 months apart. Randomisation of contact centres to sequences was conducted in May 2019, using stratification by centre size (≤ 500 vs. > 500 employees). Stratification by centre size ensured that the combined centre size was approximately balanced across time points. Randomisation in this way allowed us to introduce the intervention to each site in an unbiased way, unrelated to time or the particular circumstances of each site. It also aimed to ensure that there was approximate balance, on average, across all of the intervention start times in terms of participant or contact centre characteristics. Allocation concealment and centres were not informed of exactly when they were to start the intervention until close to the intervention visit, was used as far as possible.
A complete list of the contact centres that agreed to take part in the study was compiled by Divya Sivaramakrishnan and Jillian Manner. The contact centres were numbered 1 to 11, in fixed order, and this list was signed and dated by Divya Sivaramakrishnan and Jillian Manner. Randomisation was then conducted in May 2019 by Richard Parker, who was fully blinded to the names of the contact centres and who generated a list of centre numbers showing the sequences that each centre should be allocated to (see Figure 5).
Control/comparator group
All sites received no intervention for between 3 and 12 months after the start of the study, as a waiting list control. Sites then received the intervention in accordance with the schedule set out in Figure 5.
Steps to minimise bias
Allocation
Allocation to trial groups was carried out by the statistician after recruitment, who was blind to the contact centre identity.
Contamination
Although it is possible that staff may move between contact centres allocated to different trial groups, we anticipated that this would have little impact. We did, however, attempt to evaluate the extent to which this occurs. To our knowledge, this did not occur during the study.
Sampling and sample size
We anticipated that all employees at a site were likely to take part in some or all of the intervention activities. However, employees also had the option of taking part in the research evaluation component. The sample size refers to the number of people taking part in the research evaluation (not those taking part in intervention activities). The sample size and target difference are the same as another similar study73 that proposed a sample size of 160 participants per group to detect a reduction in workplace sedentary behaviour of 45 minutes per day. Given that we aimed to have six control and post-intervention cross-sectional comparisons (see Figure 5), the target sample size was 160/6, which equals ≈ 27 participants per contact centre per data collection period. We anticipated that 10 contact centres would be recruited, so we aimed to recruit at least 270 employees to take part in the research evaluation. An aim of this feasibility study was to test sample size assumptions and produce a more accurate sample size calculation for a future study. We also aimed to recruit 6–8 individuals per contact centre for the qualitative data collection (60–80 individuals in total).
Ethics/regulatory approvals
The study was conducted in line with Medical Research Council and the Economic and Social Research Council ethics framework. Ethics approval was obtained from the School of Health in Social Sciences ethics committee, University of Edinburgh (ref STAFF142).
Informed consent
Although the employees did not have to provide informed consent to take part in the intervention activities, they had to provide informed consent to take part in the research evaluation (both the quantitative and the qualitative components). We provided them with information sheets and consent forms. It was made clear that participation or non-participation in the research would not affect employees’ work contracts or roles.
Confidentiality, anonymisation and data storage
Questionnaire data were collected anonymously using numerical identification codes in a locked cabinet or stored electronically on Qualtrics (Qualtrics International Inc., London, UK). Interviews and focus groups were recorded using encrypted digital devices, or recorded using Zoom (Zoom Video Communications, San Jose, CA, USA) or Microsoft Teams (Microsoft Corporation, Redmond, WA, USA). Audio and video files were sent to an authorised transcription service using a secure file transfer link, transcribed and then anonymised by the study team. All data were stored on password-protected university-networked computers. A separate database of participant names and unique identification numbers was stored securely and in a separate location to the study data. In reporting the results of the qualitative data and process evaluation, care was taken to avoid the identification of participants through quotations.
The specific methods for each aim of the study and the results are presented in the subsequent chapters.
Data management and research governance
The project was sponsored by the University of Edinburgh, Edinburgh, and was funded by the NIHR. The trial was registered as ISRCTN11580369. Ruth Jepson (principal investigator) was responsible for ensuring that the study was carried out with strict adherence to the principles of good governance. We established a Study Steering Committee, which met once face to face and fed back via e-mail during the pandemic. The Study Steering Committee comprised researchers, experts on workplace health and staff (at different levels) from contact centres.
Patient and public involvement
Public involvement (in this case, contact centre staff) is at the heart of this intervention. Contact centre staff at all levels were encouraged to work with us to develop activities that worked for them, and they were encouraged to take ownership of both the problem and the solution. We have successfully tested the intervention in a single contact centre; staff from that contact centre were on the Study Steering Committee and also worked with us to develop content for the study’s website and social media accounts.
Chapter 3 Process evaluation: methods and results
Background
Stand Up for Health is a multicentre feasibility study. The study employs a cluster-randomised stepped-wedge design, and aims to assess the feasibility of intervention delivery and data collection methods, as well as procure preliminary estimates of effectiveness. The primary outcome was the activPAL device-measured sedentary time in the workplace, measured over 7 continuous days. This will subsequently be referred to as the primary outcome for the remainder of this report. 67 Secondary measures include subjective measures of workplace sedentary time, total sedentary time, physical activity, mental well-being, work engagement and musculoskeletal health. This component is referred to as the feasibility outcome evaluation study in this report.
Randomised controlled trials have traditionally focused on outcome evaluation, and the underlying processes and reasons why the intervention was or was not effective are not always properly understood. 74 To address these aspects, a process evaluation was carried out. Process evaluation refers to activities relating to intervention implementation, acceptance and reach. 75 It aims to understand the influence of contextual factors, explain discrepancies between expected and observed outcomes, and clarify causal mechanisms. 76 Within this study, the process evaluation sought to gather views and experiences of the SUH intervention activities and implementation processes with a view to refining the theories of change and overall programme theory. It examined whether or not the SUH activities worked as intended, the reasons why they did or did not work, and assessed any unintended consequences of the intervention. The process evaluation also aimed to provide insight into the feasibility of the study design and procedures.
Objectives
The process evaluation aimed to:
-
gather views and experiences of the SUH intervention activities and implementation processes
-
understand whether or not SUH activities worked as intended and investigate any unintended consequences of the intervention
-
explore differences in delivery of the intervention, differences between different contact centres and the reasons for these differences
-
assess the feasibility of the range of study procedures (e.g. recruitment strategies and outcome measurement tools) and understand differences between centres.
Methods
The process evaluation predominantly utilised qualitative methods substantiated with quantitative indicators from data collected over the course of the study. The overall SUH study had three aims, and the process evaluation addressed the first two aims:
-
acceptability and feasibility of the SUH intervention
-
feasibility of study design and procedures.
Acceptability and feasibility of the Stand Up for Health intervention
RE-AIM framework
RE-AIM (reach, effectiveness, adoption, implementation, maintenance) was the main framework adopted for the process evaluation to assess acceptability and feasibility of the SUH intervention. RE-AIM was developed to include reach and representativeness of participants and settings within the evaluation framework, with a focus on external validity. 77,78 The framework aims to improve assessment and reporting on five dimensions:77–79
-
Reach – the proportion of the target population that participated in the intervention. This is also defined as the reach (absolute number/proportion) and representativeness of individuals willing to participate in the intervention.
-
Effectiveness – success rate if implemented as in guidelines, defined as positive outcomes minus negative outcomes.
-
Adoption – proportion of settings, practices and plans that will adopt the intervention. This is the extent to which those targeted to deliver the intervention are participating, and can be measured as the percentage of providers participating in the programme.
-
Implementation – extent to which the intervention is implemented as intended in the real world. This also includes agents’ fidelity to the various elements of the protocol and the time and cost of the intervention.
-
Maintenance – extent to which a programme is sustained over time.
The RE-AIM dimensions were adapted for this process evaluation so that they were meaningful and captured essential and beneficial information. The reach dimension explored whether or not the intervention was available to everyone within each contact centre and if there were sectors of the organisation that did not have the opportunity to participate. The appeal and acceptance of the programme was also captured under the reach section. The effectiveness element included a qualitative exploration of the perceived benefits and consequences of the programme among staff and stakeholders. Given that this was a feasibility study, adoption (the percentage of contact centres that participated in the SUH programme) has limited relevance. Here, the proportion of centres that participated out of those that were targeted was assessed. The implementation element examined the activities implemented by the contact centres. Plans to continue implementation of the intervention were included within the maintenance element. The RE-AIM elements were explored mainly through qualitative methods. In addition, activity preferences among staff were captured using questionnaires, and these data were analysed and presented under the reach section to further understand programme appeal. The adoption element included a quantitative indicator showing the number of centres that participated compared with those that were recruited.
Programme theory and theory of change
The SUH intervention is an adaptive programme that does not prescribe specific activities to allow for flexibility, scalability and transferability. Programme implementation could vary between centres, with each choosing different activities within the organisational, environmental, social and individual levels. Hence, this process evaluation did not aim to assess fidelity to specific activities or consistency of delivery across sites. 79 Instead, it focused on whether or not the theories of change operated as intended. The process evaluation aimed to verify the programme’s theory of change and refine and adapt the change processes if required. This aspect is considered to be part of the implementation section of RE-AIM in this report. Organisational, environmental, social and individual factors were explored during the focus groups and interviews. We also aimed to discern underlying processes, such as increased motivation, ownership and increased awareness, as well as unintended consequences (both positive and negative).
Feasibility of using study design and procedures
The feasibility of using a cluster-randomised controlled design was evaluated using qualitative methods along with quantitative indicators. This component of the process evaluation is not considered under the RE-AIM framework. The range of study procedures evaluated, and methods of analyses, were as follows:
-
Recruitment and randomisation of contact centres and dropout– researchers’ reflections on completion of recruitment and randomisation of contact centres, including quantitative indicators on actual, compared with planned, recruitment and randomisation figures. Reasons for centre dropouts were explored using data from exit questionnaires completed by two centres.
-
Recruitment of participants and dropout – (1) quantitative indicators on actual, compared with planned, recruitment numbers and data on dropouts; (2) qualitative data on recruitment procedures through focus groups and interviews with staff and stakeholders; and (3) statistical analysis of reasons for participant dropout.
-
Data collection procedures and tools – assessed using qualitative data through focus groups and interviews with staff and stakeholders. Data from activPAL logbooks pertaining to detachment of the activPAL device and reasons for detachment are presented in this report, along with data on the number of activPAL devices issued and returned, and questionnaires completed.
A summary of the framework and measurement for the process evaluation is presented in Table 4.
| Dimension | Elements | Measurement |
|---|---|---|
| Acceptability and feasibility of the SUH intervention | ||
| Pre lockdown | ||
| Reach |
|
|
| Effectiveness | Perceived benefits |
|
| Adoption |
|
|
| Implementation |
|
|
| Post lockdown | ||
| Reach |
|
|
| Effectiveness |
|
|
| Implementation |
|
|
| Maintenance |
|
|
| Feasibility of study design and procedures | ||
| Pre lockdown | ||
| Recruitment and randomisation of contact centres |
|
|
| Participant recruitment and dropout |
|
|
| Data collection procedures |
|
|
| Post lockdown | ||
| Participant recruitment and dropout |
|
|
| Data collection procedures |
|
|
Formats and time points for qualitative component
Focus groups and interviews were conducted with staff members from five centres. In addition, one individual interview was conducted with key stakeholders (primary centre co-ordinator) from six centres. The focus groups and interviews were scheduled to be conducted approximately 6 months after the start of the intervention. We were able to conduct the focus groups and interviews for centres 2 and 11 as per this schedule. However, owing to the COVID-19 pandemic, we conducted the qualitative sessions for centres 3, 6, 7 and 10 approximately 3 months after the delivery of the post-lockdown intervention (see Figure 5).
Face-to-face focus groups were conducted with staff and telephone interviews were conducted with stakeholders from centres 2 and 11. Virtual focus groups and interviews were conducted using Microsoft Teams with staff and stakeholders from centres 3, 6, 7 and 11.
Participants and recruitment for qualitative component
Ethics approval for the qualitative component was procured from the School of Health in Social Sciences Ethics Committee (University of Edinburgh). Convenience sampling was used to recruit staff members for the focus groups and interviews. Stakeholders organised the session for face-to-face focus groups in centres 2 and 11, and arranged for staff to be off the telephones and attend the group discussion. Information sheets were circulated in advance and provided on the day (see Report Supplementary Material 2). Staff then provided written consent before participating (see Report Supplementary Material 3).
For the virtual focus group in centre 11, the SUH team co-ordinated with the stakeholder who organised the session at a convenient date and time. It was difficult to organise a virtual focus group in centres 6 and 7. In centre 6, the SUH team used Doodle poll (Doodle AG, Zurich, Switzerland; www.doodle.com) to set up interviews with staff. In centre 7, the SUH team procured the names of available and interested staff and co-ordinated with them to arrange interviews. Staff were sent an online information sheet and consent form (on Qualtrics) in advance of the session and provided electronic consent before participating.
The SUH team co-ordinated with centre stakeholders to find a suitable date and time to conduct the interview sessions. The information sheet and consent forms were sent to stakeholders from centres 2 and 6 before the call, and participants provided consent and returned the forms before the interviews. Stakeholders from centres 3, 6, 7 and 10 were sent an online information sheet and consent form prior to interviews, and provided electronic consent before the session.
Instrumentation for qualitative component
Topic guides for the focus group discussions and interviews were developed by Divya Sivaramakrishnan, Jillian Manner, Graham Baker and Ruth Jepson, based on the process evaluation framework, and covered topics relating to (1) the acceptability and feasibility of the SUH intervention, and (2) the feasibility of using the study design and procedures. These were then reviewed by the other SUH team members and further refined based on their comments. The topic guides for the post-lockdown focus groups and interviews were developed through amendment of the pre-lockdown guides. The post-lockdown guides included questions pertaining to post-lockdown activities (consults, activity plan and step count challenge). Topic guides are presented as supplementary material (see Report Supplementary Material 4).
Qualitative analysis
All focus group discussions had a moderator and co-moderator. The face-to-face focus groups and telephone interviews were recorded using an audio-recorder. The online sessions were recorded using the record function on Microsoft Teams. Data were transcribed verbatim by a transcription agency.
An initial coding framework was developed by Divya Sivaramakrishnan, Jillian Manner and Graham Baker based on the RE-AIM process evaluation framework (see Table 4). Five transcripts were coded by both Divya Sivaramakrishnan and Jillian Manner (two pre-lockdown staff focus groups, two pre-lockdown stakeholder interviews and one post-lockdown staff interview). The other transcripts were coded by one researcher (DS/JM). Graham Baker and Richard Parker acted as critical friends, who discussed the themes and subthemes with Divya Sivaramakrishnan and Jillian Manner; clarified and offered interpretation; and provided insights and suggestions to refine the themes. Transcripts were coded deductively based on the coding framework, with a deductive approach to capture themes within the broad framework. Thematic analysis was used to generate themes and subthemes following a six-step process. 80 Differences between centres within each theme were examined during analysis. A computer software package (NVivo version 11; QSR International, Warrington, UK) was used to code the transcripts and manage the thematic structure.
Other sources of data
activPAL experience
In addition to data from focus groups and interviews on experiences with the activPAL device, data from activPAL logbooks are also presented in this chapter. All staff that wore the activPAL device were requested to complete logbooks to capture work and sleep times. One section of the logbooks captured data on whether or not the activPAL device was detached and the reason for detachment, and whether or not it was reattached. These responses were summarised and converted to percentages. An open-ended question captured additional comments and issues relating to wearing the activPAL device. Responses to this section were analysed along with the qualitative data.
Activity preferences
As a part of the outcome analysis, staff completed a questionnaire relating to the outcome measures. The pre-lockdown questionnaire asked staff how often (number of days per week, ranging from ‘did not participate’ to ‘participated daily’) they had participated in five activities over the last 6 months (use of desk-based equipment, use of non-desk-based equipment, mindfulness activities, group activities and individual activities). The post-lockdown questionnaire asked participants if they participated (yes, no, not sure) in nine activities (step count challenge, virtual social activities with an active component, goal-setting, desktop stretches, exercise videos and apps, mindfulness activities, other individual activities, using the SUH website, environmental changes). The activity preferences of staff members were captured within the post-intervention questionnaire (see Report Supplementary Material 5 for the pre-lockdown questionnaire and Report Supplementary Material 6 for the post-lockdown questionnaire). Responses were summarised using Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) and presented as percentages.
Exit questionnaires
Two centres that dropped out (centres 5 and 8) completed an exit questionnaire. The questionnaire was designed by Divya Sivaramakrishnan and Jillian Manner, who also summarised and discussed the responses to the questionnaire. The responses were reported as a part of the section on recruitment and randomisation of centres.
Researcher’s reflections
Throughout the recruitment and data collection process, Divya Sivaramakrishnan and Jillian Manner regularly discussed concerns and issues and aspects of the process that were (or were not) working. These were noted in a shared Microsoft Word document (Microsoft Corporation, Redmond, WA, USA) and the reflections were used as a part of the qualitative analysis to substantiate themes and provide additional, deeper insights.
Participant dropout
The SUH team considered individuals who participated in pre-lockdown data collection, but not post-lockdown data collection, as well as those who provided baseline measurements but not follow-up measurements (3 months later) in the post-lockdown phase. We also asked stakeholders the reasons for participant dropout (e.g. left the company, moved to a different part of the company, were unavailable, did not want to participate, technological barriers, did not receive communication, I don’t know, other – elaborate). Centres 3, 6, 10 and 11 were included in the pre-lockdown analysis and the following binary variables were considered: left company, moved job and lost to follow-up. A multiple logistic regression model was fitted to each of the three binary outcomes. The multiple logistic regression model had the following explanatory variables (all entering the model as fixed effects): contact centre, sex, part-time working, age and how long the participant had worked for the contact centre. Centres 3, 6, 7, 10 and 11 were included in the post-lockdown analysis. A multiple logistic regression model was fitted to the ‘lost to follow-up’ variable, adjusting for contact centre, sex, part-time working, age and how long the participant had worked for the contact centre.
Reporting
The process evaluation framework (see Table 4) was used for reporting and the results are organised under two main sections: (1) acceptability and feasibility of the SUH intervention and (2) feasibility of the study design and procedures. Within these two sections, pre- and post-lockdown results are examined separately.
Results
Centre characteristics
Contact centre locations were London, Durham, Tyneside (Newcastle-upon-Tyne, Gateshead, South Shields and Jarrow), Sunderland and Edinburgh. The number of staff members in the centres ranged from 33 to 2000, with an average of 559 staff members.
Participant characteristics
In total, 33 staff and stakeholders from six centres participated in the process evaluation focus groups and interviews. Specifically, four focus groups (centre 2: eight participants; centre 6: two participants; centre 10: six participants; centre 11: six participants) and three interviews (centre 7: two interviews; centre 6: one interview) were conducted with staff members. Interviews were conducted with stakeholders from all six centres (eight participants).
Acceptability and feasibility of the Stand Up for Health intervention: pre-lockdown results
Reach: programme significance and appeal
The majority of staff described participating in the pre-lockdown SUH intervention as a positive experience overall. The intervention was well received and was enjoyable for individuals and teams:
I honestly think it was a really positive experience. I think, for some people, it made a difference. It really kind of . . . it changed the way they worked . . . as an employer, giving our staff the opportunity to work differently, is fantastically positive. You can’t force people to do it, but the fact that we’re able to give them the opportunity to work differently, to move around and, you know, to look after themselves and keep well, while they’re working, I think, is fantastic. I think it’s just been brilliant.
Centre 10, stakeholder
Staff and stakeholders emphasised the importance of the SUH programme for contact centres to improve physical, mental, emotional and social well-being. It was felt that SUH was a particularly significant and unique programme because it brought attention to the lack of movement in the sedentary contact centre environment, and encouraged movement in this environment. Stakeholders reported that the SUH programme helped them look after their staff better. Staff associated SUH with health in the workplace and regarded it as a means of improving their mental and physical health and well-being (specifically, musculoskeletal issues and mental health). Staff felt that SUH helped them to manage stress and cope with stressful calls. Encouraging teamwork and uplifting team spirt was another aspect of SUH that was valued by staff and stakeholders.
Stand Up for Health led some staff to think about their general health and well-being, as a first step to making lifestyle changes. Several centres noticed a morale boost in the workplace during this period and described SUH as providing fun, excitement and novelty in the office:
For me, the Stand Up for Health . . . it’s about being healthy, bringing health into the workplace, it’s about getting our staff to look at their health in more detail, get them concentrating on doing something that’s good for them . . . We deal with some really, really difficult phone calls . . . and something like Stand Up for Health can really, really help with that. It can really help with de-stressing and making things a lot calmer on the section.
Centre 11, stakeholder
Staff also felt that their organisation’s willingness to participate in SUH and implement intervention activities made them feel that management really cared about their health and well-being. For example, one centre purchased wireless headsets, a suggestion made by the research team during a discussion with the centre’s SUH committee. The wireless headset made staff feel more comfortable standing and moving while on calls and removed the notion of being physically tied to the desk:
We’ve also tried a wireless headset as well as a part of that and that’s been a real success, now we’re just putting in an order to purchase some more of those for the team.
Centre 11, stakeholder
Reach: programme awareness
Many staff felt that SUH was well advertised and reported being aware of the SUH programme through e-mails, posters and attending or reading and/or hearing about the workshops. Once the equipment was set up in the centres, staff who were previously unaware of the programme were intrigued by the presence of new equipment, and subsequently became aware of SUH. Some staff reported noticing the equipment but did not know what it was for because of miscommunication or lack of communication and labelling of equipment. This sometimes led to confusion over who the equipment was to be used by, particularly if it was located in shared spaces. Several centres described creating programme awareness within the centre to be challenging and recognised the need to consider more effective ways to do so in future:
. . . it’s quite a hard organisation to get messages across because we’re so sort of risk averse, and everything takes time. Yeah, I was a bit naughty and just put the stuff out and got it sort of going really. It’s just one of those things, as with any large organisation, it’s never going to be perfect when we’re experimenting with things.
Centre 2, staff member
Reach: programme participation (coverage and participant engagement)
All centres reported that > 50% of staff participated in at least one aspect of the SUH activities. Centres felt that several staff members were actively involved in the programme and participated in activities on a consistent basis. Activity participation and preferences of staff were analysed from questionnaire data. Out of 51 staff who completed the post-intervention questionnaire (pre lockdown), 65% reported participating in at least one activity. The proportion of staff who used equipment or participated in activities once or more during the 6-month pre-lockdown intervention period is presented in Table 5.
| Activity | Proportion of staff who used equipment or participated in activities once or more during the SUH programme (n = 48) |
|---|---|
| Desk-based equipment (e.g. treadmill and standing desk) | 31% |
| Non-desk-based equipment (e.g. power plate and table tennis) | 15% |
| Mindfulness (e.g. Lego, colouring in and jigsaw) | 25% |
| Group activities (e.g. group walks and team challenges) | 13% |
| Individual activities (e.g. walks, running and cycling) | 38% |
The SUH activities were commonly perceived to be accessible to all staff who wanted to participate, regardless of their job role or physical ability:
. . . so those that were using the equipment, I would say we probably got 80% of the staff of the whole centre because that was available obviously for a longer stretch of time . . . when it disappeared, I had lots of messages asking, where’s it gone? So, it certainly was noted and, as I say, a far higher degree of people obviously had the opportunity to use it and then obviously managed to attend the workshops.
Centre 2, stakeholder
However, some participants reported that the office layout and location of staff and activities (namely equipment) affected their participation. Staff whose desks were closer to the equipment and in offices with a more open floor plan found it easier to use the equipment and see others using it. Both stakeholders and staff in many of the centres noted small numbers of employees who were generally disinterested in engaging in activities that were not immediately related to their job and, therefore, did not participate in the programme.
Reach: stakeholder buy-in
Buy-in and ongoing, open communication was needed from all teams, including senior management, middle management, health and safety teams and all of the other ‘right’ people. All centres had some form of buy-in from middle and/or upper management, and stakeholders described the process of obtaining buy-in as fairly easy. Seeing managers engage with and motivate others to participate in the intervention motivated staff to take part and made them feel that it was acceptable to do so. Centres with managers actively involved in the programme were the most enthusiastic and had the highest uptake of activities:
Yeah, both of them [i.e. managers 1 and 2] have been pushing this 100% and they’ve given it 100% backing right from the start.
I think if we didn’t have someone like [manager 1] and [manager 2] pushing it, it could . . .
Yeah, and it probably would have to be fair, it probably would have been shelved. But they’ve made it . . .
It’s a daily thing.
Centre 11, staff
There were issues identified in some centres that related to buy-in by management or senior levels. A lack of communication between the various managerial levels made it difficult for the research team to discern who was aware of and on board with the programme. In a few centres, there were also concerns from management that activities would impact on productivity; this meant that involvement in SUH was not perceived as a priority. It was, therefore, suggested that lower levels of buy-in could be a result of insufficient justification to management on the practical benefits of SUH, such as increased productivity and decreased sickness absence. Some centres took only small steps to obtain buy-in and make the necessary changes for SUH and other staff well-being initiatives. This minimal involvement was often owing to bureaucratic challenges and the ongoing need to repeat communication about the programme and evidence its benefits to management:
. . . they [higher management] were all open. Their only reticence, and again, it comes back to that: how is it going to impact the productivity, are people going to be delayed or . . .? And so their negativity was if you’re abstracting people, that’s going to have a negative impact on the productivity.
Centre 2, stakeholder
Barriers and enablers
A range of barriers to and enablers of engagement in intervention activities were presented in interviews and focus groups.
There were a number of organisational factors that influenced participation in intervention activities. The most prominent barrier was time: the rigidity of the contact centre environment (timing and length of break times, targets, percentage of staff required to take calls) did not allow for participation in intervention activities. This was mitigated by some centres in which management tried to schedule ‘active breaks’. Managers were also asked by staff to consider changing shift patterns and break times. Most centres, however, were inflexible on these items, but some found workarounds, such as scheduling intervention activities before and after work or incorporating activities that staff could do while working:
So, in dispatch, you’re tied to your desk, especially when it’s busy, which is mostly 24 hours. You’re very much tied to your desk, almost literally, in the side where the calls come in, because you don’t choose to answer the phone, your phone goes and it’s in your ear. Your breaks are tightly monitored, including going to the toilet.
Centre 2, staff
As previously discussed in earlier themes, advertising the intervention was a key factor in participation. Centres in which management actively advertised the programme (e.g. through individual e-mails and conversations) saw increased participation. Other centres noted that there could have been better advertising of the programme and activities, including placement and labelling of equipment and advertisements. Despite efforts to advertise SUH, some centres acknowledged that it was generally difficult to get any initiative off the ground for various reasons, such as the office environment and general logistical issues:
. . . I suppose it’s the advertising of it, how do we get it across all the different channels without it becoming just another paper exercise or another spam e-mail? . . . I think when you’re trying to do it through e-mail or, you know, just a poster here and there, it’s a challenging one, it is a challenging one.
Centre 3, stakeholder
The presence or absence of stakeholder buy-in acted respectively as an enabler of and barrier to participation. In addition, health and safety policies and other organisational rules presented barriers to certain activities. The lengthy approval process for granting exceptions to rules or getting permission for certain activities (e.g. the use of exercise equipment) provided additional challenges. Staff in one centre were required to wear a uniform to work and some felt that this made it less comfortable to be physically active at work.
The physical environment of the centre, and the placement and appropriateness of equipment in the office, was viewed by staff as important. If equipment was well placed, was visible and fit well in the desk space or the office generally, this enabled its use. Staff from a few centres described not having enough space for physical activities at desks and/or common areas and having a rigid office environment as challenges to participation. Some were unable to use the equipment provided while working owing to the risk of being out of breath or distracted while on calls. The placement and labelling of equipment was important in determining if equipment was noticed and used. Some centres were unable to, or did not, put equipment in places where staff were prompted to use it. In addition, if equipment was not labelled properly, staff got confused and did not know if it was meant for them, what it was for or how to use it:
I would just probably say space because we only had like a little room where you could go in. I used to hula hoop every day and because I didn’t want to be watched by certain people in the team, I’d have to pull the blinds down. So it was just basically to do stuff I suppose. Because that room did get cramped and it did get smelly.
Centre 10, staff
Some centres embraced social activities, such as competitions and walking groups, whereas others felt that there was a lack of enthusiasm from enough people to gain momentum. Another social barrier was the perceived lack of social acceptability of some activities. Some participants reported feeling judged by other staff, with some opting out of certain physical activities because the idea of others watching them made them uncomfortable. The social acceptability was mitigated at times by the participation of managers and their encouragement of other staff members:
I think, probably where we had the most negativity, was other teams. So other teams in the office would kind of look and say, well, you know, why are they doing that? Why . . . you know, they’re just playing golf, or they’re just, they’re playing table tennis, they’re supposed . . . you know, they’re asking us for help with work, but this is what they’re doing. So we had to do a lot of comms to kind of just kind of, you know, just try and reduce that negativity from other teams. But senior leadership buy-in was really good, but it was about a lot of communication.
Centre 10, stakeholder
Individual mindsets and circumstances of staff played a part in the uptake of activities. It was acknowledged that there were always staff who refuse to participate in any initiative and are never satisfied with what is offered by the organisation. Other staff simply want to go to work and go home without engaging in non-work-related activities.
Effectiveness
The staff and stakeholders from participating centres felt that the SUH programme was successful with positive outcomes, and that the programme promoted healthier thinking and behaviour. They consistently noted an increase in physical activity and reductions in sedentary behaviour among staff.
Several other perceived benefits were reported, including:
-
Mental health benefits – it was felt that the SUH programme improved staff morale and mood. Staff reported feeling happier, more relaxed, energised and alert, and less stressed. One stakeholder reported an observed reduction in staff absence owing to mental health issues since the SUH study started.
-
Physical health benefits – staff reported reductions in weight and improvements in musculoskeletal issues and health conditions, such as Reynaud’s syndrome, as well as improvements in blood pressure:Centre 11, staff
I’ve actually gone down from 14 stone 7 to 13 stone 8 in the last couple of months. I’m really feeling better. My blood pressure’s improved and I just feel generally 10 times better than I did a few months back.
-
Staff engagement and productivity. Staff and stakeholders felt that, as a result of the SUH programme, staff were engaging as a team and supporting each other. Stakeholders felt that staff were more efficient and alert, and noted improvements in productivity and reduced sickness absence:Centre 10, stakeholder
. . . it made a difference to sickness absence. It made a difference to productivity. So for us, kind of call time and after call time, before the programme, was 12 minutes. After the programme, it was about 10 minutes.
A total of 34 centres from across the UK were targeted, and 16 of these centres got in touch with the SUH team to express an interest in participating. Of those centres, 11 actually participated, as study protocol required that only 10 centres take part.
Implementation of the Stand Up for Health intervention
Organisational changes
As mentioned above, most centres felt that the various levels of the organisation supported the SUH programme, and SUH was seen as part of the agenda to promote health and well-being among staff:
. . . we’ve kind of given them something to think about in terms of us going for a health award in the workplace because they see Stand Up for Health as being a really key part of that, not just actually obviously within the customer service team but something that can be implemented across the whole organisation . . . I think Stand Up for Health is seen as part of a bigger picture which is about making sure we have happy, healthy staff.
Centre 11, stakeholder
Initiatives undertaken at the organisational level included sanctioning hands-free wireless headsets (centre 11) and allowing staff to take an extra 30-minute SUH break on a weekly basis (centre 10). Two centres did not report any initiatives implemented at the organisational level (centres 2 and 6). These centres had more rigid organisational set ups, and implementing new ideas was perceived by stakeholders as a time-consuming process. However, it was felt that the SUH programme had initiated change, and there were discussions around ideas and suggestions at the organisational level. These small steps were seen as important changes.
A SUH committee (sometimes, the SUH committee was comprised of a centre’s existing health and well-being committee) consisting of multiple staff members across teams was set up in four centres (centres 2, 3, 10 and 11). These committees were perceived by participants to be integral to successful implementation of the programme through developing, operationalising and implementing several activities. In one centre (centre 10), the committee also promoted the SUH equipment, thinking through safety and arranging logistics (instructions, photos, hygiene and booking system). A SUH committee was not set up in centre 6.
Environmental changes
Staff described enjoying using the various pieces of physical equipment supplied by the research team, such as the ball desk chair, desk bike, treadmill and standing-desk risers. Some noted that participating in non-physical activities, such as jigsaws and colouring in, was appealing to those who did not want to take part in physical activities. Some centres and individual staff reported purchasing their own equipment, or utilising items that were already in the office to reduce sitting and increase physical activity (a few centres secured funding to purchase these items). Staff who had limited break length and frequency preferred activities that could be carried out at their desk, such as colouring in, the use of hand-held equipment (e.g. bands), under-desk pedals and ball chairs.
Initiatives at the environmental level in the participating centres included the following:
-
Meetings were held in a room in which equipment was set up, with the staff using different pieces of equipment (centre 10).
-
A dedicated room for exercise classes with yoga mats, wrist weights and hand weights, and purchasing disco lights was set up (centre 10).
-
Hands-free wireless sets were purchased after a successful trial (centre 11). The use of hands-free headsets had been suggested by the SUH team and allowed staff to move freely without being tied to their desk.
-
Based on the SUH experience, centres purchased several pieces of equipment (centre 11: two or three ball chairs, cycle equipment, colouring pens, jigsaws and Lego; centre 10: small weights). Staff also brought in their own equipment (stepper, twisting discs, pedals, hula hoops, colouring sheets, word searches, puzzles and jigsaws in centres 3, 10 and 11).
-
Reminders to take a break were set up on computers (centre 11).
-
Centres came up with mindfulness initiatives (centre 10: purchased jigsaws and supplied more colouring sheets; centre 2: planned mindfulness sessions).
A range of equipment was used by the staff. Popular equipment used by the staff is listed in Table 6.
| Popular equipment | Mindfulness equipment/activities | Social activities | Individual activities |
|---|---|---|---|
|
|
|
|
Staff were very positive about the desk risers donated by Sit–Stand.com® (Coalville, UK) and felt that they were helpful to those with health issues, such as back problems. Several centres were considering purchasing desk risers and desk bikes (centres 2, 3 and 10). Staff especially liked the equipment that created social interaction and competitions, such as table tennis, darts, pedals and the stationary bike, as well as equipment that they could use at their desk, such as exercise bands, wrist weights and power spin. They enjoyed mindfulness activities, such as colouring in, jigsaw, Lego and word search, and felt that these simple activities made a big impact. Some mindfulness activities, such as colouring in and jigsaws, became a team effort. However, some staff reported that they found the colouring in and Lego childish.
Implementation aspects of environmental change
Co-operation, co-ordination, communication and planning in advance with health and safety teams and facility managers were perceived by stakeholders as crucial for environmental change, especially for the use of equipment. In one centre (centre 6), insufficient communication (between the SUH teams and the centre, as well as within the centre) led to the removal of the SUH equipment during the initial phases of programme implementation. Excellent co-ordination and advanced planning, meanwhile, resulted in successful programme implementation and strong environmental change in centre 10.
Social change
Many social activities were implemented (see Table 6). Staff and stakeholders felt that these helped bring groups together, allowing individuals to support each other and cultivate new friendships. Through promoting teamwork and engagement and enabling staff to share their stories and ideas, the programme generated motivation and enthusiasm among staff to stand up more and be active. Staff from one centre said that there was increased social interaction during later shifts. SUH equipment, mindfulness activities and competitions provided opportunities for social interaction, and the range of activities engaged more shy staff members, as well as those who were not initially interested in the programme:
At the beginning, me personally, I was like, oh, I’m so excited – [the vibroplate] and the treadmill. But to be honest, it was more of the engagement activities, it was more of the ping pong and things like that, that you were doing with other people that, you know, got me involved. And I think that’s what a lot came out of . . . with it was that the engagement that it made across the team as well, it just heightened everything, it was really good.
Centre 10, staff
There’s definitely an increase of discussion, particularly when I’d go around the pods and ask, how’s the ball chair and whatever? The feedback I was getting was that it has definitely improved morale because they were definitely talking about it and there was quite a lot of amusement or even sort of interaction about it. But again, most of it stems around the ball chair, some around the little steppy kind of thing as well, and the vibration plate that . . .
Centre 2, stakeholder
Staff and stakeholders from two centres reported that they were not aware of any social activities being implemented as a part of SUH. In one centre, logistical issues (e.g. lack of space/time) affected the implementation of some activities despite stakeholder buy-in and enthusiasm from staff.
Individual change
Staff members described individual-level activities that they undertook (see Table 6). They reported being motivated to take up and participate in activities that made them feel better, and even feeling inspired to undertake activities outside of the office. Seeing others undertake activities prompted them to be more active and do the same. Another mechanism staff employed to increase their physical activity was goal-setting (e.g. celebrating when they achieve their goal of 10,000 steps per day). A few staff members were proud to say that they had lost weight through participating in SUH activities within and outside of the office.
Website and forum
A small number of staff from a few centres signed up to the SUH website and forum and said that they found it to be useful. They contributed photos and used some of the suggested ideas.
However, the website and forum was not used extensively and was not used at all in some centres. Some stakeholders reported that logging into the website and forum was difficult. Stakeholders also felt that they (themselves and the research team) could have promoted it better. They expressed a need to explore the best means of promoting it to staff members. E-mails and posters were considered ineffective promotion formats and an event dedicated to the website was suggested. Staff also felt that maintaining anonymity on the website and forum was important.
Staff and stakeholders provided suggestions to increase website and forum usage, such as ensuring that there is content on the website with regular input; offering incentives or having a reward scheme; generating interest through competitions and challenges (including competitions with other centres); offering ideas on what to post; and providing a window to the SUH activities of other organisations.
Ownership
A sense of ownership among staff is a proposed mechanism of change within the SUH programme theory. In most centres, staff described feeling a strong sense of ownership. They were very involved and engaged in the programme and felt that they could give ideas and have their voices heard. They suggested activities (e.g. Pokémon Go, Dungeons and Dragons, Clubercise class, walking; see Table 6) and brought in their own equipment and supplies (e.g. funny colouring in, colour pencils, jigsaws and pedals). They also acted as role models within teams, that staff would then follow:
And which aspect of the programme do you think worked well?
I think the actual getting people involved in coming forward with their own activities of what we could do, because I think that, sort of, went out to the wider audience . . .
Centre 3, stakeholder
However, in two centres (centres 2 and 6), staff did not feel a sense of ownership. They felt that voicing an opinion did not lead to implementation or change in their centre owing to logistical barriers (venue, time and public liability insurance). They noted some progress towards a more inclusive approach, with discussions and meetings being held to procure suggestions for programme activities from teams.
Sedentary behaviour and physical activity awareness
There was an increased awareness of the importance of sitting less and moving more in contact centres. Staff were also more aware of the risks associated with prolonged sitting, as well as the positive aspects of sitting less and moving more. Some staff noted that they had not thought about sedentary behaviour before the programme and felt that SUH had highlighted the dangers of being sedentary, a behaviour particularly prevalent in the contact centre environment. They reported that they were now more conscious of sitting too much at work and that SUH had spurred on staff to look for solutions, such as wearing activity trackers, searching for equipment on Amazon (Amazon.com, Inc., Bellevue, WA, USA) and taking more breaks. Staff from one centre (centre 10) also felt that participating in SUH made them realise that they could be active whilst working. In this centre, the stakeholder reported that the increased awareness among staff about sedentary behaviour and physical activity had longer-term effects and helped staff to stay active and sit less during the transition to home working:
I would agree with Marie. I think for me I had recognised that I sit too much during work and there’s been so much in the media now, we know that it’s not good for you. I think it just means that you’re trying to improve your mental well-being as well as your physical well-being.
All the mindsets are being changed since we started this, just even little things like sitting at you desk doing a puzzle, you’re not just sitting there, you’re doing something. Everybody’s changed in a way, even if it’s just a little way.
So, you think the mindset’s changed as a result of Stand Up for Health?
Uh huh, yeah.
Centre 11, staff
Programme suggestions
Contact centre staff and stakeholders made suggestions at organisational, environmental, individual and social levels to improve programme delivery and implementation. Suggestions to improve the use of the SUH website and forum were provided. It was felt that SUH should be better promoted and staff made suggestions for promoting the programme. A detailed list of programme suggestions can be found in Table 7.
| Level of change or other aspects | Participant suggestions |
|---|---|
| Organisational |
|
| Environmental |
|
| Social |
|
| Individual |
|
| Promotion and awareness |
|
| Website and forum |
|
| Other suggestions for programme delivery |
|
Unintended consequences
There were three main positive unintended consequences reported by staff. The first was the adoption of a healthier diet by staff members, both individually and at group work events. Staff would ensure that healthier options were included in menus. The second was increased physical activity outside work, including swimming and Parkrun. Finally, there was interest and participation from other centres, departments and teams. Staff and stakeholders mentioned that those visiting from other centres were intrigued by the equipment and even used some of the equipment and participated in activities that were organised as a part of SUH. One participating centre mentioned that they shared the principles of the programme with another centre:
. . . and as a team we have dress down days, where we have buffets and now when we have a buffet nobody ever bought healthy food in, but now on the list of the things to bring in, bring salads and pastas . . .
They’re still not healthy though.
There is a healthy option.
There is a healthy option but at one time we never ever had anything like that on a buffet.
Centre 11, staff
Acceptability and feasibility of the Stand Up for Health intervention: post-lockdown results
Reach: programme significance and appeal
Stand Up for Health was still viewed by stakeholders and staff as important post lockdown. Staff from centres that had already participated in the pre-COVID programme appreciated that the programme was adapted and continued, and felt that the SUH team did well in adapting the programme given the COVID-19 pandemic and the various restrictions that it gave rise to.
Staff associated SUH with looking after themselves and felt that this was especially important during lockdown. Lockdown was a tough period, during which staff had feelings of depression and did not really take time for themselves. They felt that SUH provided a purpose and a variety of activities to help them cope and that the individual consults provided a much-needed well-being ‘check-in’. The post-lockdown activities provided staff with motivation and reminded them why it is important to sit less and attend to their well-being. They also felt that the SUH message of sitting less and moving more was very pertinent during lockdown, especially in the call centre setting, where back pain was rampant:
Everyone who works in an office job knows that pain when you try and get up in the morning and you’ve got that shooting pain in the back everyone feels that. It doesn’t matter what job you do. So I think the message you guys project is so pure that people will just naturally rotate around it because literally you’re doing it for the betterment of people.
Centre 7, staff
Staff noted that the consults were effective in promoting and inspiring lockdown-friendly activities and initiatives that were novel, safe and enjoyable. They found the online resources for breaking up sedentary time and increasing physical activity provided by the SUH team to be helpful and informative. The consults and resources helped staff mitigate increases in sedentary behaviour and decreases in physical activity owing to the restrictions on activities during the pandemic and, for many, the shift to home working:
So I think it was possibly June when you . . . when we kind . . . when you first contacted us, and staff were starting to struggle at that point. We had a few kind of staff members struggling with kind of back pain and neck pain, and not moving around as much. So it was perfect timing for us, because we knew that kind of staff weren’t moving around as much.
Centre 11, stakeholder
Staff who were on site enjoyed using the equipment, and there were appropriate hygiene measures in place to ensure that they did not put employees at risk of COVID-19. A few centres were able to arrange for staff to borrow and use various pieces of equipment while working from home. Some staff said that using the equipment helped them to deal with stress and supported their mental health during the pandemic.
Many staff recalled the fun that they had during step count challenges, which were organised by either the SUH team or the centres themselves. During a time when social gatherings and activities were challenging and/or against the lockdown rules, step count challenges provided a fun way to encourage and support staff to engage in physical activity, with competitive elements that many staff welcomed and enjoyed.
Dislikes
Many staff were unaware of the SUH website and, therefore, did not access it. Some staff who were aware of and did use the website found it difficult to navigate. Other staff members mentioned a reluctance to use equipment (if they were working from the office) because they felt that they would stand out and the difficulty of using equipment while on calls.
Programme awareness
The majority of staff said that they received e-mails that made them aware of SUH. However, staff tended to receive many e-mails per day and sometimes missed those that contained information about the programme. Some centres received more e-mails during the lockdown and were substantially busier, which further impacted staff awareness levels. E-mails, messages, other personalised (as opposed to mass), and in-person communication tended to be the most effective in increasing awareness. Some staff who were able to go into the office became aware of the programme after the equipment was brought in, noticing its presence and reading posters nearby or asking colleagues about it. Several staff in one centre noted becoming aware of the programme through a step count challenge, which was facilitated by the research team, and noted that this specific activity was well advertised and well attended.
Reach: programme participation
Coverage
Post lockdown, it was more difficult for managers to quantify physical activity and consult participation because their staff, and sometimes they themselves, were working from home. This limited their ability to see or be prompted to check participation levels. As mentioned above, it was difficult to get in contact with people working from home and make them aware of SUH activities.
The consultations were made available to everyone; however, the use of the Microsoft Teams platform to conduct them presented a barrier because not all staff were able to access this software (although most did). In centre 7, it was noted that roughly 30% of staff had consults.
The equipment was available only to staff who went into the office and for some staff at centres that were able to establish equipment-borrowing procedures for home working.
Forty-seven participants completed the post-intervention questionnaire for the post-lockdown period. A total of 95% of staff participated in at least one activity. The proportion of staff who participated in the different activities over the 3-month post-lockdown intervention period is presented in Table 8.
| Activities | Proportion of staff who participated in different activities during the post-lockdown SUH programme (n = 41) |
|---|---|
| Social activities (e.g. step count challenge and walks/activities with those in your household/colleagues) | 44% |
| Virtual social activities with an active component (bingo/quiz with active component/virtual social exercise classes) | 59% |
| Individual activity | |
| Goal-setting | 54% |
| Desktop stretches | 51% |
| Exercise videos and apps | 35% |
| Other (e.g. walking, running and cycling) | 85% |
| Used mindfulness resources | 36% |
| Used SUH website | 10% |
| Environmental activity: made changes to desk space to help reduce sitting | 37% |
Barriers and enablers
Organisational
Similar to the barriers reported pre lockdown, time was a persistent issue influencing activity participation post lockdown. Key reported barriers included the difficulty for staff getting time off the telephones to participate in the consultations and any group activities. Centres were generally busier and more target focused during lockdown, and there was a significant amount of ‘firefighting’ to swiftly adjust to the constantly changing circumstances brought on by the pandemic:
We have a lot of, you know, mental health issues, at the moment, and that’s across the board, and that’s mainly brought on by the whole COVID situation, and I just think, for me, personally, it’s a little bit more challenging [to engage with SUH].
Centre 6, stakeholder
Environmental
Some staff who worked from home noted working longer hours owing to the blurring of the home and work environment. In addition, many staff did not have the appropriate space or equipment to sit less and move more while working from home, and working from home also led to less incidental movement (such as walking around the office to attend meetings, speak with a colleague or use the washroom):
You know, this morning I logged in at 8 o’clock and then before I knew it, it was half 12, and basically, I haven’t moved from this seat for that period of time, whereas at work I definitely would be moving about at work, you know? Even if it was to go for a coffee or to speak to someone or something. It’s almost worse when you’re working from home because you’re on your own, you’re in your own room and you’re not getting that opportunity.
Centre 6, staff
As mentioned above, the change in working environment had a detrimental impact on staff awareness of the intervention. The weather, particularly the winter darkness, was discussed as demotivating and a barrier to participation in outdoor physical activity, which was one of the few options during lockdown.
Social
Engaging staff in social activities was difficult, as not all staff worked in the office and it was felt that online social events were not the same as in-person social events. Several centres onboarded staff who had never set foot in the office, which presented an added challenge to the social aspect of teams and participation in social activities. Some staff had previously been motivated by simply being in the office environment and around colleagues who inspired them. Despite this, staff still managed to get involved with online social events and competitions, such as step count challenges, which boosted morale and gave them a reason to be more active:
I think the main thing I’ve been lacking in is motivation because I am lazy and I am someone who needs spurring on. In the office, we were spurring each other on, you know. At home, probably not so much.
Centre 10, staff
Individual
Individual barriers included increased stress and anxiety and generally poorer mental health owing to the pandemic and the circumstances it put people in. This and the shift to home working, made it difficult for employees to keep physical activity and sedentary behaviour at the forefront of their minds. Several staff noted a lack of motivation to sit less and move more and expressed a need for additional encouragement and reminders during the pandemic. In some centres, this was mitigated by managers reminding people to get up and keep active during the day:
. . . it’s just sometimes then having the time and motivation to go and, you know . . . [be active]
Centre 6, staff
Effectiveness
Perceived benefits
Staff perceived several benefits from the post-lockdown programme, including increased physical activity, improved mental and physical health, increased focus and concentration and reduced stress. Benefits were mainly reported by centres 6 and 7 and related to the step count challenge and use of equipment:
I believe it was a balance board you guys had sent in so I really enjoyed the balance board . . . but it was really good to sort of get that level of concentration because I feel like especially in my sort of job when you have a monotonous day, it’s just one call after another, the same old people trying to save money, so the fact that I could go on my break and when I was on the balance board I had no choice but to fully focus . . . I think that was a good thing because it gets your attention off the long monotonous day that you have ahead of you . . .
Centre 7, staff
Implementation
Only a few organisational and environmental changes occurred as a result of the post-lockdown programme. In centre 7, higher management were aware of the programme and had discussions about it. Centre 7 buildings were being refurbished and there were plans to incorporate elements and principles of the programme to encourage more movement among staff (e.g. pitch and putt areas).
A large proportion of staff were working from home and felt that home working environments were quite constrained. Staff made small changes, such as moving around the house during breaks and using toilets upstairs, to increase activity. They also made some ergonomic changes, including purchasing a more comfortable chair and using a yoga ball chair. Staff made use of equipment either in the office (if they were able to go in) or at home (if their centre had arranged for them to borrow items). Staff enjoyed using equipment, such as balance boards and ball chairs, in both settings.
It was felt that SUH generates social interaction in the workplace through equipment use and competitions, but generating social interaction is more challenging while staff are working from home. The step count challenge increased interaction as well as physical activity. Staff communicated with each other on WhatsApp (Meta Platforms, Inc., Menlo Park, CA, USA), inspiring and motivating each other, and even discussed different topics. SUH also enabled staff to get more active with family members. Social interaction was severely reduced owing to COVID-19 and it was felt that the programme was beneficial in this regard. Another effect of SUH was that staff were meeting each other and walking in parks and at the beach when lockdown was eased.
Changes at an individual level included goal-setting strategies (having a target number of steps per day, standing up in meetings). The motivation to increase physical activity came mainly from the step count challenge. Staff purchased activity trackers to help reach the target step count. The step count challenge helped to create routines that enabled an increase in physical activity in the longer term. Staff were motivated to do exercises because they helped with musculoskeletal issues (such as a stiff neck). The stakeholder from centre 7 noticed a change in thinking among staff and a shift to healthier and more active behaviour. For example, staff were more likely to take a walk rather than sit and use their mobile telephones. Motivation to move more during breaks and finding ways to increase activity also stemmed from a desire to improve mental and physical health. Staff said that the consults provided suggestions for improving mental health and increasing physical activity:
Yes, and I also got myself a Fitbit during the challenge and . . . I used to get the activity reminders, the hourly activity reminders and do you know, because sometimes it’s just these little reminder things. I mean, one thing I would say that kind of a longer-term change that’s come off the back of the walk challenge was that . . . I extended the walk in the morning that I would go on. Like I would drop them off and then extend the walk slightly and I have more or less kept that up . . .
Centre 6, staff
Ownership
Feelings of ownership were not strong during the post-lockdown programme because staff were more isolated while working from home. Some staff reported being able to make suggestions and contribute to the step count challenge.
Sedentary behaviour and physical activity awareness
Awareness regarding reducing sedentary behaviour and increasing physical activity has been mentioned in Sedentary behaviour and physical activity awareness and has been summarised here. Staff felt that the consultations helped to create awareness about sedentary behaviour and physical activity, and encouraged them to think about moving more and about physical activity guidelines. They noted that the consults made them aware that they were even more sedentary while working from home. A stakeholder perceived that SUH was instrumental in initiating a change to more healthy and active behaviour among staff.
Website and forum
In general, staff from participating contact centres did not really use the website and forum. They felt that the website was not easy to navigate; most did not access the resources on the website. Some staff reported that they were unsure about where to register for the step count challenge and felt that better signposting would have helped.
Consults
In total, 64 staff members from four centres participated in the consults. Staff reported finding the consults useful. It made them consider their current activity levels and think about being more active. It prompted them to get more active (e.g. taking up running, walking or cycling) and take active breaks (e.g. jigsaw and moving around the house on a break). A stakeholder from centre 10 commented on the timeliness of the consults, as staff had started to feel the strain of the lockdown and were struggling with back and neck pain. Staff found that the suggestions made by the SUH team were useful and appreciated that the consultation was tailored to each individual. They felt that the consults acted as an encouragement and several ideas were discussed that may not have occurred to them otherwise:
They [the consults] were received really well. I think they came at a time where staff were starting to kind of flag . . . I think it was possibly June when you first contacted us, and staff were starting to struggle at that point. We had a few kind of staff members struggling with kind of back pain and neck pain, and not moving around as much. So it was perfect timing for us, because we knew that kind of staff weren’t moving around as much . . .
Centre 10, stakeholder
The SUH team faced issues with reaching staff members in a few contact centres, as some teams did not have access to a telephone or Microsoft Teams. One centre was planning to set up a manager’s laptop with Microsoft Teams because the desktops did not have this facility. They then encouraged staff to download the software on their telephones and personal laptops. The lack of appropriate technology made organising consults with staff more difficult.
Some centres (centre 3) did not have the capacity to allow staff to go offline to take part in the intervention. Staff had to take part in their own time and many did not want to do this. It was also a very busy time for the centres (owing to the pandemic and package changes), making it burdensome for staff to take part.
Activity plan
Staff felt that the activity plan gave them a comprehensive list of ideas and resources that they would not have had access to otherwise. Staff found the plans useful and took up activities (e.g. running and spinning) after receiving them. The desk stretches suggested in the plan helped staff with musculoskeletal issues, such as stiff neck and shoulders. Movement was restricted during lockdown and the plan reminded staff to move and inspired them to find new routines and take breaks from the screen. Another positive aspect mentioned was that the plan could be adapted and included different options (e.g. mindfulness activity for a staff member who broke her foot):
So I think checking in was really good because it kind of just reminded me like, you know, to try and find a new routine to just do like little and often type thing. And then you guys suggested like loads of different stuff that I could do, just like take breaks from the screen and stuff like that. So, it was a really good resource and there was, like, loads of suggestions in the pack that got sent through.
Centre 10, staff
Step count challenge
Staff experienced physical and mental benefits from participating in the step count challenge. Staff reported increased activity during the challenge, set goals and purchased activity trackers. They felt that the challenge made them aware of how inactive they were on most days. It had a perceived long-term effect of increasing activity through forming new habits and routines. It was also felt to help increase social interactions in which staff would challenge and inspire each other, which was also a motivation.
The stakeholder from centre 6 had hoped for more participation in the step count challenge, but reported that workload was a barrier and co-ordination with individual participants was difficult. Staff felt that better signposting on the website on how and where to register would have been helpful. Not everyone was aware of the SUH website and forum, and not everyone was posting their steps. Introducing participants to each other and encouraging people to interact would have enhanced the experience for staff.
The weather was cited as an important factor to the success of the challenge and it was felt that increased physical activity was difficult to sustain as it got dark earlier. Staff perceived that sustaining activity would be easier if the challenge started in the spring, so that they could create a habit over the course of the summer, which could then be sustained. It was felt that the challenge would not be successful if it started in winter.
Programme suggestions
Most staff felt that the programme had been adapted well, given the COVID-19 lockdown restrictions. Working with staff members to come up with individual, customised programmes for their circumstances was seen as useful and important during the move to hybrid working formats. It was felt that mechanisms to keep the momentum going were required and the following mechanisms were suggested: regular, brief check-ins with staff; staff could updating the website with their undertakings; encouragements and reminders; weekly e-mails; and means by which staff could help and motivate each other.
Having somebody from the centre (e.g. a stakeholder) on site, who was hands-on and promoted the programme, would encourage staff engagement and participation. Stakeholders felt that greater promotion of the social channels, such as the website and forum, would be helpful. It was also deemed to be important to find the right time to conduct activities, as some centres may be extremely busy during certain months. In one centre (centre 6), it was felt that the focus was often on the front-line staff and that the back-line staff were overlooked. It was considered important to work with stakeholders to ensure that all staff were included in the programme.
As in the pre lockdown period, staff suggested conducting challenges. One staff member from centre 7 felt that the SUH message was strong and relevant, but to entice staff to participate comedic and creative tools could be used, for example the SUH team and staff could create funny videos. It was felt that adding a twist to the challenges (e.g. dressing up, taking pictures) would further increase social interaction.
As mentioned in Step count challenge, the weather was cited as an important factor to the success of the step count challenge, and it was therefore suggested that the challenge should be conducted in the spring or summer months. It was felt that if this were the case, staff would continue to be active over the course of the summer and that being active would become a habit. Other suggestions relating to the challenge included better signposting on where to register, introducing participants to each other and encouraging people to interact. Staff suggested that the challenge could be extended to something even bigger, such as walking around the world.
Other consequences
The main negative unintended consequence mentioned was the potential for injury while using equipment, such as a balance board. A positive unintended consequence of the programme was the adoption of healthier diets by staff.
Maintenance
Budget for Stand Up for Health
A key aspect influencing the maintenance of implementing the SUH intervention is the need for an appropriate budget, primarily for physical equipment. Several centres reported having budget approval based on the creation of a business case around improvement in productivity (call time) and a reduction in sickness absence as a result of programme feedback. This has, or will, lead to the purchase of equipment, such as wireless headsets, desk bikes and desk raisers, and smaller items, such as small weight sets and yoga mats. However, it was noted that the purchasing of equipment in some centres had been put on hold because of COVID-19. In one centre, no specific budget was allocated to maintaining SUH; however, the availability of internal and external budgets/grants for changes to the environment and well-being initiatives were identified as alternative funding mechanisms. In addition, staff in several centres reported purchasing equipment (including pedals, jigsaws, table tennis sets, steppers and hula hoops) themselves to allow them to continue to engage in SUH activities.
Future of Stand Up for Health
The centres were happy that the programme did not ‘fizzle out’ and was adapted for the COVID-19 pandemic. Stakeholders from the centres wanted to continue with the programme and were expecting that the programme would grow slowly. They acknowledged that creating change was a slow process and that benefits would accrue in the long run. Some practices (e.g. huddles and walking) and initiatives (e.g. wireless headsets) have already been set up and will continue. However, it was not possible for some activities to continue (e.g. colouring in and jigsaw) because of COVID-19 restrictions. Staff said that they would like to continue and focus on SUH after the pandemic. The programme has created an awareness of sedentary behaviour and given staff a lot of ideas for working on site, as well as at home.
Feasibility of study design and procedures: pre-lockdown results
Recruitment and randomisation of centres
The recruitment target was 10 centres, and the SUH team was able to recruit 11 centres for the study. We had anticipated some difficulties in recruiting contact centres; however, in reality, it was a straightforward part of the project and we had recruited the majority of centres before the study had even begun. Contact centres welcomed the idea of new workplace health programmes and were very keen to take part. One of the major enablers was having input from Scott Lloyd (our co-investigator who is an Advanced Public Health Practitioner for Public Health South Tees). He arranged a day during which the research team went to the North East of England and presented to several employees responsible for workplace health from a number of workplaces. We showed a short video that we had made and answered questions from the employees. By the end of the day, we had secured six contact centre workplaces that were interested in taking part in the study. Once we had these workplaces, it was easier to secure more.
Randomisation of centres was conducted as intended. Centres were assigned a number by Jillian Manner and Divya Sivaramakrishnan. The statistician was blinded and randomly allocated centres to a time point based on the stepped-wedge plan for SUH.
Centre dropout
Five centres dropped out before the end of the study. One centre (centre 9) dropped out after the intervention was delivered but before the data collection procedures. One centre (centre 1) completed baseline data collection and programme delivery, but dropped out because of the COVID-19 pandemic. Three other centres (centres 4, 5 and 8) that had not started the programme or data collection also dropped out. The COVID-19 pandemic was the reason for two of these dropouts, as described in an exit questionnaire completed by centre 5 (summarised in Appendix 1). One centre (centre 8) reported in an exit questionnaire (summarised in Appendix 1) that changes in circumstances since registering their interest in participating was the main reason for dropping out. The SUH team retained four centres that had started pre lockdown (centres 3, 6, 10 and 11) and had one centre starting afresh (centre 7) with the post-lockdown programme. Responses to exit questionnaires completed by centres 5 and 8 are presented in Appendix 1.
Participant recruitment and dropout
Stakeholders felt that the recruitment process was generally easy for themselves and their staff, so long as it did not interfere with operational needs. They felt that the posters, information sheets and video provided by the research team explained the intervention well, were straightforward to distribute and generated interest in staff. They also felt that the research team worked effectively and efficiently with them to co-ordinate recruitment efforts and explain the recruitment process.
Managers making active efforts to recruit was an enabler for recruitment, and staff were often happy to have a break from being on the telephones. The SUH team making an in-person recruitment visit to centres, during which they could personally meet and explain the study to staff, was also an enabler. A barrier to recruitment in some centres was the perceived impact on productivity, leading to difficulties in conducting some elements of the evaluation; there were many staff who wanted to participate but could not for this reason.
For the outcome evaluation, we aimed to recruit 27 participants from 10 centres. The SUH team achieved recruitment targets until March 2020 to recruit 155 participants from six centres (centre 1: 21 participants; centre 2: 28 participants; centre 3: 27 participants; centre 6: 23 participants; centre 10: 33 participants; centre 11: 23 participants). Although the target of 27 participants was not met in some centres, this was mitigated by the fact that we had recruited 11 centres rather than the originally planned 10 centres. Participants completed the questionnaires, and a subset wore the activPAL device. However, owing to the COVID-19 pandemic, the SUH team could not make any more in-person visits. The teams post-lockdown recruitment efforts will be described in Feasibility of study design and procedures: post-lockdown results.
The recruitment aim of the process evaluation was to collect data from six to eight participants from each contact centre (with a total of 60–80 participants, assuming that 10 centres participated). This was meant to include six participants per centre for a focus group and one stakeholder for a stakeholder interview. However, interviews and focus groups were conducted with staff from five centres, with one focus group having only two participants. This is further discussed in the section on post-lockdown Data collection logistics.
By March 2020, the study had recruited 155 participants from six centres. Owing to the structure of the stepped-wedge design, this included follow-up data from two centres and baseline data from four centres. Unfortunately, before we could engage in follow-up data collection, the COVID-19 pandemic started and we had to move to online delivery and data collection. The study took on a slightly different form post lockdown; the SUH team contacted and co-ordinated with the centres, and staff members participated in a modified intervention and data collection. Owing to these unusual circumstances, we cannot definitively say that participants were lost to follow-up because the format had changed. However, a statistical analysis on reasons for dropping out was conducted and results are presented in the following section.
Statistical analysis of reasons for drop out (pre lockdown)
There were 13 out of 106 participants recorded as having left the company after the pre-lockdown data collection [12%, 95% confidence interval (CI) 7% to 20%]. There were 23 out of 106 participants recorded as having moved jobs after the pre-lockdown data collection (22%, 95% CI 14% to 31%). A multiple logistic regression model was fitted to each of the two binary outcomes (left the company and moved jobs). No variables were statistically significant predictors of outcome. The ORs for centre were of a high magnitude, indicating strong centre effects in the observed data, although these did not reach statistical significance. Interestingly, older participants (aged ≥ 55 years) and those working part time were more likely to have left the company after the pre-lockdown data collection, but again this did not reach statistical significance, perhaps owing to the small sample size. It is important to note that these effects may be at least partly because of the COVID-19 pandemic.
Data collection
Overall, staff reported the data collection methods to be appropriate and straightforward. Staff were typically keen to participate and happy to contribute to research.
Questionnaire experience
The staff did not report any issues with filling in the questionnaire and said that the process seemed ‘reasonable and fitting’. In total, 155 participants from six centres completed the questionnaire during the pre-lockdown period. Two centres (centres 2 and 11) completed the 6-month follow-up questionnaire only, and four centres (centres 1, 3, 6 and 10) completed the baseline questionnaire only. The study plan was to have 27 questionnaires completed at each centre, and this target was met or exceeded in three centres (centre 10: 33 participants; centre 2: 28 participants; centre 3: 27 participants). The SUH team fell short of targets in three centres (centre 1: 21 participants; centre 6: 23 participants; centre 11: 23 participants). As mentioned earlier, the additional centre recruited (11 instead of the initially planned 10) compensated for these shortages.
The activPAL device and logbook experience
Contact centre staff experiences of the activPAL devices were mixed. Some participants were intrigued by the devices and perceived the specified data collection procedures to be reasonable and appropriate. They reported that it was not awkward or uncomfortable and forgot that it was there. By contrast, some staff members were apprehensive about wearing the activPAL device because they felt that they were lazy and did not move much. Other concerns about wearing such a device were around not wanting to have something on their skin or having the device show through clothes (especially during outings or parties); these concerns prevented some participants from following data collection procedures.
The analysis of logbook data from 110 participants revealed that 34 participants (31%) removed the activPAL device before the removal date; 10 participants did not reattach this. A further 25 participants did not complete the section on activPAL device detachment. From the logbook data and qualitative focus groups and interviews, it was apparent that several staff members disliked the activPAL device and found wearing the device uncomfortable and irritating. They complained that they experienced burning sensations and skin rashes, which persisted after removal for some participants. Logbook data showed that most participants removed the activPAL device owing to skin irritation and the dressing peeling off. A recommendation to enhance adherence to the protocol would be to provide more dressing for the activPAL device to be reattached. Staff suggested that the activPAL device should be removed (and reattached) halfway through the 7-day period, or even every 2 days, so that the skin can be cleaned.
Staff found the activPAL device logbooks challenging to complete, reporting difficulties in accurate and detailed recall. In addition, staff from centres that had night shifts felt that the logbook was confusing. Therefore, the logbook needs to be better adapted for varying shift patterns. Suggestions included using an electronic medium with reminders, such as an app.
Data collection logistics
Data collection procedures, including the frequency and duration of visits, were deemed acceptable to centre stakeholders. These were considered appropriate to organise and co-ordinate. A recommendation to enhance data collection was to lengthen the period of collection over 1 week or train staff to issue activPAL devices so that the whole centre (with varied shift patterns) could be covered:
And did you think that, you know, the number of time points that we were making with it, was that, you know, a burden for your organisation or was that doable?
No, that’s absolutely doable, absolutely doable, no problem at all.
And how about the [inaudible 44:22] data collection that, you know, we came and I think . . .
I thought that was quite quick actually, I thought it really went quite smooth and I think it was good how we did it, I mean, we selected times for everyone, the majority of people were on time, which meant it went quite smooth, so I don’t think that was a problem at all.
Centre 10, stakeholder
Stakeholders found that the process of returning activPAL devices to the SUH team was ‘relatively smooth’. Some found it challenging to remind staff members about returning the activPAL device and chase up with them on this. The research team also needed to chase up stakeholders to post back devices that were not returned on their follow-up visits to the centres. Out of 132 activPAL devices issued, only one device was not returned over the data collection period. Owing to the closure of office buildings, 14 devices from centre 1 were lost.
There were several recommendations identified from the process evaluation that could be utilised to enhance data collection in future studies in this setting:
-
Additional recruitment planning and consideration for busy periods and for when staff were available.
-
Additional strategies for recruitment, such as the use of social media.
-
Staff should be given time off the telephones for data collection, which would encourage them to participate.
-
Staff should be informed in advance of the full details of data collection procedures, to set expectations of involvement as a research participant.
-
Staff members are shown the activPAL devices in advance, in the light of the concerns about the device.
-
Emphasising to participants the significance of data being collected and how it informs the study to improve adherence and completeness.
Feasibility of study design and procedures: post-lockdown results
Participant recruitment and dropout
Participant recruitment
The content of recruitment attempts provided by the SUH team was perceived by stakeholders as appropriate and effective. Enablers of recruitment during this period were methods such as Doodle polls, which reduced the administrative burden for stakeholders. However, there was some confusion when staff who had not previously participated in the programme or data collection were recruited, as they were unsure what they were recruited for.
As with recruitment pre lockdown, shift patterns and offline time posed a barrier to recruitment, and it was suggested that the research team liaise with centres to understand how to work around this more effectively. As mentioned above, having managers take an active role in the recruitment process, through sending out tailored, individualised communication, yielded the most interest in participating in data collection, whereas generic recruitment e-mails did not always get picked up.
One centre (centre 7) participated in only the post-lockdown programme. The SUH team recruited 24 staff members from this centre to participate in data collection. In addition, 46 staff were recruited from four centres (centres 3, 6, 10 and 11) to participate in pre or post measures. A statistical analysis was conducted to understand reasons for dropout, and the results are presented in the following section.
Overall, 5 out of 54 participants left or moved after the baseline post-lockdown data collection (9%, 95% CI 3% to 20%). There were no clear patterns in the demographics among those leaving. Overall, there were 26 out of 54 participants lost to follow-up (48%, 95% CI 34% to 62%). Results of the multiple logistic regression model to the ‘lost to follow-up’ variable showed that participants in the 35–54 years age bracket were significantly less likely than those aged < 35 years to be lost to follow-up (p = 0.02). Male participants were significantly more likely than female participants to be lost to follow-up after 3 months in this analysis (p = 0.01).
Data collection
Questionnaires, focus groups and interviews
Staff felt that the questionnaires were easily accessible and simple and straightforward to complete.
In total, 53 staff (from five centres) completed the baseline questionnaire and 45 completed the follow-up questionnaire. In accordance with the study protocol, although those who completed the baseline questionnaire were encouraged to complete the 3-month follow-up questionnaire, additional staff could complete the questionnaire at follow-up. Twenty-four staff members who completed the baseline questionnaire did not complete the follow-up questionnaire. One reason for this, provided during the qualitative focus groups and interviews, was that some thought that they had already completed it. It was felt that the SUH team should emphasise the importance of completing the questionnaire at both time points. Staff said that they enjoyed participating in the focus groups.
Data collection logistics
Contact centres are often extremely busy owing to a myriad of reasons, including changing staff role, new staff interviewing and training, challenges of remote working and influx of calls. Certain periods may be busier for different call centres (e.g. centre 7 may have changes in packages or price increases, which results in certain time points being busier than others). In addition, the SUH team was unable to set up focus groups with staff from one centre (centre 3) because staff were working from home and using client systems that would not allow them to use the internet or telephone for any other business.
The SUH team would need to find less busy periods for interviews and focus groups by talking to team leaders. They would also need to be flexible and find times that work for staff (e.g. early mornings). One suggested option was to have data collection activities during team meetings if the team leader was comfortable with that. Group sessions are difficult to organise and individual chats may be more practical in some contact centres.
Contact centres have complex environments and systems, and differences between centres can influence programme implementation and success. Some differences between the centres are as follows:
-
Communication. Effective communication and co-ordination between the SUH team and the centres, as well as between individuals and teams within centres, is important and can impact on staff engagement and provision and usage of SUH equipment. In addition, enthusiasm and support from stakeholders can ensure that staff are aware of the programme and feel like they are encouraged to participate. Stakeholders being hands-on with the programme and promoting it among staff (centres 10 and 11) enabled successful implementation. In one centre (centre 6), poor communication led to the removal of equipment owing to safety concerns.
-
SUH committee. Setting up a SUH committee generated ownership among staff, encouraged ideas and aided the implementation of activities. The committee also managed logistical aspects, such as setting up a rota for standing desks and hygiene measures for the equipment. Centres that set up a SUH committee saw more successful implementation.
-
Organisational support. Change at the organisational level can be difficult to create, especially in centres that are more bureaucratic and resistant to change. Rigidity at the organisational level can act as a barrier to programme implementation.
Strengths and limitations of the process evaluation
Strengths
The process evaluation used a mixed-methods approach, utilising both qualitative data, obtained through focus groups and interviews, and quantitative data, which were also analysed as part of the feasibility outcome evaluation. The breadth of objective and subjective data collected, utilising the RE-AIM framework, allowed us to address the aims of the process evaluation robustly and rigorously. A range of views and experiences of SUH delivery, implementation and feasibility of study procedures were collected. This included detailed feedback and suggestions for improving participant recruitment, as well as intervention delivery and engagement, which will be useful for a future full-scale trial.
Using a multicomponent approach in the context of the socioecological model provided a strong foundation for the programme and allowed for ease of programme activity idea generation and implementation. Introducing intervention activities at different levels meant that there was a suitable activity for everyone and led to the recognition that changes at multiple levels supported sustained behaviour and cultural change within the workplace. The adaptive, non-prescriptive nature of the intervention meant that activities and initiatives could be tailored and implemented within the unique context of each contact centre.
The mixed-methods approach to data collection and analysis, as well as the multicomponent approach to the intervention, allowed the research team to address the research questions and continue rolling out the intervention despite the substantial limitations on in-person contact owing to the COVID-19 pandemic, which forced the UK into lockdown in March 2020. Interviews, focus groups and questionnaire data were still collected post lockdown and, as described above, the intervention was adapted to allow for online delivery.
Limitations
Time was a persistent challenge for data collection, workshops, meetings and SUH activity participation. Each of these elements involved staff and/or stakeholder time, which was often scarce and centred around productivity and business needs. Staff found it difficult to get time away from the telephones (or sometimes other tasks) to attend workshops, meetings with the researchers and data collection sessions, as well as to participate in activities during the work day. Future trials should focus on scheduling communication, data collection and other time-intensive elements at the most convenient times for the centre. Encouraging centres to think long term and understand that change takes time, especially at the organisational level, should be another focus. This shift in thinking might offset the view of some centres that they were too busy to participate in certain elements of the intervention and allow them to consider SUH activities in the context of supporting employee well-being and, therefore, improving business in the longer term (e.g. by reducing sickness absence or increasing productivity).
Owing to the intervention’s flexible, multicomponent approach, and in the light of the COVID-19 pandemic, the SUH team were able to adapt the intervention for fully online delivery through offering consults and providing support and ideas for activities that were safe to do during lockdown. The post-lockdown results outline the success of these efforts. Many participants felt that the team did all they could given the difficult circumstances, and participation in activities helped to mitigate some of the negative mental and physical impacts of the pandemic. However, the inability to conduct workshops, host meetings and collect data in person and within the contact centres themselves limited the team’s ability to introduce the intervention and build rapport with stakeholders and staff. It also limited what data collection and recruitment measures could be used, and what programme activities could be carried out owing to home working and social distancing. Although feedback was received from a few centres that participated in the pre-lockdown programme, results related to the use of equipment and other office-based activities are limited. Some centres dropped out during the pandemic, which lessened the pool of staff who were able to participate. These circumstances reduced activity and data collection participation rates, which suggests that the overall impact of the programme, and the evidence to support this, could have been more significant had the team continued with the pre-lockdown project plan.
Summary of findings from the process evaluation
Process evaluation findings are summarised with respect to the acceptability and feasibility of the SUH intervention, and feasibility of study design and procedures:
-
Acceptability and feasibility of the SUH intervention.
The pre-lockdown SUH programme was well received by the centres, with staff and stakeholders reporting several benefits, including a perceived increase in physical activity, reduced sitting, improved morale and mood, and stress reductions. Centres reported that more than 50% of staff participated in at least one SUH activity. Contact centre staff implemented several initiatives at the organisational, environmental, social and individual levels. Staff in many centres also expressed a strong sense of ownership and an increased awareness of the significance of sitting less and moving more during the pre-lockdown programme. Although the programme was still seen as valuable during the post-lockdown period, few or no initiatives were implemented at the organisational and environmental levels. Staff reported that the post-lockdown programme created awareness about sedentary behaviour and physical activity, but they did not feel a strong sense of ownership over the programme.
-
Feasibility of study design and procedures.
Eleven centres were recruited for the study, with participant recruitment on target until the COVID-19 pandemic. Five centres dropped out, with three of these dropping out because of the pandemic. One centre dropped out because their circumstances had changed during the period between recruitment and programme delivery. This is a disadvantage of using the stepped-wedge design, and better communication and measures are required for centres that are randomised to a later time point. Recruitment methods were found to be appropriate both pre and post lockdown, with active engagement from managers aiding recruitment of staff. With respect to data collection instruments, questionnaires were easy to administer and staff had no issues completing them. Uptake of the activPAL device was lower, with some staff not wanting to wear these devices because of concerns relating to appearances and attachment to their skin. Discomfort and irritation were reported by several staff members who wore the activPAL device. In addition, several reported that the logbooks were challenging to complete. The frequency and duration of data collection visits were found to be acceptable for the pre-lockdown visits, and some recommendations for data collection in contact centres are provided in the following sections.
A summary of findings for pre- and post-lockdown periods covering the main elements of the process evaluation framework is provided in Table 9.
| Process evaluation component | Pre lockdown | Post lockdown |
|---|---|---|
| Acceptability and feasibility of the SUH intervention | ||
| Reach: programme significance and appeal |
|
|
| Reach: programme participation |
|
|
| Effectiveness: perceived benefits |
|
|
| Implementation: organisational level | Initiatives included:
|
|
| Implementation: environmental level |
|
|
| Implementation: social level |
|
|
| Implementation: individual level |
|
|
| Implementation: ownership |
|
|
| Implementation: sedentary behaviour and physical activity awareness |
|
|
| Implementation: unintended consequences |
|
|
| Maintenance: budget for SUH/future of SUH |
|
|
| Feasibility of study design and procedures | ||
| Recruitment and randomisation of centres |
|
|
| Centre drop out |
|
|
| Participant recruitment |
|
|
| Participant dropout |
|
|
| Data collection |
|
|
| Data collection logistics |
|
|
Based on the process evaluation findings, the following sections discuss several key recommendations for how researchers could adapt the pre-lockdown and post-lockdown programme and evaluation to increase acceptability, participation and ease of implementation in anticipation of a future trial.
Key recommendations for programme adaptation
-
Set more realistic expectations for the speed of changes to behaviour and implementation of activities and changes at the various levels.
-
Ensure appropriate placement and labelling of, and communication about, equipment for staff.
-
Incorporate or suggest more competition-type activities for staff within and between teams and organisations, and using the website to showcase this.
-
Share results and benefits of the programme, especially at the individual level, to motivate staff.
-
Have a higher amount and variety of communication and advertising measures to create awareness of the programme and check in with staff. This advertising and communication should include information relating to the risks of high rates of sedentary behaviour and low levels of physical activity to emphasise the programme’s importance and increase motivation to participate.
-
Visit the centres more often and at different time points to maximise in-person contact with staff (if possible).
-
Encourage active participation in programme activities from stakeholders and others at the various management levels.
Key recommendations for study evaluation procedures
-
The use of a cluster-randomised stepped-wedge design meant that some centres were randomised to a much later date, which had an impact on their ability to take part. If this study design is used, ensure communication and engagement with all centres during the time gap between expressing interest and participation.
-
Have more and a greater variety of recruitment measures to create awareness of the evaluation.
-
Encourage active participation in recruitment from stakeholders and others at the various management levels using tailored, individualised communication.
-
Work more closely with stakeholders to effectively and flexibly work around staff schedules to maximise opportunities for evaluation participation.
-
Emphasise to participants the importance of completing follow-up measures.
-
If in-person visits are safe (as with the pre-lockdown evaluation), provide more detailed information on activPAL device risks and how to fill out logbooks.
Chapter 4 Feasibility outcome evaluation
Research questions
The feasibility outcome evaluation utilised mainly quantitative methods. Aim 2 of the study was concerned with assessing the feasibility of using a cluster RCT study design. The feasibility outcome evaluation was designed to answer the following research questions:
-
Is the study design (cluster RCT) feasible for a confirmatory trial of an intervention to reduce sedentary behaviour in staff working in contact centres?
-
How many clusters and participants per cluster are required for a confirmatory trial?
-
What is the recruitment rate of participants in each cluster and how many are lost to follow-up (e.g. because of staff turnover)?
-
Are the range of study procedures (e.g. recruitment strategies and outcome measurement tools) feasible for a future confirmatory trial?
-
Are there differences in aspects of study procedures (e.g. uptake) between different contact centres? If so, what are the reasons for these?
-
What are the preliminary estimates of the variability of primary (reduction of sedentary behaviour in the workplace) and secondary outcomes within and between contact centres?
Methods
Study design
The original stepped-wedge study design is shown in Figure 5. Clusters were sites (call centres). The original study design included five sequences (A, B, C, D and E) of at least two clusters each. One of the sequences (A) contained three clusters because there were 11 sites in total. Each ‘step’ in the stepped-wedge design consisted of 3 months, with a total of five periods (i.e. data collection time points). The participants assessed in different periods were expected to be mostly the same people (although we did not prevent new individuals being recruited and assessed at the different time points). For this reason, this stepped-wedge study has an ‘open cohort’ design.
It was planned for data to be collected at a maximum of three visits per site: at the end of the control period and at 3 and 6 months after the end of the intervention. This limited number of data collection visits was in place to minimise cost and participant burden. Participants were also given £5 vouchers each time they participated in data collection to increase response rate.
However, not all data collection visits were completed because of some centres dropping out, and we were unable to continue with the intervention and collect in-person data beyond 20 March 2020 because of the COVID-19 pandemic. Nevertheless, even before the pandemic began in the UK, we experienced difficulties with the stepped-wedge design. In particular, we experienced a difficulty in maintaining contact centre interest and it proved difficult to ensure that data collection took place on schedule. There were also issues with collecting device-measured data from all participants in all centres using accelerometers (e.g. activPAL devices).
The actual stepped-wedge design for the pre-lockdown phase was as shown in Figure 5.
For the pre-lockdown questionnaire analysis, there were six centres involved that belonged to three different randomised sequences (A, B and C). These sequences are described as follows:
-
sequence A – started the intervention in July 2019 and had data collected at the 6-month follow-up (no within-site control group comparison) (site numbers 2 and 11 in Figure 5)
-
sequence B – started the intervention in October 2019 with baseline data collected only (sites 3 and 10 in Figure 5)
-
sequence C – started the intervention in January 2020 with baseline data collected only (sites 1 and 6 in Figure 5).
The concurrent cross-sectional comparison involves comparison between sequence A and sequence C only, for which data were collected at a similar time (approximately January 2020). Sites in sequence B had baseline (control) data collection 3 months previously in October 2019.
Owing to the COVID-19 pandemic and associated lockdown restrictions, we changed the design of our trial after March 2020 to include a simple before-and-after comparison. In the post-lockdown phase, questionnaire data were collected in participants at baseline and 3 months later (see Figure 5).
There were five centres involved in the post-lockdown data analysis. The aim was to collect questionnaire data in participants at baseline and at the 3-month follow-up. However, although a total of 51 participants completed at least some information at baseline or follow-up, only 25 participants provided questionnaire outcome responses at both baseline and the 3-month follow-up.
Intervention and control conditions
The intervention is an adaptive theory-based complex intervention called SUH (full details are provided in Chapter 1). The intervention was delivered once in each phase (pre lockdown and post lockdown) at the level of the contact centre, with data collected at both the contact centre and individual levels. Participants recruited were employees of the contact centres, including managers, supervisors and call operators in Scotland and England (primarily in the north of England).
Under the control condition, no component of the SUH intervention was delivered.
Outcomes
The primary outcome in a definitive trial was the activPAL device-measured sedentary time in the workplace, measured over a continuous 7-day period. This will be referred to as the primary outcome for the remainder of this report. 67
Secondary outcomes included:
-
subjectively measured sedentary time in the workplace, as measured by the Occupational Sitting and Physical Activity Questionnaire (OSPAQ)81
-
activPAL device-measured () prolonged sitting time in the workplace (bouts of ≥ 30 minutes)
-
activPAL device-measured total sedentary time (i.e. including time outside the workplace, such as at home and leisure time)
-
activPAL device-measured workplace and total standing time
-
activPAL device-measured workplace and total physical activity (based on stepping)
-
activPAL device-measured workplace and total sit-to-stand transitions
-
Utrecht Work Engagement Scale (UWES)82
-
mental well-being, as measured by the Warwick–Edinburgh Mental Well-being Scale (WEMWBS)59
-
musculoskeletal health, as measured by the Musculoskeletal Health Questionnaire (MSK-HQ)83
-
Scottish Physical Activity Screening Question (PASQ)84
-
activities questionnaires to measure use of activities and preference
-
staff turnover – number of people leaving and number of new joiners over the study period.
Participant sampling and recruitment
Pre-lockdown sampling and recruitment
For the pre-lockdown programme, Divya Sivaramakrishnan and Jillian Manner co-ordinated with centre stakeholders to recruit participants. Convenience sampling was used to recruit participants across all centres. Recruitment posters were displayed at centres, and the SUH team created a recruitment video to be played during team meetings at the contact centres and circulated among staff members. In addition, Jillian Manner and Divya Sivaramakrishnan made a recruitment visit to two centres (centres 3 and 10) at which they set up a table, spoke to staff members about the study and distributed the participant information sheet. All staff of working age (i.e. ≥ 16 years) in the participating contact centres had the opportunity to take part, provided that they satisfied the following two inclusion criteria:
-
provisionally scheduled to work during the 7 days of data collection of the primary behavioural outcome measure (activPAL activity monitor), aside from scheduled non-work days
-
not planning to leave the company in the 3 months after recruitment.
Post-lockdown sampling and recruitment
Convenience sampling was used to recruit participants across all centres. For centres 3, 7 and 10, Jillian Manner and Divya Sivaramakrishnan co-ordinated with the centre stakeholder to schedule a 30-minute consult with staff members. In centre 6, the SUH team set up a Doodle poll on which staff could select a time when they were free for a consult. In centre 11, a survey version of the consults was circulated to staff members (along with information sheet and consent form). Contact centre staff were sent an online version of the questionnaire immediately after the consults and at 3 months after the consults.
Data collection and outcome measures
Given that this is a feasibility study, we tested out the methods of collecting data on outcomes, as well as preliminary estimates of effectiveness. Table 10 outlines the methods/instruments used.
| Outcomes | Measurement |
|---|---|
| Primary | |
| Sedentary time in the workplace (device measured) | The activPAL monitor is a small, thigh-worn device for assessing posture and is the preferred measurement instrument for assessing changes in occupational sitting.85,86 Participants wear the device continuously for 7 days (during waking/sleeping hours and water-based activity) to provide adequate reliability.86,87 Following recommended procedures,87 we isolated and determined changes in accumulated sedentary time while at work as our primary outcome86,87 |
| Sedentary time in the workplace (subjectively measured) | The OSPAQ was used as a secondary measure given the favourable validity and reliability properties of this instrument85,86 |
| Sedentary behaviour (overall) | The activPAL device was used to assess changes in:
|
| Physical activity | Physical activity was assessed using both objective and subjective instruments:
|
| Productivity |
Objective measures of productivity include absenteeism, presenteeism, call handling time, time spent talking, time spent on hold, time spent wrapping up a call, attendance or sick leave. These were considered in the economic scoping exercise (see Model-scoping exercise) Subjective measures were assessed using the Utrecht Work Engagement Scale and other measures in similar studies82,87 |
| Mental well-being | WEMWBS88 |
| Musculoskeletal health | MSK-HQ |
| Activities | Questionnaires developed by the researchers to measure use and preference |
We also collected data on demographics, such as age, sex and any medical conditions, that may impact on sedentary behaviour.
Data collection instrumentation and procedures
The activPAL device and logbooks
To capture work and sleep times of contact centre staff, the SUH team designed logbooks to accompany the activPAL device. The logbooks were designed by Jillian Manner, Divya Sivaramakrishnan and Richard Parker. Table 11 describes the content and data collected using the logbooks.
| Logbook section | Details |
|---|---|
| Instructions for participants | This section included instructions on how long they have to wear the activPAL device, what to do in case of skin irritation, how to reattach the activPAL device if it gets detached and how to complete the logbook |
| Work and sleep times | This section is to record work and sleep times for each of the 7 days that a participant wore the activPAL device |
| Information on detachment and additional comments | This section is to record whether or not the activPAL device became detached and reasons for detachment. There was also an open-ended question to record any other comments related to wearing the activPAL device, as well as sleep and physical activity patterns over the 7 days |
| Researcher contact information | The logbook contained an e-mail and a mobile number for participants to contact the SUH team if they had any questions or issues pertaining to the activPAL device and logbook |
Participants received a pack consisting of an activPAL device, a logbook, two alcohol wipes and two Tegarderm™ (3M™, Bracknell, UK) strips. During pre-lockdown data collection, Jillian Manner and Divya Sivaramakrishnan visited the centres and explained how to attach the activPAL device to staff members. They also attached the activPAL device for participants who requested help. The pack contained an additional alcohol wipe and Tegaderm for participants to reattach the activPAL device in case it became detached.
The activPAL processing and analysis
The activPAL devices were plugged into the researcher’s desktop computers, and the data were downloaded using activPAL3 (PAL Technologies Ltd, Glasgow, UK) software and then exported as Microsoft Excel files. The data were anonymised and provided to the project statistician, who used the ‘activpalProcessing’ package in R software to process the data (The R Foundation for Statistical Computing, Vienna, Austria). 89 We required the logbook work and/or sleep time sections to be completed (indicating participants were working) for each participant for a particular day, plus at least some valid sedentary time/activity data recorded via the activPAL device. We included all data where possible, but as a minimum we required an indication of when participants started and ended work on a particular day.
Questionnaires
Divya Sivaramakrishnan and Jillian Manner created an online questionnaire (paper version provided as supplementary material; see Report Supplementary Material 5 for pre-lockdown questionnaire and Report Supplementary Material 6 for post-lockdown questionnaire) on Qualtrics consisting of:
-
demographic questions
-
OSPAQ
-
Utrecht Work Engagement Scale
-
WEMWBS
-
MSK-HQ
-
Scottish PASQ
-
activity preferences.
During the data collection visits to the centres, participants were asked to complete the questionnaires on tablets provided by the SUH team. Paper questionnaires were used if the tablet malfunctioned or if there were internet issues.
Divya Sivaramakrishnan and Jillian Manner visited the centres for pre-lockdown data collection. Information sheets (see Report Supplementary Material 7) were distributed and informed consent procured (see Report Supplementary Material 8) prior to collecting the activPAL device and questionnaire data. Post-lockdown data collection included questionnaires only. Participants received an online version of the information sheets and online consent was procured before data collection.
Progression criteria
In the original study protocol,67 we reported that we could proceed to a future larger study if the following criteria were satisfied:
-
The 95% CIs for the primary outcome include a clinically relevant reduction in sedentary time of 45 minutes per day or greater in favour of the intervention. This would reflect substantial progression towards accumulating the recommended quantity of 2 hours per day standing/light activity during working hours55 for employees in predominantly desk-based occupations.
-
Intervention successfully delivered in at least five of the sites within the study period, if at least one person in each site was able to use/experience at least one activity.
-
At least 10% of employees at a site being able to use/experience at least one of the intervention activities in the sites at which the intervention was successfully delivered.
-
Primary and secondary outcome data being collected for at least 75% of participants overall.
-
Contamination between sites being low or else it being envisaged that contamination can be addressed in the study design of a future study.
-
It being feasible that any practical difficulties in delivering the intervention across multiple sites or in measuring effectiveness can be overcome when conducting a future large-scale study.
Statistical analysis and results
Introduction
The statistician was blind to the allocation of the contact centres. The analysis and presentation of results adhered to Consolidated Standards of Reporting Trials (CONSORT) guidance,90 and a statistical analysis plan. 67 A stepped-wedge version of the CONSORT checklist was added as a supplementary file (see Report Supplementary Material 9). The analyses were all exploratory to investigate if it is feasible to fit such a model in a future trial.
The quantitative analyses were stratified according to whether data were collected before or after the UK lockdown measures were introduced because of the COVID-19 pandemic. In what follows, we distinguish between pre-lockdown analyses/results and post-lockdown analyses/results. The ‘post-lockdown’ phase refers to any data collected after the lockdown measures began in March 2020, whereas ‘pre lockdown’ refers to data collected prior to March 2020. Our study design and pre-specified statistical analysis plan has already been described in detail in an open access publication. 67 However, we had to make changes to the planned statistical analysis plan owing to the impact of the COVID-19 pandemic.
A total of 155 individuals were recruited pre lockdown and 70 individuals were recruited post lockdown for the feasibility outcome evaluation.
The CONSORT flow diagram
A CONSORT flow diagram is shown for the pre-lockdown phase in Figures 6 and 7, and for the post-lockdown phase in Figure 8.
FIGURE 6.
The CONSORT flow diagram (pre-lockdown phase).
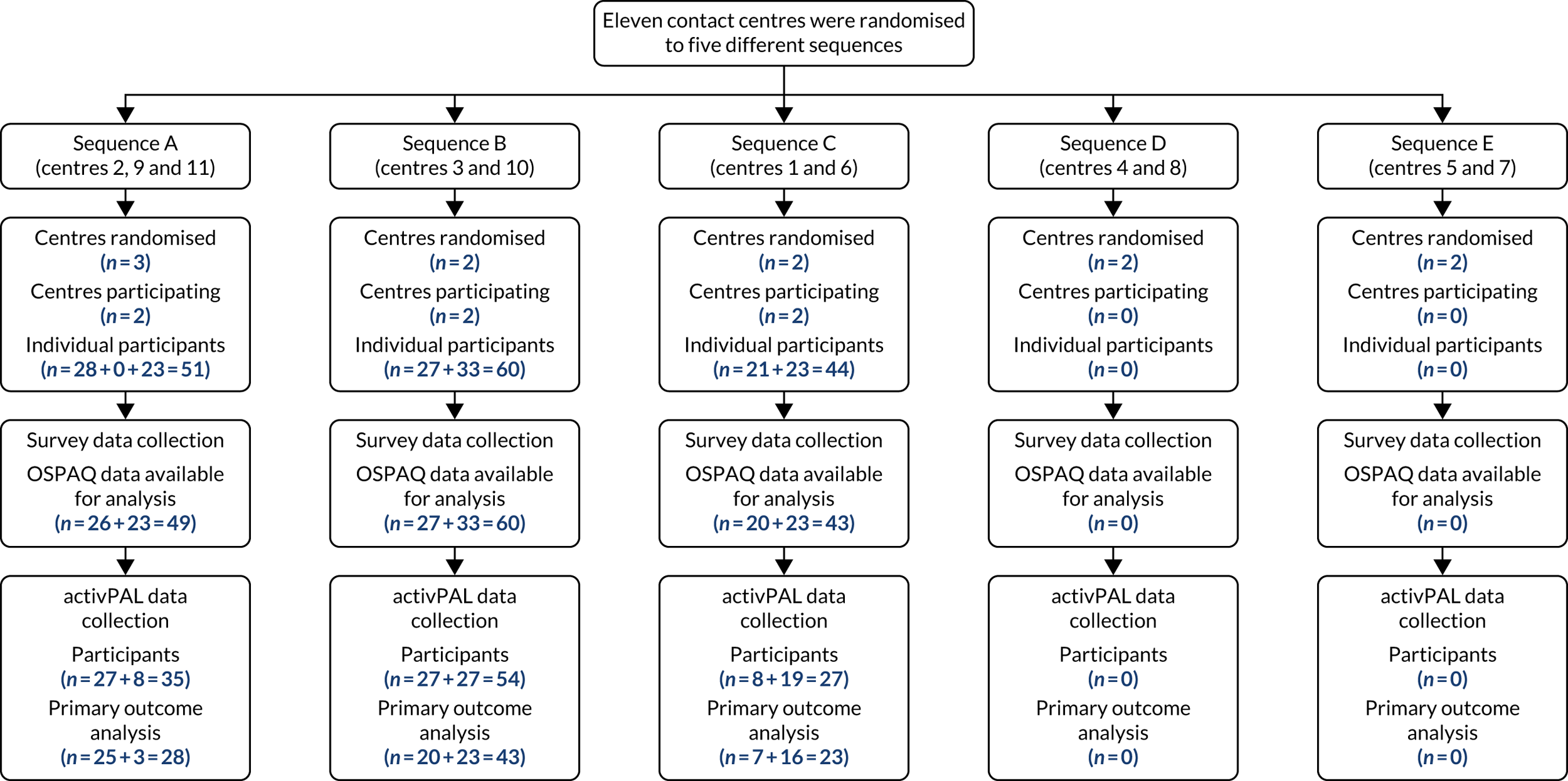
FIGURE 7.
The CONSORT flow diagram: non-participation and missing primary outcome data (pre-lockdown phase).
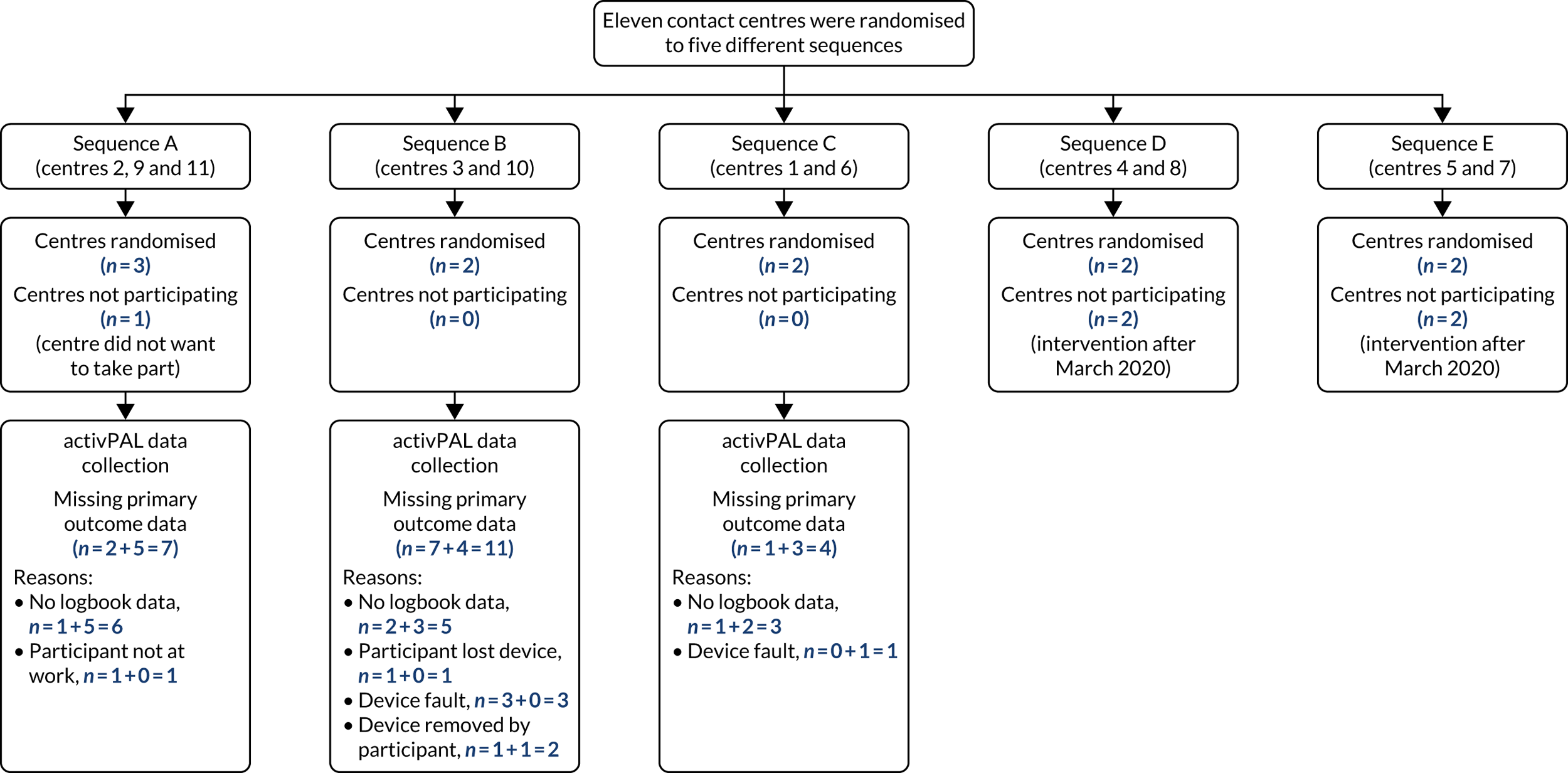
FIGURE 8.
The CONSORT flow diagram (post-lockdown phase).
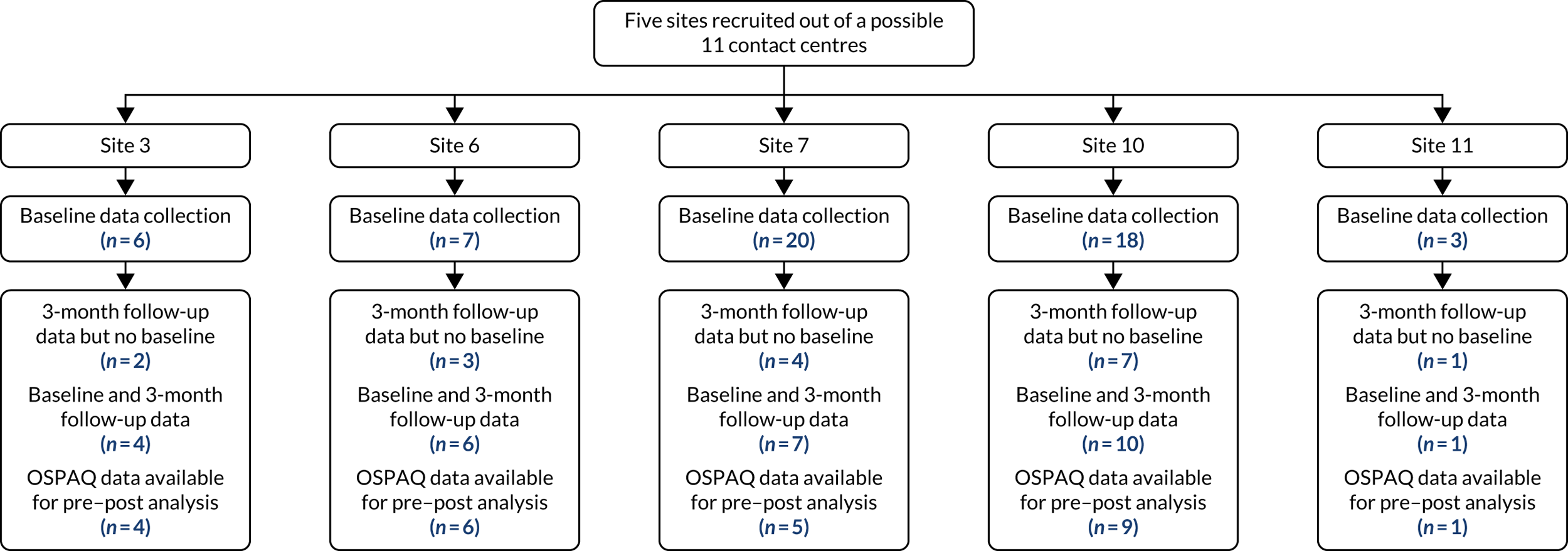
Any missing values for the questionnaire data analysis at baseline were because of incomplete responses. Not everyone who completed the questionnaires used the activPAL devices. For the primary outcome analysis (based on the activPAL data), reasons for missing data included failure to complete logbooks (recording time spent at work and sleeping), incomplete logbooks or failure to extract valid data from the system (perhaps because of device faults or the way that the activPAL device was attached) (see Figure 7).
Baseline demographics
Participant demographic details (age, sex, job title, employment type, length of time working at the contact centre, any health problems reported) were summarised using descriptive statistics. Table 12 shows the baseline demographic information for participants recruited in the pre-lockdown data collection period, split by sequence (see Report Supplementary Material 10, Table S10.1, for the same table but split by contact centre). In total, 154 out of 155 participants recorded at least some demographic information pre lockdown, whereas this information was complete for 150 participants.
| Demographic | Sequence, n (%) | Total, n (%) | ||
|---|---|---|---|---|
| A | B | C | ||
| Age (years) (N = 153) | ||||
| 18–24 | 3 (6.0) | 3 (5.1) | 8 (18.2) | 14 (9.2) |
| 25–34 | 13 (26.0) | 25 (42.4) | 13 (29.5) | 51 (33.3) |
| 35–44 | 15 (30.0) | 17 (28.8) | 10 (22.7) | 42 (27.5) |
| 45–54 | 10 (20.0) | 9 (15.3) | 8 (18.2) | 27 (17.6) |
| 55–64 | 8 (16.0) | 4 (6.8) | 4 (9.1) | 16 (10.5) |
| > 65 | 1 (2.0) | 1 (1.7) | 1 (2.3) | 3 (2.0) |
| Sex (N = 153) | ||||
| Male | 13 (26.0) | 21 (35.6) | 18 (40.9) | 52 (34.0) |
| Female | 37 (74.0) | 38 (64.4) | 26 (59.1) | 101 (66.0) |
| Job title (N = 151) | ||||
| Call handler/customer services advisor | 27 (54.0) | 38 (64.4) | 12 (28.6) | 77 (51.0) |
| Supervisor/manager/team leader | 13 (26.0) | 14 (23.7) | 10 (23.8) | 37 (24.5) |
| Other | 10 (20.0) | 7 (11.9) | 20 (47.6) | 37 (24.5) |
| Employment type (N = 151) | ||||
| Full time | 35 (71.4) | 48 (81.4) | 28 (65.1) | 111 (73.5) |
| Part time | 14 (28.6) | 11 (18.6) | 15 (34.9) | 40 (26.5) |
| How long have you been working for this contact centre? (N = 154) | ||||
| < 3 months | 4 (8.0) | 3 (5.0) | 0 (0.0) | 7 (4.5) |
| 3–6 months | 3 (6.0) | 3 (5.0) | 1 (2.3) | 7 (4.5) |
| 6–12 months | 1 (2.0) | 6 (10.0) | 7 (15.9) | 14 (9.1) |
| 1–2 years | 4 (8.0) | 7 (11.7) | 8 (18.2) | 19 (12.3) |
| 2–3 years | 3 (6.0) | 12 (20.0) | 5 (11.4) | 20 (13.0) |
| > 3 years | 35 (70.0) | 29 (48.3) | 23 (52.3) | 87 (56.5) |
| Health problems reported that may prevent participant from standing and moving more at work (N = 154) | ||||
| No | 43 (86.0) | 55 (91.7) | 36 (81.8) | 134 (87.0) |
| Yes | 7 (13.7) | 5 (8.3) | 8 (18.2) | 20 (12.9) |
Sites in sequence A (intervention sites) had slightly older participants, on average, with a higher proportion of females and people working in the company for more than 3 years than sequence C (concurrent control sites). None of the participants had previously worked for a company that used the SUH intervention.
There were five centres involved in the post-lockdown data analysis in a before-and-after study design. Questionnaire data were collected from participants at baseline and at the 3-month follow-up.
Participant demographic details (age, sex, job title, employment type, length of time working at the contact centre, any health problems reported) were summarised using descriptive statistics split by contact centre. Although 51 participants completed at least some information at baseline or follow-up, only 25 provided questionnaire outcome responses at both baseline and the 3-month follow-up. Therefore, the baseline descriptive statistics were also computed for the subset of 25 participants providing outcome responses at both baseline and the 3-month follow-up (henceforth called the ‘adherent participants’). Table 13 shows baseline data for all adherent participants involved in post-lockdown data collection (n = 25). Baseline data for all participants recording baseline data in the post-lockdown phase (n = 51) can be found in Report Supplementary Material 10 (see Table S10.2).
| Demographic | Centre, n (%) | Total, n (%) | ||||
|---|---|---|---|---|---|---|
| 3 | 6 | 7 | 10 | 11 | ||
| Age (years) | ||||||
| 18–24 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (11.1) | 0 (0.0) | 1 (4.0) |
| 25–34 | 1 (25.0) | 0 (0.0) | 4 (80.0) | 0 (0.0) | 0 (0.0) | 5 (20.0) |
| 35–44 | 2 (50.0) | 4 (66.7) | 1 (20.0) | 5 (55.6) | 0 (0.0) | 12 (48.0) |
| 45–54 | 1 (25.0) | 1 (16.7) | 0 (0.0) | 2 (22.2) | 0 (0.0) | 4 (16.0) |
| 55–64 | 0 (0.0) | 1 (16.7) | 0 (0.0) | 1 (11.1) | 1 (100.0) | 3 (12.0) |
| > 65 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Sex | ||||||
| Male | 2 (50.0) | 2 (33.3) | 3 (60.0) | 1 (11.1) | 0 (0.0) | 8 (32.0) |
| Female | 2 (50.0) | 4 (66.7) | 2 (40.0) | 8 (88.9) | 1 (100.0) | 17 (68.0) |
| Job title | ||||||
| Call handler/customer services advisor | 2 (50.0) | 2 (33.3) | 5 (100.0) | 9 (100.0) | 1 (100.0) | 19 (76.0) |
| Supervisor/manager/team leader | 2 (50.0) | 2 (33.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 4 (16.0) |
| Other | 0 (0.0) | 2 (33.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (8.0) |
| Employment type | ||||||
| Full time | 4 (100.0) | 4 (66.7) | 5 (100.0) | 7 (77.8) | 0 (0.0) | 20 (80.0) |
| Part time | 0 (0.0) | 2 (33.3) | 0 (0.0) | 2 (22.2) | 1 (100.0) | 5 (20.0) |
| How long have you been working for this contact centre? | ||||||
| < 3 months | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| 3–6 months | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| 6–12 months | 3 (75.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 3 (12.0) |
| 1–2 years | 0 (0.0) | 0 (0.0) | 2 (40.0) | 1 (11.1) | 1 (100.0) | 4 (16.0) |
| 2–3 years | 0 (0.0) | 1 (16.7) | 0 (0.0) | 2 (22.2) | 0 (0.0) | 3 (12.0) |
| > 3 years | 1 (25.0) | 5 (83.3) | 3 (60.0) | 6 (66.7) | 0 (0.0) | 15 (60.0) |
| Health problems reported that may prevent participant from standing and moving more at work | ||||||
| No | 3 (75.0) | 6 (100.0) | 2 (40.0) | 8 (88.9) | 1 (100.0) | 20 (80.0) |
| Yes | 1 (25.0) | 0 (0.0) | 3 (60.0) | 1 (11.1) | 0 (0.0) | 5 (20.0) |
Descriptive statistics of outcome data
The device-measured activPAL outcome data and continuous participant self-reported outcomes recorded at baseline or the 6-month follow-up were summarised using descriptive statistics [mean, median, standard deviation (SD), minimum, maximum, interquartile range] and box plots split by sequence.
The purpose of this analysis was to help answer research question 6:
-
What are the preliminary estimates of the variability of primary and secondary outcomes within and between contact centres?
Table 14 shows descriptive statistics for the primary outcome (device-measured sedentary time per day in the workplace) and all secondary outcomes for the pre-lockdown analysis, stratified by sequence. The anonymised data sets for the secondary outcomes (questionnaire data) collected pre and post lockdown have been uploaded into a University of Edinburgh repository. 91
| Sequence | n | Missing (n) | Mean | Median | SD | Minimum | Maximum | Lower quartile | Upper quartile |
|---|---|---|---|---|---|---|---|---|---|
| activPAL | |||||||||
| Sedentary time per day in the workplace (minutes) | |||||||||
| A | 28 | 1 | 367.5 | 365.8 | 103.6 | 117.8 | 541.1 | 288.1 | 441.6 |
| B | 43 | 1 | 379.5 | 386.2 | 103.1 | 158.7 | 659.2 | 321.2 | 440.7 |
| C | 23 | 0 | 322.5 | 325.5 | 89.7 | 134.0 | 461.6 | 256.0 | 383.2 |
| Sedentary time per day while awake (minutes) | |||||||||
| A | 28 | 1 | 676.0 | 660.2 | 108.8 | 419.0 | 910.0 | 609.7 | 767.9 |
| B | 41 | 3 | 658.8 | 651.6 | 127.6 | 334.4 | 892.7 | 600.8 | 753.1 |
| C | 22 | 1 | 612.9 | 602.6 | 90.8 | 483.4 | 783.3 | 523.2 | 675.3 |
| Prolonged sitting time over 30 minutes in the workplace (minutes) | |||||||||
| A | 28 | 1 | 203.9 | 197.3 | 91.0 | 46.7 | 396.9 | 130.5 | 286.1 |
| B | 43 | 1 | 205.7 | 204.5 | 110.6 | 0.0 | 446.9 | 114.5 | 273.3 |
| C | 23 | 0 | 220.5 | 237.6 | 87.5 | 11.7 | 329.9 | 152.5 | 285.8 |
| Prolonged sitting time over 30 minutes while awake (minutes) | |||||||||
| A | 28 | 1 | 408.6 | 385.1 | 104.5 | 241.0 | 646.0 | 337.0 | 491.0 |
| B | 41 | 3 | 377.7 | 374.4 | 123.3 | 87.7 | 679.8 | 287.9 | 469.7 |
| C | 22 | 1 | 370.8 | 350.9 | 118.8 | 167.2 | 665.7 | 302.7 | 459.8 |
| Standing time in the workplace (minutes) | |||||||||
| A | 27 | 2 | 100.7 | 76.1 | 79.8 | 18.5 | 396.1 | 63.6 | 111.0 |
| B | 43 | 1 | 96.6 | 66.1 | 84.8 | 18.3 | 380.0 | 42.3 | 108.6 |
| C | 22 | 1 | 64.3 | 42.7 | 69.5 | 3.7 | 316.6 | 20.9 | 88.4 |
| Standing time while awake (minutes) | |||||||||
| A | 25 | 4 | 193.2 | 187.1 | 73.9 | 83.0 | 394.0 | 131.7 | 245.4 |
| B | 36 | 8 | 175.7 | 164.7 | 81.3 | 63.8 | 420.8 | 111.1 | 221.5 |
| C | 21 | 2 | 201.0 | 199.3 | 69.4 | 61.5 | 336.3 | 145.2 | 257.7 |
| Stepping time in the workplace (minutes) | |||||||||
| A | 26 | 3 | 36.9 | 29.5 | 23.1 | 12.0 | 99.0 | 18.9 | 47.7 |
| B | 43 | 1 | 28.9 | 21.4 | 23.2 | 9.5 | 137.1 | 15.9 | 31.0 |
| C | 20 | 3 | 24.9 | 24.4 | 13.2 | 7.0 | 60.6 | 15.7 | 35.3 |
| Stepping time while awake (minutes) | |||||||||
| A | 25 | 4 | 82.7 | 78.9 | 34.7 | 33.0 | 171.0 | 56.5 | 105.9 |
| B | 35 | 9 | 79.8 | 72.5 | 35.8 | 13.8 | 179.1 | 53.6 | 100.8 |
| C | 21 | 2 | 99.9 | 87.8 | 46.0 | 45.1 | 210.2 | 66.8 | 137.9 |
| Light-intensity activity time in the workplace (minutes) | |||||||||
| A | 26 | 3 | 36.9 | 29.5 | 23.1 | 12.0 | 99.0 | 18.9 | 47.7 |
| B | 43 | 1 | 28.9 | 21.4 | 23.2 | 9.5 | 137.1 | 15.9 | 31.0 |
| C | 20 | 3 | 24.9 | 24.4 | 13.2 | 7.0 | 60.6 | 15.7 | 35.3 |
| Light-intensity activity while awake (minutes) | |||||||||
| A | 25 | 4 | 82.7 | 78.9 | 34.7 | 33.0 | 171.0 | 56.5 | 105.9 |
| B | 35 | 9 | 79.8 | 72.5 | 35.8 | 13.8 | 179.1 | 53.6 | 100.8 |
| C | 21 | 2 | 99.9 | 87.8 | 46.0 | 45.1 | 210.2 | 66.8 | 137.9 |
| Sit-to-stand transitions in the workplace (minutes) | |||||||||
| A | 26 | 3 | 25.1 | 20.8 | 12.4 | 13.0 | 64.0 | 15.6 | 31.0 |
| B | 43 | 1 | 28.3 | 26.4 | 10.5 | 11.0 | 52.3 | 20.8 | 36.2 |
| C | 22 | 1 | 16.5 | 15.8 | 8.6 | 5.5 | 38.2 | 8.8 | 20.8 |
| Sit-to-stand transitions while awake (minutes) | |||||||||
| A | 24 | 5 | 46.6 | 45.9 | 12.3 | 24.0 | 73.0 | 36.7 | 54.8 |
| B | 36 | 8 | 48.1 | 49.3 | 12.8 | 20.0 | 83.2 | 38.2 | 55.9 |
| C | 21 | 2 | 53.4 | 45.7 | 36.7 | 20.6 | 192.4 | 32.1 | 60.2 |
| OSPAQ | |||||||||
| Hours sitting at work per week | |||||||||
| A | 49 | 2 | 32.3 | 29.6 | 15.5 | 7.2 | 72.0 | 21.0 | 42.0 |
| B | 60 | 0 | 26.6 | 27.0 | 8.5 | 4.8 | 39.2 | 21.6 | 33.6 |
| C | 43 | 1 | 24.6 | 25.2 | 7.5 | 6.0 | 37.2 | 21.0 | 31.2 |
| Minutes sitting at work per day | |||||||||
| A | 49 | 2 | 417.5 | 421.1 | 180.4 | 96.0 | 720.0 | 265.2 | 576.0 |
| B | 60 | 0 | 343.0 | 360.0 | 96.0 | 135.0 | 540.0 | 266.4 | 422.1 |
| C | 43 | 1 | 330.1 | 329.3 | 62.9 | 154.0 | 446.0 | 294.0 | 378.0 |
| WEMWBS | |||||||||
| Total score | |||||||||
| A | 50 | 1 | 47.8 | 48.0 | 8.3 | 30.0 | 70.0 | 42.0 | 53.3 |
| B | 60 | 0 | 49.1 | 50.5 | 7.5 | 28.0 | 64.0 | 44.0 | 54.0 |
| C | 44 | 0 | 49.5 | 50.0 | 7.3 | 34.0 | 67.0 | 44.0 | 54.0 |
| UWES | |||||||||
| Total score | |||||||||
| A | 50 | 1 | 4.1 | 4.2 | 1.0 | 1.4 | 6.2 | 3.6 | 4.8 |
| B | 60 | 0 | 4.9 | 5.0 | 0.9 | 2.4 | 6.7 | 4.4 | 5.6 |
| C | 43 | 1 | 4.8 | 4.7 | 0.9 | 2.5 | 6.5 | 4.4 | 5.6 |
| Vigour | |||||||||
| A | 50 | 1 | 4.3 | 4.3 | 1.0 | 1.7 | 6.7 | 3.8 | 5.0 |
| B | 60 | 0 | 5.0 | 5.2 | 0.9 | 2.7 | 6.7 | 4.4 | 5.8 |
| C | 43 | 1 | 4.8 | 5.0 | 0.9 | 2.2 | 6.5 | 4.2 | 5.5 |
| Dedication | |||||||||
| A | 51 | 0 | 4.4 | 4.4 | 1.2 | 1.2 | 6.8 | 4.0 | 5.2 |
| B | 60 | 0 | 5.0 | 5.0 | 1.2 | 1.0 | 7.0 | 5.1 | 6.0 |
| C | 44 | 0 | 5.1 | 5.1 | 1.2 | 1.4 | 7.0 | 4.4 | 5.8 |
| Absorption | |||||||||
| A | 50 | 1 | 3.8 | 3.8 | 1.0 | 1.2 | 6.2 | 3.1 | 4.3 |
| B | 60 | 0 | 4.8 | 4.8 | 1.0 | 1.5 | 7.0 | 4.2 | 5.3 |
| C | 44 | 0 | 4.5 | 4.6 | 1.0 | 2.2 | 6.5 | 4.0 | 5.0 |
| MSK-HQ | |||||||||
| Total score | |||||||||
| A | 42 | 9 | 28.1 | 25.0 | 12.0 | 14.0 | 55.0 | 17.0 | 40.3 |
| B | 58 | 2 | 25.5 | 23.5 | 10.6 | 14.0 | 61.0 | 17.0 | 28.0 |
| C | 35 | 9 | 25.9 | 26.0 | 10.9 | 14.0 | 53.0 | 14.0 | 16.0 |
For the adherent participants in the post-lockdown phase, descriptive statistics (mean, median, SD, minimum, maximum and interquartile range) were computed for the subjective continuous questionnaire outcomes split by time point (baseline or 3-month follow-up) for comparison (Table 15).
| Outcome | n | Missing (n) | Mean | Median | SD | Minimum | Maximum | Lower quartile | Upper quartile |
|---|---|---|---|---|---|---|---|---|---|
| OSPAQ | |||||||||
| Hours sitting at work per week | |||||||||
| Baseline | 25 | 0 | 28.96 | 30.36 | 10.24 | 5.00 | 49.50 | 24.40 | 35.27 |
| 3-month follow-up | 25 | 0 | 29.43 | 30.40 | 10.61 | 7.20 | 47.00 | 21.40 | 36.90 |
| Minutes sitting at work per working day | |||||||||
| Baseline | 24 | 1 | 379.51 | 368.16 | 101.70 | 60.00 | 594.00 | 338.55 | 445.23 |
| 3-month follow-up | 23 | 2 | 394.20 | 403.20 | 78.62 | 180.00 | 552.00 | 352.44 | 432.00 |
| WEMWBS | |||||||||
| Total score | |||||||||
| Baseline | 25 | 0 | 44.00 | 44.00 | 6.76 | 32.00 | 56.00 | 38.50 | 50.50 |
| 3-month follow-up | 25 | 0 | 43.60 | 42.00 | 7.89 | 32.00 | 68.00 | 38.00 | 48.50 |
| UWES | |||||||||
| Total score | |||||||||
| Baseline | 25 | 0 | 4.56 | 4.71 | 0.72 | 2.88 | 5.65 | 4.15 | 5.03 |
| 3-month follow-up | 23 | 2 | 4.57 | 4.53 | 1.02 | 2.47 | 6.76 | 4.18 | 5.12 |
| Vigour | |||||||||
| Baseline | 25 | 0 | 4.59 | 4.67 | 0.67 | 3.67 | 6.33 | 4.08 | 5.08 |
| 3-month follow-up | 24 | 1 | 4.60 | 4.50 | 0.92 | 3.00 | 6.83 | 4.04 | 4.96 |
| Dedication | |||||||||
| Baseline | 25 | 0 | 4.62 | 4.60 | 1.16 | 1.60 | 6.40 | 3.80 | 5.40 |
| 3-month follow-up | 25 | 0 | 4.71 | 4.80 | 1.22 | 2.00 | 6.80 | 3.90 | 5.60 |
| Absorption | |||||||||
| Baseline | 25 | 0 | 4.48 | 4.67 | 0.90 | 2.67 | 6.00 | 3.83 | 5.08 |
| 3-month follow-up | 24 | 1 | 4.39 | 4.33 | 1.08 | 1.83 | 6.67 | 4.04 | 4.96 |
| MSK-HQ | |||||||||
| Total score | |||||||||
| Baseline | 25 | 0 | 26.96 | 26.00 | 9.06 | 14.00 | 49.00 | 19.00 | 34.00 |
| 3-month follow-up | 23 | 2 | 24.83 | 25.00 | 6.84 | 15.00 | 41.00 | 19.00 | 30.00 |
Simple statistical and graphical analyses of outcome data
Pre-lockdown phase
Figures 9 and 10 show box plots of the primary outcome (sedentary time per day in the workplace measured by the activPAL device), stratified by centre and sequence, respectively, for the pre-lockdown phase.
FIGURE 9.
Box plot of primary outcome (sedentary time in the workplace, as measured by the activPAL device), stratified by centre, in the pre-lockdown phase.
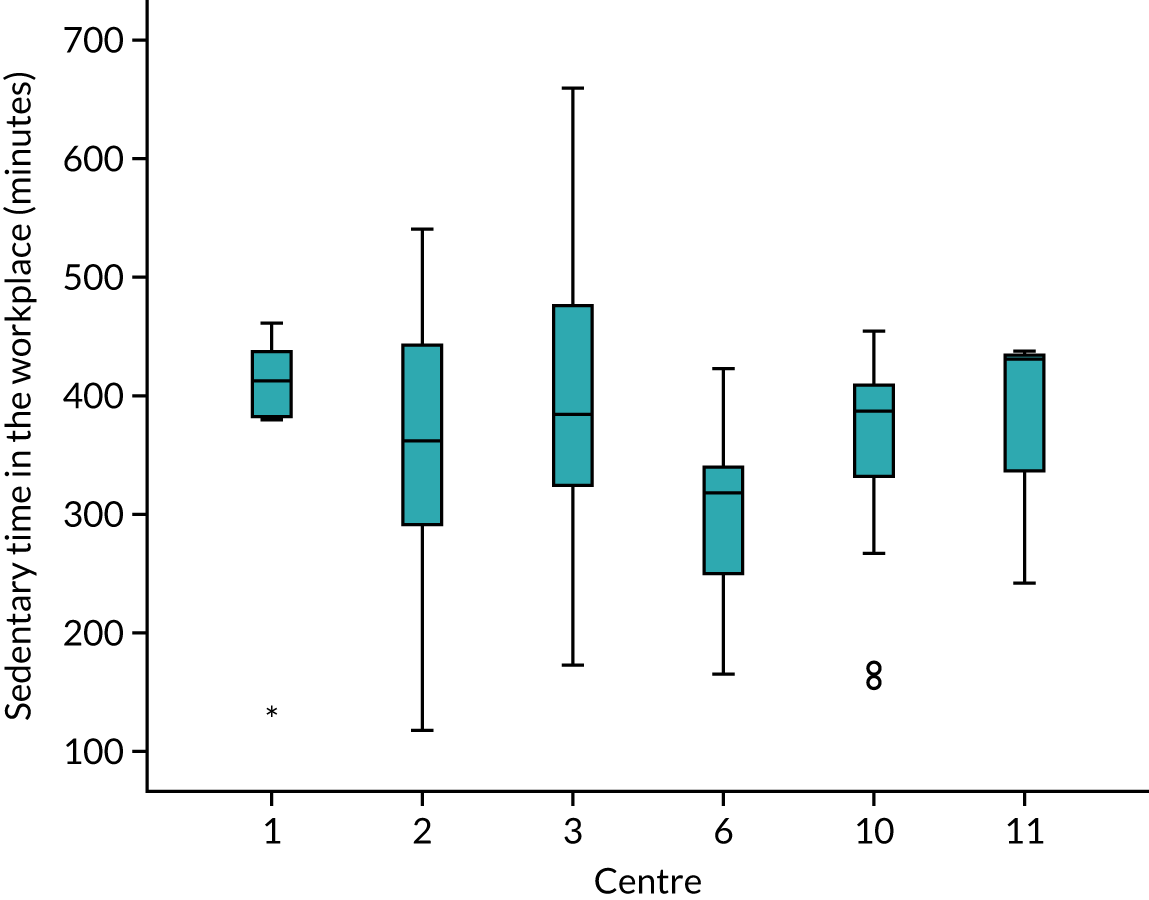
FIGURE 10.
Box plot of primary outcome (sedentary time in the workplace as measured by the activPAL device), stratified by sequence, in the pre-lockdown phase.
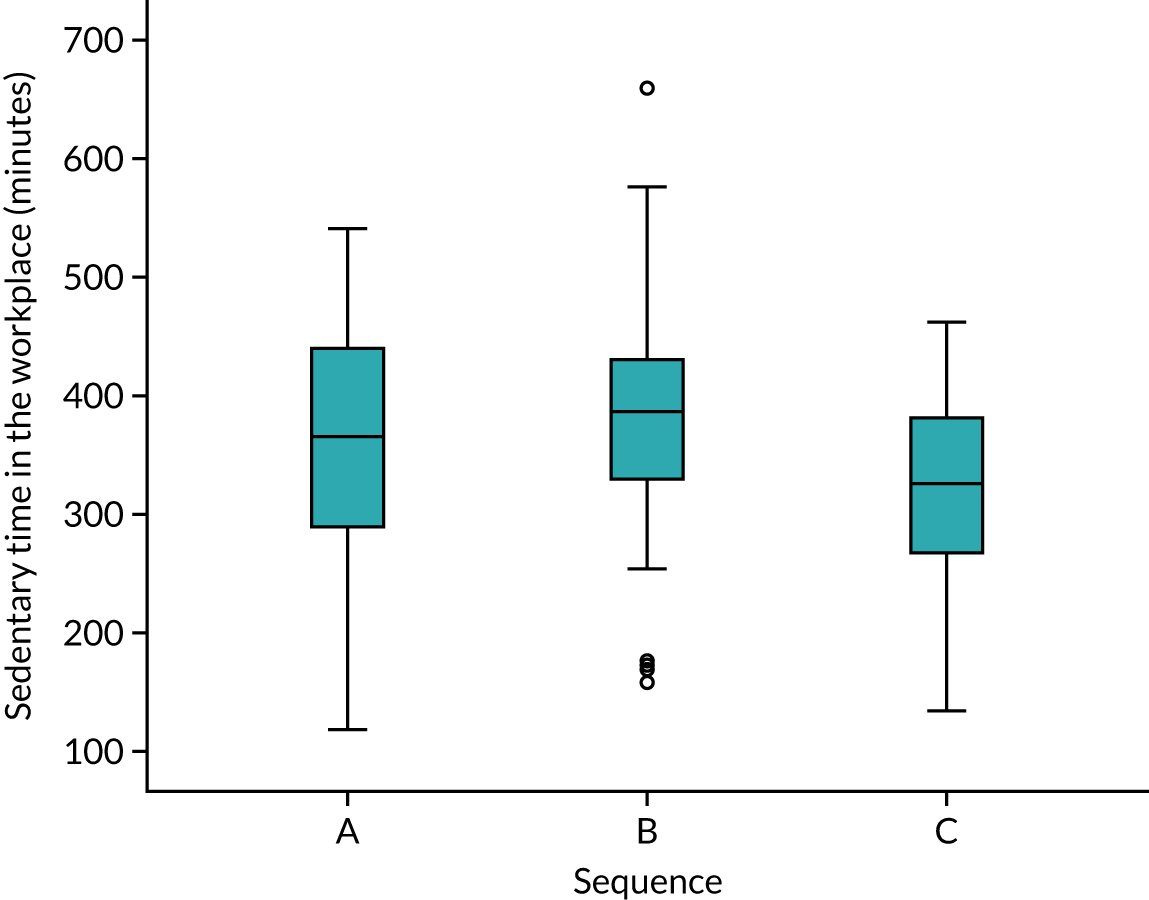
In the pre-lockdown phase, the number of participants (%) meeting physical activity guidelines was 30 (60%), 41 (69%) and 26 (62%) in sequences A, B and C, respectively. Overall, 97 (64%) participants met physical activity guidelines. The proportion meeting physical activity guidelines in each centre is shown in Table 16. The percentage meeting physical activity guidelines per centre ranged from 57% to 79%.
| Centre | n (%) |
|---|---|
| 1 | 13 (61.9) |
| 2 | 16 (57.1) |
| 3 | 15 (57.7) |
| 6 | 13 (61.9) |
| 10 | 26 (78.8) |
| 11 | 14 (63.6) |
| Total | 97 (64.2) |
Box plots for the subjective secondary outcomes are shown in Report Supplementary Material 10 (see Tables S10.3–12).
Post-lockdown phase
Regarding the post-lockdown phase analysis, crude paired t-tests of each outcome were computed to compare baseline with follow-up (Table 17). Mean differences and 95% CIs were reported. Only participants responding at both baseline and the 3-month follow-up (n = 25) were included in the descriptive analysis and paired t-test.
| Outcome | n | Mean difference (3-month follow-up – baseline) | 95% CI | p-value |
|---|---|---|---|---|
| Hours sitting at work per week | 25 | 0.47 | –2.77 to 3.71 | 0.768 |
| Minutes sitting at work per working day | 23 | 13.62 | –20.65 to 47.90 | 0.418 |
| WEMWBS total score | 25 | –0.40 | –3.18 to 2.39 | 0.771 |
| UWES mean score | 23 | 0 | –0.37 to 0.37 | 1.00 |
| MSK-HQ total score | 23 | –2.09 | –4.83 to 0.65 | 0.129 |
For the binary outcome of ‘meeting physical activity guidelines’ according to the Scottish PASQ, a cross-tabulation of the number of participants meeting physical activity guidelines at baseline and follow-up was constructed (Table 18).
| 3-month follow-up (n) | Total (n) | |||
|---|---|---|---|---|
| No | Yes | |||
| Baseline | No | 3 | 3 | 6 |
| Yes | 4 | 15 | 19 | |
| Total | 7 | 18 | 25 | |
A crude McNemar’s test for paired data was performed as an exploratory test to determine if there was any statistically significant difference in the proportion of participants meeting physical activity guidelines between baseline and follow-up. This McNemar’s test produced an exact p-value of 1.00, indicating no evidence of a difference between baseline and the 3-month follow-up. There was no change for 18 out of 25 (72%) participants.
A scatterplot of the number of hours sitting at work for baseline compared with the 3-month follow-up is shown in Figure 11. The solid line represents the line of equality. Similar plots are shown for the other outcomes in Report Supplementary Material 10, Figures S10.13–16.
FIGURE 11.
Scatterplot showing number of hours sitting at work at baseline and the 3-month follow-up.
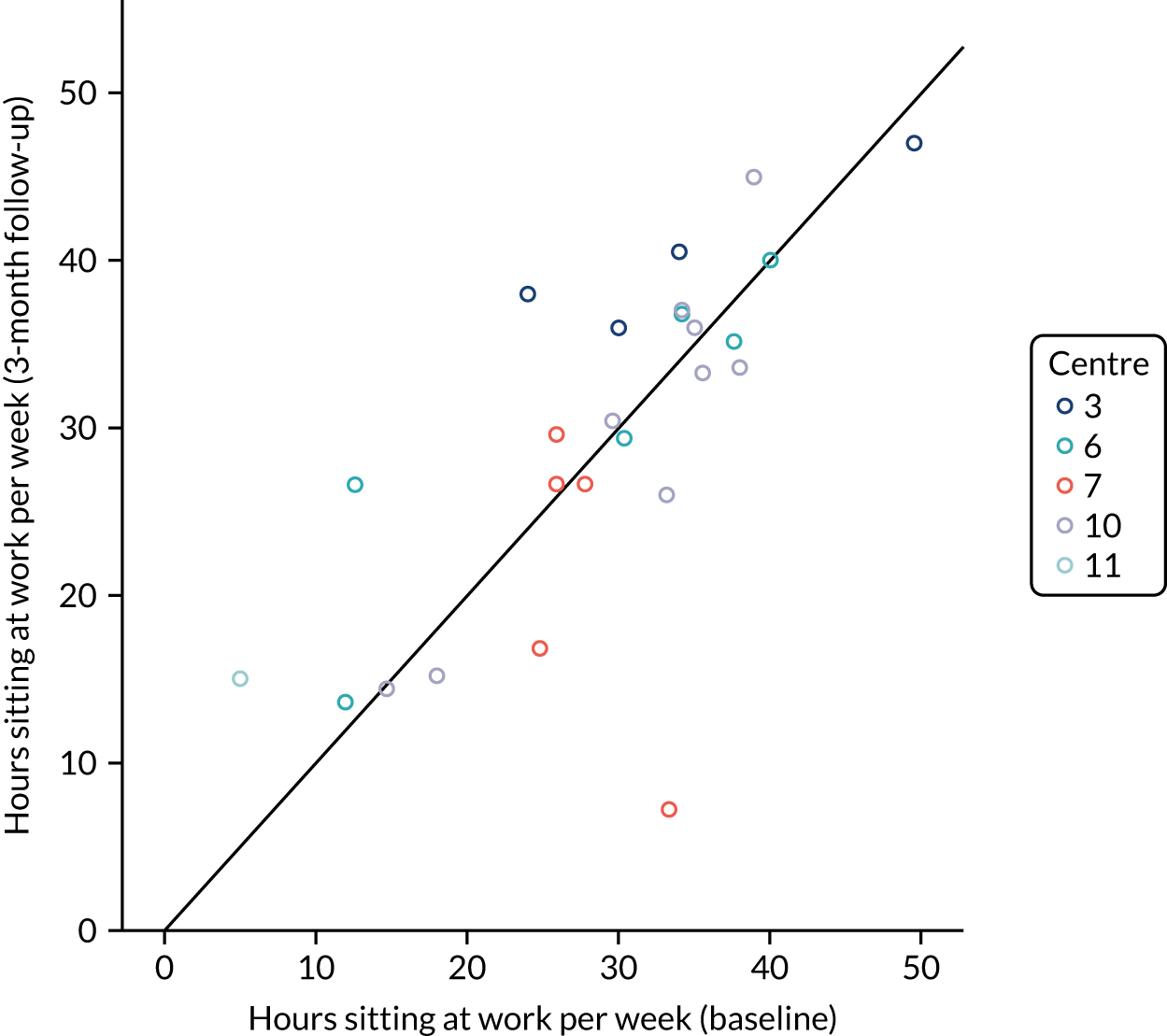
Mixed-effects model analysis
Pre-lockdown phase
A linear mixed-effects model was fitted to each outcome to compare the intervention with the control group, adjusting for centre, time point (baseline vs. 6 months), age, female sex, part-time working, working at the centre for more than 3 years and any health problems preventing more participant movement at work. Contact centre was included in the model as a random effect, but all other explanatory variables were fixed effects. In the statistical analysis plan, we originally planned to include participant as a random effect, and adjust for calendar time since the start of the study and season (spring, summer, autumn, winter) as fixed effects, but in the actual fitted models these covariates could not be included. This was because we had to adjust our planned analysis so that we were fitting a more suitable statistical model owing to the impact of the COVID-19 pandemic and major changes to the study design. The primary analysis and all secondary analyses were based on the actual study design and intervention implementation, not the planned schedule.
Owing to the small sample size and potential confounding between centre and treatment, the mixed-effects analyses were considered to be purely exploratory. Intervention effect estimates (mean differences), 95% CIs and p-values were reported. Model-based estimates of the between-centre SD were extracted from the model output to give rough estimates of the variability between centres.
Table 19 shows the intervention effect estimates from the linear mixed-effects models, with 95% CIs and p-values, which also shows a model-based estimate of the between-centre SD.
| Outcome | n | Intervention effect (6-month follow-up – baseline) | 95% CI | p-value | Between-centre SD |
|---|---|---|---|---|---|
| Total sedentary time in the workplace per day (minutes) | 92 | 60.30 | –3.62 to 124.27 | 0.058 | 0.00014 |
| Total sedentary time while awake per day (minutes) | 88 | 84.06 | 4.07 to 164.1 | 0.044 | < 0.0001 |
| Prolonged sitting time over 30 minutes in the workplace (minutes) | 92 | 5.21 | –95.8 to 106.2 | 0.880 | 11.2 |
| Prolonged sitting time over 30 minutes while awake (minutes) | 88 | 18.17 | –211.9 to 248.2 | 0.818 | 58.9 |
| Standing time in the workplace (minutes) | 90 | –2.98 | –88.56 to 82.61 | 0.919 | 11.8 |
| Standing time while awake (minutes) | 80 | –31.18 | –83.69 to 21.3 | 0.155 | 0.000668 |
| Stepping time in the workplace (minutes) | 87 | 4.097 | –26.74 to 34.93 | 0.701 | 6.7 |
| Stepping time while awake (minutes) | 79 | –14.27 | –87.02 to 58.5 | 0.577 | 18.4 |
| Light-intensity activity stepping time in the workplace (minutes) | 87 | 4.097 | –26.74 to 34.93 | 0.701 | 6.7 |
| Light-intensity activity stepping time while awake (minutes) | 79 | –14.27 | –87.02 to 58.5 | 0.577 | 18.4 |
| Sit-to-stand transitions in the workplace (minutes) | 89 | 6.22 | –5.95 to 18.40 | 0.202 | 1.8 |
| Sit-to-stand transitions while awake (minutes) | 79 | –2.11 | –34.35 to 30.13 | 0.848 | 6.81 |
| OSPAQ | |||||
| Hours sitting at work per week | 148 | 6.54 | –15.76 to 28.85 | 0.419 | 6.73 |
| Minutes sitting at work per day | 148 | 68.55 | –276.50 to 413.60 | 0.572 | 107 |
| WEMWBS total score | 149 | –1.28 | –4.79 to 2.24 | 0.332 | 0.23 |
| UWES mean score | 148 | –0.76 | –1.49 to –0.03 | 0.045 | 0.11 |
| MSK-HQ total score | 130 | 0.88 | –11.08 to 12.84 | 0.830 | 2.89 |
There was insufficient evidence of any difference in sedentary time in the workplace between groups, with a mean difference of 60.30 minutes (95% CI –3.62 to 124.27 minutes). However, there was a significantly greater total sedentary time spent while awake in the centres that received the intervention than in those that did not (mean difference 84.06 minutes, 95% CI 4.07 to 164.1 minutes). The other outcome results shown in Table 19 also tended to favour the control group, as indicated by the direction of the intervention effects and CIs. However, please note that this pre-planned analysis has important limitations owing to the impact of the COVID-19 pandemic; notably, centre is potentially heavily confounded with the intervention effect in this analysis. Interestingly, the between-centre SD was almost zero for the primary outcome, as shown in Table 19.
For the subjective outcomes, the results of the OSPAQ were consistent with the primary outcome and favoured the control group, although the differences were not statistically significant. There was a significantly lower level of work engagement in the intervention group, on average (mean difference in UWES score –0.759, 95% CI –1.486 to –0.033; p = 0.04), after adjusting for centre, time point, age, female sex, part-time working, working at the centre for more than 3 years and any health problems preventing more movement at work. There was insufficient evidence of any difference in the number of hours sitting at work per week (OSPAQ), number of minutes sitting at work per day (OSPAQ), WEMWBS total score or MSK-HQ total score. Between-centre SD varied substantially depending on the outcome. The OSPAQ showed very high levels of between-centre variation.
For the self-reported outcome of ‘meeting physical activity guidelines’, this was a binary (yes/no) outcome; therefore, an exploratory logistic mixed-effects model was fitted to the data adjusting for the same variables of centre, time point (baseline vs. 6 months), age, female sex, part-time working, working at the centre for more than 3 years and any health problems preventing more movement at work. The logistic mixed-effects model showed insufficient evidence of any difference in the proportion meeting physical activity guidelines between the intervention and the control group [odds ratio (OR) 0.82, 95% CI 0.32 to 2.08], after adjusting for centre, time point, age, female sex, part-time working, working at the centre for more than 3 years and any health problems preventing more movement at work. The between-centre variance was estimated to be zero.
Post-lockdown phase
For the linear mixed-effects model analysis in the post-lockdown phase, all participants who had an outcome recorded at either baseline or 3 months were included, to improve the power and precision of analysis. A linear mixed-effects regression model was fitted to the data, after adjusting for participant and centre as nested random effects. Model-based estimates of between-centre, between-participant (within centre) and residual SD were calculated (Table 20).
| Outcome | n a | Intervention effect (3-month follow-up – baseline) | 95% CI | p-value | Between-centre SD | Between-participants SD | Residual SD |
|---|---|---|---|---|---|---|---|
| OSPAQ | |||||||
| Hours sitting per week | 92 | 1.37 | –1.39 to 4.13 | 0.315 | 5.20 | 6.75 | 5.39 |
| Minutes sitting at work per working day | 89 | 17.69 | –11.39 to 46.78 | 0.220 | 59.02 | 61.64 | 55.20 |
| WEMWBS | 93 | –0.15 | –2.53 to 2.22 | 0.894 | 1.19 | 5.60 | 4.66 |
| UWES mean score | 85 | 0.19 | –0.14 to 0.53 | 0.244 | 0.23 | 0.76 | 0.63 |
| MSK-HQ total score | 84 | –2.01 | –4.55 to 0.54 | 0.116 | 0.002 | 8.43 | 3.66 |
There was insufficient evidence of any difference in outcomes between baseline and the 3-month follow-up. A logistic mixed-effects model (n = 89) showed that there was insufficient evidence of any difference in the proportion meeting physical activity guidelines between the intervention group and the control group (OR 0.88, 95% CI 0.28 to 2.80), after adjusting for participant and centre as nested random effects. The between-centre SD was zero. The between-participant (within-centres) SD was 1.25 on the log-odds scale.
Calculating estimates of variability
The assumptions underlying the sample size calculation that was carried out by a similar study73 were tested and compared with the estimates that we calculated using real data from the feasibility trial (e.g. SD, within-site correlation and intracluster correlation coefficient) to inform the power calculation for a future trial. The heterogeneity of quantitative outcomes across sites (e.g. estimated via intracluster correlation coefficients) and the variability in intervention delivery and processes across sites was of particular interest. Our aim was to determine the feasibility of conducting a future multisite study with a larger number of contact centres.
The purpose of this analysis was to help answer research questions 2 and 6:
-
Research question 2 – how many clusters and participants per cluster are required for a confirmatory trial?
-
Research question 6 – what are the preliminary estimates of the variability of primary (reduction of sedentary behaviour in the workplace) and secondary outcomes within and between contact centres?
Using the pre-lockdown data, we calculated indicative approximate estimates of empirical between-centre SD, within-centre SD and coefficient of variation of means between clusters (κ) to inform sample size calculations for future cluster randomised trials. 93 This analysis was carried out for the subgroup of centres recording information at baseline (pre intervention), as well as overall (across all centres). These estimates were computed to identify objective and subjective outcomes, with the lowest or highest levels of between-centre variation to help identify likely candidates for the primary and secondary outcomes of a future study, and also to inform sample size calculations for future cluster randomised trials. Empirical estimates of SD and coefficients of variation were computed for the pre-lockdown analysis (Table 21). High values of kappa indicated high levels of between-centre variation. The results suggest that device-measured total sedentary time exhibits potentially low levels of between-centre variation.
| Outcome | Empirical between-centre SD | Empirical within-centre SD | κ (coefficient of variation) | Empirical between-centre SD (baseline only) | Empirical within-centre SD (baseline only) | κ (coefficient of variation, baseline only) |
|---|---|---|---|---|---|---|
| OSPAQ | ||||||
| Minutes sitting at work per week | 368.26 | 508.08 | 57.89 | 139.58 | 434.39 | 72.45 |
| Minutes sitting per workday | 87.32 | 83.20 | 17.11 | 14.82 | 73.46 | 20.66 |
| Hours sitting at work per week | 6.14 | 8.47 | 0.96 | 2.33 | 7.24 | 1.21 |
| WEMWBS total score | 3.16 | 7.49 | 0.08 | 2.04 | 6.86 | 0.12 |
| UWES mean score | 0.48 | 0.89 | 0.03 | 0.11 | 0.85 | 0.03 |
| MSK-HQ total score | 3.23 | 11.45 | 0.00 | 2.55 | 10.41 | 0.00 |
| Total sedentary time in the workplace per day (minutes) | 34.14 | 100.08 | 0.12 | 43.59 | 96.04 | 1.16 |
| Total sedentary time while awake per day (minutes) | 33.25 | 108.14 | 0.00 | 35.39 | 111.04 | 0.32 |
| Prolonged sitting time over 30 minutes in the workplace (minutes) | 22.62 | 94.34 | 0.00 | 25.01 | 101.98 | 0.00 |
| Prolonged sitting time over 30 minutes while awake (minutes) | 47.56 | 102.20 | 2.79 | 51.25 | 119.24 | 3.89 |
| Standing time in the workplace (minutes) | 27.97 | 70.86 | 2.38 | 24.16 | 80.30 | 4.69 |
| Standing time in while awake (minutes) | 15.95 | 75.16 | 0.00 | 17.19 | 76.61 | 0.00 |
| Stepping time in the workplace (minutes) | 10.42 | 15.85 | 2.60 | 9.36 | 16.32 | 3.18 |
| Stepping time while awake (minutes) | 13.94 | 37.04 | 0.33 | 15.29 | 38.58 | 0.86 |
| Light-intensity activity stepping time in the workplace (minutes) | 10.42 | 15.85 | 2.60 | 9.36 | 16.32 | 3.18 |
| Light-intensity activity stepping time while awake (minutes) | 13.94 | 37.04 | 0.33 | 15.29 | 38.58 | 0.86 |
| Sit-to-stand transitions in the workplace (minutes) | 5.85 | 9.72 | 0.96 | 7.34 | 9.41 | 1.12 |
| Sit-to-stand transitions while awake (minutes) | 11.13 | 15.75 | 1.91 | 10.60 | 19.25 | 2.05 |
Attrition and staff turnover
Pre-lockdown phase
We aimed to examine how many participants were lost to follow-up as a result of staff turnover in the period from the start of the trial to the start of the post-lockdown phase. The purpose of this analysis was to help answer research question 3:
-
What is the recruitment rate of participants in each cluster and how many are lost to follow-up (e.g. owing to staff turnover)?
After recruiting participants in the pre-lockdown period, four of the centres (centres 3, 6, 10 and 11; 106 participants in total) were invited to participate in the post-lockdown programme (approximately 10–12 months later), although only three of the centres agreed to participate (centres 6, 10 and 11; 79 participants in total). We investigated the rates of the number of staff known to have left the company and the number of staff moving jobs within the same company during this time.
We considered two binary outcomes:
-
left company – whether or not the participant was known to have left the company in the period between collection of pre-lockdown data and collection of post-lockdown data (approximately a 10- to 12-month gap depending on the centre)
-
moved job – whether or not the participant moved departments within the company or left the company completely between the pre-lockdown and post-lockdown data collection periods.
The proportion of participants leaving the company and moving jobs was computed with exact 95% CIs. Regarding attrition, there were 13 out of 106 participants recorded as having left the company after pre-lockdown data collection (12%, 95% CI 7% to 20%). There were 23 out of 106 participants recorded as having moved jobs after the pre-lockdown data collection (22%, 95% CI 14% to 31%). Note that these proportions do not include loss to follow-up owing to participant loss of interest or participant-level dropout because of other personal reasons. Unfortunately, it was not possible to calculate accurate estimates of overall loss to follow-up because participants from the pre-lockdown data collection phase were not individually or specifically followed up in the post-lockdown phase. Only centres were contacted and recruitment was achieved within each centre via recruitment champions based in each centre. There was also a dramatic change in working environment for many centres between the pre-lockdown and post-lockdown recruitment phases.
We fitted a multiple logistic regression model to each of the binary outcomes to investigate predictors of moving jobs or leaving the company. The multiple logistic regression model had the following explanatory variables (all entering the model as fixed effects): contact centre, sex, part-time working, age and how long the participant had been working at the contact centre. Odds ratios were presented with 95% CIs. The aim of this analysis was to investigate which types of participants were most likely to leave the company owing to staff turnover to help inform the design of a future trial.
Table 22 presents ORs with 95% CIs from the logistic regression models fitted to each of the attrition outcomes. If the OR is > 1, this indicates that leaving the company or moving jobs is more likely for that category compared with the reference category.
| Variable | Left company (n = 103), OR (95% CI) | Moved job (n = 103), OR (95% CI) |
|---|---|---|
| Centre | ||
| 3 | 9.11 (0.94 to 88.60) | 0.60 (0.14 to 2.51) |
| 6 | 3.63 (0.43 to 30.63) | 0.49 (0.11 to 2.10) |
| 11 | 3.88 (0.42 to 35.60) | 0.48 (0.11 to 1.97) |
| 10 (reference category) | ||
| Male sex | 1.59 (0.32 to 7.83) | 1.67 (0.49 to 5.62) |
| Part-time worker | 3.42 (0.59 to 19.64) | 2.61 (0.75 to 9.07) |
| Age (years) | ||
| 18–34 (reference) | ||
| 35–54 | 1.37 (0.31 to 6.00) | 1.06 (0.35 to 3.24) |
| ≥ 55 | 4.01 (0.44 to 36.43) | 2.50 (0.50 to 12.56) |
| How long working for the contact centre? | ||
| < 1 year (reference) | ||
| 1–3 years | 2.52 (0.49 to 13.04) | 2.04 (0.50 to 8.29) |
| > 3 years | 0.39 (0.06 to 2.35) | 1.45 (0.38 to 5.49) |
No variables were statistically significant predictors of outcome. However, the ORs for centre were of a high magnitude, indicating strong centre-level effects in the observed data, although these did not reach statistical significance. Interestingly, older participants (aged ≥ 55 years) and those working part time were more likely to have left the company after the pre-lockdown data collection, but, again, this did not reach statistical significance, perhaps because of the small sample size. Note that these effects may be at least partly due to the COVID-19 pandemic.
Post-lockdown phase
Regarding attrition, we examined how many participants involved in post-lockdown data collection left the company, moved jobs or were lost to follow-up over the 3-month follow-up period. Exact 95% CIs were reported for the percentages. We also investigated descriptively if there were any common themes or patterns in the types of people leaving or moving within the company.
Regarding attrition after post-lockdown baseline data collection, two participants from one centre (centre 7, n = 20) left the company between baseline and follow-up (3 months). In addition, two participants from another centre (centre 10, n = 18) left the company and one moved departments within the same company. This equates to a staff turnover rate of approximately 10–20% in each of these two centres. Overall, 5 out of 54 participants left or moved after the baseline post-lockdown data collection (9%, 95% CI 3% to 20%).
The five participants who left or moved departments after the baseline post-lockdown data collection were of various ages (two were in the 18–24 years age category, one in the 25–34 years age category, one in the 35–44 years age category and one in the 55–64 years age category) and of roughly even sex split (three were male and two were female). Four participants were full time and one part time, and they had worked in the company for different lengths of time (ranging from < 1 year to > 3 years). Therefore, there were no clear patterns in the demographics among those leaving.
Overall, 26 out of 54 participants who were lost to follow-up (48%, 95% CI 34% to 62%) were lost to follow-up for any reason.
We fitted a multiple logistic regression model to the ‘lost to follow-up’ variable, adjusting for contact centre, sex, part-time working, age and how long the participant had been working at the contact centre. Table 23 presents ORs with 95% CIs for the ‘lost to follow-up’ model. An OR of > 1 indicates that loss to follow-up is more likely.
| Variable | Lost to follow-up (n = 54), OR (95% CI) |
|---|---|
| Centre | |
| 3 | 0.10 (0.004 to 2.78) |
| 6 | 0.20 (0.01 to 2.83) |
| 7 | 0.37 (0.05 to 2.88) |
| 11 | 0.72 (0.03 to 15.25) |
| 10 (reference category) | |
| Male sex | 12.14 (1.77 to 83.31) |
| Part time worker | 3.51 (0.37 to 33.33) |
| Age (years) | |
| 18–34 (reference) | |
| 35–54 | 0.08 (0.01 to 0.62) |
| ≥ 55 | 0.17 (0.02 to 1.87) |
| How long working for the contact centre? | |
| < 1 year (reference) | |
| 1–3 years | 0.28 (0.01 to 5.21) |
| > 3 years | 0.16 (0.01 to 3.53) |
Participants in the 35–54 years age bracket were significantly less likely than those aged < 35 years to be lost to follow-up (p = 0.02). Male participants were significantly more likely than females to be lost to follow-up after 3 months in this analysis (p = 0.01).
Evaluation of relevant research questions based on study findings
-
Is the study design (cluster RCT) feasible for a confirmatory trial of an intervention to reduce sedentary behaviour in staff working in contact centres?
We found that a stepped-wedge design would not be suitable for a future larger-scale trial. We experienced difficulties in maintaining site interest, which would be exacerbated in a trial of longer duration (e.g. if some sites were randomised to receive the intervention 12 months later), and it was challenging to ensure that each site adhered to the scheduled data collection time points. In addition, 22% of participants moved jobs after 10 to 12 months. Instead of a stepped-wedge trial design, we suggest that a parallel-group cluster-randomised trial, in which sites are recruited in pairs (or groups) over time, would be much more practical.
-
How many clusters and participants per cluster are required for a confirmatory trial?
This research question can be answered using the data presented in Table 21. For example, for the primary outcome (total sedentary time in the workplace per day in minutes), the overall coefficient of variation was 0.12 minutes, and the within-site SD was 100.08 minutes overall and 96.04 minutes at baseline. In addition, the mean value of the primary outcome at baseline was 359.6 minutes and we recruited a mean of 15.6 participants providing valid primary outcome data per cluster (see Figures 6 and 8). Therefore, using equation 6 from Hayes and Bennett,93 we calculate that we would need 25 clusters in a future cluster-randomised trial to detect a clinically relevant difference in sedentary time of 45 minutes with 90% power and two-sided 5% significance level. We suggest that a future cluster trial, with clusters recruited in pairs, would have a low cluster-level dropout rate of 10% because in this future trial, design clusters would not have to wait long to begin the intervention. We, therefore, suggest that a future trial should aim to recruit 28 clusters, taking centre-level dropout rates into account. We also recommend that a future trial aims to recruit 40 participants per centre, on average, to use the activPAL devices and to have at least 15 or 16 participants per centre recording valid primary outcome data.
-
What is the recruitment rate of participants in each cluster and how many are lost to follow-up (e.g. owing to staff turnover)?
As shown in Figure 6, the CONSORT flow diagram (pre-lockdown phase), there was a mean of 26 participants per cluster, of whom 16 per cluster provided valid primary outcome data and 25 per cluster provided valid secondary outcome data (i.e. data from the OSPAQ), on average. Considering specific outcomes relating to attrition, of the four centres invited to participate in the post-lockdown data collection (centres 3, 6, 10 and 11; n = 106), 13 out of 106 staff were recorded as having left the company after the pre-lockdown data collection (12%, 95% CI 7% to 20%). In total, 23 out of 106 staff were recorded as having moved jobs after the pre-lockdown data collection (22%, 95% CI 14% to 31%).
-
What are the preliminary estimates of the variability of primary (reduction of sedentary behaviour in the workplace) and secondary outcomes within and between contact centres?
Estimates of variability for the primary and secondary outcomes are presented in Table 21. The OSPAQ showed very substantial variability in our study (SD at baseline of 7.2 hours of sitting), although the primary outcome SD at baseline was lower (1.6 hours).
Conclusions
We found no evidence of an improvement in sedentary behaviour or other outcomes in either the pre-lockdown or the post-lockdown analysis. However, each analysis has important limitations. Namely, in the pre-lockdown analysis, the intervention effect may be confounded by centre because of the small number of centres and, in the post-lockdown analysis, we are unable to exclude the possibility of non-intervention-related changes over time biasing the analysis. The available sample size was also relatively small for both analyses, leading to imprecise model estimates. Nevertheless, we collected detailed descriptive information on all outcomes both pre and post lockdown that could be used to design a future study and be used in sample size calculations. We found that the level of between-centre variation for the OSPAQ was very high, which should be taken into account if considering this outcome as a primary outcome in future cluster RCTs. By contrast, the activPAL device-measured outcome appeared to exhibit very low between-centre variation.
One of the progression criteria for the feasibility study was that our 95% CI for the primary outcome included a 45-minute reduction in sedentary time per day. However, our CI did not even contain a 5-minute reduction in sedentary time in the pre-lockdown analysis. For the post-lockdown analysis, we were unable to collect device-measured data on sedentary behaviour, but according to the OSPAQ (subjective measure), differences of 12 minutes or more per day in favour of the intervention were excluded. The generalisability of these results is limited because of the important limitations and potential bias associated with both analyses. Nevertheless, these results do not imbue confidence that clinically important reductions in sedentary behaviour would be seen in a larger study.
In terms of participant characteristics at baseline, a greater proportion of participants than we expected had been working in the company for more than 3 years, and it is recommended that future questionnaires are designed with this in mind. In particular, we recommend that the ‘> 3 years’ category should be subdivided into further categories so that we have more precise data on the duration of employment in the company. For example, the questionnaire options could include ‘3–5 years’, ‘5–10 years’ and ‘> 10 years’ as options, instead of only ‘> 3 years’.
The COVID-19 pandemic was a big confounder in the analysis of dropouts (especially for the pre-lockdown analysis) and it is difficult to use this information to confidently ascertain what might happen in a future study. Rates of drop-out are likely to be overestimates of what might happen in a future study owing to the impact of the COVID-19 pandemic. Nevertheless, it is interesting that the level of dropout over 12 months varied substantially by centre in the pre-lockdown analysis. In the post-lockdown analysis, younger and male participants were more likely to be lost to follow-up over the 3-month period post pandemic. It is particularly important that efforts to reduce attrition and maintain participant involvement in the study are targeted primarily at the centre level, rather than at the individual level.
The planned statistical analysis methods were feasible, even in the situation of reduced sample size, because of the COVID-19 pandemic. In particular, we had no problems with model fitting or convergence for the linear mixed-effects models.
Chapter 5 Scoping the feasibility of a future health economic evaluation
Introduction
The third aim of the study was to scope the feasibility of a future health economic evaluation of SUH. The research question that we aimed to answer was ‘Is it feasible to provide estimates of the cost-efficiency of Stand Up for Health from (a) an NHS and Personal Social Services perspective and (b) an employer’s perspective?’.
Rationale and guiding principles
Typical cost-efficiency analyses used in health technology assessment rely on estimating impacts on ‘hard’ health outcomes and associated improvements in morbidity, mortality and health and social care service utilisation. 91,93,94 Although it may be plausible that increased fitness could in the long term lead to such improvements, the trial follow-up period was insufficient to reasonably result in measurable `differences. Direct surveying of individual participants was also not possible given that only centre-level data were recorded. Hence, health economic assessment was instead designed to scope the feasibility of future trials. Of additional interest was identifying outcomes (including costs) from an employer’s perspective that could be important at an implementation stage to leverage commercial support and scoping potential methods of measurement, should the programme demonstrate benefits. Economic perspectives for analyses, therefore, comprised a mix of an NHS and PSS perspective [as per the standard National Institute for Health and Care Excellence (NICE) Reference Case98] and employer’s perspective assessments.
In March 2020, national lockdown restrictions because of the COVID-19 pandemic changed the nature of the study and the nature of office working. It was not possible to know what future office environments would look like relative to before or during the lockdown period. Hence, working environments may be considered on a spectrum between pre-lockdown office environments and full home-working office environments. Many of the analyses were, therefore, split into results before and after lockdown, representing the two possible extremes. In principle, should the world move to some form of long-term hybrid working or different offices adopt different rates of hybrid working, each may reasonably be considered to be somewhere on a spectrum between these two points, although it is recognised that such assumptions are necessarily speculative and post hoc. A CHEERS (Consolidated Health Economic Evaluation Reporting Standards) checklist highlighting key principals (where relevant) and where they are located in this report has been included in Report Supplementary Material 12.
Methods
The health economics substudy of SUH comprised three principal components:
-
a qualitative survey of prospective outcome measures for future trials from an employer’s perspective completed by site leads
-
an activity-based costing (ABC) exercise of the direct implementation costs of the programme
-
a scoping of the literature to identify potential economic modelling structures for future trials.
Qualitative survey of prospective outcome measures from an employers’ perspective
A questionnaire was developed with aid from, and administered by, qualitative researchers in the team (see Report Supplementary Material 11). This aimed to identify employers’ priorities for outcomes of the programme that might drive decisions to adopt or form criteria for judging success and, therefore, continuation of a programme in a hypothetical future rollout. The questionnaire included free-format questioning regarding the metrics they use:
-
to measure productivity, absenteeism, presenteeism, staff turnover or other metrics of importance to them
-
how and how frequently these were measured
-
whether or not they attribute a financial cost to these routinely and, if so, how
-
whether or not they benchmark these measures between teams within the site, against other sites, other organisations, industry standards and/or other groups
-
what arrangements were in place to assess ergonomics and mental health
-
what measures would be of use to measure in a future follow-up trial and which were of highest priority
-
would they, hypothetically, be willing and able to share any of their internally collected metrics and, if so, what form of data might be possible.
Surveys were issued after the trial observation period. Notably, in all cases, survey responses decreased post lockdown and resulting changes in office working patterns. As such, respondents may reasonably be assumed to have attempted to take these into account in their replies. However, the specifics of these would not have yet been established and, therefore, any adjustments were necessarily speculative.
Completed forms were analysed using descriptive statistics and reported narratively. Qualitative (free-form text) data from the five returned forms were summarised and general themes were reported. We did not use a more rigorous analysis (such as thematic analysis) owing to the small pool of data and the short length of the individual answers. The themes and key points identified were then incorporated into the model-scoping exercise (component 3) to examine whether or not there may be any potential to build in any identified outcomes, such as absenteeism/productivity measures, alongside more traditional health-related cost-efficiency outcomes.
Activity-based costing
A taxonomy of activities involved in programme provision was generated by the research staff providing the service. This included equipment, SUH staff time, call centre workforce and management staff time, travel costs, and stationery and sundries. In accordance with standard ABC principles,95,97,98 staff were asked to record items that may reasonably be expected to occur in a hypothetical mass rollout of the programme only, that is excluding activities specific to research, such as interviewing or data collection. This was initially planned to be measured prospectively; however, before this could be undertaken, lockdowns were initiated, which prevented direct measurement. Instead, a breakdown of activity was generated from records and invoices, with durations of workshops based on professional judgement and experience of what would be needed in practice.
An opportunistic post hoc analysis repeated the exercise for workshops held during lockdown. This was undertaken to investigate how changes to remote working might influence the intervention and costable activities, potentially reflecting two different options for programme provision and testing the feasibility of ABC measurement in a future trial.
We initially planned to record details of devices purchased by centres on completion of the SUH programme. In practice, sites initially borrowed devices from a central pool of equipment held by the SUH programme, but adoption/purchase of their own devices became a moot point with the need to prioritise home-working arrangements as a result of lockdowns. The feasibility of attributing costs to equipment use was, therefore, based on SUH programme costs alone.
The primary focus of assessment was to estimate the rates of various forms of activity rather than their implicit costs in a hypothetical rollout, given that there is a great deal of heterogeneity in the components of price weights between sites. Examples include differences in rates of facilities available, differences in wage or other labour cost elements for staff at different organisations, and scope to have different types of staff providing different programme implementation activities, were the intervention implemented at scale. The time horizon considered cost/activities on a per-annum, per-site basis.
Finally, it should be noted that these results should be considered indicative and not definitive owing to small samples and low power.
Model-scoping exercise
Health economic decision analytic modelling methods frequently rely on grouping individuals into common pooled ‘health states’ or events of broadly similar impact on health-related quality of life and health-care resource implications. Models typically include a clinically based core that simulates patient transitions between health states and/or critical health events. A set of health and cost outcomes are then attached to each health state/event to convert these into economic outcomes of interest, usually accumulated over a prespecified time horizon. Both elements are often based on established probabilities or risk equations and synthesise a wide range of evidence. 93,97
To scope the potential for modelling of both of these aspects of the model, two principal steps were undertaken:
-
Potential health states or groups of health states were identified – experts within the team were asked to describe potential long-term outcomes that the intervention might reasonably aim to improve if successful.
-
A non-systematic search of the literature was undertaken to look for potential similar models; literature linking surrogate outcomes, such as secondary behaviour, to these target health states; and potential studies attributing cost, quality of life [as measured using quality-adjusted life-years (QALYs)] or outcomes identified by qualitative consultation with sites as desirable to employers to these health states.
Consideration was then given to how well these data might fit the available options for collection alongside a future trial.
Results from qualitative survey of prospective outcome measures from an employers’ perspective
Questionnaires were returned from five out of seven sites approached. The following section provides a qualitative description of the responses received.
Companies defined productivity as a measure of how efficiently their employees met service demand, the quality and quantity of their work, and how well they worked in teams to meet targets. Productivity was often measured by the number and pace of calls answered, combined with customer satisfaction. Companies collected productivity data via several different automated systems on a regular basis, typically daily. They used these data to determine the rate of calls taken, allowing comparison of productivity with that of previous months. Two of the companies translated productivity to costs, for example the number of calls drove staffing numbers, although the other three companies said that they did not translate productivity directly to cost as their team was linked to workflow in other departments.
Absenteeism was commonly defined by sites as the number of hours lost compared with the total number of hours scheduled. There were several reasons for absenteeism, including special leave (e.g. bereavement; could be paid or unpaid) and unpaid leave. However, the main cause was often sickness, which was measured in isolation as the number of days employees were absent owing to sickness. Several sites also included annual leave, parental leave and shift swap among absenteeism outcomes, which would not match the definition of absenteeism. However, it is thought that these were included for completeness only in an attempt to aid the study rather than a perception that these are equivalent to absenteeism. One company reported using the Bradford factor (a human resource theory that refers to the use of the Bradford formula to measure absenteeism) to follow trends in absenteeism, which identified 9 or more days absent per year or three separate occasions of absenteeism as a trigger. Similar to productivity, absenteeism was measured daily by all but one company, which measured it monthly. All companies reported including a record of the reason for absence.
Presenteeism was measured more inconsistently between companies. Three of the companies did not measure this at all, whereas the other two companies measured it based on absenteeism data. One company described the use of an annual survey to assess employees’ engagement index as a measure of presenteeism. Absenteeism and presenteeism were more consistently translated to costs, often because of the effect of reduced staffing on productivity; therefore, reducing income and contributing to poorer customer service. All but one of the companies agreed that absenteeism was linked to productivity and was sometimes used to determine staffing needs; however, the remaining company argued that these factors were independent because productivity is a measure of those who were present on that day, suggesting that presenteeism influences productivity more.
Staff turnover was determined by the number of employees leaving the business, including those ‘on loan’ to other departments. Details of which department they were leaving, the reason for leaving and the duration of employment were often recorded. However, one of the companies did not, or could not, provide this information. The exact cost of staff turnover was not provided by any participating companies, although they often acknowledged that it was a significant amount, with one participant suggesting that it would cost roughly £2500 in staff time to recruit per vacancy.
Staff requirement of additional support was continuously assessed by all participating companies. Several methods were used to assess this, including desk assessments to ensure that all necessary equipment was provided, line managers having regular contact with employees and an occupational health service for physical and mental health support. Display screen equipment risk assessments were used by three of the companies to assess support needs, along with regular discussions with staff to ensure that they were aware of the support that they have access to. Staff support requirements were assessed on a specific request or concern being identified and via regular formal assessments that were conducted by all participating companies roughly once per month.
Four out of five of the participating companies benchmarked themselves internally team by team, against organisation targets and against published industry standard, in addition to comparison with other centres (potential competitors). This was used as a quality assurance technique, and one organisation mentioned that external awards were used to aid in benchmarking themselves (e.g. best call centre awards).
Overall, productivity was the most important measure for three of the companies surveyed, with the remaining two acknowledging the equal importance of absenteeism, presenteeism and staff turnover, and how these measures are interlinked with productivity. One organisation highlighted the damage that high staff turnover can have on the reputation of a business, thus impacting sales. Staff feedback assessments of how participants felt, changes in their engagement or absence and whether or not their productivity increased were perceived to be the best way to gauge the impact of SUH. In addition, absenteeism or improvements in staff well-being were identified as other metrics that could be helpful in determining the impact of the SUH programme. Despite this consensus, participating organisations were unable to provide any full reports or samples of data recorded on presenteeism, absenteeism and productivity for scrutiny by the SUH team. Some were unable to share these data for confidentiality reasons or ongoing union disputes. Others who reported willingness to share data in principle warned that current samples would be skewed owing to additional leave relating to the pandemic (sickness and special leave). However, in practice, no samples were made available owing to complications linked to COVID-19 disruptions and sites needing to prioritise other activities. Therefore, although it is possible that some sites may have been able to provide data under other circumstances, the degree to which this would be achieved outside a pandemic remains unclear and it was not possible to scrutinise the data directly.
Implications for future health economic evaluations
This section considers the implications of these results with respect to onsite data collection within a hypothetical future trial. Implications with respect to potential modelling are discussed separately in Model-scoping exercise. Respondents measured productivity with a variety of metrics. Although many of these revolved around call-handling time and quality, the lack of primary specific common metrics between sites may make this challenging to measure quantitatively, at least directly. It is, therefore, important to first consider its components individually.
Absenteeism was commonly measured in terms of some form of percentage full-time equivalent (FTE) lost, whether this was converted from days or hours, probably reflecting the relative simplicity of the concept. Those not stating this directly at least implied it to be in use within the organisation, for example via a central department. A common method of quantifying this (when stated at all) was to multiply percentage FTE lost by wage. This method is consistent with the methodological and theoretical framework available in a human capital approach from the economic literature. 92 Thus, a simple theoretical and methodological framework for future analysis is at least available. 94 There were no indications of anything akin to, or usable with, the alternative friction costing approach,95 probably because of its relative complexity in calculation. Such an approach may require synthesis with external data or bespoke surveying; however, a specific method to do so beyond standard measures was not identified.
Few sites were able to provide data on staff turnover directly. Several did indicate that staff turnover was recorded elsewhere within their organisation, and it was implicit that these data were recorded in a consistent manner, although recoded reasons for turnover differed. It is possible that a future trial may be able to obtain rates of total turnover by contacting the appropriate department or collecting them prospectively. With differences between organisations driving per-trainee cost implications and sites themselves not able to provide known estimates of cost per trainee, reporting simple rates of turnover or change in percentage turnover may be sufficient information for prospective organisations considering a SUH rollout. This would enable them to interpret this in their own context, rather than consolidating this to an abstracted financial figure.
Although sites recognised that presenteeism was an important factor in productivity, they also recognised that it was challenging to measure, and few collected any metrics or converted it to a cost. In economic analyses, this often carries an inherently subjective element of perceived self-reported percentage loss in productivity. This component both carries risk of being perceived as less credible than days/hours absent and requires individual-level surveying, which was not possible in this style of study. By contrast, ‘harder’ outcomes, such as days/hours absent, are recorded centrally. Several sites also considered staff engagement to be important, but similarly did not offer a means to convert this to cost. There was an implicit understanding that engagement has the potential to lead to improved productivity and staff turnover savings, even if the specific mechanism(s) involved may not be easy to disentangle. Sites also indicated desirability for engagement improvements beyond a purely financial/productivity level. It is unclear how much weight this would be given in a rollout decision, although it remains an option for measurement where possible in its own right, irrespective of purpose.
First, we look at the productivity angle of presenteeism and engagement collectively. Given their acceptance of the challenges of recording metrics to enable conversion to cost, organisations may be open to lower grades of evidence to inform their decisions, should direct measurement prove impractical. Options could include:
-
Allowing sites to record productivity using their metric(s) of preference, which could be reported in terms of percentage change.
-
Measuring perceived productivity change in categorical format, such as a Likert scale-based questionnaire issued to management.
-
Use of some form of discrete choice experimental design. 97 Non-productivity/financial changes in engagement might then be recorded separately using bespoke metrics, possibly within the same questionnaires to management if used.
For those sites willing, as well as for sites unwilling or unable to share internal data, particularly around absenteeism for which metrics are likely to be more comparable between sites, discussions should be held with sites at recruitment and disclosure agreements put in place where needed.
Activity-based costing exercise
Table 24 displays the approximated costs of a SUH programme for 11 centres, which are estimated separately for programmes run under pre-lockdown and post (during)-lockdown structures. Pre-lockdown activities were measured as per standard ABC principles; however, some elements of post-lockdown activities had to be estimated on a hypothetical basis by SUH programme staff, as all sites had completed workshop 1 at initiation of lockdown. Nevertheless, the figures provided are intended to be a proof of concept that an ABC exercise could be achieved. They are also indicative rather than definitive, and display two hypothetical extremes of programme design between a fully office-based and a fully remote model of provision. In each case, the programmes include a fixed component of £3747.60 (in both models) and a per-centre component of £2671.00 pre lockdown and £2138.85 post lockdown, the per site breakdown of which is shown in Table 25. Per-centre costs were higher in the office-based model than the fully remote model, which were driven predominantly by the need for travel, longer initial meetings with management, including touring the facilities, and the need to book rooms and set up equipment. However, these were partially offset by additional ad hoc communication and increases in the total time needed per participant in workshops using the remote model, which was caused by consultations requiring an additional ≈ 10 minutes to discuss the nature of each participant’s home-working environment.
| Activity | Pre lockdown (office model) | Post lockdown (remote model) | Notes | ||
|---|---|---|---|---|---|
| Composition | Cost (£) | Composition | Cost (£) | ||
| Equipment | Twenty-one pieces of equipmenta | 2100.00 | Twenty-one pieces of equipmenta | 2100.00 | Assumes replacements required annually. Further important caveats in table notes |
| Website/forum hosting | Annual server costs | 600.00 | Annual server costs | 600.00 | Source: trial invoicing |
| Website/forum development and monitoring | 60 hours of staff timeb | 1047.60 | 60 hours of staff timeb | 1047.60 | |
| Activity costs for 11 centres | Delivery of two workshops, travel, meetings and general communication with sites | 28,804.82 | Delivery of two workshops,meetings and general communication with sites | 23,335.29 | See Table 25 for composition |
| Total | 33,128.60 | 27,274.95 | |||
| Activity | Pre lockdown (office model) | Post lockdown (remote model) | Notes | ||
|---|---|---|---|---|---|
| Composition | Cost (£) | Composition | Cost (£) | ||
| Initial meeting with management | 2 hours, two SUH staff members | 69.84 | 1 hour, two SUH staff membersa | 34.92 | |
| Workshop 1 staff time | 7.5-hour preparation/action plan creation, 7-hour run time, two SUH staff membersa | 506.34 | 7.5-hour preparation/action plan creation, 1-hour run time, two SUH staff membersa | 279.36 | |
| Workshop 2 staff time | 3-hour preparation, 7-hour run time, two SUH staff membersa | 296.82 | 3-hour preparation, 1-hour run time, two SUH staff membersa | 69.84 | |
| Workshop sundries | Sundries (for both workshops) | 135.00 | N/A | – | Posters, stationary, prize support and food |
| One-to-one consultations with staff | N/A | – | Four 1-hour consultations, 30 30-minute consultations, two SUH staff membersa | 663.48 | |
| Report writing for one-to-one consultations | N/A | – | 30 15-minute consultations, one SUH staff membera | 130.95 | |
| Follow-up meeting with manager | 1 hour, two SUH staff membersa | 34.92 | 1 hour, two SUH staff membersa | 34.92 | |
| Travel, accommodation, and expenses | Four visits, two SUH staff membersa | 790.00 | N/A | – | Based on 1- to 3-hour journey. For comparison, ≥ 3-hour journey (i.e. London) is ≈ £850 higher, < 1-hour journey (i.e. local) is ≈ £470 lower |
| Quarterly SUH committee meetings | Four 1-hour meetings, two SUH staff membersa | 139.68 | Four 1-hour meetings, two SUH staff membersa | 139.68 | |
| Other communication | ≈ 45 hours, two SUH staff membersa | 698.40 | ≈ 45 hours, two SUH staff membersa | 785.70 | 1-hour monthly meetings with manager, additional telephone calls, e-mail handling and general co-ordination with sites for workshops etc |
| Total | 2671.00 | 2138.85 | |||
Table 26 shows an approximation of the centre side staff time commitments required to participate in the programme. These are divided into activities that require management time, or at least a designated local SUH lead/authorisation, and activities that would depend on the grades of staff selected to participate (some of whom may also be management). Because the latter included a mix of grades, and per-hour staff costs for a given grade of staff will depend on the organisation adopting SUH, we have not attempted to multiply these by an estimated wage. Staff time requirements were estimated to be doubled in the remote model, owing to the need for participants to watch a 1-hour video and the additional ≈ 10 minutes added to consultations. Similarly, each workshop would also require the use of an appropriately sized room. However, it was not possible for a meaningful price to be applied to this owing to heterogeneity of sites and variability in the opportunity cost of accessing these rooms for other purposes (e.g. meetings) being highly context and locality specific.
| Activity | Pre lockdown (office model) | Post lockdown (remote model) | Notes | ||||
|---|---|---|---|---|---|---|---|
| Composition | Manager specific (hours) | Any staff (hours) | Composition | Manager specific (hours) | Any staff (hours) | ||
| Initial meeting with the SUH team | 2 hours of manager time | 2.00 | 1 hour of manager time | 1.00 | |||
| Workshop 1 staff time | 20 minutes per staff member attending | 11.67 | 1 hour per staff member attending | 35.00 | Assumes 35 staff attending. Typically ranged from 30–40 staff | ||
| Workshop 2 staff time | 20 minutes per staff member attending | 11.67 | 1 hour per staff member attending | 35.00 | Assumes 35 staff attending. Typically ranged from 30–40 staff | ||
| One-to-one consultations with staff | N/A | – | – | 35 30-minute consultations | 17.50 | ||
| Follow-up meeting with manager | 1 hour of manager time | 1.00 | 1 hour of manager time | 1.00 | |||
| Quarterly SUH committee meetings | Four meetings, each with eight staff members, assumes one or more manager | 4.00 | 28.00 | Four meetings, each with eight staff members, assumes one or more manager | 4.00 | 28.00 | |
| Internal co-ordination of rollout | Assumed 30 minutes per week, ≥ 2 hours for workshop preparation | 28.00 | Assumed 30 minutes per week, ≥ 2 hours for workshop preparation | 28.00 | For example, room booking, co-ordination/purchase of equipment, and/or ad hoc correspondence with SUH team | ||
| Other communication with SUH team | Three 1-hour meetings, nine 30-minute meetings | 7.5 | Three 1-hour meetings, nine 30-minute meetings | 7.5 | For example, monthly meetings with manager, additional telephone calls, e-mail handling and general co-ordination with sites for workshops | ||
| Total | 42.50 | 51.33 | 41.50 | 115.50 | |||
Model-scoping exercise
Two areas of health with potential for modelling were identified: cardiovascular and musculoskeletal health.
Cardiovascular
The methodology for economic modelling in cardiovascular health is well established compared with many disease areas. Therefore, many pre-existing models provide a ready list of candidate health states and events for modelling, with associated cost and QALY weightings derived from well-established sources and/or literature review (Table 27).
| Model | Example health states/events | Cost–utility/health utility weight availability |
|---|---|---|
| NICE guideline NG136: Hypertension in Adults: Diagnosis and Management. Cost-effectiveness analysis: treatment initiation threshold for people with stage 1 hypertension. 201998 |
|
UK costs and health utility weights listed for all health states and events. Derived from literature search and/or standard UK price weight sources98 |
| York Health Consortium publish NICE guideline, An Economic Analysis of Workplace Interventions that Promote Physical Activity, PHIAC Report. 200899 |
|
UK costs and health utilities taken from cost-of-illness (per annum) estimates for each non-healthy state. Note that costs were uplifted to a base year of 2007 and, therefore, are out of reasonable date for reuse |
| Gao et al. 2019100 |
|
Australian costs and health utility weights listed for all health states and events derived from systematic review |
At the most complex end of the modelling spectrum, transitions between long-run rates are modelled based on sets of validated risk equations derived from large population data sets, such as Framingham Risk Score(s),96 the QRESEARCH Cardiovascular Risk Algorithm (QRISK) series (which has current NICE recommendation)98 or similar studies. 101 Although such models and equations are published in the public domain to enable their reuse or the reuse of their subcomponents in future modelling, a number of the input parameters for the risk equations underpinning the models require biomarker data, preferably at the individual level. For example, the QRISK3 series includes age, sex, ethnicity, deprivation, smoking status, diabetes status, family history of angina/heart attack, presence of stages 3–5 chronic kidney disease, atrial fibrillation, several variables on current blood pressure treatment and comorbidities, cholesterol/high-density lipoprotein ratio, blood pressure, and height and weight to calculate BMI.
It is possible in some cases to use these equations to estimate the effect of a change in one component of risk holding all others equal if reasonable assumed/mean population values can be found for the other parameters.
However, the challenge at conception of the SUH trial was that several key aspects of these parameters, such as blood pressure, cholesterol or weight, are challenging to record in a trial without direct measurement, which would add an impractical need for physical examination that may deter some participating centres and participants. Hence, such an approach would necessarily rely on more tertiary inputs with smaller effect sizes. Additional barriers to this method include staff turnover and the sharing of equipment, which are not easily measurable. Model scoping for this area, therefore, focused on identifying alternative options for modelling the identified health states that were compatible with the restricted data collection options.
Older modelling has been based around dividing participants into mutually exclusive binary groups of active versus sedentary, and then applying differential relative risks to the development of health conditions. 99 Although this approach is, in principle, simple to apply with a literature review, a more granular breakdown of degree of activity would be desirable where possible.
A recent systematic review by Lutz et al. 102 of economic evaluations of interventions to increase workplace physical activity and decrease sedentary behaviour found 18 studies, including one (also recent) fully modelled study by Gao et al. 100 which may provide a pragmatic approach. 100 Gao et al. 100 provide a Markov model of different workplace interventions to reduce standing time. Differences in energy expenditure were estimated for each intervention based on meta-analysis of changes in standing time, converted via metabolic equivalent units, a measure of estimating energy expenditure derived from body weight and increase in physical activity/standing time. Population-level rates of coronary heart disease and/or stroke, and associated outcomes, were then adjusted for relative risks of associated with estimated improvements in energy expenditure. A similar approach may be possible utilising metabolic equivalent unit-based on activity accelerometer data. Although the relative risks reported may not all be applicable to the specific SUH style of intervention or accelerometer data, the same method could be applied, potentially using a new or updated meta-analysis. Owing to the acknowledged impracticality of physical examination(s), some assumptions around the use of population-level weight/BMI may still be necessary, but this has the advantage of focusing on the most directly modified aspect of cardiovascular risk of a SUH-style programme. The model also includes Australian health-care perspective costs and QALY waiting sets for the health states, although UK equivalent remain available for substitution (see Table 27) or could similarly be derived by fresh/top-up review.
Although, in principle, significant cardiovascular events would reasonably have long-term implications for absenteeism, presenteeism, engagement and staff turnover (the primary areas of interest identified from an employer’s perspective from the consultation exercise detailed in Qualitative survey of prospective outcome measures from an employers’ perspective), modelling these may be challenging. The health states and events identified are low frequency, long-term outcomes. For this reason, meaningful differences may be observable at a population level only, and a given employer is unlikely to observe modifiable differences in their targeted metrics. It is not implausible that there could be behavioural changes in staff turnover and engagement when staff are aware of the impacts of sedentary behaviour on long-term health and make conscious efforts to avoid it. However, these may be better examined within trial using the methods discussed in Qualitative survey of prospective outcome measures from an employers’ perspective above.
Musculoskeletal
To identify candidate health states and other parameter data to populate a model, physical activity experts within the team were asked for details of any known literature relating to musculoskeletal disorders caused or worsened by office working that were plausibly modifiable by a SUH-style programme. Specific focus was given to matters that might reasonably alter productivity, absenteeism, health-care resource use and/or quality of life and, thus, justify categorising as a ‘health state’ in a simulation model. Further ad hoc literature searches were carried out for studies of economic burden, cost of illness, cost–efficiency/–utility and/or long-term modelling of musculoskeletal disorders in a work/office environment.
Potential modifiable health states identified two main categories of outcomes commonly applied by both fields of literature to group disorders:
There were also plausible links to their development being in part because of combinations of ergonomics, prolonged sitting and computer use. 103 Should a programme be able to demonstrate an ability to modify the appropriate risk factors and appropriate other parameter data available, this provides a potentially plausible mechanism to model long-run musculoskeletal disorders health state trajectories. Alternatively, one model of long-term musculoskeletal disorder absence grouped employees into health states denoting 6-monthly increments of absence rather than medical cause, and simulated cost-efficiency of different workplace interventions based on differences in rates of return to work reported in the literature. 106
In general, attempts to locate usable economic literature highlighted some challenges. The terms back or upper limb pain can be used to refer to a range of heterogeneous symptoms104 and searches can be confounded by a number of other conditions, including work-related pain as a result of non-office activities, such as manual labour and associated arthritis. 105 Crucially, patients’ treatment for a different form of pain may follow a different profile of health-care resource use or QALYs and, at least within the economic literature, there was no obvious common lexicon used to categorise degrees of severity of symptom. Hence, in addition to an increased degree of complexity needed in literature searching, synthesising data from multiple sources into common health states may be more challenging than in cardiovascular health and it may be advisable to aim to build health states around results from a singular study, in which we can be more confident that health-care resource use and health-utility weightings reported are attributable to the same patient group.
Cost-of-illness surveys, which have the potential to offer broader categories of care depending on study design, wielded few UK studies, with a recent systematic review107 of methodology of cost of illness work for back pain identifying only three UK studies. Two of these were over 20 years old and potentially not reflective of current care108 (including the primary health-care resource use source for the long-term absence model106,108) and the third was from 2013, but available in abstract only. 109
Several musculoskeletal disorder trials including cost–utility components were found, including recent UK-based trials in which health-care resource use are likely to be most relevant and/or trials using UK-based health-utility tariffs from the EuroQol-5 Dimensions (EQ-5D) or Short Form questionnaire-6 Dimensions tool groups. 110 Those with UK health-care resource use did provide detailed breakdowns of care, the most promising of which provides EQ-5D utilities and health-care resource use profiles for groups of patients defined using the Roland Morrison Disability Questionnaire111 as being at low, medium or high risk of developing long-term disability. 110
Therefore, although on face value there appears to be a reasonable evidence base to populate a potential model, the need to synthesise evidence from a heterogeneous literature base may provide challenges, and the specific model structure may be best selected in part to fit the available parameters rather than derived top down, as was attempted here. Such an approach may be better started with a systematic review, which was beyond the scope of this study.
Time horizon considerations
A key assumption for modelling is that any modelled benefits are sustained beyond the observed duration. Gao et al. 100 apply an assumed 5 years based on previous modelling in the wider area of public health100,112 and note an absence of evidence of decaying effects;100 however, to our knowledge, this assumption has not been validated and an absence of evidence cannot rule it out. 100,112 Similarly, any modelling of a SUH-style programme would need to take into account staff turnover, as those who change jobs would not have a continuation of SUH unless by chance a similar programme was in place in their next employment. A simple solution to this would be for a model to instead solve for the minimum duration of continued benefits needed for the intervention to be cost-effective.
Value-for-money considerations
Although potential options for modelling cardiovascular health and musculoskeletal disorders were identified, both would rely on some form of systematic, or at least in-depth, review to identify the most suitable parameters. Such reviews are often time-consuming and costly aspects of research, and need to demonstrate likelihood of value for money. Any intervention that increases costs needs to offset these with sufficient effect size if it is to be considered not only cost-effective but also effective.
Although the trial was never powered to be definitive, it was hoped that at least a broad indicator of the direction and degree of activity improvement might be achieved at this stage, around which at least subjective judgement of the potential value of modelling could have been speculated. Unfortunately, COVID-19 disruptions prevented this. With broader literature on programmes to improve office-based physical activities having mixed results, depending greatly on the nuance of the specific intervention method,102,104 an argument can be made that such modelling should be deferred until a programme has successfully demonstrated an element of effectiveness to minimise potentially sunk research expense.
Summary of findings and recommendations
The proof-of-concept ABC exercise was broadly successful, indicating that doing so in a future trial would be expected to be feasible. The small number of factors not measured owing to COVID-19 disruption primarily relate to items for which there are limited reasons to doubt future measurement; the only notable potentially uncertain aspect was site adoption/purchase of their own equipment after initially borrowing demonstration equipment from the SUH programme. This became a moot point owing to lockdowns initiating early in this process and sites needing to prioritise adaptation to home-working arrangements. We were, however, able to estimate costs of the SUH programme equipment; therefore, if rates of purchasing of equipment can be obtained, there is no reason to believe that they cannot have costs attributed to them.
We were also able to repeat the ABC under a remote delivery model, albeit in a post hoc design. However, comparisons between models may be premature owing to small samples and simplified methodology. However, they may be treated as an early indicator of differences and point to higher cost of delivery in a face-to-face setting because of the need for travel, longer initial meetings with management and touring of facilities, and the need to book rooms and set up equipment. These were partially offset in the remote model by increased communication time and time per participant in workshops to discuss the nature of each participant’s home-working environment.
Some elements of centre side costs, such as the ‘value’ of a minute of staff time or the opportunity cost of room use, were too heterogeneous between sites to apply a single pricing structure. Although measurement appears viable and consolidating these into a single ‘total cost’ metric may be desirable from a theoretical perspective, doing so may give a misleading sense of accuracy. The raw rates of use, that is one suitably sized room for the number of staff attending (which will vary by site), and estimates of the minutes of staff time (per staff) needed to attend are probably more relevant to sites themselves to allow them to apply their own context. Hence, a more piecemeal and descriptive approach to reporting may be warranted.
Absenteeism, presenteeism, staff turnover and engagement were identified in our qualitative surveying of sites as desirable outcomes for a future trial from an employer’s perspective. Although absenteeism and staff turnover were measured relatively consistently between sites, and in a manner consistent with human capital methodology, presenteeism and engagement were not. Although this was anticipated to be the case, no common metrics of productivity (which would capture important implications of presenteeism and engagement) were identified between sites. There was, however, a general acceptance that, although these metrics were desirable, they were less tangible and, therefore, less-precise measurement methods may be more acceptable to sites. Alternative means of measuring productivity may be necessary, such as surveying management using Likert scales denoting perceived change in staff productivity, asking them to state a percentage change in productivity based on their metric of choice, or conducting some form of discrete choice experiment.
Not all sites reported being willing or able to share internal productivity/absenteeism data, and we were unable to access data from those who were. The latter was primarily owing to sites not responding to requests. Although it is never possible to be certain, it is likely this was primarily because of the sites needing to prioritise change to home working, with some specifically stating that such data would be too skewed by COVID-19. Nevertheless, even if we had been able to scrutinise these data to assess the variables available, data would not have been available from many sites; in addition, the other survey responses hinting heterogeneity on non-absenteeism/staff turnover outcomes suggest that this approach may be of limited value.
Two areas of health with potential for modelling were identified: cardiovascular and musculoskeletal health.
Economic modelling is from an NHS and PSS perspective and is well developed in the field of cardiovascular research in general, with many candidate models and sources for cost and health utility parameterisation available. Linking the underlying clinical core of the model to sedentary behaviour is more restrictive, although a promising Markov model approach based on changes in muscular metabolic equivalent units100 was located raising the possibility of a similar method based on the activity accelerometer data. Modelling of cardiovascular health appeared less meaningful for outcomes identified from an employer’s perspective (absenteeism, presenteeism, engagement and staff turnover); given that the health states and events identified were of low frequency, very long-term outcomes were probably observable at a population level in terms of hard outcomes only. Passive knowledge of their risk, however, might plausibly change staff behaviour; therefore, efforts by organisations to provide fitness or well-being measures may be motivational. However, measurement of such factors may be better dealt with using the within-trial methodologies described above.
Modelling in musculoskeletal health, on the other hand, spanned both the NHS/PSS and employer perspectives but suffered from a high degree of heterogeneity of symptoms/health states covered and modelling approaches. There were also plausible indications that the development of musculoskeletal disorders was in part due to combinations of ergonomics, prolonged sitting and computer use. 110 Therefore, should a programme be able to demonstrate an ability to modify these, there is a potentially plausible mechanism to model long-run health state trajectories from. However, the specifics of this would be better designed around the nature of the risk factor being adjusted and would realistically require a bespoke targeted literature review to populate, if possible at all.
The available cost-of-illness studies were generally out of date, despite several trials being identified, including cost–utility approaches and breakdowns of UK health-care resource use, as would be needed for an NHS/PSS perspective. Linking these to employer-perspective outcomes may be substantially more challenging, with one of the more promising models that considered absenteeism ignoring health state categories altogether in favour of 6-monthly increments of absence, and simulating cost-efficiency of different workplace interventions based on differences in rates of return to work reported in the literature. 112 Such an approach offers at least a proof of concept that modelling is possible, although this would be as a standalone model not necessarily utilising any of the methods or data scoped for the SUH study.
All model structures considered would appear to be heavily reliant on systematic or at least highly detailed reviewing to populate. Such reviewing has the potential to be a time-consuming and costly aspect of research and a sunk cost if undertaken in parallel with an intervention that ultimately proves to be ineffective at modifying underlying risk factors. Future modelling may, therefore, be better deferred until after an intervention that is effective is found. This would also allow the review to target specific searches for literature around the area of health improved.
Chapter 6 Discussion and conclusions
Introduction
This study evaluated the feasibility and acceptability of a theory-informed intervention to decrease sedentary behaviour in contact centres. It also evaluated the acceptability and feasibility of the research design and the outcome measures. We had previously developed and piloted the SUH intervention in one contact centre in Edinburgh and wanted to test and refine our programme theory, as well as test out the trial design in other contact centres. To meet these aims, we delivered the intervention in multiple centres and then undertook a process evaluation, a feasibility study of the trial design and measurements, and a scoping study for a full economic evaluation.
The research questions primarily focused on measuring the feasibility of the research design and the intervention itself. However, sedentary behaviour (during work as measured by the activPAL device) was assessed as a potential primary outcome for a full evaluation. Other health outcomes included subjective measures of sedentary behaviour, mental well-being and musculoskeletal health. Non-health outcomes (which would potentially drive the support and implementation of the intervention in workplaces and are a measure that can be used in a future economic evaluation) included productivity, absenteeism and presenteeism.
The main study findings were considered in the following section in relation to the study objectives and the trial progression criteria. Key learning points and considerations for a future evaluation will also be discussed.
Principal findings
As mentioned in earlier chapters, delivery of the planned study intervention and some of the data collection was affected by the outbreak of COVID-19. This was mainly because of the influence of lockdown, which shifted much of office-based working to home-based working. It also meant that the researchers were not able to travel to sites as planned. This affected the study in three main ways:
-
the development of the intervention activities with staff
-
the delivery of intervention activities to staff
-
data collection (particularly in relation to the activPAL data).
Table 28 provides an overview of the progression criteria that were met. The progression criterion (number 1) for the reduction of sedentary behaviour was not met. All other criteria were partially or fully met. Although effectiveness is always the aim of any intervention, the process evaluation showed that the intervention is acceptable and sustainable (with the potential to be more effective as the organisational culture embraces and enhances the activities).
| Progression criterion | Was the progression criterion achieved? |
|---|---|
| 1. A 95% CI for the primary outcome includes a clinically relevant reduction in sedentary time of ≥ 45 minutes per day in favour of the intervention. This would reflect substantial progression towards accumulating the recommended quantity of 2 hours per day of standing/light activity during working hours for employees in predominantly desk-based occupations | No. For the pre-lockdown analysis, the 95% CI for the difference in daily sedentary time in the workplace was from –3.62 to 124.27 minutes greater for the intervention group. Therefore, given that this CI does not contain –45 minutes (indicating a reduction in favour of the intervention), this progression criterion has not been achieved. For the post-lockdown analysis, no device-measured sedentary time was measured. However, based on the OSPAQ (minutes sitting per working day), the CI was from –11.39 to 46.78 minutes, which, again, did not include the –45-minute reduction in sedentary time. Nevertheless, both the pre-lockdown and the post-lockdown analyses were subject to potential bias |
| 2. The intervention was successfully delivered in at least five of the sites within the study period, and at least one person in each site was able to use/experience at least one activity | Yes. The intervention was successfully delivered in six sites pre lockdown and at least one person in each site was able to use/experience at least one activity. We also recruited one additional site post lockdown |
| 3. Primary and secondary outcome data were collected in at least 75% of participants overall. | Partially. Out of 155 participants recruited and assigned a participant ID pre lockdown, all of them provided at least some secondary outcome data and 152 (98%) provided valid data on the key secondary outcome of the OSPAQ. For the activPAL device-measured primary outcome, however, only 116 (74.8%) participants had primary outcome data collected and there were only 94 (61%) who recorded valid data suitable for analysis |
| 4. Contamination between sites is low or else it is envisaged that contamination can be addressed in the study design of a future study | Yes. None of the participants reported that they previously worked for a company that used the SUH intervention in either the pre-lockdown or the post-lockdown data collection periods. Although we accept that our pre-planned stepped-wedge design could not be fully achieved, based on the lack of evidence for contamination observed, we expect that contamination would be very low in a future cluster-randomised trial in this setting |
| 5. It is envisaged that any practical difficulties in delivering the intervention across multiple sites or in measuring effectiveness can be overcome when conducting a future large-scale study | Yes, provided that a future trial is designed differently. We think that the stepped-wedge design will be too difficult to achieve on a larger scale owing to the difficulties in maintaining site interest (e.g. if they are randomised to receive the intervention 12 months later) and ensuring that data collection takes place on schedule. Instead, we suggest that a parallel-group cluster-randomised trial in which sites are recruited in pairs (or groups) over time would be more practical |
Aim 1: to test the acceptability and feasibility of implementing the Stand Up for Health intervention in contact centres
Research questions for aim 1
What is the acceptability, feasibility, and utilisation of the various components of the intervention in a range of contact centres?
For the pre-lockdown programme, process evaluation findings showed that the staff members found the activities at the individual, social and environmental levels acceptable, and at least 50% of all contact centre staff took part in at least one activity. This high level of engagement is probably because of the adaptative nature of SUH, and its focus on ownership and co-production. The adaptive nature of SUH meant that preferences and contexts were considered when developing the activities, and further activities were developed as SUH became more embedded in the culture and systems as staff and management started to see positive changes to their working lives. These were not always related specifically to changes in sedentary behaviour but more of a healthier workplace culture and environment. The barriers to delivery in some centres stemmed from lack of communication between SUH team and centres, as well as between individuals and teams within centres, not setting up a SUH committee, and lack of strong buy-in at the organisational level.
Does the programme theory and process of implementing the intervention work as intended?
The initial draft of the SUH programme theory was based on data from the pilot centre (see Figure 2). Although the outcome evaluation did not yield adequate evidence, the pre-lockdown process evaluation results indicated that several aspects of the programme theory were supported. Pre-lockdown process evaluation findings showed that, for most centres, the SUH programme triggered changes at each of the levels (organisational, environmental, social, individual, ownership and information). Figure 12 highlights the aspects of the programme theory model that were supported by process evaluation data. In some centres, the mechanisms of change were not activated and the reasons are discussed in detail in Chapter 3. Lack of communication (between the SUH team and the centres, as well as between individuals and teams within centres), not creating a SUH committee and organisational rigidity in some centres (centres 2 and 6) had a negative effect on ownership and awareness about the programme, sedentary behaviour and physical activity among staff. These factors also impacted individual, environmental and social levels and overall programme success. Two new medium-term outcomes were identified: increased physical activity outside work and the adoption of a healthy diet.
FIGURE 12.
Refining programme theory: pre lockdown. Note that the figure does not include outcome data as data collection was incomplete and did not provide evidence to accept or refute hypotheses.
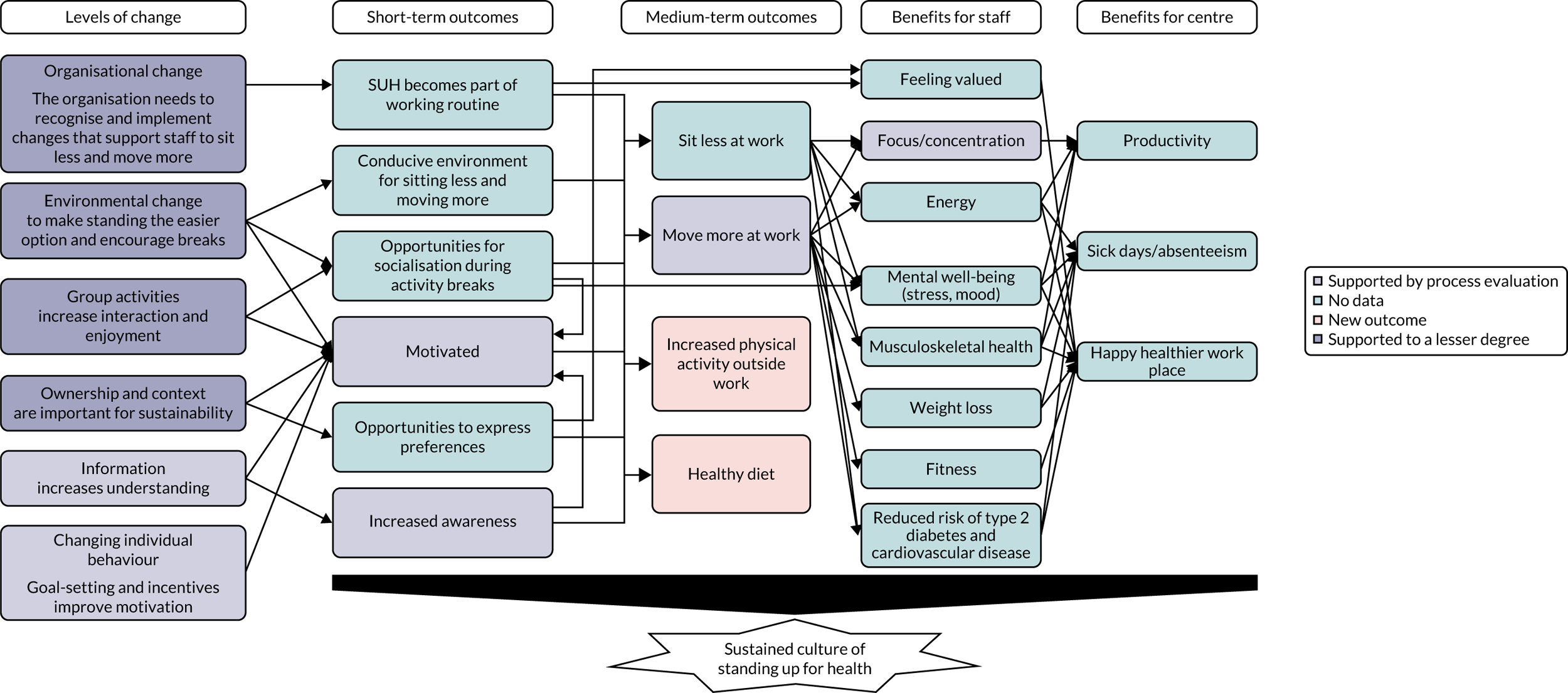
During the post-lockdown period, several contact centre staff members were working from home. Although the initial programme theory model and activities were not designed for home working, the programme was adapted to suit the new working pattern. However, the post-lockdown process evaluation results showed that the mechanisms of change at all levels of the programme theory model were activated to a lesser degree than pre lockdown (Figure 13). In particular, post lockdown, the SUH programme did not produce a strong change with respect to organisational, social and environmental levels, or create a sense of ownership among staff. An improved understanding of activities that trigger changes at these levels is required to set the mechanisms of change in motion for staff working from home. Adopting a healthy diet was identified as an unintended consequence and a medium-term outcome for the post-lockdown programme also.
FIGURE 13.
Refining programme theory: post lockdown.
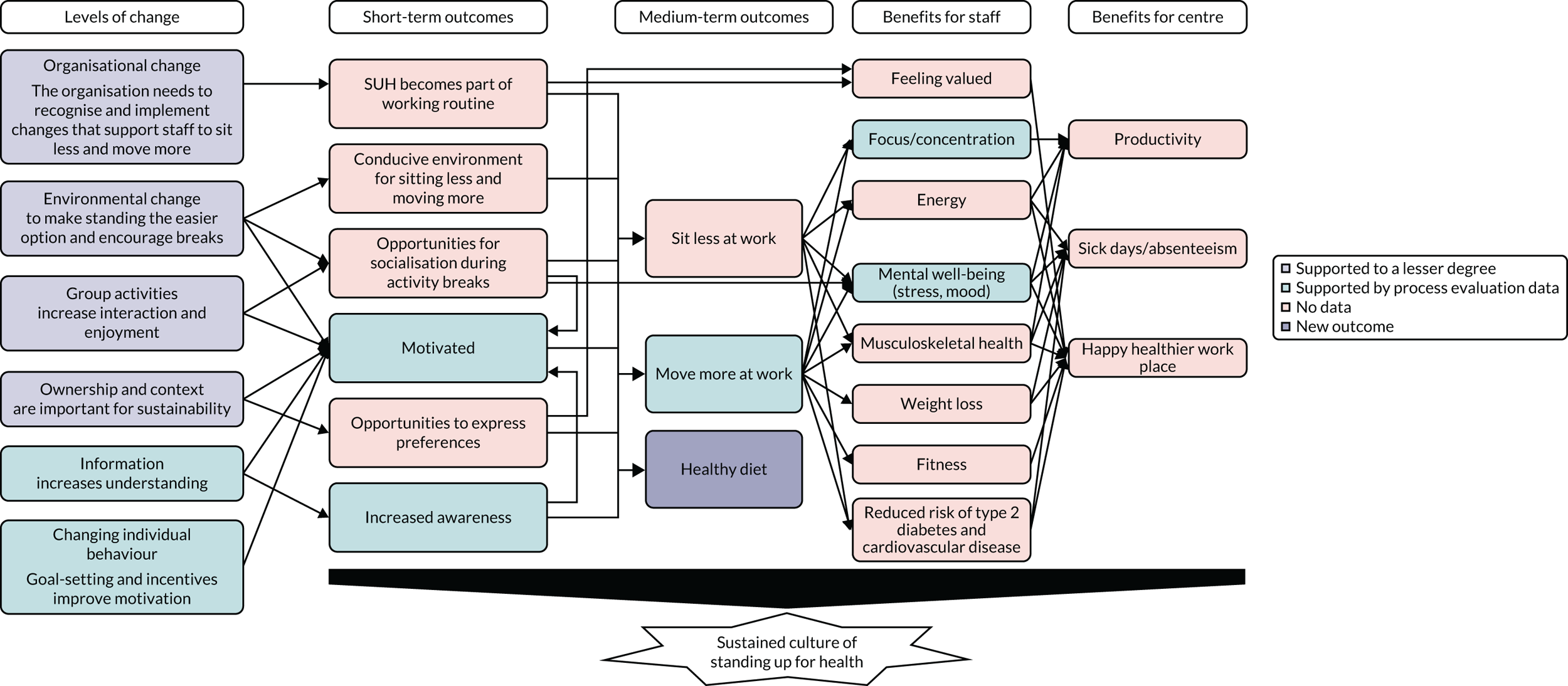
Does the programme theory/intervention need adapting and if so, in what ways?
Although the pre-COVID programme theory worked as intended, the SUH programme could not achieve change at some levels during the post-COVID programme. More work is required to understand the hybrid working models and refine the programme theory in accordance with these. Working with contact centres during the COVID-19 pandemic provided an opportunity, and we are now at the forefront of thinking about these new models in the context of workplace health interventions.
Are there differences in delivery of the intervention between different contact centres? If so, what are the reasons for these?
There were differences found in the delivery of the intervention between contact centres. Some identified reasons were communication, the existence (or not) of a SUH committee and organisational support. Effective communication and co-ordination between the SUH team and the centres, as well as between individuals within centres, aided implementation. The SUH committee created a sense of ownership among staff and supported implementation activities. Centres that had these elements saw more successful implementation. Organisational support was also a key element to successful implementation, and rigid organisational structures and bureaucracy were posed as barriers to implementation.
Can Stand Up for Health be adapted for those working remotely, and what is the acceptability and feasibility of this mode of delivery?
The intervention was successfully adapted for online delivery by replacing the in-person workshops with online consults and conducting the step count challenge to address the social level. Several resources for individual activities were also provided, including mindfulness and other online resources to reduce sedentary behaviour and increase physical activity. The process evaluation findings from the post-COVID programme showed that staff members found the activities at the individual and social levels acceptable and feasible.
The data indicate that SUH can be adapted successfully for hybrid working. However, more activities are required to trigger the environmental and organisational levels of change and maximise participant engagement. A greater understanding of working from home is required to adapt the programme theory for hybrid working.
Aim 2: to assess the feasibility of using a cluster randomised controlled trial study design
Is the study design (cluster RCT) feasible for a confirmatory trial of an intervention to reduce sedentary behaviour in staff working in contact centres?
Research questions for aim 2
What is the recruitment rate of participants in each cluster and how many are lost to follow-up (e.g. because of staff turnover)?
There were between 21 and 33 participants recruited per centre across six centres (mean 25 participants per centre). After recruiting participants in the pre-lockdown period, four of the centres agreed to participate in the post-lockdown programme (approximately 10–12 months later). Regarding loss to follow-up, there were 12% recorded as having left the company after the pre-lockdown data collection, and there were an additional 22% recorded as having moved jobs within the same company after the pre-lockdown data collection. Only 61% of participants recorded valid activPAL data at baseline, although a greater proportion recorded OSPAQ data (98%).
How many clusters and participants per cluster are required for a confirmatory trial?
For the primary outcome (total sedentary time in the workplace per day in minutes), the overall coefficient of variation was 0.12, and the within-site SD was 100.08 minutes overall and 96.04 minutes at baseline (see Table 21). In addition, the mean value of the primary outcome at baseline was 359.6 minutes, and we recruited a mean of 15.6 participants providing valid primary outcome data per cluster (see CONSORT flow diagram in Figure 6). Therefore, using equation 6 shown in Hayes and Bennett,93 we calculate that we need 25 clusters in a future cluster-randomised trial to detect a clinically relevant difference in sedentary time of 45 minutes with 90% power and two-sided 5% significance level. We suggest that a future cluster trial, with clusters recruited in pairs, would have a low cluster-level dropout rate of 10%, because in this study design clusters would not have to wait long to begin the intervention. We, therefore, suggest that a future trial should aim to recruit 28 clusters, taking centre-level drop-out rates into account. We also recommend that a future trial aims to recruit 40 participants per centre on average to use the activPAL device and to have at least 15 or 16 participants per centre recording valid primary outcome data.
Are the range of study procedures (e.g. recruitment strategies and outcome measurement tools) feasible for a future confirmatory trial?
Although the recruitment strategies generally worked well, they were dependent on the level of involvement of main point of contact at the centres. The subjective data collection using surveys was feasible, but the collection of device-measured data using the activPAL device was not logistically feasible, particularly when in-person visits to the contact centres stopped during the pandemic. This was because of the number of participants needing to record their activity at any one time and the number of activPAL devices needed (at peak data collection times the number being actively used was 54); in a large trial this number would increase significantly. The time and co-ordination, as well as the risk of damage to or loss of the devices (which cost about £200 each), would create barriers to their use.
Although focus groups provided rich insight and generated good discussions around intervention and data collection experiences, it was difficult for the research team and the centres to arrange them because only so many staff could be off the telephones at once. In a future evaluation, small group or single interviews may be a better way of collecting data. It may also be useful to consider other qualitative methods, such as art-based approaches (e.g. photo elicitation).
Are there differences in aspects of study procedures (e.g. uptake) between different contact centres? If so, what are the reasons for these?
From our experience, we did not perceive any significant differences in study procedures between the different centres. However, when centre points of contact were engaged in activities, such as recruitment and advertising, the uptake increased.
What are the preliminary estimates of the variability of primary (reduction of sedentary behaviour in the workplace) and secondary outcomes within and between contact centres?
Empirical estimates of SD and coefficients of variation were computed for the pre-lockdown analysis (see Table 21). High values of kappa indicate high levels of between-centre variation. The results suggest that device-measured total sedentary time exhibits potentially low levels of between-centre variation.
Is it feasible to adopt an online format and does this affect the use of a stepped-wedge study design? Does the mode of delivery impact on the feasibility of the study design (online vs. face-to-face delivery)?
Given that we were unable to collect the data as per the original stepped-wedge design, we are unable to comment on this. Post-COVID data collection collected only baseline and 3-month follow-up data and did not follow the original data collection timeline. With respect to data collection measures, the activPAL devices were not used during post-COVID data collection because sending out and ensuring accurate use of these devices was not feasible.
Aim 3: to scope the feasibility of a future health economic evaluation of Stand Up for Health
Research questions for aim 3
Is it feasible to provide estimates of the cost-efficiency of Stand Up for Health from (a) an NHS and Personal Social Services perspective and (b) an employer’s perspective?
We were able to identify feasible methods for estimating cost-efficiency from an NHS and PSS perspective (NICE reference case specification). This requires a mathematical modelling approach owing to within-trial data collection limitations and the need to account for long-term outcomes beyond the trial period. Candidate approaches for modelling cardiovascular and musculoskeletal health were identified, with options to model both. Both approaches necessarily add what may be seen as sizable caveats and would require systematic reviewing to populate parameters to minimise loss of validity. Such reviewing has the potential to be a time-consuming and costly aspect of research. To prevent modelling potentially incurring a sunk cost and, therefore, poor value for money, it may be preferable to defer modelling until a more reliable (unconfounded by COVID-19) indicator of a possible effect is demonstrated in any hypothetical future studies. Since the modelling approaches identified at least appear adaptable to any context, this has the additional advantages of allowing time for home-/office-/hybrid-working practices to become better established, and any future similar programme be adapted to whatever arrangements or set of arrangements become the status quo.
Work from an employer’s perspective may necessarily require a more piecemeal approach. Responses to our survey of desirability of employer’s perspective outcome were poor because of centres needing to prioritise adaptation to COVID-19, hence our results are more speculative than planned. Nevertheless, some loose similarities in responses may be useful. Those who responded reported using varying metrics aspects, such as productivity and staff turnover; however, the easier-to-calculate aspect of absenteeism appeared to follow an approach consistent with human capital principles, whereby absenteeism was measured in terms of percentage FTE lost. There was an absence of common ‘hard’ productivity measures, such as call time, that were used by all centres, and recognition from respondents that subjective measures, such as presentism or engagement, are necessarily more challenging to quantify or accurately cost. Therefore, although these are largely considered desirable, centres may be more open to lower grades of evidence on these aspects. Offering data on a range of metrics rather than a consolidated financial cost is likely to be beneficial. This has the additional advantage of enabling centres to interpret each metric in their own context and may be viable to measure within trial through surveying of centres and/or team leads directly to optimise credibility. However, it is noted that methods for modelling at least absenteeism and staff turnover among musculoskeletal health also appear possible, if challenging, and come with the same caveat that deferring to a later stage of research may be worthwhile.
Detailed ABC of direct intervention costs, which would be an important component for either perspective, was achieved with minimal caveats and, therefore, deemed feasible. Of note, elements of centre side costs, such as the ‘value’ of 1 minute of staff time or the opportunity cost of room use, were deemed too heterogeneous between sites to apply a single pricing structure to. Although consolidating the cost of these may be desirable from a theoretical academic perspective, doing so may give a misleading sense of accuracy. The raw rates of use, that is one suitably sized room for the number of staff attending (which will vary by site) and estimates of the minutes of staff time (per staff) needed to attend, are probably more relevant to sites themselves, enabling more meaningful local interpretation.
Aim 4: consider previous aims under the context of COVID-19
The post-COVID-19 programme has been discussed in detail within aims 1–3 above. The post-COVID-19 period was challenging for the contact centres, many of whom were struggling to set up new systems of working while being busier than usual. Despite this, several activities were implemented and were found to be acceptable within certain levels of change (such as the step count challenge and consults). However, it was challenging for the post-COVID-19 programme to create significant changes at the environmental and social levels. For this reason, further work is required to explore how to adapt the programme to ensure that it is suitable for organisations with hybrid workers. It is possible that our contact centres have tried more than ever to support well-being (or at least staff engagement) but that taking part in a formal research trial was too much of a commitment or their focus was on something else (e.g. mental health or more basic staff engagement).
Strengths and limitations
Strengths
The intervention was co-produced with significant input from contact centres and their staff from the outset. It was developed with them and for them and used the 6SQuID intervention development framework. It was piloted in one contact centre, and the intervention has been sustained in that centre for over 3 years now. To enable the intervention to be adaptive and respond to both the opportunities and the constraints within individual contact centres, we stressed fidelity to the theory of change rather than the theory of action. This is a significant departure from most interventions, which stress fidelity to a particular activity and can specify how often, who by and how much of an activity is needed. From initial conversations with the contact centre, it was obvious that this approach would not work to make it sustainable and acceptable over the longer term. Instead, we worked with them to develop activities and approaches that were adaptive and could be implemented to fit in with the system constraints, such as budget, shift patterns, the working environment and the contact centre culture. We believe that creating an adaptive intervention that contact centres could feel proud of and take ownership of was key to successful implementation in some of the contact centres.
In terms of the research design, we used a mixed-methods approach to assess the feasibility and acceptability as well as the potential impact of the intervention. Rigorous methods were used for data collection and analysis of this feasibility trial, including device-based measures to assess sedentary behaviour and self-report measures for other outcomes. Methods to inform a future cost-effectiveness analysis were also identified.
The process evaluation aimed to explore the feasibility and acceptability of the intervention and trial methods as well as to obtain feedback on and suggestions for improving the intervention and adapting the programme theory. The qualitative methods were robust and the large number of interviews and focus groups gave extensive, in-depth accounts of the experience of the intervention. Further strengths of the trial were that 3 out of 4 key progression criteria were achieved (at least partially), recruitment rates were adequate, retention was good and engagement with the intervention was acceptable.
Limitations
A key limitation was the study design, which we would not consider for a larger evaluation study. The stepped-wedge design, although pragmatic and cost-effective, presented challenges in maintaining engagement with the centres and their staff, and ensuring that the intervention start times followed the complex, pre-planned timeline. Owing to the long study duration, there was also an increased risk of contamination and dropout.
Limitations of data collection included the use of activPAL devices and organising focus groups for the process evaluation. The use of activPAL devices was not logistically feasible, particularly when in-person visits to the contact centres stopped during the pandemic. Although focus groups provided rich insight and generated good discussions around intervention and data collection experiences, it was difficult for the research team and the centres to arrange them as only so many staff could be off the telephones at once. This was also an issue for implementation of the intervention.
Limitations of the intervention included the time that it took for implementation and the communication and promotion of the intervention and specific intervention activities. Implementation of the intervention involved running two workshops with each centre (open to all staff), as well as various meetings with stakeholders and with the SUH committee. These implementation activities required substantial staff time, which was often scarce in productivity-driven contact centre environments, in which a certain number of staff needed to be on the telephones at all times. It was challenging for staff to partake in non-desk-based SUH activities because their shifts were quite rigid and they had little flexibility for taking time away from their desks. Communication about, and promotion of, the intervention took an unexpected amount of time and co-ordination between the researchers and the centres, and also within the centres themselves. For some centres, it was challenging to ensure that communication was received by all levels and to effectively promote the intervention, especially during the COVID-19 pandemic.
If SUH is to be evaluated in a larger study, a more traditional trial study design and more flexible approaches to intervention implementation and data collection would be used, taking into account the specific needs and context of each participating contact centre. The intervention implementation and data collection activities that require interaction between the researchers and the centre staff will be offered at various times of day, more frequently and for longer chunks of time so that they are more accessible for staff who may be busy. The researchers will work with each centre to determine what dates and timings work best for them. Interviews may be used instead of focus groups so that only one staff member is removed from the telephones at once. In addition, more attention will be paid to the SUH website in attempting to engage staff in intervention participation.
Maximising the impact of our findings: dissemination
We have already taken a number of actions to disseminate our findings. First, in addition to our published protocol,67 we plan to publish at least two more open access papers: an overall outcomes paper and a qualitative paper that includes the analysis of the 64 consults we completed with contact centre staff during the COVID-19 pandemic, after the research team were forced to shift to online intervention implementation and data collection. Our paper on the programme theory (developed during the pilot phase) is currently under review.
We have already presented our study at five conferences: Scottish Physical Activity Research Connections (2019, 2020), International Society of Behavioral Nutrition and Physical Activity (ISBNPA; 2020, 2021) and the School of Health in Social Science Postgraduate Conference, University of Edinburgh (2021). We have also recently presented at two further conferences: Centre for Exercise, Nutrition, and Health Sciences, University of Bristol (22 April 2022) and the Invited Speaker Series, Centre for Organisational Health and Wellbeing, Lancaster University (13 May 2022).
On 14 May 2021, the research team hosted an online event celebrating the end of the study, at which we shared findings and discussed future health priorities for the contact centre industry. We had speakers from contact centres share their experiences of participating in the study, as well as experienced public health professionals. The event was open to the public, and anyone interested in sedentary behaviour or workplace health was encouraged to sign up via our academic and non-academic networks, especially staff from contact centres that participated in the study. The event was illustrated live by a professional illustrator (Figure 14) and was a success. We received lots of positive feedback, and it outlined what a positive impact the programme had on the contact centres that participated, from their perspective and in their own words.
FIGURE 14.
Illustration from SUH event, used with permission from Joel Cooper. Ilustration by Joel Cooper.
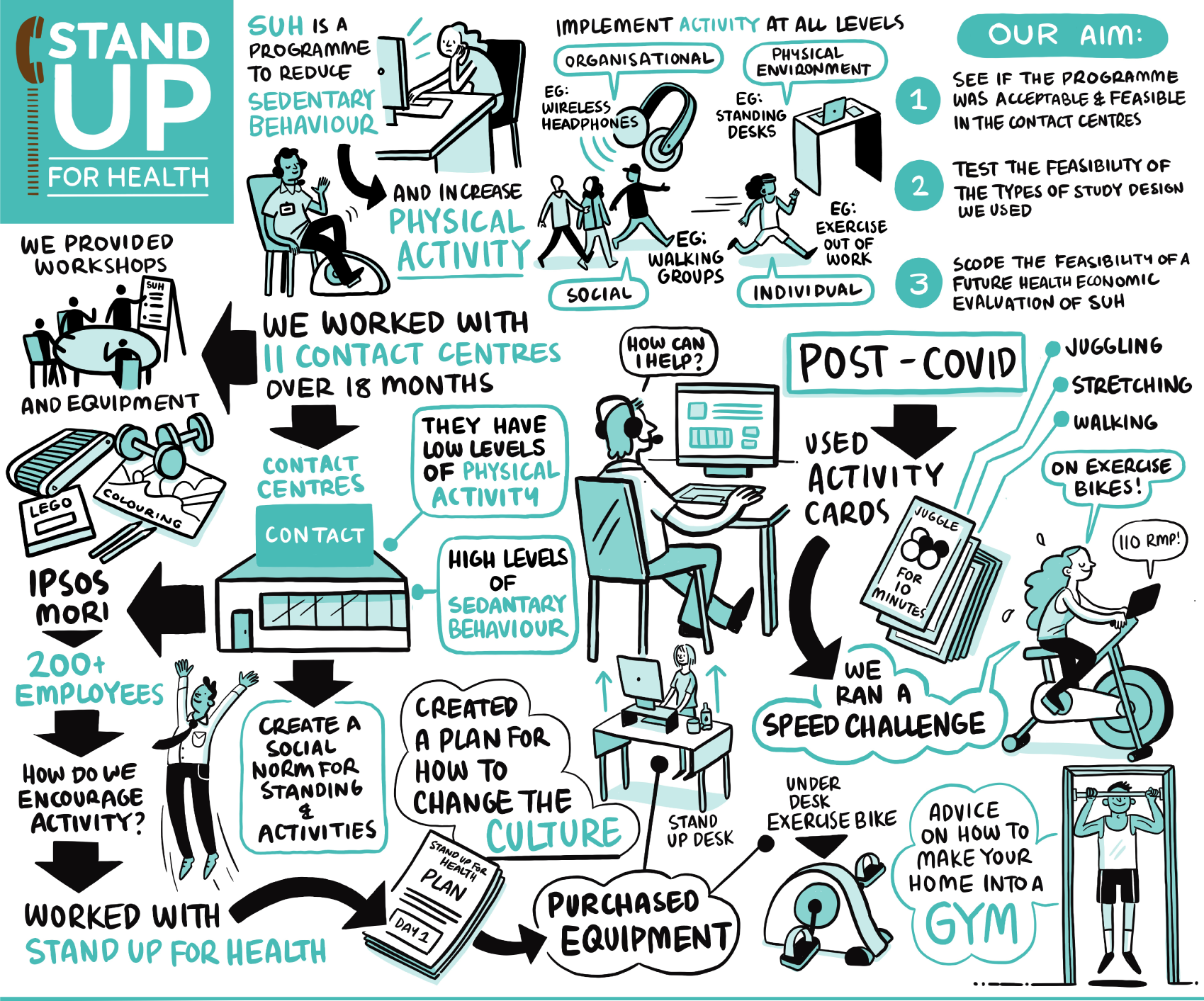
Implications for policy and practice
Since we started developing and evaluating the SUH intervention, there has been a sizable shift in where and how contact centre staff work (this is similar for much of the desk-based UK workforce across the whole economy) owing to the impact of national and local lockdowns. When we started this study, all of the contact centres had a physical site at which employees came to work. Our programme theory assumed that this would remain the case for the foreseeable future. Many of the activities that we had developed for the contact centres were based on a central space in which equipment could be shared, policies and procedures standardised, and social events could take place.
The lockdown meant that contact centres, as with other workplaces, had to either fully or partially shut their physical sites and get their employees to work at home. This change to more home-based working disrupted many of the systems and procedures that had been in place for decades. It also meant that we needed to make changes to the times of activities we were able to suggest. Our amended plans allowed us to test out some home-based activities, such as personal action plans and step count challenges. However, the contact centres were often struggling to manage their core business and the SUH programme was not at that time a priority.
There is anecdotal evidence that, as the patterns of home/office working settle and as many countries come out of the more acute stages of lockdown and the pandemic, workplaces are saying that the health and well-being of their staff has never been so important. There will be a focus on the health and well-being of the workforce, although there is little formal evidence about how to support staff working in this context, particularly on the current scale. Indeed, the impact of COVID-19 and the lockdown could have major implications for the health of the workforce, and all policies and practices will need to be re-adjusted to hybrid working. In addition, how we work with employers to develop and deliver interventions for people working mainly from home that go beyond the individual is a challenge (i.e. how do we change the ‘working environment’ when that is someone’s home?). Although SUH needs further adaptation to incorporate the new ways of working and the new systems that will develop, it has the potential to provide a significant resource for contact centres and other workplaces that may have similar organisational approaches. It has the ability to become embedded in the culture and contexts of the contact centres (and indeed this was demonstrated in the study) in a way that many other interventions are not designed to be.
One important finding from the study was that sedentary behaviour interventions, such as SUH, have the potential to impact on other health behaviours, with multiple possible direct and indirect health benefits. Sedentary behaviour is far from being a siloed behaviour in the workplace and many of the activities that were delivered triggered positive changes to other behaviours, such as physical activity, healthy eating and smoking. It is unlikely to be a sustained intervention if it does not have more than one meaning and purpose. For example, our pilot centre (Ipsos MORI) contacted us to ask about mental health interventions and whether or not they could be linked to the SUH programme. We worked with them to introduce sedentary behaviour activities that could, at the same time, reduce feelings of stress. These included mindfulness activities (which could be placed on a table and undertaken standing up), such as jigsaws, Lego, drawing and knitting, and they also created a quiet room for people to have some space and peace. In other centres, people wanted to get physically active and were drawn to, for example, the treadmills and stationary bicycles.
Sedentary behaviour is something that is closely tied to the work day in high-income countries and, therefore, can be impacted significantly through interventions aimed at employees with sedentary jobs. Workplace sitting is, by definition, directly caused by the working environment whereas other behaviours, such as smoking and alcohol use, are not. Using an intervention, such as SUH, to show an organisational commitment to health and well-being (something that is directly within the control of the organisation) can then lead to further activities that link sedentary behaviour with another health behaviour or are specific to another health behaviour.
Recommendations for future research
Based on the findings of this study, the following research recommendations are made:
-
Although not an initial aim of this study, our study provides preliminary findings from implementing and evaluating a health behaviour intervention in a hybrid fashion as a result of the COVID-19 lockdown. It is clear that a full return to a physical workplace for all employees will not occur in the immediate future. The recommendation is that further research is required to develop a greater understanding of working from home, and hybrid working, to further develop hybrid (office and/or home working) activities and implementation approaches for an amended version of the SUH intervention (and other workplace sedentary behaviour interventions).
-
The quantitative results from this study for the primary outcome (as assessed by the activPAL device) do not support an immediate progression to a larger-scale trial, despite all other progression criteria being met (partly or fully) and positive process evaluation findings. However, there were limitations associated with COVID-19 which meant that full implementation was not possible, and we have highlighted concerns over the appropriateness of the study design for this intervention in this context. The recommendation is to conduct further feasibility and pilot work to more confidently assess the possible intervention effect and the preliminary estimates of the variability of the outcomes. This work would come after the intervention development and refinement research proposed in the above recommendation.
-
The process evaluation findings from this study identified several barriers to and facilitators of the implementation of, and participation in, the SUH intervention that related to organisational and cultural aspects of the contact centres. The recommendation is that further research is required to develop a greater understanding of the organisational and system-based factors, and how these differ between centres, which could impede or assist the implementation and sustainability of workplace interventions aimed at reducing sedentary time.
-
The findings of this study highlighted important concerns about the use of the primary outcome measure, the activPAL. This was carefully selected during the development of the study because of the high accuracy of the device in assessing posture. It is also the preferred tool in intervention studies in which sitting time is the primary outcome. However, in this study we experienced compliance levels that were lower than what has been reported in the literature previously. The recommendation is that, prior to any future progression to a definitive trial, further research should be undertaken to assess the appropriateness of the activPAL device as the primary outcome measure in a definitive trial, given the associated cost and burden of using such a device.
Acknowledgements
With many thanks to Ipsos MORI Scotland, especially Wayne Gilbert and Eilidh Gordon who made the pilot research project possible, sat on our Study Steering Committee, and have been supporters of SUH from the outset.
Original Masters students
Audrey Buelo, Christina Katan, Laura Tirman, Florence Ashdown, Ruth Miller and Isis Guerrero Castillo.
Contact centres
With many thanks to the businesses and organisations that took part in the research:
-
British Telecom (BT) Contact Centre, South Shields (Kareema Hay and Christine Carruthers, Health Advocates)
-
Legal Aid Agency, North East Region (Tracey Armstrong, Customer Services Team Manager)
-
South Tyneside Homes, Customer Service Team (Elaine Wallace, Assistant Head of Housing; Christopher Perry, Customer Services Manager)
-
London Metropolitan Police (Thomas Bolton, Sergeant, Metropolitan Police)
-
NHS 24 Scotland, East Contact Centre (Clare Baillie, Well-being Team Manager; Elaine Frazer, HR Advisor)
-
Teleperformance, Gateshead (Lorna Kay, Assistant Contact Centre Manager)
-
Inspired Outsourcing Ltd (Sinead Linsley, Brand and Communication Manager).
Equipment
Many thanks to Sit–Stand.com, which provided desk risers and anti-fatigue mats to participating centres free of cost. Special thanks to Rik Mistry and Nicola Davenport from Sit–Stand.com for their help and enthusiasm.
Research assistance
Additional research assistance was provided by the following researchers and research students: Bradley MacDonald, Kieran Turner, Lara Tarvit, Matthew Northcote, Zhen (Leo) Yang, Yueshun (Shaun) Shi, Daichun (Ellen) Zhan, Fariha Mosaddeque, Justyna Kedziera, Hannah Houghton, Ioannis Psomadakis-Karastamatis and Li Jiahang.
Study Steering Committee members
Dr Alison Kirk, University of Strathclyde; Dr Claire Fitzsimons, University of Edinburgh; Ms Laura Mandefield, University of York; Mr Wayne Gilbert, Associate Director, Ipsos MORI (Leith, Edinburgh); Ms Eilidh Gordon, Administrator, Operations, Ipsos MORI (Leith, Edinburgh); Mr Graeme Russell, CWU Regional BT safety chairperson; and Ms Sharon Currie, NHS Health Scotland.
Project/research expertise
The team brings together expertise in intervention development and evaluation, physical activity and sedentary measurement, statistics, workplace health promotion and health economics.
Ruth Jepson is Director of the Scottish Collaboration for Public Health Research and Policy. She was PI on the grant. She is PI on a NIHR PHR-funded project (PHR 15/82/12). Ruth Jepson was part of the team that developed the 6SQuID framework and has expertise in intervention development and evaluation. Ruth Jepson was the PI and was responsible for project management, and ensuring that all milestones were completed in a timely and robust manner. She was the line manager for the research assistants.
Graham Baker is a Lecturer in Physical Activity for Health and has expertise in the measurement of sedentary and physical activity behaviours. Graham also has expertise in qualitative methods and currently leads a qualitative work package as part of a NIHR PHR-funded project (PHR 15/82/12) evaluating the programme theory and effects of a complex public health intervention on health inequalities.
Divya Sivaramakrishnan is a Chancellor’s Fellow at the Scottish Collaboration for Public Health Research and Policy. She is a mixed-methods researcher, with expertise in intervention development and evaluation. Her PhD focused on developing a yoga programme for older adults in Scotland. She is also experienced in facilitating workshops and conducting knowledge exchange events.
Jillian Manner is a Research Assistant and PhD Candidate at the Scottish Collaboration for Public Health Research and Policy. She has expertise in qualitative methods and is currently completing her PhD looking at the impact of organisational and cultural factors on workplace health programmes, such as the SUH programme.
Richard Parker is a Senior Statistician based in the Edinburgh Clinical Trials Unit. He has statistical expertise and expertise in designing and running cluster-randomised controlled studies and stepped-wedge evaluations.
Scott Lloyd is Advanced Public Health Practitioner for Obesity, Physical Activity and Settings at Public Health South Tees, a shared service for both Middlesbrough Council and Redcar & Cleveland Borough Council. He has held lead roles in workplace health programmes since 2005, including supporting at least eight call centres to improve the health of staff with demonstrable results. His role in the study was to assist with the recruitment of call centres via the North East Better Health at Work Award (engages over 400 employers in the North East of England, including a number of large call centres) and to provide expert advice and guidance, including making links with trade unions.
Andrew Stoddart is a Senior Health Economist with over 10 years’ experience of clinical trials. He has an active interest in costing methodology and the application of routine data linkage in health technology assessment, particularly in the estimation of service costs and/or remote patient follow-up.
Contributions of authors
Ruth Jepson (https://orcid.org/0000-0002-9446-445X) (Professor of Public Health in Social Science) was the principal investigator leading on the design and execution of the study, oversaw the research governance and led the preparation of the final report.
Graham Baker (https://orcid.org/0000-0002-9547-6778) (Lecturer in Physical Activity for Health) was a co-investigator on the study, leading the design and execution of the qualitative components of work, as described in Chapters 3 and 5 of the final report.
Divya Sivaramakrishnan (https://orcid.org/0000-0002-3013-4793) (Chancellor’s Fellow) was a research fellow/assistant on the study. She was responsible for programme delivery and data collection (with JM). She also contributed to the design and analysis of the process evaluation components.
Jillian Manner (https://orcid.org/0000-0003-4411-5056) (Research Assistant, PhD Candidate) was a research assistant on the study, carrying out programme delivery and data collection and analysis of the process evaluation.
Richard Parker (https://orcid.org/0000-0002-2658-5022) (Senior Statistician) was a co-investigator on the study, leading the design and execution of the quantitative components of work, as described in Chapter 4 of the final report.
Scott Lloyd (https://orcid.org/0000-0001-9617-4838) (Advanced Public Health Practitioner) was a co-investigator on the study, supporting the recruitment of contact centres, and design and execution of the study.
Andrew Stoddart (https://orcid.org/0000-0002-1958-3897) (Senior Health Economist) was a co-investigator on the study, leading the design and execution of the health economic components of work, as described in Chapter 5 of the final report.
Publication
Parker RA, Manner J, Sivaramakrishnan D, Baker G, Stoddart A, Lloyd S, Jepson R. Design, rationale and analysis plan for the Stand Up for Health trial in contact centres: a stepped wedge feasibility study. Pilot Feasibility Stud 2020;6:139.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the PHR programme or the Department of Health and Social Care.
References
- Chau JY, Grunseit AC, Chey T, Stamatakis E, Brown WJ, Matthews CE, et al. Daily sitting time and all-cause mortality: a meta-analysis. PLOS ONE 2013;8. https://doi.org/10.1371/journal.pone.0080000.
- Proper KI, Singh AS, van Mechelen W, Chinapaw MJ. Sedentary behaviors and health outcomes among adults: a systematic review of prospective studies. Am J Prev Med 2011;40:174-82. https://doi.org/10.1016/j.amepre.2010.10.015.
- Cho CY, Hwang YS, Cherng RJ. Musculoskeletal symptoms and associated risk factors among office workers with high workload computer use. J Manipulative Physiol Ther 2012;35:534-40. https://doi.org/10.1016/j.jmpt.2012.07.004.
- Thorp AA, Owen N, Neuhaus M, Dunstan DW. Sedentary behaviors and subsequent health outcomes in adults a systematic review of longitudinal studies, 1996–2011. Am J Prev Med 2011;41:207-15. https://doi.org/10.1016/j.amepre.2011.05.004.
- de Rezende LF, Rodrigues Lopes M, Rey-López JP, Matsudo VK, Luiz Odo C. Sedentary behavior and health outcomes: an overview of systematic reviews. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0105620.
- Zhai L, Zhang Y, Zhang D. Sedentary behaviour and the risk of depression: a meta-analysis. Br J Sports Med 2015;49:705-9. https://doi.org/10.1136/bjsports-2014-093613.
- Owen N, Healy GN, Matthews CE, Dunstan DW. Too much sitting: the population health science of sedentary behavior. Exerc Sport Sci Rev 2010;38:105-13. https://doi.org/10.1097/JES.0b013e3181e373a2.
- Bankoski A, Harris TB, McClain JJ, Brychta RJ, Caserotti P, Chen KY, et al. Sedentary activity associated with metabolic syndrome independent of physical activity. Diabetes Care 2011;34:497-503. https://doi.org/10.2337/dc10-0987.
- Tremblay MS, Aubert S, Barnes JD, Saunders TJ, Carson V, Latimer-Cheung AE, et al. Sedentary Behavior Research Network (SBRN) – terminology consensus project process and outcome. Int J Behav Nutr Phys Act 2017;14. https://doi.org/10.1186/s12966-017-0525-8.
- Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Lancet Physical Activity Series Working Group . Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet 2012;380:219-29. https://doi.org/10.1016/S0140-6736(12)61031-9.
- Wilmot EG, Edwardson CL, Achana FA, Davies MJ, Gorely T, Gray LJ, et al. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysis. Diabetologia 2012;55:2895-905. https://doi.org/10.1007/s00125-012-2677-z.
- Santos R, Mota J, Okely AD, Pratt M, Moreira C, Coelho-e-Silva MJ, et al. The independent associations of sedentary behaviour and physical activity on cardiorespiratory fitness. Br J Sports Med 2014;48:1508-12. https://doi.org/10.1136/bjsports-2012-091610.
- Ekelund U, Brown WJ, Steene-Johannessen J, Fagerland MW, Owen N, Powell KE, et al. Do the associations of sedentary behaviour with cardiovascular disease mortality and cancer mortality differ by physical activity level? A systematic review and harmonised meta-analysis of data from 850 060 participants. Br J Sports Med 2019;53:886-94. https://doi.org/10.1136/bjsports-2017-098963.
- Ekelund U, Steene-Johannessen J, Brown WJ, Fagerland MW, Owen N, Powell KE, et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016;388:1302-10. https://doi.org/10.1016/S0140-6736(16)30370-1.
- Biddle SJH, Bennie JA, De Cocker K, Dunstan D, Gardiner PA, Healy GN, et al. Controversies in the science of sedentary behaviour and health: insights, perspectives and future directions from the 2018 Queensland Sedentary Behaviour Think Tank. Int J Environ Res Public Health 2019;16. https://doi.org/10.3390/ijerph16234762.
- Gardner B, Smith L, Lorencatto F, Hamer M, Biddle SJ. How to reduce sitting time? A review of behaviour change strategies used in sedentary behaviour reduction interventions among adults. Health Psychol Rev 2016;10:89-112. https://doi.org/10.1080/17437199.2015.1082146.
- Straker L, Coenen P, Dunstan D, Gibson N. Sedentary Work – Evidence on an Emergent Work Health and Safety Issue. Canberra, ACT: Safe Work Australia; 2016.
- Hoy D, March L, Brooks P, Blyth F, Woolf A, Bain C, et al. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis 2014;73:968-74. https://doi.org/10.1136/annrheumdis-2013-204428.
- Vos T, Barber RM, Bell B, Bertozzi-Villa A, Biryukov S, Bolliger I, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386:743-800. https://doi.org/10.1016/S0140-6736(15)60692-4.
- Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet 2017;389:736-47. https://doi.org/10.1016/S0140-6736(16)30970-9.
- Healy G, Lawler S, Thorp A, Neuhaus M, Robson E, Owen N, et al. Reducing Prolonged Sitting in the Workplace (An Evidence Review: Full Report) 2012.
- Daneshmandi H, Choobineh AR, Ghaem H, Alhamd M, Fakherpour A. The effect of musculoskeletal problems on fatigue and productivity of office personnel: a cross-sectional study. J Prev Med Hyg 2017;58:E252-E258.
- De Cocker K, Duncan MJ, Short C, van Uffelen JG, Vandelanotte C. Understanding occupational sitting: prevalence, correlates and moderating effects in Australian employees. Prev Med 2014;67:288-94. https://doi.org/10.1016/j.ypmed.2014.07.031.
- Smith L, McCourt O, Sawyer A, Ucci M, Marmot A, Wardle J, et al. A review of occupational physical activity and sedentary behaviour correlates. Occup Med 2016;66:185-92. https://doi.org/10.1093/occmed/kqv164.
- Cole JA, Tully MA, Cupples ME. ‘They should stay at their desk until the work’s done’: a qualitative study examining perceptions of sedentary behaviour in a desk-based occupational setting. BMC Res Notes 2015;8. https://doi.org/10.1186/s13104-015-1670-2.
- Waters CN, Ling EP, Chu AH, Ng SH, Chia A, Lim YW, et al. Assessing and understanding sedentary behaviour in office-based working adults: a mixed-method approach. BMC Public Health 2016;16. https://doi.org/10.1186/s12889-016-3023-z.
- MyCustomer . Infographic: What Does the Contact Centre Industry Look Like in 2016 2016. www.mycustomer.com/service/contact-centres/infographic-what-does-the-contact-centre-industry-look-like-in-2016 (accessed 6 August 2018).
- PayScale . Call Center Agent Salary 2018. www.payscale.com/research/UK/Job=Call_Center_Agent/Salary (accessed 26 January 2022).
- ContactBabel . The 2022 UK Contact Centre Decision-Makers’ Guide (19th Edition) 2022. www.contactbabel.com/downloads/the-2022-uk-contact-centre-decision-makers-guide/ (accessed 12 September 2022).
- Thorp AA, Healy GN, Winkler E, Clark BK, Gardiner PA, Owen N, et al. Prolonged sedentary time and physical activity in workplace and non-work contexts: a cross-sectional study of office, customer service and call centre employees. Int J Behav Nutr Phys Act 2012;9. https://doi.org/10.1186/1479-5868-9-128.
- Toomingas A, Forsman M, Mathiassen SE, Heiden M, Nilsson T. Variation between seated and standing/walking postures among male and female call centre operators. BMC Public Health 2012;12. https://doi.org/10.1186/1471-2458-12-154.
- Morris A, Murphy R, Shepherd S, Graves L. Multi-stakeholder perspectives of factors that influence contact centre call agents’ workplace physical activity and sedentary behaviour. Int J Environ Res Public Health 2018;15. https://doi.org/10.3390/ijerph15071484.
- Odebiyi DO, Akanle OT, Akinbo SR, Balogun SA. Prevalence and impact of work-related musculoskeletal disorders on job performance of call center operators in Nigeria. Int J Occup Environ Med 2016;7:98-106. https://doi.org/10.15171/ijoem.2016.622.
- Charbotel B, Croidieu S, Vohito M, Guerin AC, Renaud L, Jaussaud J, et al. Working conditions in call-centers, the impact on employee health: a transversal study. Part II. Int Arch Occup Environ Health 2009;82:747-56. https://doi.org/10.1007/s00420-008-0351-z.
- Taylor P, Baldry C, Bain P, Ellis V. ‘A Unique Working Environment’: health, sickness and absence management in UK call centres. Work, Employment and Society 2003;17:435-58. https://doi.org/10.1177/09500170030173002.
- Coenen P, Gilson N, Healy GN, Dunstan DW, Straker LM. A qualitative review of existing national and international occupational safety and health policies relating to occupational sedentary behaviour. Appl Ergon 2017;60:320-33. https://doi.org/10.1016/j.apergo.2016.12.010.
- Anderton E, Bevan S. Constrained Work? Job Enrichment & Employee Engagement in Low Wage, Low Skill Jobs. London: The Work Foundation; 2014.
- Renton SJ, Lightfoot NE, Maar MA. Physical activity promotion in call centres: employers’ perspectives. Health Educ Res 2011;26:1050-9. https://doi.org/10.1093/her/cyr055.
- Shrestha N, Kukkonen-Harjula KT, Verbeek JH, Ijaz S, Hermans V, Pedisic Z. Workplace interventions for reducing sitting at work. Cochrane Database Syst Rev 2018;6. https://doi.org/10.1002/14651858.CD010912.pub4.
- Hutcheson AK, Piazza AJ, Knowlden AP. Work site-based environmental interventions to reduce sedentary behavior: a systematic review. Am J Health Promot 2018;32:32-47. https://doi.org/10.1177/0890117116674681.
- Chu AH, Ng SH, Tan CS, Win AM, Koh D, Müller-Riemenschneider F. A systematic review and meta-analysis of workplace intervention strategies to reduce sedentary time in white-collar workers. Obes Rev 2016;17:467-81. https://doi.org/10.1111/obr.12388.
- Straker L, Abbott RA, Heiden M, Mathiassen SE, Toomingas A. Sit–stand desks in call centres: associations of use and ergonomics awareness with sedentary behavior. Appl Ergon 2013;44:517-22. https://doi.org/10.1016/j.apergo.2012.11.001.
- Thorp AA, Kingwell BA, Owen N, Dunstan DW. Breaking up workplace sitting time with intermittent standing bouts improves fatigue and musculoskeletal discomfort in overweight/obese office workers. Occup Environ Med 2014;71:765-71. https://doi.org/10.1136/oemed-2014-102348.
- Pronk NP, Katz AS, Lowry M, Payfer JR. Reducing occupational sitting time and improving worker health: the Take-a-Stand Project, 2011. Prev Chronic Dis 2012;9. https://doi.org/10.5888/pcd9.110323.
- Edmunds S, Hurst L, Harvey K. Physical activity barriers in the workplace. Int J Workplace Health Manag 2013;6:227-40. https://doi.org/10.1108/ijwhm-11-2010-0040.
- Munir F, Biddle SJH, Davies MJ, Dunstan D, Esliger D, Gray LJ, et al. Stand More AT Work (SMArT Work): using the behaviour change wheel to develop an intervention to reduce sitting time in the workplace. BMC Public Health 2018;18. https://doi.org/10.1186/s12889-018-5187-1.
- Rutter H, Savona N, Glonti K, Bibby J, Cummins S, Finegood DT, et al. The need for a complex systems model of evidence for public health. Lancet 2017;390:2602-4. https://doi.org/10.1016/S0140-6736(17)31267-9.
- Hadgraft NT, Brakenridge CL, LaMontagne AD, Fjeldsoe BS, Lynch BM, Dunstan DW, et al. Feasibility and acceptability of reducing workplace sitting time: a qualitative study with Australian office workers. BMC Public Health 2016;16. https://doi.org/10.1186/s12889-016-3611-y.
- Hadgraft NT, Willenberg L, LaMontagne AD, Malkoski K, Dunstan DW, Healy GN, et al. Reducing occupational sitting: workers’ perspectives on participation in a multi-component intervention. Int J Behav Nutr Phys Act 2017;14. https://doi.org/10.1186/s12966-017-0530-y.
- Parry S, Straker L, Gilson ND, Smith AJ. Participatory workplace interventions can reduce sedentary time for office workers – a randomised controlled trial. PLOS ONE 2013;8. https://doi.org/10.1371/journal.pone.0078957.
- Morris AS, Murphy RC, Shepherd SO, Healy GN, Edwardson CL, Graves LEF. A multi-component intervention to sit less and move more in a contact centre setting: a feasibility study. BMC Public Health 2019;19. https://doi.org/10.1186/s12889-019-6615-6.
- The Better Health at Work Award . Good Work Is Good for You: Employer Information Guide n.d. www.betterhealthatworkaward.org.uk/documents/Employer%20Guide%202020.pdf (accessed 12 September 2022).
- Healthy Working Lives Award Programme . Healthy Working Lives Gold Award Portfolio n.d. www.healthyworkinglives.scot/resources/publications/Documents/award-gold.pdf (accessed 12 September 2022).
- Health and Safety Executive . Work With Display Screen Equipment: Health and Safety (Display Screen Equipment) Regulations 1992 As Amended by the Health and Safety (Miscellaneous Amendment) Regulations 2002 (L26) [Online] 2003. www.hse.gov.uk/pUbns/priced/l26.pdf (accessed 23 December 2019).
- Buckley JP, Hedge A, Yates T, Copeland RJ, Loosemore M, Hamer M, et al. The sedentary office: an expert statement on the growing case for change towards better health and productivity. Br J Sports Med 2015;49:1357-62. https://doi.org/10.1136/bjsports-2015-094618.
- Sprigg CA, Smith PR, Jackson PR. Psychological Risk Factors in Call Centres: An Evaluation of Work Design and Well-being. Sheffield: University of Sheffield, Health and Safety Executive; 2003; n.d.
- Rogers PJ. Using programme theory to evaluate complicated and complex aspects of interventions. Evaluation 2008;14:29-48. https://doi.org/10.1177/1356389007084674.
- Wight D, Wimbush E, Jepson R, Doi L. Six steps in quality intervention development (6SQuID). J Epidemiol Community Health 2016;70:520-5. https://doi.org/10.1136/jech-2015-205952.
- van Rooyen H, Essack Z, Rochat T, Wight D, Knight L, Bland R, et al. Taking HIV testing to families: designing a family-based intervention to facilitate HIV testing, disclosure, and intergenerational communication. Front Public Health 2016;4. https://doi.org/10.3389/fpubh.2016.00154.
- Hartley JE, McAteer J, Doi L, Jepson R. CARE: the development of an intervention for kinship carers with teenage children. Qual Soc Work 2019;18:926-43. https://doi.org/10.1177/1473325018783823.
- Sinclair JMA, Dutey-Magni PF, Anderson AS, Baird J, Barker ME, Cutress RI, et al. A context-specific digital alcohol brief intervention in symptomatic breast clinics (abreast of health): development and usability study. JMIR Res Protoc 2020;9. https://doi.org/10.2196/14580.
- Tirman L, Biggs H, Morrison K, Manner J, Sivaramakrishnan D, Baker G, et al. Stand Up for Health: programme theory for an intervention to reduce sedentary behaviour in contact centres. Eval Program Plann 2021;89. https://doi.org/10.1016/j.evalprogplan.2021.102002.
- Bandura A. Health promotion by social cognitive means. Health Educ Behav 2004;31:143-64. https://doi.org/10.1177/1090198104263660.
- Centres for Disease Control and Prevention . The Social-Ecological Model: A Framework for Prevention 2020. www.cdc.gov/violenceprevention/publichealthissue/social-ecologicalmodel.html (accessed 26 January 2022).
- Chastin SF, De Craemer M, Lien N, Bernaards C, Buck C, Oppert JM, et al. The SOS-framework (Systems of Sedentary behaviours): an international transdisciplinary consensus framework for the study of determinants, research priorities and policy on sedentary behaviour across the life course: a DEDIPAC-study. Int J Behav Nutr Phys Act 2016;13. https://doi.org/10.1186/s12966-016-0409-3.
- Edwardson CL, Yates T, Biddle SJH, Davies MJ, Dunstan DW, Esliger DW, et al. Effectiveness of the Stand More AT (SMArT) work intervention: cluster randomised controlled trial. BMJ 2018;363. https://doi.org/10.1136/bmj.k3870.
- Parker RA, Manner J, Sivaramakrishnan D, Baker G, Stoddart A, Lloyd S, et al. Design, rationale and analysis plan for the Stand Up for Health trial in contact centres: a stepped wedge feasibility study. Pilot Feasibility Stud 2020;6. https://doi.org/10.1186/s40814-020-00683-1.
- Hemming K, Haines TP, Chilton PJ, Girling AJ, Lilford RJ. The stepped wedge cluster randomised trial: rationale, design, analysis, and reporting. BMJ 2015;350. https://doi.org/10.1136/bmj.h391.
- Hemming K, Lilford R, Girling AJ. Stepped-wedge cluster randomised controlled trials: a generic framework including parallel and multiple-level designs. Stat Med 2015;34:181-96. https://doi.org/10.1002/sim.6325.
- Kotz D, Spigt M, Arts IC, Crutzen R, Viechtbauer W. Use of the stepped wedge design cannot be recommended: a critical appraisal and comparison with the classic cluster randomized controlled trial design. J Clin Epidemiol 2012;65:1249-52. https://doi.org/10.1016/j.jclinepi.2012.06.004.
- Maxwell AE, Parker RA, Drever J, Rudd A, Dennis MS, Weir CJ, et al. Promoting Recruitment using Information Management Efficiently (PRIME): a stepped-wedge, cluster randomised trial of a complex recruitment intervention embedded within the REstart or Stop Antithrombotics Randomised Trial. Trials 2017;18. https://doi.org/10.1186/s13063-017-2355-z.
- Uneke CJ, Uro-Chukwu HC. Improving quality of antenatal care through provision of medical supply kits. Lancet Glob Health 2018;6:e4-e5. https://doi.org/10.1016/S2214-109X(17)30471-0.
- Dunstan DW, Wiesner G, Eakin EG, Neuhaus M, Owen N, LaMontagne AD, et al. Reducing office workers’ sitting time: rationale and study design for the Stand Up Victoria cluster randomized trial. BMC Public Health 2013;13. https://doi.org/10.1186/1471-2458-13-1057.
- Grant A, Treweek S, Dreischulte T, Foy R, Guthrie B. Process evaluations for cluster-randomised trials of complex interventions: a proposed framework for design and reporting. Trials 2013;14. https://doi.org/10.1186/1745-6215-14-15.
- Nutbeam D, Bauman AE. Evaluation in a Nutshell : A Practical Guide to the Evaluation of Health Promotion Programs. North Ryde, NSW: McGraw Hill Education, Medical; 2014.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350. https://doi.org/10.1136/bmj.h1258.
- Glasgow RE, Harden SM, Gaglio B, Rabin B, Smith ML, Porter GC, et al. RE-AIM planning and evaluation framework: adapting to new science and practice with a 20-Year review. Front Public Health 2019;7. https://doi.org/10.3389/fpubh.2019.00064.
- Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health 1999;89:1322-7. https://doi.org/10.2105/AJPH.89.9.1322.
- Forman J, Heisler M, Damschroder LJ, Kaselitz E, Kerr EA. Development and application of the RE-AIM QuEST mixed methods framework for program evaluation. Prev Med Rep 2017;6:322-8. https://doi.org/10.1016/j.pmedr.2017.04.002.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Chau JY, Van Der Ploeg HP, Dunn S, Kurko J, Bauman AE. Validity of the occupational sitting and physical activity questionnaire. Med Sci Sports Exerc 2012;44:118-25. https://doi.org/10.1249/MSS.0b013e3182251060.
- Seppälä P, Mauno S, Feldt T, Hakanen J, Kinnunen U, Tolvanen A, et al. The construct validity of the Utrecht Work Engagement Scale: multisample and longitudinal evidence. J Happiness Stud 2008;10. https://doi.org/10.1007/s10902-008-9100-y.
- Hill JC, Kang S, Benedetto E, Myers H, Blackburn S, Smith S, et al. Development and initial cohort validation of the Arthritis Research UK Musculoskeletal Health Questionnaire (MSK-HQ) for use across musculoskeletal care pathways. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-012331.
- Public Health Scotland . Screening For Physical Activity Levels Using Scot-PASQ n.d. www.healthscotland.scot/health-topics/physical-activity/screening-for-physical-activity-levels-using-scot-pasq (accessed 12 September 2022).
- van Nassau F, Chau JY, Lakerveld J, Bauman AE, van der Ploeg HP. Validity and responsiveness of four measures of occupational sitting and standing. Int J Behav Nutr Phys Act 2015;12. https://doi.org/10.1186/s12966-015-0306-1.
- Chau JY, Sukala W, Fedel K, Do A, Engelen L, Kingham M, et al. More standing and just as productive: effects of a sit–stand desk intervention on call center workers’ sitting, standing, and productivity at work in the Opt to Stand pilot study. Prev Med Rep 2016;3:68-74. https://doi.org/10.1016/j.pmedr.2015.12.003.
- Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003;35:1381-95. https://doi.org/10.1249/01.MSS.0000078924.61453.FB.
- Stewart-Brown SL, Platt S, Tennant A, Maheswaran H, Parkinson J, Weich S, et al. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): a valid and reliable tool for measuring mental well-being in diverse populations and projects. J Epidemiol Community Health 2011;65:A38-A9. https://doi.org/10.1136/jech.2011.143586.86.
- Lyden K. ActivPAL Processing. Process ActivPAL Events Files 2016. https://rdrr.io/cran/activpalProcessing/ (accessed 12 September 2022).
- Schulz KF, Altman DG, Moher D. CONSORT Group . CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Trials 2010;11. https://doi.org/10.1186/1745-6215-11-32.
- Sivaramakrishnan D, Jepson R. Stand Up for Health Questionnaire Data. Edinburgh: Scottish Collaboration for Public Health Research and Policy, University of Edinburgh; 2021.
- Hodgson T, Meiners M. Cost-of-illness methodology: a guide to current practices and procedures. Milbank Mem Fund Q Health Soc 1982;60:429-62. https://doi.org/10.2307/3349801.
- Hayes RJ, Bennett S. Simple sample size calculation for cluster-randomized trials. Int J Epidemiol 1999;28:319-26. https://doi.org/10.1093/ije/28.2.319.
- Koopmanschap MA, Rutten FF. A practical guide for calculating indirect costs of disease. PharmacoEconomics 1996;10:460-6. https://doi.org/10.2165/00019053-199610050-00003.
- Koopmanschap MA, Rutten FF, van Ineveld BM, van Roijen L. The friction cost method for measuring indirect costs of disease. J Health Econ 1995;14:171-89. https://doi.org/10.1016/0167-6296(94)00044-5.
- Wilson PWF, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation 1998;12:1837-47. https://doi.org/10.1161/01.CIR.97.18.1837.
- Frew E. Applied Methods of Cost-Benefit Analysis in Health Care. Oxford: Oxford University Press; 2010.
- National Institute for Health and Care Excellence (NICE) . Hypertension in Adults: Diagnosis and Management 2019. https://www.nice.org.uk/guidance/ng136/evidence/costeffectiveness-analysis-treatment-initiation-threshold-for-people-with-stage-1-hypertension-pdf-6957345277.
- Bending M, Beale S, Hutton J. An Economic Analysis of Workplace Interventions That Promote Physical Activity, PHIAC Report 2008.
- Gao L, Nguyen P, Dunstan D, Moodie M. Are office-based workplace interventions designed to reduce sitting time cost-effective primary prevention measures for cardiovascular disease? A systematic review and modelled economic evaluation. Int J Environ Res Public Health 2019;16. https://doi.org/10.3390/ijerph16050834.
- University of Oxford Diabetes Trials Unit and Health Economics Research Centre . UKPDS Outcomes Model User Manual 2015.
- Lutz N, Clarys P, Koenig I, Deliens T, Taeymans J, Verhaeghe N. Health economic evaluations of interventions to increase physical activity and decrease sedentary behavior at the workplace: a systematic review. Scand J Work Environ Health 2020;46:127-42. https://doi.org/10.5271/sjweh.3871.
- Ardahan M, Simsek H. Analyzing musculoskeletal system discomforts and risk factors in computer-using office workers. Pak J Med Sci 2016;32:1425-9. https://doi.org/10.12669/pjms.326.11436.
- Parry SP, Coenen P, Shrestha N, O’Sullivan PB, Maher CG, Straker LM. Workplace interventions for increasing standing or walking for decreasing musculoskeletal symptoms in sedentary workers. Cochrane Database Syst Rev 2019;2019. https://doi.org/10.1002/14651858.CD012487.pub2.
- Bevan S. Economic impact of musculoskeletal disorders (MSDs) on work in Europe. Best Pract Res Clin Rheumatol 2015;29:356-73. https://doi.org/10.1016/j.berh.2015.08.002.
- Squires H, Rick J, Carroll C, Hillage J. Cost-effectiveness of interventions to return employees to work following long-term sickness absence due to musculoskeletal disorders. J Public Health 2012;34:115-24. https://doi.org/10.1093/pubmed/fdr057.
- Zemedikun DT, Kigozi J, Wynne-Jones G, Guariglia A, Roberts T. Methodological considerations in the assessment of direct and indirect costs of back pain: a systematic scoping review. PLOS ONE 2021;16. https://doi.org/10.1371/journal.pone.0251406.
- Maniadakis N, Gray A. The economic burden of back pain in the UK. Pain 2000;84:95-103. https://doi.org/10.1016/S0304-3959(99)00187-6.
- Hong J, Reed C, Novick D, Happich M. Costs associated with treatment of chronic low back pain: an analysis of the UK General Practice Research Database. Spine 2013;38:75-82. https://doi.org/10.1097/BRS.0b013e318276450f.
- Whitehurst DG, Bryan S, Lewis M, Hill J, Hay EM. Exploring the cost-utility of stratified primary care management for low back pain compared with current best practice within risk-defined subgroups. Ann Rheum Dis 2012;71:1796-802. https://doi.org/10.1136/annrheumdis-2011-200731.
- Roland M, Morris R. A study of the natural history of back pain: part 1: development of a reliable and sensitive measure of disability in low-back pain. Spine 1983;8:141-4. https://doi.org/10.1097/00007632-198303000-00004.
- Cobiac LJ, Vos T, Barendregt JJ. Cost-effectiveness of interventions to promote physical activity: a modelling study. PLOS Med 2009;6. https://doi.org/10.1371/journal.pmed.1000110.
Appendix 1 Reasons for centre dropouts
Summary of responses to exit questionnaires from centres 5 and 8
Centre 5 exit questionnaire summary
There were two main reasons for dropping out:
-
Pandemic.
The pandemic was the main factor for dropping out. The centre was very comfortable with accommodating the key elements of the programme before the pandemic but felt that the safety and security of colleagues and customers’ needs were the priority during the pandemic. It felt that it would not get enough participants for the programme during the pandemic owing to its priorities and workload. The centre had moved to a hybrid model of home and office working, and felt that it would not be able to participate fully in the programme given that on-site activities were no longer possible.
-
In-house initiatives for staff well-being.
The centre had already organised several initiatives to support the mental and physical well-being of staff (e.g. online bingo, step challenge, mental health first aid training, support for homeworkers, reduced meeting times, health and well-being course for managers, other tools and communication).
Centre 8 exit questionnaire summary
There were three main reasons for dropping out:
-
Found project requirements difficult and expensive and had concerns about reduction in sales revenue.
The centre felt that, as an outsourced sales centre, it was not able to invest in projects that may reduce sales revenue. The centre found it difficult to commit to (1) allocating 27 employees for research evaluation (despite SUH offering to do this in batches), as it meant over 3 hours away from the telephone, (2) interviews with participants and (3) retention of participants, as it felt that this would be challenging.
-
Changes to circumstances since registering interest.
The centre had registered interest in April 2019 but was allocated (randomly) to start only in March 2020. Although the centre had a consistent workforce and positive levels of recruitment when it registered, it faced recruitment challenges in March 2020 and needed to carefully consider the time allocated to external projects.
-
Inadequate communication between registering interest and actually starting.
The centre felt that the SUH team did not provide sufficient communication between April 2019 (first registered) and February 2020. If the centre had known earlier, it could have planned for the project to start in March 2020. The lack of communication and allocation to a later start date also made the centre feel that it was not prioritised and not essential.
Glossary
- 6 Steps In Quality Intervention Development (6SQuID)
- A framework used to develop interventions in a transparent and systematic way.
- Absenteeism
- Periods of unplanned employee absence from work, such as sick leave.
- Activity-based costing
- A method of systematically identifying all aspects of direct cost of a programme or organisation, in this report the delivery of the Stand up for Health programme, based on the activities that it entails.
- Activity/action
- Part of an intervention aimed at reducing a risk factor (or risk factors). An intervention may consist of a single activity (e.g. mass media campaign) or multiple activities (e.g. 20 mph signs, plus educational campaign, plus legal enforcement). Cf. Theory of action.
- Contact centre
- A contact centre is a central point from which all customer interactions are managed. Their primary purpose is to provide customers with efficient and effective technical support, customer service and sales assistance. A contact centre typically includes one or more call centres, but may also include other types of customer contact, including e-mails, web chats and social media interactions.
- Co-production
- An approach in which researchers, practitioners and the public work together, sharing power and responsibility from the start to the end of the project, including the generation of knowledge.
- Cost–utility analysis
- A form of health economic evaluation based on quality-adjusted life-years with stated UK policy preference.
- Fishbone diagram
- This is also called a cause-and-effect diagram or Ishikawa diagram. This is a diagram that is used to visualise the possible causes of a problem and facilitates the sorting of causes into categories.
- Health utility
- A generic measure of preference or value that an individual or society gives a particular state of health, used to calculate quality-adjusted life-years.
- Logic model
- Diagrams showing hypothesised cause-and-effect relationships between short-, medium- and long-term outcomes.
- Presenteeism
- Reduced productivity at work owing to ill health.
- Programme theory
- Theory describing how an intervention is expected to trigger a chain of outcomes through specified activities. Consists of a Theory of change and Theory of action.
- Quality-adjusted life-year
- A generic measure of disease burden, including both the quality and the quantity of life lived. This is of specific interest in health economic evaluation in the UK owing to policy preference.
- Stepped-wedge cluster-randomised design
- Pragmatic design whereby clusters (contact centres) are randomised to time points that will receive the intervention.
- Theory of action
- Theory describing how an intervention is constructed to activate underpinning theories of change (cf. Activity/action).
- Theory of change
- Theory describing the mechanisms by which change is expected to occur.
List of abbreviations
- 6SQuID
- 6 Steps in Quality Intervention Development
- ABC
- activity-based costing
- BMI
- body mass index
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- EQ-5D
- EuroQol-5 Dimensions
- FTE
- full-time equivalent
- MSK-HQ
- Musculoskeletal Health Questionnaire
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health and Care Research
- OR
- odds ratio
- OSPAQ
- Occupational Sitting and Physical Activity Questionnaire
- PASQ
- Physical Activity Screening Question
- PHR
- Public Health Research
- PSS
- Personal Social Services
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- RE-AIM
- reach, efficacy, adoption, implementation, maintenance
- SD
- standard deviation
- SMArT Work
- Stand More AT Work
- SUH
- Stand Up for Health
- UWES
- Utrecht Work Engagement Scale
- WEMWBS
- Warwick–Edinburgh Mental Well-being Scale
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/IEXP0277).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
