Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 14/197/65. The contractual start date was in July 2016. The final report began editorial review in July 2019 and was accepted for publication in February 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Rachel Meacock is a member of the National Institute for Health Research (NIHR) Health Services and Delivery Research (HSDR) Funding Committee (2019 to present). Prior to that, Rachel Meacock was an associate member of the NIHR HSDR Board (March 2016–December 2018). Richard Emsley is a member of the NIHR Health Technology Assessment Clinical Evaluation and Trial Committee (November 2017 to present).
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Forsyth et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Literature search
At present, approximately 850,000 people have a diagnosis of dementia in England and Wales, with the rate of diagnosis projected to double by 2040. 1 Dementia is currently an NHS priority. 2 In England and Wales, a social framework to support people with dementia in the community has been adopted,3,4 with a focus on quality of life. 5 National Institute for Health and Care Excellance guidelines6 outline a clear community pathway and provide a detailed referral process, including assessment tools, provision for patients across different community settings and suggestions for best practice7 for care co-ordination once a diagnosis is made.
Recent research has concentrated on dementia and the impact that it can have on individuals in hard-to-reach communities, such as those in prison, and has focused predominently on the suitability, or otherwise, of prison environments for individuals with dementia. 8
There are currently 82,525 people in prison in England and Wales. Sixteen per cent of the total prison population are older prisoners, defined as aged ≥ 50 years. 9 In England and Wales, prisoners aged ≥ 60 years are the fastest-growing group, followed by those aged 50–60 years. 9 Between 2011 and 2019 the number of male prisoners aged ≥ 60 years increased from 3038 to 4930 and the number of male prisoners aged ≥ 50 years increased from 8899 to 13,061. At the same time, the number of female prisoners aged ≥ 60 years increased from 79 to 128, and the number of women prisoners aged ≥ 50 years increased from 397 to 559. 9 A similar pattern has been shown in other countries, including the USA,10 Australia,11 Japan12 and Canada. 13 This trend is likely to continue. 14 This growth is in part due to an overall ageing population, but also to increases in sentence length and the increase for prisoners aged ≥ 50 years in historical sexual convictions. 15
It is widely accepted that those in prison are physiologically approximately 10 years older than their chronological age. 16 This is, in part, a result of drug and alcohol misuse and lower educational attainment, but also exacerbated by the prison environment. 17 It is recognised that adjustments are required to accommodate and address the mental and physical frailty associated with ageing,8,18,19 including those conditions more prevalent in older age (e.g. dementia). 18 Older prisoners often have suboptimal access to appropriate health-care services20 and may go unnoticed in large prisons. Unlike their younger counterparts, they tend to be quieter and less complaining, and their health and social care needs may not be as immediately obvious as those with severe, acute problems, such as active psychosis or substance withdrawal. This was notably emphasised in the thematic review published by the Chief Inspector of Her Majesty’s Inspectorate of Prisons in 2004, the title of which, ‘No Problems – Old and Quiet’: Older Prisoners in England and Wales,21 reflected an entry found in an elderly prisoner’s discipline record. However, this stereotype of a quiet, helpful, older prisoner is being challenged by a growing body of research that shows that older prisoners can have serious health, social and custodial needs that often go unidentified and unmet in the prison setting. A number of studies have shown that older men in prison have different needs from both the general (younger) prisoner population and older adults in the community. 21–27
According to the principle of the equivalence of care,28 prisoners are entitled to the same level of health care as that provided to the general population. 29 All NHS standards therefore apply to prison health care, including the National Service Framework for Older People. 30 However, the standards outlined in this framework remain largely unmet in prisons in England and Wales,21 and there remains no overarching national strategy for older prisoners, despite repeated recommendations that one be developed. 21 Although equivalence is a recognised priority, it is well established that community guidelines do not adequately address the logistical challenges of prison environments and, in practice, equivalence can be difficult to achieve. 31 Prison health-care services are under continuing strain to provide comparable health and social care provision, and the continued under-resourcing of health care contributes to inefficient service delivery. 17
Dementia in prison is understudied and research is yet to establish what systematic care should be provided for prisoners with dementia or mild cognitive impairment (MCI). Research so far has been centred on men8,32 and of limited geographical representation. 19,33 Before the study commenced, dementia rates among older male prisoners were estimated at 1–2%. 19,23,24 This figure was based on small samples that did not include women and may therefore not be representative of the whole older prison population. Prevalence estimates also varied as a result of discrepancies in assessment measures used. A previous study from our research group25 investigated a sample of older male prisoners drawn from a 1-day census in 12 prisons across the north-west of England. The study25 reported that 7% of participants achieved a score on the Mini Mental State Examination (MMSE)34 that indicated possible dementia.
Studies have shown that prisoners with dementia or MCI can suffer from multiple adverse consequences in relation to victimisation and punishment for non-adherence to prison rules. 35,36 Furthermore, the prison environment in its current form is not suitable to effectively provide dementia or MCI care. Excessive noise and poor lighting can be distressing and disorientating to those with dementia or MCI,37 and often prisons are dark and use inadequate artificial lighting. Likewise, the prison regime is restrictive and, if disorientated, an individual may find it increasingly difficult to follow a routine. 38 It is therefore imperative to establish an accurate prevalence rate to inform our understanding of the ability of current services to identify and manage prisoners with dementia or MCI, and to establish what systematic care should be delivered and what adjustments should be made to the prison environment.
Although government strategies regarding ageing prisoners and dementia have been published, no a specific dementia or MCI care pathway has been developed that is applicable and appropriate for use across different prison sites in England and Wales. Recommendations have been made to translate community-based guidelines into guidance suitable for prisons;39 however, a strategic pathway is yet to be developed. For example, although some UK prisons have developed wings for older prisoners, these services are delivered on an ad hoc basis, with support often disbanded as a result of financial limitations. 8 It has been postulated that the delivery of age-appropriate services could be cost-effective and that research must endeavour to develop pragmatic solutions to support staff and prisoners. 40
To achieve this, there are contextual constraints that should be acknowledged when considering the implementation of the community model into the prison environment. These constraints include a lack of understanding between prison service staff and prison health-care staff regarding how each other’s organisations work, with lack of role clarity resulting in problematic intervention implementation. 40 Care pathway development should therefore aim to support all members of staff and include clear role guidance.
The increasing age of the prison population is a relatively new concern in prison; therefore, current understanding and awareness of dementia and MCI among prison staff is low. 41 There is potential to misdiagnose early symptoms of dementia, for example regressive behaviour can present as anger or bad behaviour. 42 Therefore, there is a need to develop training for all prison staff. 39
The Dementia Training Standards Framework,43 updated by Skills for Health, Health Education England (HEE) and Skills for Care in 2018, provides a guide on what essential skills and knowledge are needed across the health and social care sector. The framework describes three tiers of training: awareness, which everyone should have (tier 1); basic skills that are relevant to all staff in settings where people with dementia are likely to appear (tier 2); and training for leadership (tier 3). With the principles of equivalence in mind, this framework should also guide the format of training interventions in the prison setting.
A systematic review of dementia education and training for the health and social care workforce found that educational programmes should to be relevant to participants’ roles and experience; involve active face-to-face participation; underpin practice-based learning with theory; be delivered by an experienced facilitator; have a total duration of at least 8 hours, with individual sessions of ≥ 90 minutes; support application of learning in practice; and provide a structured tool or guideline to guide care practice. 44
A scoping review of the literature on dementia training in the prison setting identified a general lack of research on training needs, preferences and content. Cipirani et al. 45 described dementia remaining ‘a hidden problem’ for many reasons, including prisoners not being proactively screened for MCI when they enter facilities, prison staff lacking the skills to identify possible dementia, prisoners tending not to report any cognitive or physical symptoms for fear of repercussions and mental health services focusing on other inmates whose behaviour is more challenging. 45 Recommendations for training content included covering the early warning signs of dementia (e.g. indecisiveness, confusion about time or place, mood changes, wandering and developing problems with handwriting) and increasing awareness of the impact of dementia on a prisoner’s ability to function, thereby reducing the potential for conflict arising from misunderstandings. 8,46 Moll8 further recommended the need to explore and clarify the role of peer carers in prison and provide them with appropriate training.
Study aims
This study aimed to
-
establish the prevalence of dementia and MCI in prisons in England and Wales (part 1; see Chapter 2)
-
establish the degree and type of impairment, risk level, needs and social networks of those who screen positive on the Addenbrooke’s Cognitive Examination – Third Revision (ACE-III) (part 1; see Chapter 2)
-
validate the six-item cognitive impairment test (6-CIT) for routine use in prisons to aid the early and consistent identification of older prisoners with possible MCI or dementia (part 1; see Chapter 2)
-
identify gaps in current service provision (part 2; see Chapter 3)
-
understand the first-hand experiences of prisoners living with dementia and MCI in prison (part 3; see Chapter 4)
-
develop a prison-based care pathway for prisoners with dementia and MCI (part 4; see Chapter 5)
-
develop training packages for staff and prisoners in dementia and MCI awareness, assessment and management (part 5; see Chapter 6)
-
undertake health economic costings for the care pathway and training packages developed in parts 4 and 5 (part 6; see Chapter 7).
Chapter 2 Part 1
Method
Part 1 of the study aimed to:
-
estimate the current and likely future prevalence of dementia among the prison population in England and Wales
-
establish the degree and type of impairment, the risk of reoffending, the needs and the social networks of those who screen positive on the ACE-III
-
validate the 6-CIT for routine use in prisons to aid the early and consistent identification of older prisoners with possible MCI or dementia.
Sample
We aimed to recruit 860 prisoners (591 men and 269 women). This sample size was calculated to allow the estimation of a prevalence of 7% (based on Hayes et al. 25) with 2% precision [95% confidence interval (CI) 5% to 9%, applying finite sample corrections for each sex].
Inclusion and exclusion criteria
Inclusion criteria
-
Aged ≥ 50 years.
-
Resident in one of the participating prison establishments on the day of the census.
Exclusion criteria
-
Considered by prison or health-care staff not safe to interview alone due to their current risk.
-
Previous inclusion in the study.
-
Does not have a functional command of the English language.
-
Lacking the capacity to provide informed consent and an appropriate personal or independent consultee could not be identified or contacted, was unwilling to be consulted or made the decision to refuse consent.
Participants were included only if they could speak and understand English to a sufficient level and researchers were satisfied that their English-language ability would not adversely have an impact on their test scores. There are significant language biases in some tests, which cannot be overcome by straightforward translation or use of an interpreter. Some tests are available in other language versions, but not all translations have been validated and test administration would still have required the presence of an interpreter. In previous prison-based studies, researchers have experienced considerable difficulties in accessing translation services by telephone. The equipment required to utilise these resources is scarce within prisons, and negotiating researcher access to it on an ad hoc basis was not realistic and would have threatened the feasibility of completing the research to time and budget.
Consent
The researcher explained the project to the eligible participants and gave them the information sheet as well as explaining their ethics rights (see Report Supplementary Material 1). The researcher read and explained the information in these documents to the eligible participant, showing sensitivity to the high levels of learning difficulties and literacy problems in this population, as well as to their potential MCI. The researcher explained what participation involved, how much time it would take and answered any questions. The researcher also explained that participation was voluntary, that the prisoner was free to withdraw at any point and that their decision to participate, or not, would have no adverse effect on the care that they received or their legal rights. The researcher also discussed the arrangements to ensure confidentiality (and limits of this) and data protection. Limits to confidentiality included information pertaining to:
-
behaviour that was against prison rules
-
information that suggested either a risk of harm to self or a risk of harm to others
-
information that referred to a new crime committed or planned, or undisclosed illegal acts
-
behaviour that would be harmful to the individual (e.g. intention to self-harm or to end one’s life)
-
information that raised concerns about terrorism, radicalisation or security issues.
Researchers had a duty to inform prison staff of any of the above, in line with our written protocol.
Potential participants were given the option of participating immediately after they were approached. The reason for interviewing people so soon after the initial approach was because of the complex and challenging nature of the prison environment, the difficulties in working around the prisons’ security needs (which take priority at all times) and the very short notice periods involved when moving people around the prison estate. It would have been unlikely that we could have achieved the recruitment targets for the study in the prison environment without such an approach. However, a process consent procedure was followed to ensure that participants had multiple opportunities to consider their involvement in the study and withdraw if they chose, without any negative implications for them. Further details of this process consent method are explained in Individuals lacking capacity. Eligible participants who wanted to have longer to consider their involvement were interviewed within 1 week of their initial approach and were given at least 24 hours to consider whether or not they wanted to participate. The consent form (see Report Supplementary Material 2) was explained to the participant before they signed it, and the researcher signed the form after it had been completed by the participant. A copy of the consent form was offered to the participant and one copy was retained by the researcher. Once informed consent had been obtained, the participant was invited to begin the interview.
Each person who agreed to participate in the interview was allocated a unique participant identification (ID) number and names were not recorded. Dependent on the outcome of the initial screening on the Montreal Cognitive Assessment (MoCA), participants were invited for a further interview. Those who did not want to continue with the study were thanked for their time and their participation in the study ended. For those who consented to a further interview, it was explained that they may be contacted in the next 3 months, but that they were under no obligation to complete the next interview should they change their mind.
The researchers taking consent were aware of the potential for any coercion and how the vulnerabilities of individuals might affect the decision they make. Researchers also received specific training in recognising MCI and working sensitively with individuals affected in this way. The prisoner population has high levels of illiteracy and learning difficulties, and researchers had an awareness of these difficulties when obtaining consent. Researchers ensured that participants could demonstrate a clear understanding of their involvement in the study and their rights within the study (e.g. the right to withdraw) prior to seeking informed consent. Researchers were sufficiently trained and experienced to assess whether or not patients had the capacity to give consent.
Individuals lacking capacity
Researchers received training in assessing capacity, as outlined in the Mental Capacity Act (MCA),47 as follows:
-
Gaining ‘permission to access’ the person with possible dementia from staff, a relative or a named person.
-
Establishing the basis for consent. As capacity is situational and variable, the researcher endeavoured to find out how the person usually consented to care or other activities in day-to-day life.
-
Seeking initial consent for the specific research. Information was provided that was appropriate for that person to help them understand the study. This step included recording non-verbal communication and facial expressions, and referring back to what was already known about how the person usually consented on a daily basis. It was important that the researcher did not rely only on a lack of verbal objection and assumed this to mean consent had been given.
-
Monitoring ongoing consent monitoring in line with the idea of consent as a process. Dewing48 described this stage as ‘ensuring initial consent is revisited and re-established on every occasion or even within the same occasion’. 48
-
Providing feedback and support. This included feeding back to staff any concerns the researcher might have had about the participant.
Researchers also sought an opinion from prison health-care staff regarding capacity. If the person lacked capacity, an attempt was made to identify a ‘personal consultee’, as defined by the MCA,47 to advise on the individual’s participation. In the first instance, even when participants were considered to lack the capacity to consent to participation, researchers asked if they could contact someone else to advise on the individual’s behalf. Potential consultees from outside the prison were contacted only if the research team had established that they were aware that the potential participant was in prison and that they had difficulties that limited their capacity to consent. The initial approach to anyone outside the prison was made by prison health-care staff.
Personal consultees were provided with study information (see Report Supplementary Material 3) and their role and the reason for them being approached was explained by researchers. If the participant was unable to nominate anyone or give consent to contact someone outside the prison, researchers identified an appropriate independent consultee (again, in line with the MCA47). This was usually a clinician or health-care worker from within the prison. No pressure was placed on any individual to act as a consultee and researchers fully briefed consultees regarding the study, to enable them to offer advice on the potential participant’s behalf. If a consultee or nominee advised that the individual would not want to take part, they were not be recruited.
Researchers also discussed the study with the person themselves, in a way that was appropriate to their level of understanding. If there was any indication that the individual did not want to participate in any part of the study then the individual did not take part, even if their participation has been advised by another person on their behalf. When this occurred, researchers informed the individual’s consultee that the individual was not taking part, despite their advice, and explained the reasons for this. There was clear potential for the research to benefit individuals with MCI and the study methods (interviews and observations) posed minimal risk to participants. All data collection was completed with sensitivity and respect for the autonomy and privacy of each participant.
The following safeguards were applied once an individual had been recruited in this way:
-
No actions were taken during any part of the study if the participant seemed to object to it (unless the action was vital to protect the individual from harm).
-
Researchers considered the interests of the participant above all else throughout the study.
-
The participant was withdrawn if any conditions pertaining to his or her inclusion in the project no longer applied and/or if he or she gave any indication that they did not want to continue or take part.
The consent form (see Report Supplementary Material 2 and 4) for all individuals included an option to indicate a preference ‘for’ or ‘against’ continued participation, should the individual lose the capacity to consent during the study.
Sampling procedure
The sample was drawn randomly from all women’s prisons and a representative range of adult men’s prisons across England and Wales, including local prisons holding those on remand, those serving short sentences and those in the early part of long sentences; training and dispersal prisons holding men part-way through long sentences; high-secure establishments holding those considered to be high risk; and open prisons holding short-term prisoners deemed low risk and those in the final stages of long sentences who are preparing for community release.
We selected sites based on the proportion of each prison type in the prison estate as a whole: one of the eight high-secure sites; 3 of the 31 local sites; 5 of the 51 category B or C training and dispersal prisons, and one of the seven category D or open prisons [as defined in the Justice prison index URL: www.justice.gov.uk/contacts/prison-finder (accessed 9 May 2016)]. We also included a prison that had a specific wing for older and disabled prisoners. This is one of only two prisons in the country with a dedicated wing for prisoners based on their age and health needs.
We estimated that we would need to initially approach approximately 415 female prisoners and 896 male prisoners to allow for 20% of prisoners refusing to participate and a further 14% of prisoners who might have been unavailable on the day, unable to consent or already interviewed for the study in a previous establishment. (These estimates were based on the Hayes et al. study,25 in which researchers conducted a 1-day census of all prisons in the north-west of England and interviewed all men aged ≥ 60 years resident in each establishment.)
The total number of prisoners aged ≥ 50 years in the recruiting prisons was established and these figures were used to calculate a sampling fraction, which informed the proportion of prisoners we approached at each site. We stratified our sample according to age, an important variable when investigating MCI, as prevalence doubles with every increase of 5 years. 49
To stratify by age, we collected an age breakdown of the prisoners present in the establishment on census day for each of the sites. The latest Dementia UK: Update1 stipulated that those aged 60–69 years had two to three times the prevalence of those aged 50–59 years. Additionally, those aged ≥ 70 years had three to five times the prevalence of the youngest group. We therefore obtained the number of prisoners aged 50–59, 60–69, 70–79 and ≥ 80 years at each site on a given census day. Within each site, we sampled 30% of those aged 50–59 years, 60% of those aged 60–69 years, 90% of those aged 70–79 years and all prisoners aged ≥ 80 years. The procedure is described as follows.
Procedure
Our exact procedure varied between sites, as certain elements depended on local factors or procedures, such as the size of the health-care suite or the holding room, the freedom of movement allowed to prisoners within the establishment and whether or not researchers were authorised as key holders. The research team therefore liaised with the prison governor and relevant staff to establish a procedure in each site, which broadly followed that detailed in the following steps.
Recruitment
We utilised a 1-day census approach, specifying a census date per site. (It would not have been feasible to have only 1 census day for all sites, as it took considerable time to collect data at each site, and a long delay between the census date and data collection would inevitably have resulted in increased attrition, especially at local prisons with transient, remand populations.)
A research nurse or another appropriate staff member in each prison acted as a single point of contact (SPOC) for the research team. This was a different role across study sites (such as a clinical studies officer, researcher or research facilitator), but to avoid the potential for coercion during recruitment we ensured that the individual was not in a directly caring role for prisoners and not a member of our research team. The research team provided the SPOC at each site with a census date and the SPOC then identified potential participants who fulfilled the inclusion criteria. The SPOC did this by running a search on all prisoners in their establishment on the prison computer system (Computer-National Offender Management Information System) or health-care system [SystmOne; The Phoenix Partnership (Leeds) Ltd, Leeds, UK]. Once a numbered list of all potential participants had been generated, the SPOC informed researchers of the number of eligible older prisoners identified. A member of the university-based research team then used a random number generator to identify the numbers of those randomly selected for potential participation. We communicated these to the SPOC (e.g. numbers 1, 3, 6, 7, 9 . . ., etc., on this list). The SPOC then conducted checks using the internal prison data systems to ensure that the individual met the inclusion criteria and that it was appropriate for them to be seen. They considered if the potential prisoner’s current risk assessment indicated whether or not they were safe to be seen. This was done by reviewing the records and discussing with health-care staff, as appropriate. They had a protocol that they used to determine appropriateness in a uniform way.
The SPOC then sent an information and appointment slip to each of the individuals who had been randomly selected and were both eligible and appropriate to be seen. The slip briefly outlined the study and invited each individual to a one-to-one interview with a researcher. The slip explicitly stated that, by attending their designated appointment, individuals would be meeting with a member of the research team to further discuss the potential for participation. Details of who to approach for further information or advice regarding the study, within the prison and prior to the appointment time, was also included. This procedure was considered more realistic and feasible than someone in the prison going to see each potential participant and asking for their consent to pass details on to the research team. There were in excess of 100 eligible participants at some establishments and, given the impact of austerity measures across the prison estate, requiring a member of staff to do this amount of work was considered unfeasible.
Interviews were held in health-care clinic rooms, in visits or in wing interview rooms, depending on the availability of rooms, procedures and governor preferences in each prison. At their appointment time, eligible participants met a researcher who provided them with, initially, verbal information and then, if they were willing, written information about the study and an opportunity for further discussion. During the briefing process, participants were made aware that if they chose to take part in the study, their data would be made available to other researchers, but that this would be in an anonymised format.
Following the procedure for obtaining consent, if an individual consented to take part, the researcher conducted an initial interview (see Report Supplementary Material 5), which included the collection of demographic data and completion of the MoCA. A proportion of the sample also completed the 6-CIT for validation purposes.
Researchers obtained the prison ID number of all who attended an appointment, regardless of whether or not they had consented to participate in the study. This list was then passed to the SPOC, who matched it against the list of those invited to appointments to identify anyone who failed to attend. If any individuals identified in the initial random sample failed to attend, the SPOC attempted to make contact with them to establish whether or not the reason for their failure to attend was related to an inability to comprehend the written information provided. This was an important step in ensuring that the sample was not biased by the indirect exclusion of those with a MCI or literacy problems. The SPOC took great care to avoid coercing individuals into taking part or making individuals feel that they had to account for their decision not to attend. Instead, they made it clear that the purpose of making contact was to check if any individuals wanted to attend but were unable to, in which case-appropriate arrangements and additional support was put in place to facilitate a meeting with the research team. At some sites, multiple census day random samples were generated until the target number was achieved.
Individuals who scored positive on the MoCA proceeded to a further needs assessment interview (see Report Supplementary Material 6). The interview took place immediately after the part 1 interview or, in some cases was delayed by a short time, depending on the operational arrangements at the study site and the individual’s preference or needs. A further, fairly lengthy interview may have been difficult and distressing for individuals with MCI, so researchers considered the needs and wishes of each participant prior to continuing with the second interview. If it was operationally viable and the individual was able and willing to continue with a full needs assessment, then both interviews were conducted at the same appointment. If this was not the case, the researcher arranged a new appointment via the research nurse and returned to complete the full needs assessment at a later stage.
Interviews and consent procedures followed the same format for the second interview as described above for the MoCA. Researchers first obtained additional, more detailed demographic information. Information on current physical and mental health, as well as any diagnosis of learning difficulties or disabilities, sensory difficulties and/or use of substances or medication, was gathered on a pro forma designed for the study. This information enabled us to gauge the presence of other factors known to have an impact on cognitive test scores (e.g. pain, strong medication, poor hearing or eyesight, learning issues, mood disorders). Information on this was supplemented by the use of information gathered from SystmOne. Researchers interviewed participants using a range of standardised assessments to assess the degree and type of their impairment, their activities of daily living (ADL) needs, their mental health needs, any brain injury, and their social networks.
Subject to each individual’s informed consent, risk and follow-up data were also collected at this stage. Information pertaining to risks of self-harm and reoffending was sought from the Offender Management Unit. The NHS number, name and date of birth of each participant was also obtained and recorded to allow for the long-term follow-up of key health and criminal justice outcomes at a later date (in a further potential study). Consent was sought from the participant (or advice was sought from the consultee; see Individuals lacking capacity) for researchers to access the individual’s electronic prison health-care record. Health-care records were screened for any indication of diagnosed MCI or dementia.
Follow-up
To enable us to examine the longer-term health and criminal justice outcomes of those who screened positively at a later date, and with further funding, we sought permission from participants to collect their NHS numbers as well as their full names and dates of birth.
If consent was granted, researchers obtained this information from a health-care administrator who already had access to this information, and data were shared via secure e-mail (gov.gsi.uk and nhs.net). Participants were allocated a unique study ID, so, once NHS numbers were received by the research team, these were held with other identifiable information (name, prison ID number) in a separate and secure location from the identifier key and other study data, including test responses.
Participants were able to opt out of allowing access to their data for follow-up and/or allowing access to their risk data as generated by the Offender Management Unit to maintain individual choice and avoid any potential adverse effect on recruitment. Participants were therefore given the option to continue to participate in the study as a whole, even if they opted out of allowing researchers to access their risk information or follow-up data.
No risk or follow-up information was sought in relation to participants deemed to lack the capacity to provide informed consent, as it would not have been appropriate for a personal or an independent consultee to grant researchers access to risk or follow-up data on another’s behalf.
Measures
All participants were invited to complete the MoCA. 50
Montreal Cognitive Assessment
The MoCA50 was designed as a rapid screening instrument for cognitive dysfunction. Different cognitive domains (including attention, memory, visuospatial skills and orientation) are assessed using a series of short tests. The time taken to administer the MoCA is approximately 10 minutes. The total possible score is 30 points, with a score of ≥ 26 points considered normal in the general population. Permission to use the MoCA for research purposes was granted for this study.
The literature clearly supports the MoCA as superior to the MMSE as a global assessment tool. 51 It reportedly has a higher classification accuracy than other measures for differentiating healthy control individuals from those with MCI, and it can identify impairment indicative of specific clinical conditions, including Parkinson’s disease, Huntington’s disease and, Korsakoff syndrome. Although specialised assessment within a memory service is the ‘gold-standard’ assessment, the MoCA is considered to be the best of the short assessment measures.
However, several studies question whether or not the universal cut-off score of 26 points (developed originally on 90 Canadian healthy control individuals) is appropriate across populations.
Freitas et al. 52 compared the MoCA and MMSE for differentiating MCI from Alzheimer’s disease and healthy ageing in a large, Portuguese, clinical cohort, in which 90 patients with Alzheimer’s disease and 90 patients with MCI were compared with two groups of 90 age-matched controls. Freitas et al. 52 reported optimal cut-off scores of < 22 points for MCI and < 17 points for Alzheimer’s disease. Waldon-Perrine and Axelrod53 assessed 185 veterans referred by a physician for neuropsychological testing in Michigan, USA, and reported an optimal cut-off score of ≤ 20 points for detecting impairment. Larner54 recruited new referrals from a cognitive function clinic in Liverpool, UK. Using a cut-off score of 26 points, sensitivity was 0.97 but specificity was 0.60. A cut-off score of > 20 points for healthy control individuals increased overall test accuracy and improved specificity to 0.95, but reduced sensitivity to 0.63. Luis et al. 55 suggested a cut-off score of 23 points in a south-western US sample. Roalf et al. 51 assessed 321 people diagnosed with Alzheimer’s disease, 126 people with MCI (from Penn Memory Center, Philadelphia, PA, USA) and 140 healthy control individuals. They developed an optimal cut-off score of 23 points to differentiate between healthy control and Alzheimer’s disease, a cut-off score of 25 points to differentiate between healthy control and MCI and a cut-off score of 19 points to differentiate between Alzheimer’s disease and MCI. Lee et al. 56 validated the MoCA-K, a Korean version of the MoCA, with 196 elderly persons from a Seoul hospital (mild AD, n = 44; MCI, n = 37; HC, n = 115). Using a cut-off score of 22 out of 23 points, the MoCA-K had an excellent sensitivity of 89% and a good specificity of 84% for screening MCI.
We therefore used a cut-off score of 23 points in this study. The high rate of false positives when using a cut-off score of 26 points could have threatened the feasibility of the study, as we planned to conduct a 1.5-hour battery of assessments with individuals who screened positively on the MoCA.
Six-item cognitive impairment test
We had originally planned to complete the 6-CIT with all 869 participants. However, it became apparent that this may be unnecessary and a waste of resources and participants’ time if it transpired that the 6-CIT was not a valid screening tool. We therefore conducted a sample size calculation to ascertain the number of participants that were required to validate the 6-CIT. This sample size calculation was based on 90% sensitivity and 100% specificity, assuming an estimated prevalence of 7% (error 0.15). We established that 470 individuals from our sample of 869 were required to complete the 6-CIT57 for validation purposes. We continued to conduct both the 6-CIT and the MoCA until the required number of 6-CIT responses was obtained. We stratified the sample at each prison by age and collected data from one prison before moving on to the next. We could therefore be confident that the 6-CIT sample was representative of the overall sample.
The 6-CIT57 is a short screening measure for dementia. It is administered in around 3–4 minutes and asks questions about the current time, month and year, as well as testing the participant’s ability to recall a five-component address and list the numbers 1–20 and the months of the year in reverse. Permission to use the measure was obtained from the authors.
The 6-CIT is a much shorter assessment than the MoCA and could therefore be more easily added into current health assessments used in prison. The 6-CIT was used so that we could compare its clinical effectiveness with that of the MoCA in identifying people with potential dementia and MCI.
Participants who scored < 23 points on the MoCA were invited to complete a further battery of assessments detailed as follows.
Demographic pro forma
A demographic pro forma was designed for the study, covering participants’ health (including self-reported ADL problems, eyesight and hearing problems, learning difficulties, head injuries and whether or not they were under the influence of any substances), criminal justice information and command of the English language.
History of comorbidities and medications pro forma
A pro forma was designed to ascertain past and current comorbidities and medications. The research team took this information from prison health-care notes.
Addenbrookes Cognitive Examination – Third Revision
The ACE-III58 is one of the most commonly used cognitive tests to assess dementia and other neurological disorders. It routinely takes around 15 minutes to administer and covers five domains: (1) attention, (2) memory, (3) fluency, (4) language and (5) visuospatial ability. The gold standard for diagnosing dementia and MCI is specialised assessment within a memory service. The ACE-III is, however, a validated screening tool for dementia syndromes. 58
The ACE-III consists of tasks associated with memory, language, verbal fluency and visuospatial functioning, and it has a possible total score of 100. This is a robust clinical tool, which is most commonly used to aid a clinical diagnosis of dementia. Cut-off scores of 82 and 88 are considered to indicate dementia and MCI, respectively. 58,59 These studies have also reported sensitivity of 93–100% and specificity rates of 96–100% at cut-off scores of 82 for dementia and 88 for MCI.
The following structured assessments scales were used to describe the ADL skills and comorbidities of those with suspected MCI or dementia.
Bristol Activities of Daily Living Survey (adapted version)
The Bristol Activities of Daily Living Survey (BADLS) (adapted version)60 was designed specifically for patients with dementia. The questions assess level of independence with regard to ADL abilities, such as preparing food, dressing, washing and using the telephone. The BADLS has 20 items, but these were reduced to 18 items for the purposes of this study, as questions relating to activities that are not relevant in prison (use of public transport and managing finances) were removed. In addition, questions referring to shopping and housework were rephrased to relate to canteen ordering and keeping one’s cell area clean. As a result, we looked not at the overall score but at individual items of the assessment. The survey can be administered in approximately 5 minutes.
Geriatric Depression Scale-15
The Geriatric Depression Scale-1561 (GDS-15) is an adapted version of the long-form Geriatric Depression Scale and is used to identify depression in elderly people. It can be administered in approximately 5 minutes.
PriSnQuest
PriSnQuest62 is an eight-item prison screening questionnaire validated to screen for mental illness in prison. The questions are in yes/no format and cover previous contact with services, suicidal ideation and the presence of psychotic symptoms. A score of ≥ 3 indicates the need for further, detailed examination, and the measure can be completed in < 5 minutes.
Rivermead Post-Concussion Symptoms Questionnaire
The Rivermead Post-Concussion Symptoms Questionnaire63 is designed to assess the presence of mild to moderate brain injury. Participants are asked to rate the severity of 16 cognitive, somatic and emotional symptoms that are commonly found after a traumatic brain injury. Symptoms are rated from 0 (not experienced) to 4 (severe problem) and are judged on their severity over the course of the last 24 hours. The questionnaire takes around 5 minutes to administer and was only used with participants who reported having had a brain injury, as it is not relevant otherwise.
Lubben Social Network Scale-18
The Lubben Social Network Scale-1864 is an 18-item self-report scale that assess ES social isolation in older adults. It measures perceived social support from family, friends and neighbours. The Lubben Social Network Scale-18 takes around 10 minutes to complete and assesses the size, closeness and frequency of contacts in a participant’s social network. For the purposes of this study, ‘neighbours’ were interpreted as friends or acquaintances in the prison (rather than in the individual’s neighbourhood), whereas the section on friends was completed in relation to friends external to the prison.
When permission was granted, we also obtained individuals’ NHS numbers to allow us to obtain funding to follow up these participants in the future.
Risk information
We sought the following information from the Offender Management Unit in each prison (for each individual who participated in stage 2, i.e. MoCA-positive individuals):
-
Offender Assessment System (OASys) rating of risk of harm to self and others: very high, high, medium or low
-
Risk Matrix 2000 score (in relation to risk of sexual reoffending), if applicable
-
risk markers: sexual offender; risk to children, women, staff; hate crime (e.g. racism).
Risk information was used to describe the sample in stage 2.
Data analysis
The prevalence estimates were directly age standardised using the age distribution of the national prison population as the reference. From age 50 years and older the following age strata were applied: 50–59, 60–69 and ≥ 70 years. Each stratum-specific weight was calculated as the proportion of the whole prison population that was in that age group, divided by the equivalent proportion for the study sample. The numerator was then calculated the adjusted by taking the product of the weight and the study sample size within each age stratum.
We produced age-specific prevalence estimates to allow comparison with community-based samples (e.g. Matthews et al. 65).
The battery of tests established the broader needs of each older prisoner, including social support, ADL skills, comorbidity and risk. Descriptive statistics were produced. This information informed the case vignettes that were generated in part 4 of the study (see Chapter 5).
In addition, we measured the agreement between categories of the MoCA and 6-CIT using kappa. 66–68 We also examined the relationship between the items and combinations of items on the scales and, with these ordered data, we used weighted kappa as the measure of agreement. 69,70 This approach allowed us to establish whether or not the 6-CIT has suitable psychometric properties to be used as a routine screen in prisons. We estimated the prevalence of MCI by calculating percentages and 95% CIs using the 6-CIT, so that we could compare these with prevalence estimates based on the MoCA.
We aimed to generate a matrix of future prevalence estimates according to various hypothetical projected scenarios of overall prison population growth and of rising numbers of older prisoners in both absolute and proportional terms. Unfortunately, data were not available to enable prediction of future numbers of older prisoners and therefore this task could not be completed. The increase in numbers of older prisoners over recent years has mainly been due to recent sentencing for historical crimes largely as a result of better forensic science procedures (e.g. DNA testing). The population of prisoners aged ≥ 50 years is projected to increase, both in absolute terms and as a proportion of the total prison population. This is because the number of offenders aged ≥ 50 years being sentenced to custody is currently greater than the number being released. 70 However, the extent to which the increase in sentencing of people for historical crimes will continue is largely unknown and therefore it is difficult to predict if this will increase, decrease or stay the same. Furthermore, this growth is offset by a declining imprisoned for public protection/lifer population, who constitute a higher proportion of offenders aged ≥ 50 years. The 50–59 years group is predicted not to grow between now and 2023. 71
Cumulative percentages were calculated throughout this report.
Results
Prevalence
We recruited 869 prisoners (596 male and 273 female). Participant recruitment is detailed in Figure 1.
FIGURE 1.
Part 1 participant details for prevalence study.
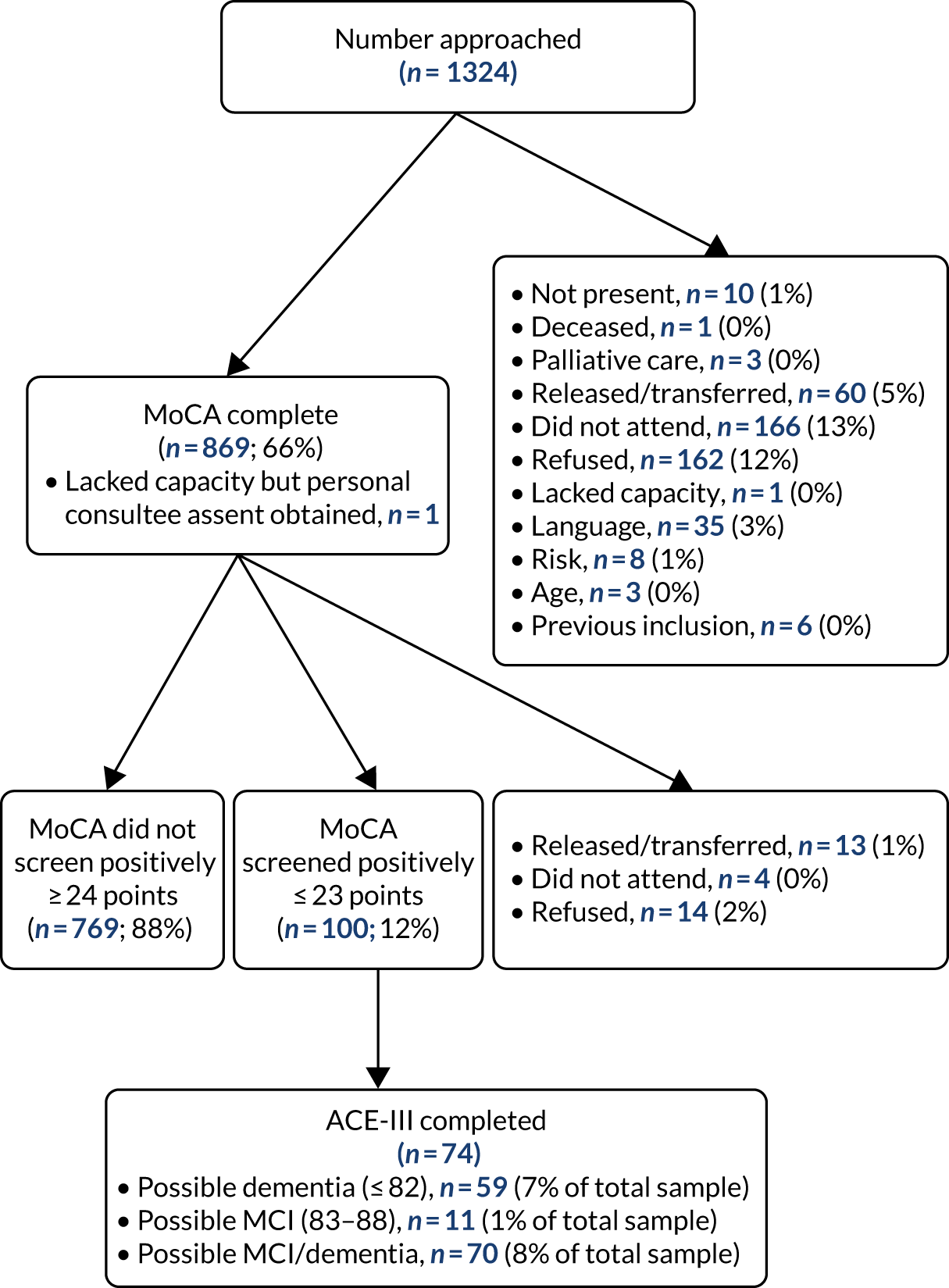
As shown in Figure 1, 100 participants screened positively on the MoCA (12%). Seventy (8%) of the total sample screened positively on the ACE-III. This included 11 individuals who screened positively for possible MCI (1% of the total sample) and 59 individuals who screened positively for dementia (7% of the total sample).
Table 1 shows the estimated prevalence of dementia and MCI among our sample of older prisoners. Across the whole sample, the prevalence was 8.1% (95% CI 6.4% to 10.1%). When this was stratified by age, the highest proportion was found among prisoners aged ≥ 70 years (16.9%, 95% CI 12.1% to 23.1%). Participants aged 50–59 years had the second highest estimated prevalence (6.4%, 95% CI 4.3% to 9.2%), followed by prisoners aged 60–69 years (4.0%, 95% CI 2.1% to 7.5%).
| Age group (years) | Number sampled | Number with suspected dementia/MCI in our sample | Prevalence, % (95% CI) |
|---|---|---|---|
| 50–59 | 425 | 27 | 6.4 (4.3 to 9.2) |
| 60–69 | 249 | 10 | 4.0 (2.1 to 7.5) |
| ≥ 70 | 195 | 33 | 16.9 (12.1 to 23.1) |
| Total | 869 | 70 | 8.1 (6.4 to 10.1) |
We estimated a prevalence of 6.8% for dementia (95% CI 5.3% to 8.7%) and 1.3% for MCI (95% CI 0.7% to 2.3%). The total weighted estimate for dementia and MCI combined is 8.1% (95% CI 6.4% to 10.1%) (Table 2).
| Type of impairment | Number impaired | Prevalence (%) | 95% CI (%) |
|---|---|---|---|
| Dementia | 59 | 6.8 | 5.3 to 8.7 |
| MCI | 11 | 1.3 | 0.7 to 2.3 |
| Total | 70 | 8.1 | 6.4 to 10.1 |
Table 3 shows estimated prevalence of dementia and MCI among the older prisoner population weighted by sex and age. There are currently 13,620 prisoners aged ≥ 50 years in England and Wales. 9 It is estimated that 8% of these prisoners have MCI or dementia. This equates to an estimated 1090 older prisoners with MCI or dementia in England and Wales. It should be noted that these findings are based on validated cognitive impairment assessments and not on a clinical diagnosis.
| Sex | Age (years) | Prisoners in England and Wales | Prisoners in sample | Dementia/MCI | Crude, % (95% CI) | Weighted, % (95% CI) |
|---|---|---|---|---|---|---|
| Male | 50–59 | 8109 | 213 | 16 | 7.5 (4.7 to 11.9) | |
| 60–69 | 3233 | 193 | 10 | 5.2 (2.8 to 9.3) | ||
| ≥ 70 | 1727 | 190 | 30 | 15.8 (11.3 to 21.6) | ||
| Female | 50–59 | 426 | 212 | 11 | 5.2 (2.9 to 9.1) | |
| 60–69 | 90 | 56 | 0 | |||
| ≥ 70 | 32 | 5 | 3 | 60.0 (23.1 to 88.2) | ||
| Total | 13,617 | 869 | 70 | 8.1 (6.4 to 10.1) | 7.9 (6.3 to 9.9) |
Only two individuals (3%) who screened positively on the ACE-III had a diagnosis of dementia recorded in their prison health-care notes, suggesting current under-recognition.
There were no individuals in our sample who were female, aged 60–69 years and screened positively for symptoms of dementia or MCI on the MoCA. A smaller number of men aged 60–69 years screened positively than (men aged 50–59 years).
Table 4 shows that the prevalence of MCI weighted by age is 0.8%.
| Age (years) | Number | MCI | Crude (%) | Weighted (%) |
|---|---|---|---|---|
| 50–59 | 425 | 1 | 0.2 (0.03 to 1.7) | |
| 60–69 | 249 | 0 | ||
| ≥ 70 | 195 | 10 | 5.1 (2.8 to 9.3) | |
| Total | 869 | 11 | 1.3 (0.7 to 2.3) | 0.8 (0.4 to 1.7) |
Table 5 shows that the prevalence of dementia weighted by age is 6.3%.
| Age (years) | Number | Dementia | Crude (%) | Weighted (%) |
|---|---|---|---|---|
| 50–59 | 425 | 26 | 6.1 (4.2 to 8.8) | |
| 60–69 | 249 | 10 | 4.0 (2.2 to 7.3) | |
| ≥ 70 | 195 | 23 | 11.8 (7.9 to 17.2) | |
| Total | 869 | 59 | 6.8 (5.3 to 8.7) | 6.3 (4.9 to 8.2) |
Comparison with the community
We aimed to compare the prevalence rates of dementia and MCI among the older prisoner population with those that exist for the wider community. Data were not available for individuals aged 50–59 years living in the community. Community prevalence estimates are broken into 5-year age brackets; however, we used 10-year age groups. It is estimated that 0.9% of individuals aged 60–64 years and 1.7% of individuals aged 65–69 years living in the community have dementia. 1 The prevalence rate among our sample of older prisoners (4%) is approximately two times higher for individuals aged 60–69 years than it is for those living in the community.
The prevalence of dementia for individuals living in the community varies greatly for individuals aged ≥ 70 years. For example, among those aged 70–74 years the estimated prevalence is 3% and among those aged ≥ 95 years the estimated prevalence is 41.1%. The median age of individuals aged ≥ 70 years in our sample of older prisoners was 73 years. Therefore, it is logical to compare the estimated prevalence of individuals aged 70–74 years (3%) in the community with our estimated prevalence of those aged ≥ 70 years (12%). Consequently, we can estimate that prisoners aged ≥ 70 years are approximately four times more likely to have a diagnosis of dementia than their age-matched counterparts living in the community. However, it should be highlighted that our evidence is based on cognitive assessments and not on a clinical diagnosis.
Characteristics of participants screening positive on the Addenbrooke’s Cognitive Examination – Third Revision
Seventy participants screened positive on the ACE-III (for MCI or dementia). Demographic and criminogenic information for these participants is detailed in Tables 6 and 7.
| Demographic | Frequency (N = 70), n (%) |
|---|---|
| Ethnicity | |
| White British | 55 (79) |
| White Irish | 4 (6) |
| Black African/Caribbean | 4 (6) |
| Asian/Pakistani | 1 (1) |
| Other | 1 (1) |
| Marital status | |
| Single | 22 (31) |
| Separated/divorced | 8 (11) |
| Married/partner | 33 (47) |
| Widowed | 7 (10) |
| Employment status (before prison) | |
| Full- or part-time employment | 25 (36) |
| Unemployed | 13 (19) |
| Retired | 19 (27) |
| Long-term sick (benefits) | 12 (17) |
| Accommodation (before prison) | |
| Private house | 60 (86) |
| Temporary accommodation | 2 (3) |
| Homeless | 2 (3) |
| Supervised hostel | 3 (4) |
| Living circumstances (before prison) | |
| Alone | 33 (47) |
| With spouse/partner with children | 13 (19) |
| With parents | 1 (1) |
| With spouse/partner without children | 16 (2) |
| Criminogenic detail | Frequency (N = 70), n (%) |
|---|---|
| Prisoner status | |
| Convicted | 69 (99) |
| Remand | 1 (1) |
| Previously convicted | |
| Yes | 27 (39) |
| No | 43 (61) |
| Wing location | |
| Remand/induction | 2 (3) |
| Health care | 2 (3) |
| Normal location | 24 (34) |
| VPU | 41 (59) |
| Drug free | 1 (1) |
| Regime | |
| Standard | 31 (44) |
| Basic | 12 (17) |
| Enhanced | 26 (37) |
The majority of prisoners were white British (n = 55, 79%). Within the general prison population, 26% of prisoners identified as non-white;72 this varied greatly from the older prisoner population more specifically. Twenty-five (36%) of the sample were employed prior to prison; however, among the wider prison population, 68% were unemployed in the 4 weeks prior to custody. 73 Prior to imprisonment, 33 (47%) of our sample were married or living with a partner, 33 (47%) were living alone and 60 (86%) were living in a private house. Homelessness is more prominent among the wider prison population (15%) than it was in our sample of older prisoners (3%).
These differences are largely as a result of the nature of the older prisoner population. A high proportion (45%) of older prisoners are sex offenders73 and many of these will have been convicted for historical offences.
The mean number of previous convictions was 2.95 and the mean current sentence length was 18 months.
Other conditions causing mild cognitive impairment
There are several possible reasons for MCI in this sample, including severe depression, stroke, chronic serious alcohol misuse, the impact of serious head injuries, other neurological conditions and learning disabilities. We established the proportion of the ACE-III-positive people who had these comorbid conditions. Seven people had some difficulties understanding spoken English to an extent that it may have interfered with their performance on the ACE-III. Hearing impairment may also have affected performance on ACE-III. One participant had hearing impairment recorded in their medical records; however, 23 individuals reported some hearing problems at interview.
Three participants had learning difficulties reported in their health-care records; however, 21 participants self-reported a learning disability, including 10 who had attended a special educational needs school. One participant had a brain injury recorded in their medical records; however, 22 participants self-reported a previous brain injury.
It is not known whether or not these comorbid conditions were associated with MCI and are therefore responsible for the ACE-III-positive score. It is possible that some people may have dementia or MCI and one or other of the conditions listed above.
Characteristics of people scoring positive on Addenbrooke’s Cognitive Examination – Third Revision
Table 8 shows that 42 participants scored above the cut-off score of 5 on the GDS-15 (60%). Scoring above the cut-off score indicates that further clinical exploration is needed. Only 13 of these individuals had a diagnosis of depression recorded in the prison health-care records.
| Test | Participants scoring above cut-off points (N = 70), n (%) |
|---|---|
| GDS-15 (score ≥ 5) | 42 (60) |
| PriSnQuest (score ≥ 3) | 7 (10) |
Seven participants (10%) who screened positively on the ACE-III scored ≥ 3 on PriSnQuest, indicating that further clinical assessment for mental illness is required.
Nineteen (27%) participants reported a history of head injury on the Rivermead Post-Concussion Symptoms Questionnaire; nine participants (13% of ACE-III-positive participants) reported experiencing poor memory after the head injury.
Physical health
The most common comorbidities noted in the case notes were hypertension (n = 18) and diabetes mellitus (n = 13) (Table 9).
| Comorbidity | Frequency of people with an underlying comorbidity (N = 59), n (%) |
|---|---|
| Heart disease | 8 (14) |
| Hypertension | 18 (31) |
| Atrial fibrillation | 4 (7) |
| Angina | 1 (2) |
| COPD | 5 (8) |
| Asthma | 8 (14) |
| COAD | 1 (2) |
| Epilepsy | 1 (2) |
| Parkinson’s disease | 1 (2) |
| Diabetes mellitus | 13 (22) |
| Cancer | 7 (12) |
| Renal problems/failure | 1 (2) |
| Arthritis/osteoarthritis | 7 (12) |
| Osteoporosis | 4 (7) |
| Anaemia | 3 (5) |
| UTI | 2 (3) |
| Pneumonia | 1 (2) |
| Alcohol misuse | 3 (5) |
| Drug misuse | 4 (7) |
| Recent surgery | 2 (3) |
Table 10 shows the current medication prescribed according to the health-care records.
| Medication | Frequency of people taking medication (N = 59), n (%) |
|---|---|
| Antipsychotic drug | 7 (12) |
| Benzodiazepine | 1 (2) |
| Non-benzodiazepine anxiolytic | 1 (2) |
| Non-benzodiazepine hypnotic | 1 (2) |
| Antidepressant | 18 (31) |
| Dementia medication | 2 (3) |
| Anticonvulsant | 1 (2) |
| Mood stabiliser | 1 (2) |
| Pain relief | 33 (56) |
Table 11 shows the number and percentage of participants who screened positively on the ACE-III for ADL dependence in at least one area (n = 19, 27%). The domain in which the highest number of participants experienced difficulties was mobility (n = 21, 30%).
| Descriptive assessment | Frequency (N = 70), n (%) |
|---|---|
| BADLS dependence | 19 (27) |
| OASys risk of harm: high/very high | 32 (46) |
| Risk Matrix 2000: high/very high | 4 (6) |
Thirty-two (46%) participants had a high or very high risk of harm to self or others, as measured using the OASys. In addition, four (6%) participants had high or very high scores on the Risk Matrix 2000, indicating a high level of risk of sexual offending.
Table 12 shows the proportion of participants who screened positively on the ACE-III who had no friends to talk to about private matters (n = 35, 50%) or to call on for help (n = 35, 50%). In addition, over half of these participants (n = 37, 53%) stated that they ‘never’ had a friend to talk to when they had an important decision to make.
| Social network | Frequency (N = 70), n (%) |
|---|---|
| No friends to talk to about private matters | 35 (50) |
| No friends to call on for help | 35 (50) |
| Never has a friend to talk to when has an important decision to make | 37 (53) |
Six-item cognitive impairment test validation
A total of 495 of the participants completed the 6-CIT in addition to the MoCA for validation purposes. Table 13 shows that 41 individuals screened positively on the MoCA but did not screen positively on the 6-CIT.
| MoCA status | Screened positively on 6-CIT, n (%) | Not screened positively on 6-CIT, n (%) | Total (N = 495), n |
|---|---|---|---|
| Screened positively | 24 (4.8) | 41 (8.3) | 65 |
| Not screened | 18 (3.6) | 412 (83.2) | 430 |
| Total | 42 | 453 | 495 |
An inter-rater reliability analysis using the kappa statistic was performed to determine the level of agreement between the screening tools, with respect to individuals who did or did not screen positively using the MoCA and the 6-CIT. The analysis indicated that the level of agreement between the MoCA and the 6-CIT was ‘fair’: the observed agreement was 88.1% compared with an expected agreement of 80.6% [this is the baseline agreement that we would expect to see by chance (6-CIT κ = 0.39; p < 0.001)].
Summary
-
We recruited 869 prisoners (596 male and 273 female).
-
A total of 100 participants screened positively on the MoCA (12%). Seventy (8%) of the total sample screened positively on the ACE-III. This included 11 individuals who screened positively for possible MCI (1% of the total sample) and 59 who screened positively for dementia (7% of the total sample).
-
Across the whole sample, the prevalence was 8.1% (95% CI 6.4% to 10.1%). When this was stratified by age, the highest proportion was found among prisoners aged ≥ 70 years (16.9%, 95% CI 12.1% to 23.1%). Participants aged 50–59 years had the second highest estimated prevalence at 6.4% (95% CI 4.3% to 9.2%), followed by prisoners aged 60–69 years (4.0%, 95% CI 2.1% to 7.5%).
-
The total weighted estimate for dementia and MCI combined is 8.1% (95% CI 6.4% to 10.1%).
-
We estimate that there are 1090 older prisoners with suspected MCI or dementia in England and Wales.
-
Only two individuals (3%) who screened positively on the ACE-III had a diagnosis of dementia in their prison health-care notes, suggesting current under-recognition.
-
The prevalence rate among our sample of older prisoners is approximately two times higher for individuals aged 60–69 years than it is for those living in the community.
-
We can estimate that older prisoners aged ≥ 70 years are approximately four times more likely to have a diagnosis of dementia than their age-matched counterparts living in the community.
-
It should be noted that estimates are based on structured assessments for MCI and not on a clinical diagnosis.
-
The 6-CIT was not considered an effective tool for identifying potential MCI or dementia among the older prisoner population.
Chapter 3 Part 2
Method
Part 2 established the current health and social care service provision, encompassing assessment, treatment and care for older prisoners with MCI and dementia in prisons, including how well multiagency services were integrated. Training needs were also explored.
Measures
Questionnaire
Two separate questionnaires were issued to governors and health-care managers of all prisons housing men and women in England and Wales (n = 109). The questionnaires included free-text sections, single-response questions and multiple-choice questions. The governor questionnaire (see Report Supplementary Material 7) included questions on service provision for people with dementia and MCI, including any modifications to the environment, training delivered and required, and social care provision. The health-care questionnaire (see Report Supplementary Material 8) included questions on training provision, training needs, current health and social care provision, and future care pathway delivery.
Procedure
An up-to-date list of names and contact details of all the health-care managers was obtained from NHS England and cross-checked with records held by regional offender health leads. Similarly, an up-to-date list of all prison governors was obtained from Her Majesty’s Prison and Probation Service.
The questionnaire was designed by the research team and piloted in prisons in the north-west of England before wider distribution. Small, mainly structural, changes were made to the questionnaires following feedback on the pilot.
The questionnaire was distributed electronically to prison sites where we had a direct e-mail contact. A postal questionnaire was sent if no direct contact was available. In either case, a cover letter was sent with the questionnaire (see Report Supplementary Material 9). A researcher followed up contacts 2 weeks after the initial distribution of questionnaires, by either e-mail or telephone, and then further contact was made 2 weeks later by letter. This process was repeated several times between August 2017 and June 2019. Named recipients were also given the option of completing the questionnaire in a telephone interview with a member of the research staff.
Data analysis
Data were analysed using Statistical Product and Service Solutions (SPSS) for Windows, version 22 (IBM SPSS Statistics, Armonk, NY, USA). Free-text responses were analysed thematically. 74
Results
Establishments
We collected data from 85 prison governors (78%) and 77 health-care managers (71%). There were four (3%) prisons from which we received no data (i.e. from neither the governor nor the health-care manager questionnaire).
Questionnaires were completed between August 2017 and June 2019. Table 14 shows a breakdown of establishments that responded by predominant prison function. Eleven (13%) were privately contracted prisons and 48 (62%) had either partially or fully privately managed health care.
| Prison function | Governor questionnaires, n (%) | Health-care questionnaires, n (%) |
|---|---|---|
| Category C | 35 (41) | 28 (36) |
| Local | 22 (26) | 22 (29) |
| Open | 7 (8) | 9 (12) |
| Female | 8 (9) | 6 (8) |
| Category B | 7 (8) | 6 (8) |
| High security | 6 (7) | 6 (8) |
Non-responder prisons were privately contracted in four (17%) cases and had partially or fully privately managed health care in 16 (50%) cases.
Prison and health-care staff were asked for their definition of an ‘older prisoner’ (Table 15). Sixty-four per cent of prison staff and 56% of health-care staff defined a ‘older prisoner’ as a prisoner aged ≥ 50 years. This fits with the definition in the literature. 8
| Definition | Governor questionnaires frequency (N = 85), n (%) | Health-care questionnaires frequency (N = 77), n (%) |
|---|---|---|
| Aged ≥ 50 years | 54 (64) | 43 (56) |
| Aged ≥ 55 years | 13 (15) | 17 (22) |
| Aged ≥ 60 years | 8 (9) | 7 (9) |
| Aged ≥ 65 years | 10 (12) | 9 (12) |
| Missing | 1 (1) |
For the remaining questions, ‘older prisoners’ were defined as those aged ≥ 50 years.
We asked health-care staff to estimate the number of people in their establishments with a confirmed diagnosis of dementia and/or MCI and the number of those awaiting assessment. Table 16 provides a breakdown of how many older prisoners were reported to have each diagnosis across all prisons.
| Diagnosis/status | Mean number | Cumulative number |
|---|---|---|
| Dementia diagnosis | 5 | 141 |
| Waiting or undergoing assessment for dementia | 3 | 45 |
| MCI diagnosis | 2 | 12 |
Most prisons reported that they had at least one identified older prison lead [n = 67 prisons (79%); 81 leads in total]. Most of these were at a governor grade (n = 42, 52%), followed by custodial managers (n = 18, 22%) and prison officers (n = 16, 20%).
Within health care, 45 of 77 (59%) prisons reported having an identified older prisoner lead (59 leads in total). Most commonly, these were nurses (n = 35, 59%), followed by health-care assistants (n = 11, 19%).
Activities that fell under the responsibility of the health-care older prisoner lead included producing individual care plans, conducting screening assessments for care needs, liaising with community providers, disseminating good working practices and well-being checks.
Current service provision
Health-care staff reported that prisoners with dementia or MCI were most commonly identified during a health consultation for another issue (n = 64, 83%) and/or through screening on reception (n = 62, 81%). Six prisoners (8%) were identified through screening on discharge from prison.
Routine dementia screening for all older prisoners on reception was conducted at 23 of 77 (30%) prisons. Fifteen out of 77 (19%) prisons reported that they routinely screened all older prisoners (not just new receptions) for dementia or MCI. Of these, most would reassess every 7–12 months (n = 9, 60%), three (20%) would reassess every 0–6 months, one (7%) would reassess every 13–18 months and the remainder would reassess on an individual basis. Routine screening prior to release as part of resettlement was conducted at only eight (10%) establishments.
Table 17 provides a breakdown of the screening tools used across the establishments (some establishments use more than one).
| Screening tool | Frequency (N = 23), n (%) |
|---|---|
| MMSE | 14 (61) |
| ACE-III | 8 (35) |
| MoCA | 5 (22) |
| 6-CIT | 4 (17) |
| GPCOG | 3 (13) |
| CAMCOG | 2 (9) |
| Other locally developed tool | 2 (9) |
| Clock-drawing test | 1 (4) |
Around half of prisons surveyed [46 (54%) governor questionnaires and 36 (47%) health-care questionnaires] described additional support or modifications to the prison environment that had been provided or developed specifically for prisoners with dementia or MCI.
Both health-care and prison staff were asked about all modifications, and there were some interesting discrepancies in their responses. For example, 87% of prison staff reported the use of prisoner carers, compared with 67% of health-care staff. Conversely, 59% of prison staff reported the use of regular health screening, compared with 72% of health-care staff. Table 18 provides a breakdown of types of modification taken from governor or health-care questionnaires. The sources of these data are given in Report Supplementary Material 7 and 8. The choice of source was made in relation to which would likely generate the most accurate information (e.g. information of health screening from the health-care questionnaire, information on exercise from the prison staff questionnaire).
| Modification | Frequency, n (%) |
|---|---|
| Handrailsa | 31 (67) |
| Provision of incontinence materialsb | 28 (78) |
| Regular health screeningb | 26 (72) |
| Bigger/more accessible prison cellsa | 25 (54) |
| Exercise/activity/canteena | 19 (41) |
| Signposting/highlighting of key areas or itemsa | 10 (22) |
| Improved lightinga | 6 (13) |
| Provision of easy to remove clothinga | 5 (11) |
| Removal of mirrorsa | 1 (2) |
Other modifications included alarm call bracelets and personal alarms, magnifying screens, long-handled equipment, memory boards and prompt cards, personal emergency evacuation plans, support and therapy groups, social care aids and specific older prisoner wings or units.
Eleven out of 77 (14%) of the prisons responded that there was a support group (or similar) specifically for individuals with dementia or MCI, most often run by prison staff, mental health teams or the older prisoner lead. Groups included a dementia-friendly music group or choir, gym groups, holistic care and support, memory cafes, an over ‘45s’ focus group, over 50s well-being and mindfulness, cognitive stimulation therapy, and arts and crafts.
More than half of the prisons (n = 44, 57%) reported that they had a clear referral process for more detailed assessment of older prisoners with suspected dementia or MCI, and 29 (38%) prisons reported that external health and social care services provided this assessment or treatment.
The majority of prisons reported that they did not have a defined care pathway for prisoners with dementia or MCI (n = 53, 69%); however, just under one-third of these (16/53, 30%) were in the process of developing one.
Care planning between health-care and prison staff occurred to varying degrees in 53 (69%) establishments. This was, on the whole, fairly rudimentary and involved attending care planning meetings (77%), employing prisoner carers (49%) and sharing guidelines and resources.
Social care
Health-care staff were asked about how social care needs were identified, assessed and met in their establishment. Very few prisons used standardised assessment tools for social care needs (n = 7, 9%). Staff indicated that needs would normally be identified through initial health screening on reception. Most respondents indicated that anyone could make the referral for assessment, but it was most commonly made by reception and induction staff.
The formal identification of social care needs most commonly fell to health-care and other clinical staff (n = 30, 39%) or social workers, including both prison-based social workers and local authority staff (n = 38, 49%).
The development of care planning was mostly attributed to social care staff (n = 33, 43%) or health-care staff (n = 12, 16%), with a clear link that in many cases this was multidisciplinary and involved complex case meetings with prison and safer custody staff (n = 13, 17%). In several cases, there was evidence that dementia and older prisoner leads took responsibility for this joint working (n = 4, 5%).
Almost half of health-care staff stated that they had advocacy arrangements in place for those with social care needs (n = 36, 47%). Some were internal to the prison, but others used local advocacy services, including from the local authority.
All health-care staff were asked who was responsible for meeting social care needs, as defined in the Social Care Act 2014. 75 The highest proportion attributed this responsibility to the social care team (n = 17, 22%), followed by health care (n = 13, 17%) and joint responsibility between health care and social care (n = 10, 13%). The prison was seen as having some responsibility by over one-quarter of respondents, with many (n = 15, 19%) suggesting that all three shared this responsibility or that it was down to ‘everybody’.
Both health-care staff and prison staff were asked about how well the local authority was meeting its responsibilities as outlined in the Social Care Act 2014. 75 Responses to this are detailed in Table 19.
| Response | Health-care staff frequency (N = 77), n (%) | Prison staff frequency (N = 85), n (%) |
|---|---|---|
| Very well | 23 (30) | 21 (25) |
| Fairly well | 30 (39) | 42 (49) |
| Not very well | 11 (14) | 11 (13) |
| Not at all well | 3 (4) | 5 (6) |
Ongoing issues with Social Care Act 2014 compliance
We analysed free-text comments from staff regarding their views on specific issues with their local authority and/or compliance with the Social Care Act 2014.
Staff indicated that one of the most common problems was delays in arranging assessments, diagnosis and/or the provision of care. Staff expressed frustration when prisoners did not meet the criteria for social care under the Act, with a suggestion from one that the threshold should be lower for individuals in prison.
In high-security prisons, security vetting issues resulted in limited or delayed establishment access for external staff. The high turnover of local authority staff caused further delays and inconsistency. It was felt that in some local authorities there was poor understanding of the complexities of working in a prison or with prisoners. In addition, in some establishments there seemed to be misunderstanding about the remit of the local authority and the prison and who was responsible for what.
A number of challenges were noted in practically addressing social care needs of prisoners with dementia or MCI. The environment was most commonly cited, in that the layout of many prisons and cells made any reasonable adaptations difficult to fulfil. Similarly, basic limitations of the prison regime, such as being locked up at night, led to problems with prisoners who may be disorientated and confused.
Problems identifying the signs and symptoms of dementia and MCI was another commonly reported issue; this was related to limited staff knowledge on the issue, lack of training and, particularly in local prisons, the high turnover of prisoners:
The only problems are the lack of understanding of the complexities of working in a very busy Cat [category] B local prison with a high turnover of short duration stays (6-week average). The expectations that they have are unnaturally high and are very difficult to meet.
Governor questionnaire
For prisoners with confirmed dementia and social care needs, out-of-hours provision was another concern. Staff indicated that prisoners’ needs persist throughout the night, but additional care support is frequently unavailable.
Some prisons emphasised the additional difficulties with the ageing prison population, particularly those convicted of sex offences:
Currently, nationally, there is no provision for any prisoner to access residential or nursing care needs within a prison setting. We can only offer a maximum of four social care visits per day. If someone requires more care than this, we cannot provide it. The current law states that we cannot release sex offenders on temporary licence should this be a suitable option.
Governor questionnaire
Many prisons, however, highlighted examples of good practice. One health-care team noted the benefit of the provision of a full-time social worker based at the prison, rather than based externally. The benefits included quicker assessments and the improved opportunity for joint working between the prison, health-care and social care staff. Several teams described excellent working relationships with the social care team from the local authority, whereas another commended regular engagement through meetings:
We have a very supportive relationship with the local authority; we have a monthly social care meeting, a weekly bed management meeting which they attend.
Many of the prison staff who responded had no issues with the local authority in meeting social care needs and reported very good partnerships, with one prison reporting that their local social care team had been ‘Fantastic in supporting residents and guiding staff . . .’ (governor questionnaire), whereas another said that their local social care lead was ‘. . . visible, approachable, realistic and supports the prison’ (governor questionnaire).
Prisoner carers
Forty-four out of 77 (57%) prisons reported that their establishment employed prisoner carers. The appointment of these prisoner carers mainly occurred following staff recommendation or self-referral or through an existing buddy or peer-mentor system. Twenty-seven prisons (61%) had formal selection criteria for this role, such as security vetting, training, risk assessments and enhanced status.
Training was provided in three-quarters (32/44, 73%) of establishments where prisoner carers were employed. Table 20 provides a breakdown of the areas covered in training.
| Area covered | Frequency (N = 44), n (%) |
|---|---|
| Remit of the role | 23 (53) |
| Communication | 19 (43) |
| Use of wheelchairs | 18 (41) |
| Mental health awareness | 16 (36) |
| Safe lifting | 9 (20) |
| Othera | 8 (18) |
Prison staff were involved in training delivery in 18 establishments (41%), health-care staff were involved in training delivery in 15 establishments (34%), social workers were involved in training delivery in 11 establishments (25%) and third-sector workers were involved in training delivery in 10 establishments (23%).
The range of reported responsibilities of prisoner carers are provided in Table 21. Most prisoner carers (34/44, 77%) were paid for this role, with wide variation in rates of pay (between £2 and £16 per week).
| Responsibility | Frequency (N = 44), n (%) |
|---|---|
| Carrying plates/trays | 41 (93) |
| Completing applications | 38 (86) |
| Pushing wheelchairs | 37 (84) |
| Cleaning cells | 37 (84) |
| Keeping company | 35 (80) |
| Writing letters | 34 (77) |
| Using the telephone | 29 (66) |
| Assistance with getting dressed | 7 (16) |
| Assistance with getting in/out of bed/chair | 7 (16) |
| Assistance with washing | 4 (9) |
| Other (assist with medication/canteen) | 4 (9) |
| Assistance with using the toilet | 1 (2) |
Current training provision
Prison staff training
One-quarter of prison staff (n = 22, 26%) reported that training (internal or external) was provided for the identification of dementia and/or MCI.
Staff included in the training were most commonly prison officers and governors (both n = 18, 82%). In half of the prisons (n = 11, 50%) training was also delivered to chaplaincy and education staff and in 10 prisons (45%), prisoners themselves received training on dementia and/or MCI.
The most common format for training delivery was face-to-face, meetings and lectures (n = 13, 59%) or interactive workshops (n = 8, 36%), followed by online (n = 8, 36%).
Table 22 provides a breakdown of the areas covered by current prison staff training in relation to dementia and MCI.
| Training content | Frequency: governor questionnaires (N = 22), n (%) |
|---|---|
| General awareness | 19 (86) |
| Early warning signs | 11 (50) |
| Impact on functioning | 9 (41) |
| Managing challenging behaviours | 9 (41) |
| Local referral processes | 7 (32) |
| Local care pathway | 6 (27) |
| Detecting and treating anxiety/depression | 6 (27) |
| Communication techniques | 6 (27) |
| How to offer support/make low-cost adaptations to the living environment | 4 (18) |
| Other (one-to-one key worker awareness) | 1 (5) |
Specialist external agencies were involved in the provision of training in 13 of 22 (59%) prisons. Most commonly (n = 9, 41%), this was a voluntary sector or charity (e.g. Age UK, Alzheimer’s Society or other local charities), followed by the local authority (n = 6, 27%).
Service users, carers or experts by experience were involved in the provision of training in 12 (55%) prisons. When specialist external agencies and/or service users were involved, this was most commonly in the facilitation of the training (11/16, 69%).
Health-care staff training
Sixteen (21%) health-care staff reported that training (internal or external) was provided for the identification of dementia and/or MCI. This training was most commonly received by nurses (n = 13, 81%) and health-care assistants (n = 12, 75%), followed by nurse practitioners and pharmacists (both n = 6, 38%).
The most common format for training delivery was face-to-face meetings or lectures (n = 8, 50%), followed by online (n = 7, 44%).
Table 23 provides a breakdown of the areas covered by current training for health-care staff in relation to dementia and MCI.
| Training content | Frequency: health care (N = 16), n (%) |
|---|---|
| General awareness | 13 (81) |
| Early warning signs | 9 (56) |
| Impact on functioning | 7 (44) |
| Managing challenging behaviours | 3 (19) |
| Local referral processes | 6 (38) |
| Local care pathway | 1 (6) |
| Detecting and treating anxiety/depression | 1 (6) |
| Communication techniques | 7 (44) |
| How to offer support/make low-cost adaptations to the living environment | 4 (25) |
Specialist external agencies were involved in the provision of training in seven (44%) health-care services where training is currently delivered. Most commonly, this was the local authority (n = 5, 31%) and voluntary sector (n = 3, 19%).
Service users, carers or experts by experience were involved in the provision of training in three (19%) cases. When specialist external agencies were involved, this was most commonly in facilitating training and designing the referral process.
Training needs
Both health-care and prison staff were asked about their training needs, regardless of current arrangements.
Prison and health-care staff agreed that face to face was the preferred format, using interactive seminars or workshops rather than meetings or lectures. Both groups also agreed that the least preferable option was self-study. There was also agreement that the preferred training method was group discussion or debate.
Both groups said that training should take place at the prison to enable staff to be released from duties and to allow easy access. Some staff indicated that a prison training unit, or similar, was also favoured, as there is likely to be less disruption from the prison regime and staff may find it easier to engage if they are outside their usual work surroundings.
Health-care staff stated that they would prefer training to be delivered by external clinicians (i.e. a memory clinic psychiatrist, psychologist or nurse practitioner).
Table 24 provides a breakdown of the mean rankings of what should be included in training for both prison and health-care staff (1 is most important and 9 is least important).
| Training element | Staff, mean ranking of what should be included in training | |
|---|---|---|
| Prison | Health-care | |
| Early warning signs | 1.8 | 1.9 |
| Impact on functioning | 3.8 | 3.2 |
| Local assessment process | 6.0 | 5.2 |
| Local referral process | 4.8 | 5.2 |
| Communicating with individuals with MCI or dementia | 4.1 | 3.9 |
| Local care pathway | 6.5 | 5.8 |
| Causes | 6.2 | 5.2 |
| Available support/modifications to the environment | 5.8 | 5.4 |
| Identify key individuals within the prison | 6.1 | 5.8 |
| Impact on ability to conform to prison regime | 4.7 | 5.4 |
| Links to other services/charities who can help | 8.3 | 7.5 |
| National dementia strategy | 9.2 | 8.2 |
The majority of health-care staff opted for a full or half day of training (n = 57, 80%), whereas the prison staff opted for half a day or less (n = 61, 76%).
More than 70% of both prison and health-care staff agreed that the following staff should receive training on dementia or MCI: health-care assistants, nurses, nurse practitioners, offender managers, prison officers, governors and prisoner carers.
Summary
Part 2 of this study sought to identify current health and social care service provision, encompassing assessment, treatment and care for older prisoners with MCI and dementia in prisons, including how well multiagency services are integrated. Training needs were also explored.
Two separate questionnaires were issued to governors and health-care managers of all prisons housing males and females in England and Wales (n = 109).
Data were collected from 85 prison governors (78%) and 77 health-care managers (71%). Analysis showed the following:
-
Most prisons reported that they had at least one identified older prison lead (n = 67, 79%).
-
Health-care staff reported having an identified older prisoner lead in 45 (59%) respondents.
-
Health-care staff reported that prisoners with dementia or MCI were most commonly identified during a health consultation for another issue (n = 64, 83%).
-
Fifteen out of 77 (19%) prisons reported that they routinely screened all older prisoners for dementia and MCI.
-
Interestingly, around half of prisons surveyed (n = 46, 54%) described additional support or modifications to the prison environment and 36 (47%) health-care questionnaires reported adaptations.
-
The majority of prisons (n = 53, 69%) reported that they did not have a defined care pathway for prisoners with dementia or MCI.
-
One-quarter of prison staff (n = 22, 26%) reported that training (internal or external) was provided in the identification of dementia and/or MCI, whereas only 16 (21%) health-care staff reported such provision.
The questionnaire was successful in establishing current dementia and social care provisions, and establishing future training needs, as part of an initial scoping exercise for part 5 (see Chapter 6).
Chapter 4 Part 3
Method
The aims of part 3 were to explore the experiences of older prisoners with dementia and MCI and to engage with a range of informants around the day-to-day issues faced by staff and residents with regard to dementia and MCI. A focused ethnographic qualitative study of a small number of individuals76 was conducted. Semistructured interviews were undertaken with a range of prisoners from sites included in part 1 (see Chapter 2). Relevant individuals supporting these prisoners and those in key strategic positions also took part in semistructured interviews.
Focused, time-limited ethnography is a valuable research method for capturing experiences of dementia. 77,78 The observation identified important aspects of care, or barriers to support, that may not have been picked up in the semistructured interviews, and provided rich data on the discrete contextual and environmental influences of being in prison with dementia and how these differ from those in the community with dementia. Hubbard et al. 77 suggested that the combination of observation and flexible qualitative interviewing is an effective way of privileging the voice of people with dementia so that quality of life in care and institutional settings can be understood. These combined methods revealed important issues, with implications for training, about the level of communication and interaction, as demonstrated in other institutional ethnographic studies. 77
Focused ethnography
Sample
A purposive sample was recruited. Nine male prisoners were identified from various types of prisons who had a range of severity of cognitive impairment. The same informed consent process as detailed in part 1 (see Chapter 2) was followed.
Procedure
The approach to conducting the focused observations was pragmatic and flexible, with observations concentrating particularly on aspects of prison life in which there was contact and interaction with other prisoners and staff. This varied according to institutional context. Focused ethnographic observations of each person undertaking discrete, time-limited tasks and activities were conducted, and detailed field notes were made.
We know from our experience of research in prisons that the regime consists of key events for most prisoners on most days. These include multiple communal activities, including mealtimes and exercise, and focused work, educational activities and interaction with health-care providers, when appropriate. Specific examples of activities we observed included:
-
collecting meals from the wing servery
-
spending time at work
-
negotiating access to off-wing activities [e.g. health-care appointments (routine and acute), vocational activities, gym]
-
attending off-wing activities
-
attending social activities in the wing
-
using time in cell.
For participants included in this part of the study, we recorded field notes that included details of the place and time of the observation, the setting and the details of what happened during the observation.
The details of field notes varied depending on the event being observed. Observations recorded detailed verbatim verbal interactions, as well as non-verbal. In the instance of activities in communal spaces, the observer focused on consenting prisoners and staff. The main focus of observation was to consider how the physical space, environment and material objects may have had an impact on prisoners with dementia and MCI. Consideration was given to how the physical environment may present difficulties for those with impaired cognitive function, and how successfully that individual could complete tasks and navigate their environment.
After each observation session, the researcher completed more detailed field notes, expanding concise notes into sentences and adding further comments and reflections. These notes were typed up into a narrative account describing what happened and what the researcher had been able to learn about the prisoners’ day-to-day experiences. The researcher differentiated between their perceptions and the actual activities that occurred.
Please see Consent/ethics issues for details of the researcher safety protocol.
Informed consent
Following the general principles of ethnographic research, not every prisoner on a wing was consented individually. Instead, in line with accepted practice, some general information was provided to prisoners that we were completing an observational study aiming to understand some aspects of prison life and to understand the management of health problems for some prisoners. Those eligible to be involved received further information (see Report Supplementary Material 10–12) and their consent was requested (see Report Supplementary Material 13–15). No details were recorded during the observations that revealed the identity of prisoners.
Semistructured interviews
Sample
Semistructured interviews were conducted with staff members, other prisoners and carers, as well as with the individuals themselves, to provide multidimensional narratives of the experience of living with dementia or MCI in prison. When possible, we asked the prisoners with suspected MCI or dementia to identify an individual who they felt could provide a valuable insight into how they managed their needs on a day-to-day basis. Speaking with individuals in the following different key roles helped us to achieve triangulation of data:
-
prison staff member (e.g. personal officer, senior officer, wing officer)
-
prisoners (e.g. cellmate, carer, cleaner, co-worker)
-
health-care staff [e.g. health-care assistant, nurse, psychologist, psychiatrist, general practitioner (GP)].
Health-care managers, governors and any other key members of staff who could provide a more strategic or organisational-level perspective were also approached to participate in semistructured interviews.
A semistructured interview schedule was used (see Report Supplementary Material 16), based around a number of a priori themes. These preliminary themes were based on our academic and clinical knowledge of the subject area. Additionally, interviewees were given the opportunity to expand on any issues that they felt were relevant but had not been covered by the interview schedule.
Procedure
Staff members were encouraged to reflect on their responsibilities for this prisoner group in the context of the wider environmental and organisational setting in which they work. This included critical consideration of their training needs, role, and personal confidence and competencies.
The interviews were audio-recorded. Interviews lasted between 20 minutes and 1 hour. If individuals preferred that the interviews be conducted over a number of occasions, then this was accommodated.
Qualitative analysis
The qualitative data (transcriptions and field notes) obtained during interviews and observations were analysed using the framework method. This method produced a matrix of summarised data that provided a structure for analysing and reducing the data. A key benefit of this approach, in comparison with other forms of thematic analysis, is that the context of participants’ data was not lost. 79 In addition, the framework method was selected because it is particularly useful for informing the design of training materials (part 5; see Chapter 6), as both predefined and emergent themes can be used.
Gale et al. 80 proposed seven stages in this approach. Stage 1 involved professional transcription of the data. Transcriptions were produced verbatim; however, the focus was on content, rather than pauses and tone. During stage 2, the researcher who conducted the qualitative element familiarising themselves with the whole interview. Coding commenced at the third stage of the process, which involved marking text directly on paper. Stage 4 involved the development of a working analytical framework. After the initial few transcripts had been coded, a set of codes was developed and applied to the analysis of all subsequent transcripts. Numerous adaptations were made to the analytical framework throughout the analysis process until no new themes emerged. The analytical framework was applied to all subsequent transcripts using the existing categories and codes during stage 5 of the analysis. During stage 6, framework matrices were developed and data were charted into the matrices. This involved summarising the data by category for each transcript. The chart included references to illustrative quotations. The final, seventh stage was the process of interpreting the data.
This part of the study provided rich data describing the lived experience of people with dementia in prison.
Consent/ethics issues
Prisoner and staff participants (focused ethnography: direct and indirect participation)
The focus of observations was on prison staff and the individual prisoners with dementia or MCI. The direct consent of the specific prisoner being observed was obtained. Similarly, the individual consent of wing staff and health-care staff dealing directly with the prisoner was sought. We ensured that only details from observations concerning these consented individuals were recorded. Field notes did not detail any actions, speech or interactions with staff or other prisoners who did not provide consent.
Posters displayed on the residential wing where the individually consented prisoner lived stated the purpose of the research and the dates of researcher visits, giving prisoners the ability to opt out verbally via the researcher. Similar posters were displayed in all other parts of the prison that the consented individual prisoner may have visited (e.g. library, gym, education, chapel), which allowed verbal opt-out for prisoners, accompanied by verbal opt-out for staff. The verbal opt-out procedure is the process whereby an individual verbally declines to take part in a research activity. The individual may have read a poster, been informed by peers/colleagues or observed the research being undertaken and have subsequently decided they would prefer not be involved. To verbally opt-out they can approach the research team, or peers can approach prison staff, to inform them of their decision. Prison staff will then inform the researcher.
Specific individual consent was sought from any prisoner who had a more formal, rather than ‘passing’, interaction with the subject (i.e. a peer carer/buddy/mentor, etc). When a ‘passing’ interaction became a potentially more meaningful or in-depth interaction and was referred to in detail in observation notes, consent from the second prisoner included in the data was sought post hoc.
Prisoners’ carers and family members (semistructured interviews)
Prisoners’ carers were approached only with the consent of the prisoner participant. Informed consent of carers was obtained prior to their participation.
Results
A total of 42 interviews were conducted with a range of informants. Interviews were undertaken across five prisons, either in person or over the telephone. Prison characteristics and interviewee roles are given in Tables 25 and 26.
| Prison | Description | Operational capacity (n)a |
|---|---|---|
| A | Category C sex offender-only prison, with population aged ≥ 50 years approaching 50% | 751 |
| B | Local prison with a high-secure function; no discrete facilities for elderly prisoners | 1072 |
| C | Local prison; no discrete facilities for elderly prisoners | 700 |
| D | Category C prison with an older persons’ wing and a significant sex offender/vulnerable prisoner population | 1169 |
| E | Local prison; no discrete facilities for elderly prisoners | 1212 |
| Role | Number of interviewees |
|---|---|
| Governor grade | 3 |
| Prison officer | 9 |
| Prisoner with or suspected to have MCI or dementia | 9 |
| Prisoner, peer | 4 |
| Prisoner with caring responsibilities | 1 |
| Social care worker | 4 |
| Third sector/volunteer | 1 |
| Head of health care/mental health | 5 |
| Probation worker | 1 |
| Health-care worker | 2 |
| GP | 2 |
| Psychiatrist | 1 |
From the data, four main themes emerged:
-
the challenge of an ageing prison population
-
what it is like to be old in prison
-
the importance of collaborative working relationships across professional boundaries
-
the challenge of training the workforce and peers.
Theme 1: the challenge of an ageing prison population
With the ever-aging population coming through the prison gates, I think it is a new presentation that a lot of staff aren’t used to.
Social worker, prison C
A number of the professional respondents noted how much the age demographic of the prison population had changed since they had started working in the prison. Staff working in prison A noted that nearly half of their prisoners were now aged ≥ 50 years, a situation that they would have regarded as inconceivable perhaps 10–15 years ago. Although we were asking questions specifically around dementia and MCI, staff and prisoners alike expressed concerns around the full range of chronic health conditions that are commonplace in this ageing population.
Officers spoke of how the ageing demographic had an impact on the duties that they were routinely undertaking, which may not have been the case previously:
We sit and help do everything, from social workers to a shoulder to cry on, to counsellors; we do everything. I mean . . . there’s even talk that somebody has got some of the prisoners help to brush their teeth, have a shave.
Prison officer, prison A
A number of staff members, particularly prison officers and governors, noted how prisoners who were ageing and potentially cognitively impaired provided them with a fundamental challenge to how they dealt with behaviour, which in ‘normal’ circumstances with younger prisoners would routinely be viewed as refractory:
It’s not so much rolling round the floor with them nowadays, it’s looking to see what’s wrong with them and to see what we can do that’ll help them. If we’re not going to help them, they’re going to be more distressed and that distress . . . it’s just going to make them worse, and then it’s going to look like they are being destructive.
Prison officer, prison A
This difference in approach was echoed in other establishments:
. . . instead of using force straight away, it’s more of talking to them, explaining what’s happening, we’re going to have to put hands on, we’re just going to have to guide and hold you back. And they kind of realise then, right, this is what’s happening, they’ll calm down.
Prison officer, prison C
Another officer appeared to question some basic principles of their role around the management of this group:
I always felt that a prisoner with dementia should be treated differently. Because if a (young) prisoner is violent they know what they’re doing, but someone with dementia doesn’t . . . how do we discipline prisoners who don’t actually know what they’re doing? But they are a prisoner in prison subject to prison rules and regulations like everyone else.
Prison officer, prison D
A prisoner raised an even more fundamental issue: whether or not there was a need for those who had been convicted of historical offences and posed no risk to the community to be imprisoned:
I think the criminal justice system is a bit wrong with people with dementia. They can’t fully remember everything that’s happened . . . they just tend to feel, well, yeah, he’s guilty and that’s it, whether you are or not . . . Older people with a historical offence that haven’t been in trouble since . . . should be allowed to maybe be tagged.
Resident, prison A
Both staff and prisoners commented on the unsuitability of the physical environment in many establishments for coping with less mobile residents. Staff in one prison noted that the possibilities for changes to the environment were limited because of the prison’s age and listed building status. Others noted limitations that were perhaps more easily addressed. For example, in one prison, all accommodation for vulnerable prisoners (including many elderly men, owing to the nature of their offences) was located at least two floors up.
On more than one occasion senior staff noted that their ability to effect change locally was limited by resources, which had reduced significantly over the period of public sector austerity introduced nearly 10 years before. The view was expressed that local initiatives were bound to be limited in their impact until there was recognition from central government of the size of the problem:
There needs to be an awareness at the centre, at headquarters that, first of all, we’ve got to identify the numbers, haven’t we . . . It needs to come at a Ministerial level . . . because that’s where the money comes from ultimately, doesn’t it?
Governor grade, prison D
One prisoner offered a straightforward response to the issue of resource availability for older prisoners:
The senior support group. Sometimes you have to split them up because there’s not enough room for them all. Well, make room. If the prison’s catering for the older population, increase the space so the community grows.
Peer of elderly resident, prison A
The same prisoner maintained this pragmatic approach to the ‘problem’ of accommodating people in prison throughout the conversation, which was informed by time spent in other prisons:
If they’ve got a problem with the bunk beds, put two single beds in there. They do that at [name of prison].
Peer of elderly resident, prison A
A number of respondents spoke of the fragility of some local initiatives. For example, one prison officer spoke of an approach championed by a former member of staff:
Our old senior officer did start . . . a little quiet corner and on an afternoon. She used to get them out and give them board games, for them all to come out.
Prison officer, prison C
The officer said that the idea of the quiet corner had waned, attributing this to older residents losing interest in the initiative. However, a peer carer on the same wing offered a different reason for its demise:
When [name of senior officer] was on, she started getting the . . . older lads out, but that seems to have gone now she’s moved to another wing. So, things change with new officers and what have you.
Peer carer, prison C
The same prison officer also wondered whether or not, because they were working in a local prison, their ability to respond to the needs of elderly prisoners properly was impeded by having to serve a large and transient population. The pressure to serve the courts and deal with short-term prisoners seemed to overtake the prison’s ability to plan and provide for those with dementia:
There’s nothing that’s been put in place. I don’t think it’s been identified properly . . . when they go to another jail, I’m not sure if they have more of an input into it, but I think being a local, they haven’t implemented anything.
Prison officer, prison C
A governor in another prison noted that the process of benchmarking had served to remove staff’s ability to do the ‘nice to do’ tasks, leaving resources only for essential tasks to be undertaken.
Members of health-care teams shared that they were unsure how comprehensively they were identifying those at risk of dementia, as their current systems had been designed with a younger demographic in mind:
We do a reception screen on everybody that comes through . . . is it robust enough to actually pick up people with dementia . . . I don’t know whether that’s been tested . . . it would be useful for me to know that our reception processes are picking people up and their needs are being met.
Health-care manager, prison E
The enormity of the task faced by health-care departments in meeting the needs of elderly prisoners was commented on by a number of interviewees, who had the shared view that resources were too scarce and were negatively affected by regular changes in health-care providers, and that there were ongoing problems with recruiting and retaining staff:
They’re putting a sticking plaster on a dam. They have too little GPs. When you look at how many men we’ve got here and what complex needs we have the team we have is far too small, it’s quite transitory . . . staff come in, we’re going to conquer the world, we’ll get this sorted, within 3 weeks they’re gone.
Third-sector worker, prison D
One senior manager succinctly summed up how prisons were struggling to provide a holistic service for older prisoners and those with dementia:
These prisoners . . . if they were out in the community they would be in residential care setting with lots and lots of support and day centres and, you know, the stuff that helps people, whereas in prison we’re not able to do that.
Governor grade, prison D
Theme 2: what is it like to be old in prison?
The different moods, the way they’ve changed over the year, the way they do things differently to other people; how some of them just look lost, and they walk round the landings literally lost, like a ghost almost.
Prison officer, prison A
The previous theme explored how prisons and prison staff are now required to cope with an increasing number of older prisoners, which has resulted in a population with complex medical needs compounded by dementia and MCI. We noted above how this had led a number of staff to question their professional role, as tasks they would previously not have thought twice about (e.g. restraining or disciplining prisoners displaying refractory behaviour) now seemed wholly inappropriate for this group.
That said, the role of front-line officers was noted as very important in influencing how well older prisoners were able to live in prison. Good staff were described as caring, with personal knowledge of people living on their unit and able to use this familiarity to highlight, particularly to health-care staff, changes in a person’s well-being and any deterioration in their health and/or functioning. Prisoners interviewed often named particular officers as being concerned for their welfare and, importantly, trustworthy. Several examples were given of when staff had developed local initiatives for particular difficulties that prisoners were experiencing. For example, at prison A, a resident told us of a reminder board that an officer had developed for him, which allowed him to tick off everyday tasks as they were completed on a daily basis.
At a prison-wide level, the senior prison manager interviewed at prison A, where those aged ≥ 50 years accounted for nearly half of the prison population, spoke about his vision of the prison community being positively influenced by adopting an approach of ‘active citizenship’. The overarching aim of this was for staff and residents to be jointly responsible for developing the prison as a community, with shared goals and ideals, rather than living and working in a ‘them and us’ environment.
Residents, and some staff, highlighted the issues that arose as they tried to negotiate the many rules, both formal and informal, that influence life in prison on a day-to-day basis. Although prisons across England collectively share the same overarching purpose, establishment-specific customs and practice require prisoners to learn and adapt as they move around the estate. This can influence even the most basic elements of daily life. For example, a resident in prison A noted that, at a previous jail, he had been able to simply ask for a more comfortable chair for his cell and ‘you would get it and there was no problem at all’, whereas in his current prison ‘it is hard to get a chair in your cell . . . you’re only allowed a stool, but you’re allowed to have a cushion to put it on’. Although he had not yet received a comfortable chair, he did note that the cell he was currently in was quite well equipped with a range of mobility aids, for example grab-rails for the toilet, although at present he had no need for them. The same person also noted that in prison A he feared slipping on the floors, which were always kept well mopped and polished, whereas in a previous establishment cleanliness was not of the same standard and thus he had no such concern. Similarly, one respondent with suspected dementia described falling foul of staff expectations:
I’m a bit slow. But I get there but some younger officer[s] shout, come on, hurry up, we haven’t got all day. And I think . . . I’m going as fast as I can here.
Elderly resident, prison A
Another resident noted the need to adhere to the regime, including the timing of activities:
We all have blips don’t we, but in here if you’re not at a certain place at a certain time, you miss the boat anyway.
Elderly resident, prison C
Concern was expressed that older prisoners, potentially vulnerable due to dementia, could be preyed on or exploited by younger prisoners. One prisoner shared his experiences of this:
These tough nuts as I called them in here, they’d pick on you more ‘cause they knew you couldn’t really stick up for yourself much. And you’d tend to give in . . . You just go into your own little shell a bit then. It’s terrible.
Resident, prison A
Another prisoner told us:
I’m scared . . . because sometimes people will hit me and I’ll fall over.
Resident, prison D
In another prison, having a very mixed population on vulnerable prisoner wings was highlighted as contributing to the issue:
We get young fellas who are from other wings, because they’re getting bullied on other wings, who think they’re big boys, which they’re not. But they can intimidate the older guys . . . if someone says, have you got a vape in this place, next minute you’ve got them at your door every 2 minutes.
Peer carer, prison C
This carer felt that the answer lay, at least partly, in having discrete accommodation for older prisoners:
This prison itself is not made to look after these guys, they need to be in a place, there’s too many young guys running around, and they get . . . intimidate[ed]. [Even] if they go to the health care . . . they’re intimidated by the mains because they’re VPs [vulnerable prisoners].
Peer carer, prison C
However, this issue is not straightforward. One younger man spoke of the benefits he had experienced from sharing with an older person:
. . . this is the first time I’ve ever been with somebody not my own age . . . I always find that when I’m in with somebody my age I end up getting into trouble so it’s not a bad thing me being with somebody a bit older . . . I’m staying out of trouble.
Cellmate of elderly resident, prison A
Similarly, the idea of older prisoners being ‘protected’ by younger peers was brought up in a number of interviews:
If anyone’s being funny with him [older prisoner] . . . I’ll say . . . just make sure you’re looking after my dad, yeah. And he chirps up a bit then, see. It’s like a boost, a confidence boost.
Peer of elderly resident, prison A
What was clear throughout the interviews was that the vast majority of staff regarded elderly prisoners as different from, rather than simply older versions of, younger prisoners:
You just can’t treat an older person the same as a 20-year-old. Completely different, [a] 20-year-old can be self-sufficient, get on . . . if they haven’t got pillows they’ll pinch it from someone else or they’ll go to officers and they’ll ask for some. A lot of our guys if they haven’t got a pillow, they’ll just make do with what they’ve got because they haven’t got the capacity or the confidence or the ability to go to the officers and say this is my problem.
Third-sector worker, prison D
Peer carers are widely used across the prison estate. There are guidelines for the roles and responsibilities of peer carers; for example, they cannot undertake personal care tasks, such as helping a person with dementia to shower or use the toilet, but they can offer support with the requirements of the prison regime. Those we spoke with who had dementia or suspected dementia were positive about this service:
They come in and do things I’m struggling with like mopping the cell out for me . . . and doing certain jobs for me, doing my bed, which I have difficulty with. And pushing me over to meds when I need to be in my wheelchair.
Elderly resident, prison A
One of the other residents, he does my canteen . . . for me and adds it up. And the other carer comes in, does my menu for me.
Elderly resident, prison A
It would seem that the boundary between being an official peer carer and ‘just’ another resident can be blurred on occasion. A cellmate (not an official carer) of an elderly peer with dementia told us:
He’s not asked me to do it but because, like I say, we do get along and obviously I take his age into account, I’ll try and do things in the cell, like, you know, tidying up . . . He can make himself a drink or a lot of the time I’ll make him a drink or I’ll wash up his plate and his cutlery . . . he’ll always say to me, oh, you don’t have to do that . . . but I’m like, no, no, you sit there, you’re alright and I’ll quite happily do it for him.
Cellmate of elderly resident, prison A
This concern extended to the man speaking to staff to try to ensure that the elderly resident would be cared for after his release, which was imminent:
I’m getting out in May . . . I’ll make sure if I can to staff and to maybe some of the officers that they don’t just put anyone in there, you know what I mean, somebody who they think he might get along with and who is going to pull his weight in the pad.
Cellmate of elderly resident, prison A
One member of staff working in a large local prison expressed concern that the needs of elderly, confused prisoners may be neglected by staff:
If they’re coming out and saying I need help with this, that and the other, I don’t know where I am, I don’t know how to get my food, it can be quite irritating almost, having to keep repeating the same process to them. Quite often it results in them being . . . I wouldn’t say neglected but definitely left alone a lot of the time.
Mental health worker, prison E
Similar concerns were echoed in other prisons:
I don’t think [name] had let the wing know just how much he was struggling and it’s a very busy wing and if you don’t make your voice heard, you’re just locked, unlocked, and if you don’t ask for something you just get what you’re entitled to and that’s it.
Offender supervisor, prison B
We knew that he had dementia. But because he was compliant, because he was institutionalised, they let him get on with [it] where he was. It didn’t cause them a problem so therefore they let him be as he was.
Third-sector worker, prison D
In such circumstances, peer carers and the informal support networks provided by other residents seem indispensable.
A further defence against neglect and unmet needs was noted to be maintaining a stable group of staff on wings in which there were a significant number of vulnerable elderly prisoners, although this was not easy to achieve:
The problem is that on most of the wings there are not constantly the same officers. So [name of older person’s wing] tends to be the wing where almost anyone is put on there for a morning or an afternoon. So if you talk to the staff, well, I don’t know the people here, I’m just here for the morning, so the number of staff that are on there quite regularly tends to be quite small, so if they’re not around you’re kind of stumped a bit.
Third-sector worker, prison D
This respondent thought that the older person’s unit was an ‘easy target’ to poach staff from to serve other parts of the prison, as it was seen as a settled wing that could get along with less. Senior management in the prison accepted that, although consistent staffing was a goal, operational pressures often had an impact on the degree to which this was achieved:
There is an issue of continuity, but we have a core group of staff, so I guess that at any one time there’ll always be someone from the core group that works on [elderly persons’ wing] or that’s the way we would want it to be.
Governor grade, prison D
The provision of purposeful activity for this group of prisoners was variable across the sites we visited. In one prison, a third-sector organisation ran activities on most weekdays, offering a range of vocational and leisure opportunities. The goals of this service were expressed simply:
It’s a place where they’re not put down because they are not able to engage as everyone else does. We accept them as they are.
Third-sector worker, prison D
In other prisons, as noted in Theme 1: the challenge of an ageing prison population, staff felt ill-equipped and resourced to offer such activities due to insufficient staff time and lack of physical space within the prison. Local prisons experienced this most acutely. Discrete initiatives had been tried and some had fallen by the wayside, probably because they relied on the good will and enthusiasm of individuals, rather than being a formally recognised or commissioned service. The following quotation sums up what many respondents told us:
I think there is scope to potentially develop an area or a workshop or somewhere where people with mild impairments or dementia could potentially access, make it less stimulus for them, enable them to have one to one with people . . . I think it’s very difficult at the moment, staffing constraints, resources, in any organisation.
Social worker, prison C
Finally, one respondent wondered what the future held for these prisoners as they inevitably became older and frailer:
The thing is with these guys, they are now past that stage of feeling involved . . . hands up . . . had enough . . . they need to be in an area or place where they are actually, you know what they say, nursing homes for the infirm and what have you. They need to be in . . . they are going to have to start building prisons [for older prisoners] . . .
Peer carer, prison C
Poignantly, one elderly resident seemed to survive by simply ignoring the fact of being in prison:
I like to [be in] my own little world really. Thinking about things what I used to . . . when I was a young kiddie when we lived on the farm and that with my dad and it used to be great.
Resident, prison A
Theme 3: the importance of collaborative working relationships across professional boundaries
I would like to think that we mirror services within the prison estate that we do in the community . . . a joint approach.
Social worker, prison C
Throughout our interviews, staff from different professional groups described the challenges that caring for prisoners with dementia, and older prisoners more generally, presented on a daily basis. No professional group regarded their systems as wholly functional, and many commented on the difficulties of achieving joined-up care across organisational boundaries, both within and outside the prison walls.
Overall, resources from a range of agencies were noted as inadequate for the size of the task:
There’s just not enough support at all. So, in in the end, it will get to a point where it’s all going to be a massive challenge to help them. Because we don’t have that support, and the nurses are struggling as it is anyway, so they can’t come and support them.
Prison officer, prison C
The health-care provider changed here, and we thought, oh great, this could be good. But it’s not. And we have people come and they’re here for a matter of weeks or months and then they go again, and you’re back to square one.
Third-sector worker, prison D
Staff working with prisoners on residential units felt that they had a valuable role in noticing changes in a person’s presentation, but they often felt unsupported and undervalued by health-care staff when they raised concerns:
We’re with [them] all the time, from when the doors open ‘til the door shut; so, when we see something and we think that’s not quite right, we like to put it forward and we’ll make a request [for health care] to come and see them; it’s like there’s nothing wrong with them. But we’re with them all the time, so we can identify a little bit more than they can by just seeing them for 2 minutes.
Prison officer, prison A
It’s a case with health care, get off us, this is our business, it’s nothing to do with you, you don’t understand.
Third-sector worker, prison D
In such circumstances, the importance of nurturing individual relationships as a way to ‘get things done’ was emphasised:
We had a nurse here who was absolutely fantastic and she had a great relationship with us and we used to say to her we’ve got a problems, leave it with me, she would talk to the doctors, I’ll sort it, and she’d pass it through, and it was great. She went to another jail and since then we would never really be able to gain that kind of rapport.
Third-sector worker, prison D
The issue of ‘medical in confidence’ was raised, and the impact that a lack of information sharing had on wing staff’s ability to safeguard at-risk residents on the wing was noted:
If we all got together and all dealt with it together and had meetings on a regular basis; because they won’t tell us. Health care don’t tell us, so I can’t be aware that somebody’s got dementia or . . . to me it’s they’re saying it’s a confidentiality thing . . . but surely to God we should be there to help them and be aware . . . they don’t seem to want us to tell us which I find really difficult for us.
Prison officer, prison A
Non-health-care staff generally felt that they needed more information than they currently routinely received, but that this needed to centre around how to manage people’s care on the wing, rather than providing in-depth diagnostic details:
We need liaisons from our mental health teams, for them to actually say to staff, you know, you’ve got this prisoner, he’s got this problem, this is how you deal with it.
Safer custody officer, prison B
Health-care staff also wrestled with this issue, wondering if current practices were supporting discipline staff adequately:
When we identify people, are we giving the wing the right information?
Health-care manager, prison E
A health-care manager described the challenges of working in a prison setting:
[We are] constantly working in an environment which isn’t your own and largely a disciplined environment with men that have behaved quite badly and can behave quite badly, officers tend to automatically assume that if someone isn’t conforming or acting in a normal way that they would expect, that it is a disciplinary issue, until it becomes quite serious really.
Health-care manager, prison E
This was echoed by a member of the probation service:
Probation staff, unless they’ve worked in a prison . . . don’t know the workings of a prison and the fact that it can be a very uphill battle and that you’re working against a big machine that is the prison service.
Probation worker, prison D
Even though a range of health and custodial support services were operational in each prison, many respondents expressed concerns that services were not integrated, and vulnerable older people found themselves being passed from one service to another, hampering their ability to receive suitable care:
We’ve got so many different services in the prison and that’s quite unique in a way, so it’s its own community in itself [but] people segregate their thinking, so you deal with that, you deal with this.
Health-care manager, prison E
So every day we have that big handover at half one and all the different agencies from health care get together and it was [that] cases had been brought there and just kind of bounced between teams. No-one was really getting any kind of continued care. No-one was really sure how to manage them . . . it was like no-one would really take ownership for any of them.
Mental health worker, prison E
From an officer’s point of view, it was described as very difficult to navigate the system to identify ‘who does what’:
There’s a whole load of disconnects because . . . most prison officers don’t understand the difference between psychology, psychiatry and mental health teams.
Safer custody officer, prison B
Concern was also expressed that prisoners with suspected dementia or other cognitive issues did not receive services from the wider NHS and social services on an equivalent basis to those in the community. This was attributed to limited resources in community-based services that led to the prioritisation of people in the community, as those in prison were viewed as being in a safe place:
Appointments are made for CT [computerised tomography] scans and MRIs [magnetic resonance imaging scans] and things like that, so, yes, it’s accessible but time scales are probably not as quick as what they would be if you were accessing it from the community.
Social worker, prison C
Speaking about their experience of trying to arrange community support for a person due to be released from prison, a probation worker described their frustrations:
We became quite stuck because he wasn’t in the community . . . I had a really difficult time getting them to actually take the application seriously and actually allocate him a social worker, because obviously he’s not in the community. He’s not a priority for them.
Probation worker, prison D
We have failed everywhere in this. It isn’t just particularly at one particular department.
Probation worker, prison D
In what was hopefully an extreme set of circumstances, ineffectual team working created an unacceptable result for one person due to be released:
We recently had a man of 82 who’d been in 7 years released from here, no fixed abode, and he’d got early signs of dementia, and the way it was he was going to be shown to the gate here as every other prisoner is. He’d got no-one in the world, and he’d got to find his way to his probation office which was quite a distance from here.
Third-sector worker, prison D
One member of staff noted that local working cultures very much influenced the success or failure of interdisciplinary working:
We work well together as a team, we have a laugh with them and they laugh with us. You find that goes a long way on the unit as well because if were having a laugh and a joke it rubs off on everybody else and everybody else is upbeat and happy with it.
Prison officer, prison E
Theme 4: the challenge of training the workforce and peers
Before I actually started here, I’d had no experience of dementia at all, I’ve come in blind. During our training we had a very, very, very small, I think it was a 20-minute presentation on dementia.
Prison officer, prison A
We sought to establish what training staff and peer carers received to guide their work with older people with dementia, and what training they thought would be beneficial.
With regard to peer carers, a lot of uncertainty was expressed around training processes and content. No member of staff we spoke to could tell us what the training consisted of, how it was accessed or who was in charge of its delivery in their establishment. This is worrying, as the role of peer carer is one that can be immensely useful to vulnerable residents or, potentially, could open them up to exploitation or even abuse.
When asked directly whether or not he had received any formal training, a peer carer answered:
No. not actually training, but it’s a bit of common sense isn’t it . . . we’ve got information but basically some of that information’s out of date . . . and it said you’re not allowed to [push wheelchairs], but there’s no-one else here to do it . . . you just generally use your common sense, I think.
Peer carer, prison C
He noted that he had not gone through an official selection procedure:
[The role of carer] just sort of, landed on me . . . and I’ve never seen the carer people yet, and I’ve been in here 2 years.
Peer carer, prison C
He had, however, requested training in the role:
There’s no-one that specifically knows, or maybe there are, but I’ve never seen then in 2 years. I had a word with the mental health man one day, I’ll come over and see you [he said]; that was over a year ago. I just wanted a bit of information of what to look for and what not to look for.
Peer carer, prison C
In terms of how prisoners were selected to undertake a carer role, in one prison staff stated that a rigorous vetting procedure was in place, resulting in only ‘gold-standard’ prisoners being appointed. At another site, trusted prisoners in other, similar, roles were heavily relied on, which was noted as potentially problematic:
The prisoner carers tend to be the same people who are on the prisoner council, and they tend to be the same people who are listeners . . . so there’s a danger of overloading one small group of trustworthy prisoners.
Safer custody officer, prison B
However, in one establishment, a peer carer who acknowledged that he had not been formally trained had seemingly been allowed to directly task other prisoners with the role:
Maybe they saw something in me, and all of a sudden it was like . . . [name], you’re in charge of such and such. And I didn’t know what I was in charge of, and basically, I get the other lads who are willing to care for people . . . I seemed to be the one who’s the go-to person who gets it all sorted and makes sure it happens.
Peer carer, prison C
He did acknowledge the importance of monitoring who undertakes carer roles:
You’ve just got to be careful how you select, because some people think oh, that’s £2.50. They’ll do anything for £2.50 in this place, and you’ve got to be wary of the people you’re actually putting in charge of these people.
Peer carer, prison C
The potential impact of taking a hands-off approach to peer carer selection and training was highlighted in other prisons:
[Name] turned round and said I’m peeved off pushing these cripples around in the chair. If he’s a carer he shouldn’t be stating or coming out with facts like that, because that then will knock an older person for six.
Peer of elderly resident, prison A
Our carers have no training and, at the moment, very little in the way of risk assessment. And there are a couple of times when we’ve found vulnerable men, probably with people caring for them who shouldn’t have been.
Safer custody officer, prison B
Training for officers was thought to be vital by all respondents who commented on the matter. A prisoner with dementia thought that awareness training was key:
More officers trained for dementia, ‘cause a lot of them don’t understand. When you’ve got dementia a lot of people . . . and officers, they don’t seem to realise what you’re struggling with.
Resident, prison A
This view was echoed by a number of staff members:
I think once staff know what they’re dealing with, then they’ll deal with it sensibly and appropriately. If they don’t know what they’re dealing with, then it’s just challenging behaviour.
Safer custody officer, prison E
[Without training] for most staff on the wing . . . it’s just you know, that idiot doesn’t understand why I keep telling him to go in the cell, or to get out of the shower, or not to do this at this time of day . . . it’s always just, he always does this, nobody asks why he always does it.
Safer custody officer, prison B
None of the staff interviewed reported that they had received any formal or significant training in dementia and MCI. Some noted that they had learnt from having family members diagnosed with the conditions and others acknowledged having some access to learning materials through work channels:
We haven’t had training whatsoever, it’s only through my life outside of the job that I understand what some of these are going through.
Prison officer, prison E
There has been a leaflet gone round, that has been handed out to us for dementia, but apart from that there’s nothing been put in place yet . . . It’s not like a big leaflet, so it’s only like key points.
Prison officer, prison C
In one prison, the health-care manager was concerned that a lot of officers were very young and new in post and, as a result, were unlikely to bring experience of dealing with vulnerable people into their role. This concern was relevant to mental health issues in general, as well as to dementia and MCI specifically:
One of the recommendations that is going to come out of the recent . . . inspection is to raise awareness around mental health for officers . . . to empower them to have a conversation with [prisoners] themselves. At [name of prison] 47% of the discipline officers are currently in probation, so they’re all really brand new and quite inexperienced.
Health-care manager, prison E
A similar view was held in another prison:
The only thing is now we have an influx of new officers who [are] an average of 11 or 12 years old.
Third-sector worker, prison D
However, the respondent also acknowledged a lack of interest in receiving further education around dementia from some more experienced staff:
The problem is there’s a group of diehard prisons officers, if you got them together and said we’re going to talk to you about dementia, oh, we don’t need to know this, this is not us, we just do this and this and we lock them up and unlock them and feed them sort of thing.
Third-sector worker, prison D
The value of training was clear to most people and was often discussed in the context of officers being able to identify early signs of dementia and to pass those concerns on to health and social care services so that assessment and specialist intervention could take place:
I think if staff were able to identify them, sort of, an early intervention could take place at that point.
Social worker, prison C
There was consensus about what training for staff should cover:
I don’t think it needs to be long, I think it would just be the basics around their identified symptoms, triggers, what can be put in place in the meantime until professionals can be involved. And how to escalate that process if you have concerns.
Social worker, prison C
There was also a strong preference for training to be delivered face to face in a group situation to allow discussion and sharing of knowledge between participants. E-learning was widely thought to be an inferior mode of delivery that had less impact:
Face to face. I think it makes much more of an impact than kind of e-learning that you can just click your way through and not actually retain that much information from.
Mental health worker, prison E
In each prison in which we conducted interviews, at least one member of staff spoke about the issue of finding the time to train officers and other staff in all manner of subjects, not least dementia. Some training is mandatory and thus must be completed to meet centrally set key performance targets; this type of training is prioritised above all others:
A lot of the other training we have is mandatory, so that takes priority over any other training . . . my stuff, the suicide and self-harm stuff is just being made mandatory so I’m going to be able to deliver that but at the moment it’s not, so even I’m fighting with . . . other training which is mandatory . . . So to have a real impact, you’d want it to be mandatory, even it was just the awareness package.
Safer custody officer, prison B
I’m one of the trainers and in 2 years I’ve not delivered any training in mental health awareness.
Safer custody officer, prison B
Access to training was an issue for all types of staff. For example, one member of health-care staff had been developing an older person care pathway as part of an external professional development course, but it did had not got as far as implementation because funding for the course had been withdrawn by the prison and the staff member had felt unable to continue with the work unsupported:
I said well actually I’m not qualified to do this, I don’t want to put people at risk, having not got the necessary training in the area.
Mental health worker, prison E
Summing up, one experienced officer clearly made the point that training for prison officers, from their very first day on the job, is inadequate:
Prison officer training in general, is far too short, effectively eight weeks training to deal with the kind of mental health issues, the behavioural issues, the security . . . we try and ram people through a course in 8 weeks. The difficulty they have is if you improve the quality of your course, if you make it a 16- or 20-week course, then suddenly, you’re making a more skilled job, you’ve got to pay more. And the governments not going to pay more. So, if they’re not going to pay more, they’re not going to increase the training.
Safer custody officer, prison B
Summary
We conducted ethnographic observations of prisoners living with dementia and/or MCI, augmented by interviews with staff and other prisoners who were experienced in and opinionated about the issue of older prisoners with dementia and MCI. Four themes clearly emerged from the data. The sustained increase in older prisoners across the whole of the estate had led to many staff challenging their professional norms, simultaneously embracing and questioning the new landscape in equal measure. Although local initiatives to serve this population were common, support from Her Majesty’s Prison and Probation Service headquarters and government organisations is vital for such work to be sustained and regarded as part of mainstream provision. Individual champions are commendable, but may be transitory; services need to be embedded in commissioned services.
The increase in older prisoners is, in part, attributable to convictions late in life for historical sex offending. Many of the men convicted have never been in prison before and thus a seismic change in life occurs when they may be especially vulnerable because of physical ill health or advancing dementia. Society has a responsibility to ensure that these men ‘live well’ in prison and that the new circumstances in which they find themselves do not contribute to their health failing more than it would in the community. People are imprisoned as punishment, not for punishment. Prison environments and regimes need to facilitate prisoners’ well-being and engagement with their community.
In the majority of prisons, a significant number of different health, social and other organisations provide a wide range of services. Older prisoners, especially those with dementia, have complex needs, and there is a risk that services may continue to work in silos, with little joined-up working or interagency communication. In such circumstances, vulnerable people can disappear down the cracks of provision, whereby each agency thinks another is doing the job. Vulnerable prisoners are often powerless and disenfranchised in their dealings with such agencies. Agencies must work with open channels of communication and with clarity about where responsibilities lie across organisational boundaries. Joint meetings and complex case management procedures are essential, as is involving the prisoner and their family when appropriate. Community-based agencies should be regular visitors to the prisons and fulfil their role as full partners in all care processes.
Safe services are delivered by an informed, interested and supported staff. With regard to elderly prisoners, this includes the nurture of a group of peer carers adequately trained and supervised to carry out their tasks. All staff should be offered dementia awareness training as a minimum and should have access to professional development opportunities to support them in the development of high-quality, innovative services that are sustainable.
Chapter 5 Part 4
Part 4 of the study sought to identify the service needs of and develop an appropriate care pathway for older prisoners with MCI throughout their time in custody using a balance of care (BoC) approach. BoC is a long-standing, strategic planning tool that offers service planners and commissioners a transparent and systematic framework for exploring the costs and consequences of changing the mix of resources provided for a particular client group, and uses a sequential mixed-methods design grounded in the experience and knowledge of local experts. 80,82,83 In this study, there were five interlinked activities:
-
Data from part 1 (see Chapter 2) were used to categorise the sample into subgroups of people with similar needs for care (hereafter referred to as ‘case types’) on the basis of four characteristics deemed likely to be important in determining the nature and costs of their care.
-
A series of anonymous case studies (brief vignettes) was formulated to represent the most prevalent case types.
-
A range of staff from prison and community-based services attended workshops at which participants identified how each of the individuals in the vignettes should be most appropriately supported.
-
Feedback notes from workshops were collated and summarised using a care plan template. Key themes were identified that informed an initial draft of an assessment and treatment care pathway.
-
A validation workshop was held, which was attended by a range of senior staff from prison and community services. The initial care pathway was presented and discussed. Feedback notes from this workshop were collated and supported further development of the care pathway.
Further information about each step is given below. Drawing on data from part 1 (see Chapter 2), those 70 individuals who had screened positive on the MoCA and who completed the follow-up ACE-III and supporting sociodemographic information, completed social care assessments and given consent for their risk history and selected information from health-care notes to be collected were categorised into 16 relatively homogeneous subgroups (case types) on the basis of four variables deemed likely to be important in determining the locus and costs of their care (Table 27).
| Variable | Category | Definition |
|---|---|---|
| Dementia or MCI | Yes, dementia | ACE-III rating of ≤ 82 indicates dementia |
| Yes, MCI | ACE-III rating between 83 and 87 indicates MCI | |
| BADLS | Yes | Any selection of codes 01, 02, 03 on the BADLS indicates some level of ADL needs |
| No | A selection of 00 on the BADLS indicates no ADL needs | |
| Mental health | Good | Self-reported mental health reported as good |
| Bad | Self-reported mental health reported as bad | |
| Physical health | Good | Self-reported physical health reported as good |
| Bad | Self-reported physical health reported as bad |
In the absence of any previous BoC studies of people in prison that could inform the categorisation, a two-stage approach to this process was taken. First, a list of potential attributes was compiled from the measures used in part 1 of the study (see Chapter 2). Second, an iterative approach was taken to the prioritisation and operationalisation of these attributes to develop a typology that met a number of acceptability and validity criteria. Namely, the most commonly populated groups were required to be:
-
broadly homogeneous in a number of other attributes
-
clinically meaningful, such that practitioners could recognise ‘real people’.
As a result, each of the subgroups (case types) was large enough to be of interest to planners, but homogeneous enough to retain some meaning for fieldworkers.
Formulation of vignettes
A series of eight anonymous vignettes (see Report Supplementary Material 17 for an example) were formulated to represent the most prevalent case types in the full sample (Table 28). These were drafted by a researcher familiar with the data and co-applicant and collaborator David Challis and Sue Tucker, who had expertise in the BoC approach. These vignettes were based on exemplar cases from the data set.
| Vignette | Variable characteristic | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ACE-III score (mean) | Diagnosis | Sex (majority) | Age (≥ 50 years) (mean) | Type of offence (majority) | ADL needs | Depression present (GDS-15) | Mental health problems (PriSnQuest) | Mental health problems (self-reported) | Physical health problems (self-reported) | Learning difficulties present | Risk of reoffending | |
| 1 | 68 | Dementia | Male | 60 | Sex offences | No | No | No | No | No | No | High |
| 2 | 70 | Dementia | Female | 55 | Theft | No | Yes | No | No | No | No | Low |
| 3 | 71 | Dementia | Male | 67 | Sex offences | No | No | No | No | Yes | Yes | High |
| 4 | 62 | Dementia | Male | 64 | Sex offences | No | Yes | No | Yes | Yes | No | High |
| 5 | 76 | Dementia | Male | 70 | Sex offences | Yes | No | No | No | Yes | No | High |
| 6 | 60 | Dementia | Female | 61 | Sex offences | Yes | Yes | Yes | Yes | Yes | No | High |
| 7 | 86 | MCI | Male | 79 | Sex offences | No | No | No | No | No | No | High |
| 8 | 86 | MCI | Male | 70 | Sex offences | No | Yes | No | No | Yes | No | Medium |
The vignettes took the form of short case histories or pen pictures of clinically recognisable individuals and systematically incorporated information pertaining to the four key variables listed in Table 27, as well as age, sex, type of offence, presence of learning difficulties (if applicable) and other comorbidities, using a structured format. The final versions of the vignettes were proofread by the wider research team, included experts in social work, mental health nursing, forensic psychiatry, clinical psychology and experts by experience, to ensure their content validity.
A number of staff, carers and user representatives were invited to care planning workshops, at which the most appropriate ways of meeting the needs of the people depicted in the above vignettes were explored.
Recruitment
Three workshops were held in different regions of the country: Manchester, Newcastle and London. An invitation e-mail (see Report Supplementary Material 18) was circulated via the Offender Health Research Network (OHRN) and Prison and Offender Research in Social Care and Health Network. Individuals who were interested in participating were provided with further information (see Report Supplementary Material 19) and a participant information sheet (see Report Supplementary Material 20). Participants who attended on the day were asked to sign a consent form (see Report Supplementary Material 21). Forty-nine individuals with a range of experience in prison, probation, memory assessment and older adult community services, as well as carers of people with dementia, were recruited (16 individuals in Manchester, 11 individuals in Newcastle and 22 individuals in London). A full list of the roles of the workshop participants is given in Table 29.
| Role | Workshop | |||
|---|---|---|---|---|
| Manchester | Newcastle | London | Validationa | |
| MAS assistant psychologist | ✗ | |||
| Clinical psychologist | ✗ | ✗ | ✗ | |
| Community dementia lead | ✗ | |||
| Commissioner | ✗ | |||
| Custodial manager | ✗ | ✗ | ✗ | |
| Forensic psychiatrist | ✗ | |||
| Head of health care | ✗ | ✗ | ✗ | |
| Head of nursing | ✗ | |||
| Head of residence | ✗ | ✗ | ||
| Head of safer custody | ✗ | |||
| Mental health nurse | ✗ | ✗ | ||
| Nurse practitioner | ✗ | |||
| Occupational therapist | ✗ | ✗ | ||
| Old age psychiatrist | ✗ | ✗ | ||
| Older prisoner lead | ✗ | |||
| Probation officer | ✗ | |||
| Prison officer | ✗ | |||
| Senior nurse | ✗ | ✗ | ✗ | |
| Social care lead | ✗ | ✗ | ||
| Social worker | ✗ | ✗ | ✗ | |
| Student social worker | ✗ | |||
| Third sector | ✗ | ✗ | ✗ | |
Format
Workshop participants were divided into small multidisciplinary groups of between five and eight people, each of which was allocated a subset of preselected vignettes.
Facilitated by a researcher, participants were asked to read through the provided vignettes to familiarise themselves with the format. Opportunity was given for attendees to ask questions. Participants were encouraged to make notes on their copies, should they feel the need to do so. After participants had read the first vignette case study, the researcher asked for their initial thoughts on the following open-ended questions:
-
Based on current practice, what care would this person receive in the community?
-
Based on current practice, what care would this person receive in prison?
-
Ideally, what care should this person receive in prison and how could the environment and practice be adapted to facilitate this change?
Although the group discussion was organic, an interview guide (see Report Supplementary Material 22) was used to ensure that the conversation remained on topic, enabling the researcher to find a balance between collecting rich, yet conversational, first-hand accounts, and gathering the information required to develop the ‘ideal’ care pathway and service specification. 85 Owing to the conversational nature of the groups, the researcher was able to take an observational role and take notes.
The process described was repeated for all vignettes.
Data analysis and validation
For each vignette, a researcher collated the notes made and summarised these on a care plan template (see Report Supplementary Material 23). Each vignette was discussed three times, one in each workshop, and the notes from the three were combined. From this, a table of key themes was developed, characterising both the care pathway and the service needs for each vignette (Table 30). The series of care pathway workshops identified a need to ensure that a prisoner or patient with dementia or MCI has access to a wide range of support and stimulation post diagnosis. Literature has highlighted the complexities of the older prisoner population. Many older prisoners are retired, and providing meaningful activity is therefore important. 86 Workshop discussion among professionals with expertise across different disciplines supported the findings in the literature.
| Key themes of care | Vignette | |||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
| Assessment | ||||||||
| Reception assessment (induction needs to be more thorough) | ✗ | |||||||
| Initial memory assessment | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Full medical assessment | ✗ | ✗ | ✗ | ✗ | ||||
| To establish whether or not his/her behaviour or offence was associated with his/her diagnosis | ✗ | |||||||
| Diagnosis: by dementia nurses | ✗ | ✗ | ||||||
| Post-diagnosis triage (SALT, OT, MH, LD, care package from social worker), pain management, provision of pressure mattresses, orientation clocks, etc. | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Medication | ||||||||
| Technology-assisted support | ✗ | ✗ | ✗ | ✗ | ||||
| Dosette box | ✗ | ✗ | ✗ | |||||
| Environment | ||||||||
| Normal location | ✗ | |||||||
| Adapted specialist wing (for old age, mixed diagnosis) | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| Dementia-modified wing | ✗ | ✗ | ✗ | ✗ | ||||
| Forensic hospital | ✗ | |||||||
| Secure nursing home (clear criteria for this needed) | ✗ | |||||||
| Specialist units to go from custody through to a long-term care pathway | ✗ | |||||||
| ROTL (potential concern around person being missed due to age and non-diagnosis; if in the community they could forget their appointment, leading them to break terms of release) | ✗ | |||||||
| Daily activities | ||||||||
| Peer carers | ✗ | ✗ | ✗ | ✗ | ✗ | |||
| Named nurse and officer in place | ✗ | |||||||
| Buddy to monitor deterioration (if no current nursing needs) | ✗ | ✗ | ✗ | ✗ | ✗ | |||
| Support workers to support daily activities | ✗ | ✗ | ✗ | |||||
| Social | ||||||||
| Day care (e.g. CAMEO) | ✗ | ✗ | ✗ | ✗ | ||||
| Day care for dementia, rather than specific dementia wing | ✗ | ✗ | ||||||
| Support groups | ✗ | ✗ | ||||||
| Personalised care plan to highlight issues with social networks and isolation | ✗ | |||||||
| Information | ||||||||
| Combined register (listing comorbidities or other significant information) | ✗ | |||||||
| Personalised care plan so prison staff can also view | ✗ | ✗ | ✗ | ✗ | ||||
| Information needs to move with person (including how to communicate effectively with individual, medication times) | ✗ | ✗ | ||||||
| Dementia advisor based in prison | ✗ | ✗ | ||||||
| Staff awareness training to be included in induction | ✗ | ✗ | ✗ | ✗ | ✗ | |||
| Regular information sessions for prison staff (e.g. monthly on a Friday afternoon) | ✗ | ✗ | ✗ | ✗ | ||||
| Cognitive stimulation therapies, adapted SOTP | ✗ | |||||||
| Overnight social workers and occupational therapists on older persons’ wing available overnight | ✗ | |||||||
These data informed the development of an initial assessment and treatment care pathway, which was presented at a validation workshop attended by a range of key stakeholders from prison services, probation services, memory assessment services (MASs) and older adult community settings, as well as carers of people with dementia, who were asked to review the proposed approach. Feedback from this validation workshop was recorded and final edits to the care pathway were made.
These data were then used to cost care pathways for the health economic evaluation, and to develop a final care pathway for assessing people with suspected dementia or MCI and the identify the range of environmental and care delivery adaptations needed in the prison (Figure 2).
FIGURE 2.
Care pathway. CT, computerised tomography; MRI, magnetic resonance imaging; PSI, prison service instruction.
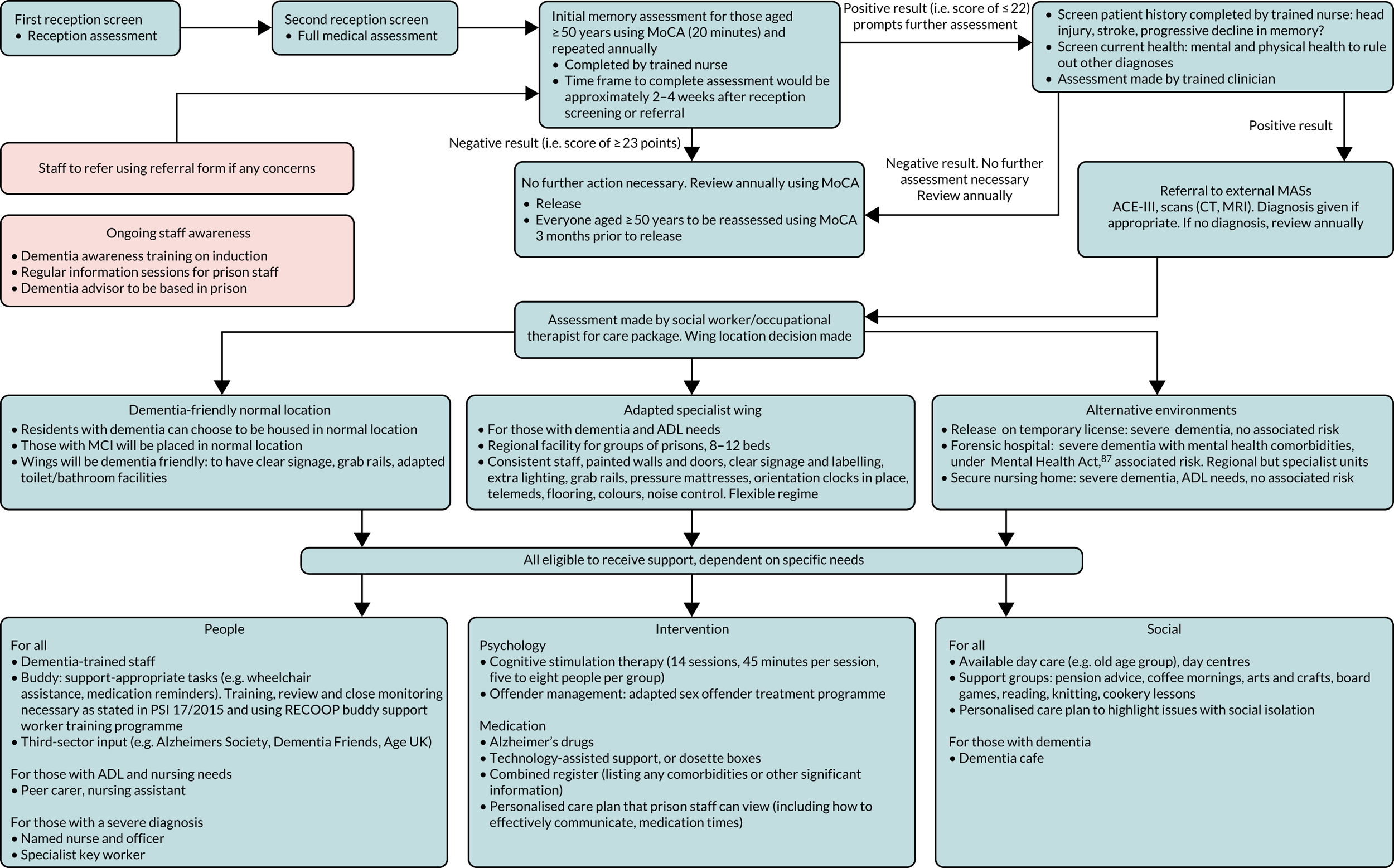
The data distilled from all the vignettes were used to develop an assessment care pathway (see Figure 2). The following is an explanation of this pathway.
Participants highlighted that an essential principle of the assessment care pathway was that it would be a pragmatic tool that fits into existing prison health-care processes. At 2–4 weeks post reception into prison (maybe a shorter period in local prisons), all those aged ≥ 50 years will be screened for an initial memory assessment using the MoCA,50 which will take approximately 20 minutes. This will be administered by a grade 5 dementia-trained nurse. If the individual receives a ‘MoCA-negative result’, that is a score of ≥ 23 points, then no further action will be necessary. These individuals will be reassessed using the MoCA annually and 3 months prior to release by a dementia-trained nurse. All those who received a ‘MoCA-positive result’, that is a score of ≤ 22 points, will be further assessed.
If any member of staff, a relative or carer, or even the prisoner themselves, becomes concerned that a prisoner may be developing dementia or MCI, they can be referred into the pathway at any point for an assessment with the MoCA by using the referral form (see Report Supplementary Material 24).
The next stage in the assessment entails a more detailed review of the patient’s history to establish possible risk factors for dementia and other potential causes of MCI. Screening via interview with the patient and examination of the case notes will include determining any previous head injuries or stroke and will also assess whether or not there has been a progressive decline in memory. A current mental and physical screen will also be completed to determine any other diagnoses. A full physical examination and gathering of relevant blood tests, scans or electroencephalograms, when appropriate, will be completed by a trained member of the nursing team in conjunction with the GP in the prison. These screenings should be completed within 2–4 weeks of the MoCA.
The results of the health screen will be reviewed by the nurse and GP, and, when dementia or MCI is still the most likely diagnosis, a referral to external MASs will be made. At this appointment, the ACE-III and full diagnostic assessment will be completed. For those with no diagnosis, no further action is required and the person will be reassessed using the MoCA annually or 3 months prior to release, as per the standard care pathway. If a diagnosis is made, medication will be considered. If medication is prescribed, it will initially be monitored by the memory assessment service (MAS). If there are no issues, then the individual will continue care and monitoring via the prison GP. Following diagnosis, a referral will also be made to a social worker or occupational therapist to assess the individual’s health and social care needs. The professional will have a range of options, including signposting to relevant third-sector and prison support and/or developing a specific, tailored individualised care plan. If necessary, an appropriate referral will be made to other services, for example occupational therapy, speech and language teams, mental health teams or learning disability services. In conjunction with prison staff, a decision will be made regarding the most suitable wing location for the individual. Care co-ordination and reviews of progress will be overseen by a dementia nurse.
Within the dementia care pathway, various accommodation options are available, dependent on an individual’s needs. Residents with a diagnosis of dementia or MCI can choose to be housed in dementia-friendly normal location if they are deemed well enough by the dementia-trained nurse, GP, prison staff and the social work or occupational therapy assessor. Those with severe dementia will be located in an adapted specialist wing.
Environmental modifications
All prisons should aim to be more dementia friendly. It was recognised that this will be relatively difficult in some establishments because of the age of the buildings and listed building status, but nevertheless some changes should be possible in all prisons. These should include:
-
having clear signage to help people find their way
-
labelling cupboards with pictures of the contents and using contrasting colours to make everyday items easier to identify
-
ensuring that handrails and door handles are easy to use, comfortable and contrasting in colour with the walls, and that they have clear safety features to indicate where they end
-
fitting call systems that are easy to identify in bedroom areas and water closet facilities
-
ensuring that the entrance to reception areas is bright and well-lit, with maximum use of natural light, and that corridors are bright and evenly lit.
A number of available resources provide information on how to make modifications to achieve dementia-friendly environments (see Report Supplementary Material 25).
For those with more severe dementia, with or without significant daily living skill deficits or comorbid mental and physical health problems, several suggestions for service development were made.
For people with severe dementia who are not manageable on the wing because of significant MCI and/or ADL deficits, an adapted specialist wing will be developed. This regional 8- to 12-bed facility will be available on a referral basis. The environment will be adapted to meet the needs of this group.
Care pathway discussion also explored alternative accommodation spaces, to be considered on a case-by-case basis.
Release on temporary licence
This would be appropriate for people with severe dementia considered to be at low risk of reoffending. They would have access to the full range of community services for dementia.
Forensic hospital
Referral made under the Mental Health Act87 for a forensic hospital bed would be appropriate for those with severe dementia, mental health commodities and associated medium to high risk of reoffending. Discussion centred around whether medium- and low-secure services should have one or two beds, or whether a regional service was more appropriate. On balance, workshop participants favoured the latter, with concentration of expertise and economies of scale. It was recognised that this regional approach was problematic when distance from home and access to family and friends was considered. Currently, this kind of regional specialist facility is not available.
Secure nursing home
Secure nursing homes were considered suitable for people with severe dementia, ADL needs or significant physical health needs who presented some ongoing risk of reoffending. It was concluded that these facilities needed to be regional services, with concentration of expertise and economies of scale. It was recognised that this regional approach was problematic when distance from home and access to family and friends was considered. Currently, this kind of regional specialist facility is not available.
People
An important aspect of the care pathway is that individuals are supported throughout. All individuals are eligible for support, although the level of support delivered is dependent on their specific needs. This is assessed by a social worker as part of an earlier needs assessment.
A dementia-trained nurse will be employed to lead the dementia care pathway. This person will receive training in managing dementia in prison (tier 2). They will manage the screening and referral process, and monitor patients. This centralised role will support both health care and the prison to care for and manage prisoners with dementia and MCI. Furthermore, to establish a dementia-friendly community, prison and health-care staff will be trained in dementia using the DeCIsion study training package (tier 1) and other relevant training depending on the staff member’s needs.
If individuals with dementia are located on the wing, consideration should be given to employing a peer carer. In part 3 of this study (see Chapter 4), staff indicated that the roles and responsibilities of peer carers need to be clearly defined and that peer carers should be trained using the peer training (see Appendix 5). Links to guidance regarding the role, training, review and close monitoring of peer carers can be found in Report Supplementary Material 26. Health-care support workers will support an individual with ADL needs as required, following the needs assessment.
For those in the advanced stages of dementia, a named nurse and officer will be allocated to each individual. This will maintain open communication among staff and achieve a multidisciplinary approach.
The proposed regional specialist units will be staffed by health and social care staff and prison staff, with input from peer carers as required.
Activities and interventions
Discussion about the pathway established that prisoners could benefit from older adult support groups. Therefore, all prisons could consider older adult day groups offering stimulating activities, such as book clubs, board games, cookery classes, and arts and crafts. These could be provided by Age UK, the Alzheimer’s Society and/or similar third-sector organisations, volunteers, peers or the older person’s prison lead. Support groups or sessions should be available to offer advice regarding pensions and legal advice. This could be provided through the third sector, such as RECOOP and Age UK. Services such as dementia cafes should be considered when appropriate to signpost dementia support in a sociable and stimulating environment.
Interventions may be available to those across the dementia pathway as required and proportional to need. Therapies such as cognitive stimulation therapy could be considered, when appropriate. Support with medication should also be available. To promote ongoing independence, technology-assisted pharmacy support or dosette boxes will be provided if suitable for the individual. For the purposes of information sharing, a multidisciplinary combined register should be designed. This will summarise any comorbidities and other significant information. This will be managed by the dementia nurse, with information shared between staff, subject to prisoners’ consent. In addition to this, a personalised care plan will be available, developed by the dementia nurse and available to all staff subject to prisoners’ consent.
Supplementary guidance information is also available for those using the dementia care pathway (see Report Supplementary Material 26).
Summary
Part 4 of the study sought to identify service needs and develop an appropriate care pathway for older prisoners with MCI throughout their time in custody using a BoC approach.
Data from part 1 (see Chapter 2) were used to categorise the sample into subgroups of people with similar needs for care. From this, a series of case types were formulated that were representative of the data set. Subsequently, the case types were presented and discussed at a series of workshops, which were attended by prison staff, community-based staff and carers of people with dementia. Using information collected at these workshops, an initial care pathway was developed. This initial care pathway was presented at a final validation workshop, which was attended by senior staff from prison and community services. Suggestions and feedback were recorded. The care pathway was updated to reflect discussion. Supplementary guidance was written as an additional resource for the care pathway.
The care pathway is yet to be implemented. Future research should seek to validate the dementia care pathway for use across prisons in England and Wales.
Chapter 6 Part 5
Method
In this study, a theory-based approach to the design and development of training was adopted. The perceived effectiveness of training framework (see Report Supplementary Material 27), developed by co-applicant Katherine Perryman for the design of optimal health-care professional training,88 draws on a number of theories pertinent to training and was the main theoretical framework used for informing the training packages in this study.
The training intervention component taxonomy, which is a list of the defined training methods with evidence of their effectiveness, was also used to inform the design of the training packages in the study. 88
A key objective of this part of the study was, first, to establish prison and health-care staff members’ training needs for identifying, assessing and appropriately supporting older prisoners with cognitive impairment and, second, to develop a training package for prison and health-care staff. A further peer carer training package was also developed. We conducted a training needs analysis, outlining who required training and what the content should be. We achieved this by exploring the literature on training for dementia in the community and prison, the current state of play regarding staff training, gaps in this training and training format preferences.
The following steps were undertaken to ensure that the training content and format was evidence based. We also drew on the training literature and theory to optimise potential effectiveness of the training.
Literature review and scoping exercise
A scoping review of the literature was conducted to see what existing research had been published on training for dementia in the prison setting and also the wider literature on dementia training in health settings. A Google Scholar (Google Inc., Mountain View, CA, USA) search of the following terms was conducted:
-
prison and staff and training and dementia or cognitive impairment
-
health professional or health-care staff and training and dementia or cognitive impairment.
This identified several papers and reports that could inform training content (see Chapter 1, Literature search, for summary of these papers). Hand-searches of the references of identified papers and searches of the grey literature were also undertaken to identify further research or reports on training interventions conducted in the prison setting. Finally, we sent an e-mail to the OHRN mailing list and a Tweet from the OHRN Twitter account (URL: www.twitter.com; Twitter, Inc., San Francisco, CA, USA) asking for people to contact us with details of any existing training for prison staff on supporting people with dementia or MCI.
Questionnaire data
Interim analysis of the questionnaire data (part 2; see Chapter 3) was conducted to inform the content and format of the training. Data were analysed from both the prison governor survey (n = 85) and the health-care manager survey (n = 37). The data included who should attend training on dementia and MCI, preferred mode of delivery, setting, length, group size and frequency of training, teaching methods and who should deliver training. Training content analysis included gaps in knowledge or areas in which staff lack confidence in relation to identification and management of MCI and dementia, and what topics should be covered in training.
Qualitative data
An interim analysis of 17 interviews conducted with prison staff (six health-care staff, two social workers, one prison officer, one probation officer, three governors or deputy governors, two prisoners and two peer carer volunteers) in part 3 also informed the training design (see Chapter 4). The interviews were coded for themes covered in the topic guide that were pertinent to training: attendees and recipients, barriers to training, content, format and previous training. The data for each theme were summarised, and this informed training design and content.
Training working group
To obtain patient and public involvement and stakeholder views to inform training design, people from a variety of backgrounds and professions were invited to participate in a training working group, which involved attending two face-to-face meetings to discuss the training with members of the project team (JS, KF, KP and JSr). Eight people accepted the invitation to the first meeting, which was held on 31 January 2019. This group consisted of a neuropsychologist, a patient carer, a lecturer in dementia, a prison social worker, three prison officers (including an older person lead) and a representative from Alzheimer’s Society (prison project). A presentation was delivered outlining the existing literature on content and format for dementia training in prison, the Dementia Training Standards Framework,43 and the interim analysis of the survey and qualitative data. The group was asked for their views on proposed content and format throughout the presentation, and agreement on key training content and format issues was reached. The feedback was incorporated into subsequent drafts of the training.
The people who attended the first meeting were invited to review the first completed draft of the dementia awareness training. At the second meeting, attended by the patient carer, social worker and two prison officers, a presentation of the proposed training was given and the group was asked for their comments on each slide. The feedback was incorporated into the final draft of the training.
Owing to the more specialist content and the size of the training (see Results), the tier 2 training was reviewed by the neuropsychologist in the working group and received specialist forensic psychiatric input from the principal investigator (JS). Katherine Perryman designed and compiled the training presentations, and all drafts of the training were reviewed internally by the project team (JS, KF, LH and JSr) to draw on their experience of conducting research and clinical work in prisons, so that the training could be further adapted to the prison setting.
The training working group was very receptive to the development of separate training for peer carers to help them to look out for signs of dementia among older prisoners and also to provide day-to-day care and support. Peer carer training was subsequently developed.
Results
Literature review and scoping exercise
We identified 29 potentially relevant papers to the prison setting and 12 papers from the wider health-care literature from our searches. The pertinent literature that could be used to inform training content and/or design is summarised in the literature search. We used the information in these papers and also existing training to inform training content.
The Dementia Training Standards Framework,43 and existing training from HEE based on this framework were the primary sources of content information. We obtained permission from HEE to adapt their training resources, which are aimed at health and social care staff. The dementia awareness training (tier 1) from HEE [URL: www.hee.nhs.uk/our-work/dementia-awareness/resources-tier-one-two-three (accessed 1 April 2020)] was used as a basis of the content of our dementia awareness training presentation, with adaptations made for the prison setting in terms of style, delivery, literacy and knowledge, and prison-relevant content. In addition, existing training on dementia awareness in prisons developed by the Alzheimer’s Society was reviewed, and some slides were adapted with the organisation’s permission.
In addition to the tier 1 training, to be delivered to all staff in the prison setting, we decided in conjunction with the training working group to develop a tier 2 training resource for prison and health-care staff who were likely to have more regular contact with people in prison with dementia. We used the resources on the HEE website to inform this training (Dementia Education and Learning Through Simulation 2) and also the e-learning developed by HEE [URL: www.e-lfh.org.uk/programmes/dementia/ (accessed 1 April 2020)]. These resources were adapted to the prison setting.
Questionnaire data
Recommendations for the training content and format were obtained from the interim analysis of the questionnaire data. To summarise, the following recommendations were presented to the training working group for discussion:
-
recipients – all staff
-
type of training – face to face, workshop training
-
setting – on site
-
length – one half-day session or shorter, modular sessions
-
training methods – interactive presentations, case studies, group discussion, small group tasks
-
facilitator – external clinician with prison experience, forensic psychiatrist or mental health nurse
-
group size – small to medium
-
content – increasing awareness by covering early warning signs, impact on functioning, communication, causes, local assessment (and referral) processes.
The training working group agreed with the recommendations, although they felt that the dementia awareness (tier 1) training did not need to be delivered by a clinician and could be delivered by a prison officer or member of health-care team, but ideally they would be involved in dementia in some way in either a specialist role or as a dementia champion within in the prison.
Qualitative data
A number of recommendations for the training design were obtained from interim analysis of the qualitative data. These were:
-
train all staff in dementia awareness, offering more detailed and in-depth training as needed
-
train peers to support other prisoners
-
have a well-trained dementia champion (health care and officer side)
-
training sessions to be no longer than 2 hours (modular training if any longer)
-
face-to-face, interactive workshop training
-
training methods to include case studies, discussion and role modelling
-
small group training (e.g. 10–12 people)
-
train-the-trainer approach is most practical
-
on-site (at the prison) training is best
-
it is more important for the facilitator to have dementia expertise than prison expertise
-
training should offer a certificate of competence to recipients.
These recommendations were presented to the training working group, who agreed that they should all be followed.
Training working group recommendations
In addition to the agreements reached on the basis of the findings from the literature review, questionnaire and qualitative data, the training working group provided a number of other recommendations for the training. A key recommendation was that prison representatives indicated that, on the whole, prison staff do not respond well to role-play techniques in training. Therefore, it was decided not to include this method in our training packages.
Furthermore, the training working group felt that we should not include any of the video case presentations available as part of the HEE training resources as proposed, as they were not relevant to the prison setting. Therefore, we filmed our own case presentations for the dementia awareness training using actors to portray prison officers and prisoners showing signs of dementia. We developed eight film clips demonstrating the signs and symptoms of dementia, the likely impact of prison on someone with dementia, and good and poor communication skills.
To summarise, the literature and scoping exercise, the interim analysis of the quantitative and qualitative data, and the feedback from the training working group indicated that a training package was needed and should consist of three separate training programmes.
Tier 1: dementia awareness in the prison setting (see Appendix 2)
Recipients
All prison staff, including officers, education staff, chaplaincy and health-care staff would receive this.
Facilitator
This would be facilitated by prison staff and a trainer who had been trained to deliver awareness training (experience of dementia preferred, but not necessary; however, they do need to have some understanding of the prison environment). Ideally, this would be a dementia lead or champion but could be a prison officer or health-care staff member.
Format
Interactive, face-to-face workshop training would be delivered onsite. The training would be delivered to all staff in small groups of up to 12, and from then on to new staff as part of induction. Training length would be 2 hours.
Aims and topics covered
-
The need for dementia awareness in prisons.
-
What is dementia? Different forms of dementia.
-
Early signs, symptoms and behaviour.
-
Supporting people with dementia, carers and staff.
-
Effective communication.
-
Peer carer support in prison.
-
What to do if you think a prisoner may have dementia.
-
Sources of support.
Tier 2: dementia care and support in the prison setting (see Appendices 3 and 4)
Recipients
Prison staff who will be supporting prisoners diagnosed with dementia would receive this [e.g. mental health team, nurses providing ongoing care, prison officers with responsibility for older prisoners or prisoners with dementia (dementia lead or champion; could be one per wing, depending on prison population) and social care staff responsible for providing care].
Facilitator
The facilitator needs to be an expert in dementia, but they do not need to have a prison background. A psychiatrist, psychologist, a social worker or a mental health nurse would be ideal.
Format
This would be an interactive face-to-face workshop training to be delivered on site in small groups. The whole training would be completed in two sessions of around 2 hours each.
Modules
-
Module 1: dementia identification, assessment and diagnosis.
-
Module 2: importance of early diagnosis.
-
Module 3: communication, interaction and behaviour in dementia care.
-
Module 4: health and well-being.
-
Module 5: equality, diversity and law in dementia care.
-
Module 6: end of life dementia care.
-
Module 7: screening and referral.
Peer carer dementia awareness and support (see Appendix 5)
Recipients
Nominated peer carers who will provide support to people with dementia would receive this.
Facilitator
This would be facilitated by a dementia champion or lead (prison officer or health care).
Format
The training would consist of a face-to-face, simple overview of dementia and information about how prisoners can be supported on a day-to-day basis, which would last no more than 2 hours.
A full description of the training components used in the tier 1 and 2 training packages, with definitions and associated theory, can be seen in Report Supplementary Material 28. This outlines pre-training preparation work that needs to take place before the training can be delivered (in conjunction with discussions on implementing the care pathway), training delivery components (content, training methods, characteristics of the facilitator, characteristics of the recipients, length and duration, characteristics of the setting) and post-training components (leadership).
Summary
Key objectives of this part of the study were to, first, establish prison and health-care staff members’ training needs for identifying, assessing and appropriately supporting older prisoners with cognitive impairment and, second, to develop a training package for prison and health-care staff.
Initially, a review of the literature was conducted to see what had been published on training for dementia in the prison setting to date, and the literature on dementia training in wider health-care settings was also reviewed. Subsequently, an interim analysis of questionnaire data (part 2; see Chapter 3) was conducted to inform training content and format, supported by an interim analysis of 17 interviews conducted with prison staff (part 3; see Chapter 4). Findings from these activities supported the development of a training working group, which worked with the research team to determine the content and format of delivery of training materials. This feedback was incorporated into subsequent drafts of the training; drafts were based on training developed by HEE. A second training working group was held; this involved a presentation of the proposed training, and the group was asked for comments on each slide.
The feedback was incorporated into the final draft of the training (tier 1). Owing to the specialist nature of tier 2 training, a neuropsychologist and forensic psychiatrist reviewed and added further detail. An additional peer carer training package was adapted from tier 1 training.
Future research should seek to pilot the training to validate the package. It is important that appropriate pre-training activities be conducted prior to training delivery. This includes meeting with prison management to ensure that there are adequate resources to implement training and organisational buy-in, and to plan implementation procedures and ensure that the working environment is amenable to change (see Report Supplementary Material 28 for descriptions of the training components). It is imperative that managerial support be obtained for successful implementation of the training and the care pathway. From the research conducted to inform the training development, we recommend that at least one dementia champion be identified in the prison to oversee the implementation of the care pathway and training, and to be involved in the delivery of the training as a facilitator. Large prisons with several wings containing older residents would benefit from more champions per wing.
Chapter 7 Part 6
Method
A costing exercise was undertaken to estimate the resources needed to deliver the staff training packages developed and the care pathways for MCI. The appropriate pathway will vary by individual need, and the costs of providing this care will vary substantially by prison site, depending on a number of factors, including the local labour market conditions and the size of the prison population with MCI. The resources required to deliver each element of the care pathways are therefore presented individually. Presenting the information in this disaggregated way aims to allow each prison site or commissioner to estimate their own projected costs, given their populations.
In addition, two typical care pathways for the detailed case vignettes have been costed. The costing exercise presented in this chapter was conducted from the public sector perspective, incorporating costs borne by the NHS, Personal and Social Services and the criminal justice system. This perspective is recommended by the National Institute for Health and Care Excellence for interventions that have health and non-health outcomes in the public sector and other settings. 89
Costs of the DeCIsion staff training packages
The costs of delivering the following three training packages were calculated separately: (1) dementia awareness for prison staff, (2) dementia care and support in the prison setting for prison staff and (3) dementia awareness and support for peer carers. When it was felt that the training could be appropriately run by different types of staff, for example prison officers, nurses and/or social care staff, cost estimates for all options are provided. The mix of training session attendees will vary in practice depending on the prison. We have therefore provided costs for an example of typical attendees representing a mix of staff involved in the care of older prisoners.
Resources required to deliver appropriate cognitive impairment care pathways
The resources required to deliver each element of the care pathway detailed in Figure 2 were estimated in consultation with a consultant clinical neuropsychologist. Only additional resources specific to the dementia care pathway were included. General prison accommodation, overhead costs and existing procedures, such as reception screening and provision of health care, were not costed, as these are already provided as part of usual care.
When possible, resource use was presented at the individual level. However, some elements of the pathway represent semifixed costs at a prison site level. For example, individuals administering MoCAs must undertake mandatory training. The cost of this would be apportioned across the number of individuals going through the pathway. As this will vary by site, we have presented these site-level costs separately.
It was possible to provide resource use and cost estimates only for the elements of the suggested care pathways that already exist in some form. Some of the suggested elements, such as secure nursing homes, are just ideas at this stage. Cost estimates for these elements were therefore unavailable.
Typical care pathways for detailed case vignettes
The detailed case vignettes designed in stage 4 were divided into three groups representing different levels of complexity and, therefore, different care needs. Individuals represented in vignettes 1–4 were judged to require standard dementia treatment. Individuals represented in vignettes 5 and 6 required standard dementia care plus additional care for ADL needs. In vignettes 7 and 8 represent the pathway is represented for individuals who are referred to MASs as a result of their initial MoCA but receive a diagnosis of MCI and not of dementia.
As the prevalence estimates produced in part 1 were available only for dementia and MCI separately, not dementia with ADL, typical care pathways for these two diagnosis groups were outlined and the resources required to deliver these care pathways calculated. The individual-level resources required to deliver the typical care pathway for individuals receiving a diagnosis of dementia and for those receiving a diagnosis of MCI are presented separately. In addition, these individual-level costs were combined with the prevalence estimates produced in part 1 (see Chapter 2), to estimate the national costs of provision.
Unit costs
Costs were calculated by multiplying the resource use data by the relevant unit cost figures. All costs were valued in Great British pounds according to the price year 2017/18. This price year was chosen as it was the most recent for which the Personal Social Services Research Unit (PSSRU) costs of health and social care were available. Any unit costs not available for this price year were inflated or deflated to 2017/18 using the Consumer Price Index. 90 This general inflation index was chosen, as costs falling on multiple sectors were inflated. Only resource utilisation falling under the public sector perspective was costed. Utilisation of services funded by charities was therefore not included in the cost calculations.
Unit cost data are not as readily available in the criminal justice field as in health care. Unit costs were therefore derived from a number of different sources, following the methodology used in the PSSRU’s Unit Costs in Criminal Justice (UCCJ) report, when possible. 91 After consulting with offender health commissioners, the authors concluded that, once the associated security costs were removed, the cost per hour of health services delivered in the prison system would be the same as those delivered in the community. This assumption was therefore applied when prison-specific unit costs were not available.
NHS health-care costs were estimated using the PSSRU’s Unit Costs of Health and Social Care 201892 and the national NHS 2017/18 Reference Costs. 93 To account for the fact that not all of NHS staff time is spent on direct patient contact, unit costs relating to the cost of face-to-face or direct patient contact were used, when available. Costs of the MoCA were taken from those listed on its website. Unit costs of prison staff were taken from the Prison Service Pay Review Body94 and prisoner pay was taken from Her Majesty’s Prison and Probation Service prison service order. 95 Unit costs for medication were derived from the British National Formulary. 96–99
Results
Costs of the DeCIsion staff training packages
Three training packages were developed in part 5 (see Chapter 6). The resources required to deliver these training packages are presented in Report Supplementary Material 29.
The dementia awareness training for prison staff (see Appendix 1) could be run by either a prison officer or a prison nurse, and each session lasts for 2 hours. The cost of facilitator time for a 2-hour session is estimated to be £32.48 if delivered by a prison officer and £72.00 if delivered by a prison-based nurse. This training session is aimed at all staff and the mix of attendees will vary by prison. We have provided costs for an example of typical attendees representing a mix of staff roles involved in the care of older prisoners. Based on 10 prison staff (eight prison officers, one health-care assistant and one prison-based nurse), the cost of attending staff time is estimated to be £356.14 for a 2-hour session. Dependent on their size, prisons may need to run these training sessions more than once. The cost of attendee time will vary in practice, depending on the number of attendees and their job roles.
The training session on dementia care and support in the prison setting (see Appendices 3 and 4) comprises two sessions, each lasting 2 hours, and is delivered by a prison mental health nurse. The cost of facilitator time is £72.00. This training session is again aimed at prison staff and the mix of attendees will vary by prison. We have provided costs of an example of typical attendees representing a mix of staff roles involved in the care of older prisoners. Based on the attendance of 10 prison staff (seven prison officers, one prison-based nurse, one mental health nurse and one health-care assistant), the cost of attending staff time is estimated to be £396.56 for a 2-hour session. Therefore, for the two sessions, the cost will be £144 for the facilitator and £793.32 for the participants. Dependent on their size, prisons may need to run these training sessions more than once. The cost of attendee time will vary in practice, depending on the number of attendees and their job roles.
The training session for peer carers on dementia awareness and support (see Appendix 5) could be run by either a prison officer or a prison nurse, and each session lasts for 2 hours. As with the dementia awareness training for prison staff, the cost of facilitator time for a 2-hour session is estimated to be £32.48 if delivered by a prison officer and £72.00 if delivered by a prison-based nurse. Peer carers receive a minimum rate of pay of £4.00 per week. Based on the attendance of four peer carers, and assuming that attending the training session represents half of their paid role for the week, it is estimated that the cost of peer carers attending time is £8.00 for a 2-hour session. The number of attendees per session will vary in practice, and prisons may need to run more than one session depending on their size.
Resources required to deliver appropriate cognitive impairment care pathways
The resources required to deliver each element of the care pathway illustrated are presented in Report Supplementary Material 30. These have been combined with the unit cost figures presented in Report Supplementary Material 31 to estimate the cost of this care provision.
For individuals to enter the care pathway, a member of the prison staff must first obtain training and certification to undertake MoCAs. This is an online process run by the MoCA Clinic & Institute and must be undertaken in addition to the DeCIsion staff training. The cost is £97.29 for the course fee. As the course takes 1 hour to complete, this also requires 1 hour of nurse time, which is estimated to cost £36.00. The key dementia-trained worker undertaking MoCAs will also require supervision. Although the amount of supervision will vary depending on the number of MoCAs undertaken, we have estimated the cost of 1 hour of supervision every month by a clinical psychologist as a guide. The staff time involved in attending and providing this supervision is estimated to cost £1092 per year, based on a clinical psychologist providing 1 hour of supervision every month to a band 5 nurse. The cost of the MoCA certification and supervision would be apportioned across the number of individuals going through the MCI care pathway. These costs are therefore presented separately as site-level costs in the top panel of the table in Report Supplementary Material 31 and 32.
The tables in Report Supplementary Material 33–35 present the resources required to deliver each element of the care pathway, which vary, dependent on the route each individual patient takes through the pathway. This includes the resources required for memory assessments conducted in the prison by the key dementia-trained worker and for referral to external dementia MASs. For an individual diagnosed with dementia after assessment at these external clinics, the additional resources required to provide adequate care for this individual in the prison are then listed. This includes the annual cost of medication prescriptions and a needs assessment from a social worker. Costs are also provided for equipment that can make the prison environment more dementia friendly, including dementia clocks, signage and wall charts. The costs of providing further support within the prison estate in the form of dementia cafes and cognitive stimulation therapy are estimated. Finally, for those receiving a diagnosis of severe dementia, the costs of some alternative environments are presented. This includes the costs of caring for individuals in forensic hospitals, as opposed to standard prison wings.
It was possible to provide resource use and cost estimates only for the elements of the suggested care pathways that already exist in some form. Specifically, we were unable to obtain cost estimates for providing adapted specialist wings and secure nursing homes. We did approach sites involved in the study regarding the cost of wing adaptations, but none had made any physical adaptations to their wings or had obtained quotes to do so. As adapted specialist dementia prison wings and secure nursing homes are merely ideas at this stage, informative cost information was unavailable. The costs presented are therefore the costs of providing memory assessments, additional health-care provision, staff support and small environmental adaptations, such as dementia clocks and signage. We also present the costs of transferring individuals with severe dementia to existing alternative accommodation options. The costs presented are those corresponding to the elements of the pathway currently available and, therefore, are those of elements that could be provided immediately within the current prison system.
Typical care pathways for detailed case vignettes
The dividing of the detailed case vignettes from part 3 (see Chapter 4) into three suggested groups is presented in Report Supplementary Material 36. Individuals represented in vignettes 1–4 were judged to require standard dementia treatment. The typical care pathway and corresponding resources required in year 1 for diagnosis and provision of standard dementia treatment for individuals represented in vignettes 1–4 is outlined in Report Supplementary Material 37. The cost of providing the individual-level elements of this care pathway is estimated to be £5159.55. When combined with the prevalence estimates from part 1 (see Chapter 2), it is estimated that providing this care pathway for the 858 individuals estimated to have dementia in the current prison population would come at a national cost of £4.4M.
Individuals represented in vignettes 7 and 8 were judged to have MCI rather than dementia. The typical care pathway and corresponding resources required for year 1 diagnosis and care provision of standard MCI treatment for individuals represented in vignettes 7 and 8 are outlined in Report Supplementary Material 38. The cost of providing the individual-level elements of this care pathway is estimated to be £4051.77. When combined with the prevalence estimates from part 1 (see Chapter 2), it is estimated that providing this care pathway for the 109 individuals estimated to have MCI in the current prison population would come at a national cost of £441,643.
It should be noted that the figures presented illustrate the resources required to provide the care pathway to individuals who receive a diagnosis. We have not included costs for those who are screened but then do not go on to receive a diagnosis. Costs have been presented for the typical care pathway of individuals who receive a diagnosis, to correspond to the prevalence estimates from part 1 (see Chapter 2). It should also be noted that the resources required, and corresponding costs, represent those applicable in only the first year, which are dominated by the costs involved with memory assessment clinics and diagnosis. They also represent only the individual-level costs of pathway provision. Additional site-level costs of DeCIsion training packages, MoCA certification and MoCA supervision would also apply. As our prevalence estimates are at a whole prison population, as opposed to prison site level, it was not possible to obtain accurate information on which to apportion these site-level costs. The figures presented in this section should therefore be interpreted with caution and subject to the above caveats.
Summary
We undertook a costing exercise to estimate the resources needed to deliver the staff training packages and the care pathways for MCI. Costing services is a relatively new area of prison-based health-care research.
Each of the three training packages would be delivered in separate 2-hour sessions, facilitated by either a prison officer or a prison nurse. Costs of delivery would vary substantially by prison site, depending on a number of factors, including local labour market conditions and the size of the prison population with MCI. For individuals who receive a diagnosis of dementia, a typical care pathway of assessments and standard dementia treatment is estimated to cost £5160 in year 1. For individuals who receive a diagnosis of MCI, a typical care pathway is estimated to cost £4052 in year 1.
It was possible to provide resource use and cost estimates only for the elements of the suggested care pathways that already exist in some form. Some of the suggested elements, such as secure nursing homes, are just ideas at this stage. Further research is required to investigate the cost of more ambitious options, such as the development of secure nursing homes.
Chapter 8 Conclusions and further research
Summary of findings
This mixed-methods study comprised four parts.
In part 1 the current prevalence of dementia and MCI among those in prisons in England and Wales was estimated (see Chapter 2). The adjusted prevalence of dementia and MCI was 8%, which would equate to 1090 people with dementia or MCI in prisons in England and Wales. These figures were considerably higher than the numbers estimated by staff in the survey (part 2 of the study; see Chapter 3), suggesting that dementia is significantly under-recognised in prisons. Some of this variance may be explained by variance in how dementia was measured (e.g. clinical diagnosis, screening tools). However, these differences may be accounted for by higher rates of alcohol misuse (and associated Korsakoff psychosis) in prisoners. It is also possible that the higher prevalence in the prison population of brain injury and vascular disease (associated with vascular dementia) could contribute to the differences found.
In part 2 a questionnaire survey (see Chapter 3) was sent to prison governors and health-care managers. We had an excellent response rate for both questionnaires. Staff told us that routine screening for MCI was conducted in around one-third of prisons at reception, but fewer prisons screened prisoners on a regular basis post reception. Few prisons used standardised measures to assess cognitive function. Prisons reported variability in modifications made to their environments to accommodate those with dementia. Around half had made no changes and others had made minor adaptations, including providing of handrails, having bigger, more accessible cells and improving signage. Many of these changes had been made to accommodate social care needs more broadly, and staff recognised that changing the environment of old Victorian-era prison buildings to make them more ‘dementia friendly’ was challenging.
The majority of prisons did not have a defined dementia care pathway. Few provided older prisoner-specific support groups or activities. Over half utilised the input of peer carers, but their training and role specifications varied significantly, with a minority engaged in inappropriate activities (e.g. assisting with dressing and washing). Around one-fifth of prisons offered training on dementia to prison and health-care staff, but many staff indicated that they would welcome training or better training. Those factors, in combination, led to the conclusion that prisons were probably missing a significant proportion of people with dementia and MCI and did not provide a dementia-friendly environment, did not adequately train their staff and did not have a robust assessment and treatment care pathway.
Part 3 (see Chapter 4) comprised qualitative interviews with a range of respondents, and researcher’s observation of individuals with suspected dementia, their peers and staff. Themes emerged around how prisons, staff and environments urgently needed to evolve and adapt to meet the challenge of the increasing older population; what it is like to be an older person in prison on a day-to-day basis and how both age and cognitive impairment impinge on living well in prison; the challenge of providing joined up care across a number of partner agencies; and the pressing need to develop a skilled and confident workforce. It was evident that staff are currently facing ongoing challenges in providing joined-up care across all the partner agencies involved, with boundaries between organisations hampering seamless care in prison itself and on release into the community. A pressing need to develop a skilled and confident workforce through the provision of high-quality training, delivered to mixed professional groups was identified.
In part the BoC approach82–84 was used to design a care pathway for people with dementia and MCI across the prison estate (see Chapter 5). We held workshops with prison staff and health and social care professionals working in the community and prisons, together with carers of people living with dementia in the community. The participants used vignettes developed from the data in part 1 (see Chapter 2) to consider the needs of people with dementia and MCI. The participants generated an assessment care pathway and guidance on service development for people with dementia and MCI. The latter included recommendations for changes to all prisons to make them ‘dementia friendly’, including adaptations to signage, with the provision of tailored groups and activities and input of peer carers and other staff, when appropriate. Our workshop participants recognised that many people with MCI and dementia could be cared for on the wing with individual care packages delivered proportional to need, as occurs in the community. For those with more severe dementia, including those with significant ADL needs or complex comorbidities, the recommendations included the creation of purpose-built or adapted regional units to house 8–12 people, staffed by trained prison and health and social care staff, and provide a therapeutic regime (i.e. the provision of dementia-specific psychological therapies). Workshop participants also recognised the need for those with dementia and comorbid mental illness who were high risk of harm to others to be transferred, under the Mental Health Act,87 to secure forensic hospitals. Discussions ensued in the workshops about the relative merits of developing regional, bespoke, secure forensic mental health units, specialising in dementia care, compared with the regional provision of one or two beds for this group. On balance, the former was favoured, although it was noted that this concentration of expertise and services in only a few places around the country would prove problematic for, for example, family visits.
Participants also indicated that there needed to be much more considered use of release on temporary licence or compassionate leave for people with significant dementia who are considered low risk. These people could then access the full range of care available in the community. Participants also considered that there may be a need to development secure nursing homes for those who have severe dementia but still require security. Again, it was considered that these should be regional developments to allow for economies of scale and staff expertise.
We developed three training packages: (1) dementia awareness training for all staff, (2) dementia care training for specified prison, health-care and social care staff who would provide assessment and treatment and (3) peer carer training. These packages were evidence based and developed from a review of the literature, from responses to the questionnaire data and from multiple workshops comprising prison, health-care and social care staff, and carers of people living with dementia in the community. The development of training for peers ensured that it addressed one of the most important themes generated in part 3, that of ensuring clarity around what the peer carer role should and should not involve (see Chapter 4). The training was subsequently costed. Finally, the assessment care pathway, the environmental adaptations and the service developments were also costed.
Strengths and limitations of the study
To our knowledge, this is the first study in UK prisons to estimate the prevalence of MCI and dementia, the service needs of this group, the training needs of staff caring for these prisoners, and the cost of the proposed care pathways and service developments.
We established a representative sample of the prison population of both sexes and had sufficient power to estimate the prevalence of MCI and dementia. These estimates are, however, based on the ACE-III and not on a clinical diagnosis by a mental health professional. Therefore, our prevalence figures may represent an overestimation. Furthermore, we were unable to distinguish subcategories of dementia.
We were also unable to distinguish between a likely diagnosis of dementia and other conditions presenting with MCI, including learning disability, severe depression or hearing impairment. We know, however, the proportion of people screening positively on the ACE-III who had these conditions. However, we do not know whether they had both (e.g. dementia and a learning disability) or just one (e.g. learning disability but no dementia). Overall, it is likely that this led to an overestimation of the prevalence of dementia and MCI in our sample.
Overall, we estimated that 1090 people across the prison estate in England and Wales have dementia or MCI. We aimed to estimate the likely change in numbers of people with dementia over the next 5 years. We know that there has been a significant rise in the population of people aged ≥ 50 years in recent years, largely due to an increase in sentencing for historical, mainly sexual, offences. Unfortunately, we were unable to estimate with any certainty whether or not this rise is likely to continue. This is largely because we were unable to ascertain if this sentencing practice is likely to proceed at the same rate or if sentencing for these historical offences has now plateaued.
The Ministry of Justice has attempted to project how the older prisoner population is likely to change from 2019 to 2023. The ≥ 50 years population is projected to decrease from 13,609 as at June 2019, to 12,500 in June 2023. Likewise, the ≥ 60 years population is projected to decrease from 5077 to 4900 over the same period. The ≥ 70 years population is projected to remain largely constant, at 1800, over the period. Historically, the number of incarcerated adults aged ≥ 50 years had been increasing steadily before plateauing in 2018, mainly as a result of an augmentation in the proportion of sexual offence cases being received. Older adults are more likely to be convicted of sexual offences than their younger counterparts. The subsequent reduction in the number of sexual offences being heard in court has led the Ministry of Justice to predict that there will be a reduction in the number of older offenders being incarcerated in the future; however, this remains uncertain. The declining numbers of people imprisoned for public protection and ‘lifer’ populations, which include a higher proportion of offenders aged ≥ 50 years, have also led to the prediction that the older age group in prison will decrease. 71 Other evidence suggests that the opposite is true and that older prisoner numbers will continue to increase. 75 However, in our view, caution is needed with these predictions as a wide range of factors could have an impact on the number of older adults being incarcerated in the future (e.g. high-profile media cases that may result in more victims coming forward). The potential reduction in the number of older prisoners in the immediate future should not prevent us from improving outcomes for the 16% of the prison population who are currently aged ≥ 50 years and suffering from inadequate health and social care provision that is not equivalent to that for their peers residing in the community.
We used a number of measures to characterise people who screened positive on the ACE-III. A number of these measures have limitations. Most had not been used previously in prisoner populations and it is likely that the cut-off scores need to be adjusted for this population. The OASys was used to estimate the person’s risk of reoffending. Risk data are important when service provision is considered and it is questionable whether or not this kind of risk data is adequate when release or placement in a secure nursing home is being considered for a prisoner. It is possible that a more appropriate risk assessment tool would need to be found, adapted or developed for prisoners with dementia.
Part 1 also aimed to validate the 6-CIT so that it could be used to screen for dementia in prisons (see Chapter 2). The advantages of the 6-CIT are that it is brief and easy to administer. We compared it with the MoCA and concluded that it was not suitable for screening in prison. However, we did not have sufficient resources in the study to compare the performance of the 6-CIT with that of the ‘gold standard’, the ACE-III. Nevertheless, the inferior performance of the 6-CIT compared with the MoCA led us to conclude that the MoCA would be the more appropriate screening tool. The other advantage of using the MoCA is that it is widely used in community services, thus contributing to equivalence of care between prison and community, and increasing the utility of information transferred between the two settings. 50
We had a good response rate for the questionnaires in part 2 (see Chapter 3). However, despite proactive attempts to maximise returns, ultimately, questionnaires were returned over nearly a 2-year period (from August 2017 to June 2019). We acknowledge that service changes, developments and improvements were likely to have taken place during that period and thus the data do not provide a ‘snapshot’ of services across the prison estate at any particular time. Additionally, the limitations of this part of the study is that of all surveys, namely that the data are self-reported. Nevertheless, this part of the study provided valuable data to inform the development of the training packages.
Part 3 achieved data saturation on a range of topic areas relating to the management of dementia and MCI in prison (see Chapter 4). We interviewed staff and prisoners, including those with dementia and peers caring for them. This resulted in a very rounded view of the issues, giving a voice to a frequently disenfranchised group. The periods of ethnographic observation were perhaps too short to provide a nuanced understanding of living with dementia in prison.
Part 4 used the BoC approach (see Chapter 5). This is an approach to service development in which a transparent and systematic framework is used to explore the costs and consequences of changing the mix of resources provided for a particular client group, and employs a sequential mixed-methods design that is grounded in the experience and knowledge of front-line practitioners. It is a useful method for translating prevalence estimates into service needs and also for providing the framework for costing of new proposed care pathways. The method relied on getting appropriate front-line staff to consider the vignettes or case types emerging from the part 1 data (see Chapter 2). In our workshops we included staff and carers with a wide range of expertise from the community and prison, as we wanted to establish ‘what works’ for care provision in the community and translate this into ‘what works’ in prisons. To gather a range of views on care pathways and service developments, we held three workshops around the country and largely achieved saturation of themes. The ideas generated in these workshops were then confirmed in a final workshop. It is possible that the range of ideas proposed was not exhaustive and that, in further workshops, more ideas on service development may have appeared. The findings from part 4 informed the health economics study.
Costing studies are rarely performed in the prison setting in the UK, and so comparatively little is known about the cost of care provision in this setting. There is great variability in individual care pathway needs and also in prison sites in terms of the size of the older prison population. For this reason, we have concentrated on presenting the information on the resources required to deliver the MCI care pathways in a largely disaggregated form. This will allow each prison or commissioner to estimate their own projected costs, given their populations and current levels of provision, and highlights the areas of variability and uncertainty in these costs.
It was possible to provide resource use and cost estimates for only those elements of the suggested care pathways that already exist in some form. Some of the suggested elements, such as secure nursing homes, are just ideas at this stage, and so cost estimates were unavailable. The costs presented therefore represent those corresponding to the elements of the pathway that are currently available and so could be provided immediately within the current prison system. Further research is required to investigate the cost of more ambitious options, such as the development of secure nursing homes.
We had intended to conduct a budget impact analysis combining a matrix of current and future prevalence estimate scenarios produced in part 4 (see Chapter 5) with the cost estimates produced in this chapter. However, as the scope of the prevalence estimates exercise was reduced (see Chapter 2), this in turn only allowed for a more simplistic cost projection exercise.
The final part of this study involved the development of training for staff and peer carers. This was done using the evidence from the literature, data from part 2 of this study (see Chapter 3) and input from staff and carers. The proposed Microsoft PowerPoint® (Microsoft Corporation, Redmond, WA, USA) training presentations are attached (see Appendices 2–5); however, the training will need further work to develop training manuals and so on.
Discussion
To the best of our knowledge, this is the first study to establish the prevalence of dementia and MCI among male and female prisoners in the UK, and to estimate their service needs. Our finding on prevalence was not dissimilar to those in previous studies. 25 The survey data mirrored findings from inspectorate reports and the recent inspectorate review of social care in prisons,21,100 which indicated that prisons do not currently have the care pathways, training or services necessary to cater for this group of prisoners. Our qualitative study revealed findings similar to those from the study by Sindano. 41 In particular, staff expressed concerns about role differentiation (i.e. who should do what), including for peer carers. These ideas were included and considered when we designed training for staff and peer carers. To the best of our knowledge, this was the first study to design a fully costed dementia care pathway and to outline the likely service requirements for this group. Similarly, it is one of the first studies to develop evidence-based training for staff and peer carers.
To achieve equivalence of service provision in prison, establishments should work towards making all prisons more ‘dementia friendly’. Simple measures could be put in place immediately and with little cost, including better signage, a notice board with the day’s date, a clock and handrails. With heightened staff awareness about how dementia may present in a prisoner, staff could detect more potential cases and, providing that a robust care pathway is in place, readily seek assessment. Around the prison estate in England and Wales there are examples of good practice, with some prisons developing social activities and groups for people with MCI and even psychological therapies for people with dementia. However, this patchy and normally relies on particular people acting as ‘product champions’ to drive changes through. There is some evidence on the impact of environmental changes on well-being in people with dementia,37,38 but, to the best of our knowledge, no other studies in a prison environment have been conducted.
The number of older people in prison has risen dramatically in the last decade,9 and the number of people in prison aged ≥ 50 years is projected to increase by 3% by 2022. The most significant change is anticipated in those aged ≥ 70 years (projected to rise by 19% by 2022). 73 Prisons therefore need to address the issues related to an ageing population generally and to an increased prevalence of dementia specifically.
The introduction of a dementia and MCI care pathway with robust screening, assessment and the provision of services based on need with individualised care planning would, in our view, improve the quality and appropriateness of care for older prisoners. To implement this care pathway, staff will need to be trained, including peer carers. Roles and responsibilities of all staff and peer carers will need to be defined and there will be a requirement for a net increase in staff to cover the assessment and treatments required. Local community mental health services will be required to facilitate MAS input into prisons. The costs of this are outlined in Chapter 7.
The benefits of providing this assessment pathway and ensuing treatments is that it will provide an equivalent service to the community and improve the health and well-being of the prisoners with dementia. The impact of the introduction of the assessment and treatment care pathway should be evaluated, measuring multiple health and well-being outcomes.
Similarly, the introduction of a range of ‘dementia-friendly’ environmental changes and the impact of these changes should be similarly evaluated so that evidence of ‘what works best’ for prisoners with dementia can be established. Our research also identified the benefits of partnership arrangements with voluntary sector organisations to increase the range of activities and services in prison for people with dementia.
Our findings suggested that a range of provision would be required for those with dementia of varying severity. Purpose-built or adapted units to provide care in prison for those with more severe dementia were recommended. Further research is needed on the environmental needs, the staffing structure, and the nature and philosophy of the therapeutic environment of such a unit. Other suggestions included increasing the use of release on temporary licence or compassionate release, so that low-risk prisoners could benefit from the range of dementia services in the community. Models of compassionate release should be developed between health-care and prison staff and evaluated. Other suggestions included the development of secure nursing homes in the community and the development of older adult forensic mental health services. The latter has been mooted previously100 owing to the rising number of older people in secure hospitals. Further research is required about who would benefit from these developments and what their physical structure, staffing requirements and philosophy of care should look like.
Finally, we received permission to follow up our sample of people who screened positive on the ACE-III. With further funding, we aim to conduct a longitudinal study to establish a range of outcomes for this cohort.
Future research
This study’s outputs include a dementia assessment and treatment care pathway, including training for all staff and peer carers. In terms of next steps, we need to consider how the care pathway should be delivered in prison and how it may need to be adapted for different types of prisons, including local prisons with high turnover of prisoners, women’s prisons, and open and resettlement prisons, with a greater focus on discharge pathways.
It is important to establish whether or not the introduction of the assessment care pathway leads to larger numbers of people with dementia and MCI being identified, assessed and supported, resulting in fewer unmet health and social care needs.
The three training packages should be evaluated to assess whether they lead to improvements in staff and peer carers’ knowledge and attitudes and, ultimately, to improvements in health and social care outcomes for prisoners with MCI and dementia.
The proposed environmental changes, including the development of dementia-friendly prisons, should be evaluated by assessing the outcomes in terms of improved well-being and orientation. Further exploratory work is required to assess the need for regional prison specialist units, secure nursing homes and older people’s services in forensic hospitals, including environmental design, service development, philosophy of care and staffing structure. Similarly, further modelling is required on the number of beds required and their geographical location. Such research should include full health economic analyses of the likely benefits.
Little is known about the longitudinal trajectory of people with MCI and dementia in the criminal justice system. We have received consent from participants in the current study for follow-up. In the first instance, we will apply for further funding to establish the health, social care and criminological outcomes of our sample of ACE-III-positive individuals over the next 3–5 years.
Finally, a repeat of our survey at intervals will chart the development of service provision across the whole prison estate over time.
Practice recommendations
Service development
-
All prisons should develop a plan for the modification of wings to be more dementia friendly. The degree of adoption of environmental changes will depend on the physical structure and adaptability of the prison, including whether or not it has listed status.
-
All prisons should consider how the regime can potentially have an impact on people with dementia and MCI and make necessary adaptations. These would include, but are not limited to, adjustments to activities (including their timing), meal provision, medication management and adjudications.
-
Dementia assessment and treatment care pathways should be commissioned and developed in all prisons.
-
All prisons should develop links with local MASs, and the input of MASs into prisons should be commissioned and provided proportional to the need of the population served.
-
The need for regional prison specialist units, secure nursing homes and older people services in forensic hospitals should be examined nationally.
-
These specialist units should be designed to meet the needs of people with severe dementia, with consideration given to environmental design, service development, philosophy of care and staffing structure. These services should be commissioned and developed.
Workforce
-
Prisons should establish the staffing needs for the dementia and MCI care pathway in their establishment.
-
Roles and responsibilities of all staff involved in the care pathway should be established.
-
Roles and responsibilities and recruitment process for peer carers should be developed.
-
Improved models for interagency working with information sharing should be developed.
Staff training
-
All staff should receive dementia and MCI awareness training, and this should be repeated at regular intervals.
-
All staff involved in the delivery of the dementia and MCI care pathway should receive tier 2 training, and this should be repeated at regular intervals.
-
Staff training should be delivered to interagency, multidisciplinary groups to encourage a better shared understanding and ownership of the issue.
-
All peer carers should receive peer carer dementia and MCI training, and this should be repeated at regular intervals.
Research recommendations
-
A study examining the implementation of the assessment care pathway in prison and its adaptation for different types of prisons, with examination of process outcomes, including numbers of people with dementia and MCI identified, assessed and supported, and the impact on the pathway in meeting health and social care needs and improving quality of life.
-
Evaluation of changes in staff and peer carers’ knowledge and attitudes about dementia and MCI, and prisoners’ health and social care needs and quality of life, following the introduction of the three training packages on dementia and MCI.
-
Evaluation of the effect of introducing ‘dementia-friendly’ environmental changes on prisoners’ social care needs, well-being and orientation, for prisoners with MCI and dementia.
-
An exploratory study with health economics modelling of the service need, geographical location, environmental design, service development, philosophy of care and staffing structure of regional prison specialist units, secure nursing homes and older people services in forensic hospitals.
-
A cohort study to establish the health, social care and criminological outcomes of a sample of ACE-III-positive individuals over a period of 3–5 years.
Patient and public involvement
Dr Stuart Ware is a co-applicant, an older ex-prisoner and a founder member of the group Restore Support Network (a registered charity for older prisoners). Dr Ware’s involvement ensured that we considered the needs of older prisoners throughout the study. The peer research group in the Restore Support Network also assisted in the development of the proposal and advised on the study throughout. The group comprised four ex-prisoners who had been trained in research methods by Dr Ware. The group welcomed the research, indicating that it would help to fill a gap in knowledge and help shape service development. They had experience of supporting other prisoners with dementia and highlighted the impact of having MCI in prison (e.g. behaviour such as forgetting to turn up for appointments being mistaken for disobedience). The group commented on drafts of this report and it has been adapted accordingly. In particular, the group co-wrote the Plain English summary. The group have also provided useful additions to the design, such as ensuring that the care pathways developed considered services on release from prison and linked into other relevant care pathways.
Dr Ware sat on the Study Steering Committee, was involved in the management of this research study and provided his expertise responsively throughout the life of the project. This ensured that the perspectives of older prisoners were considered throughout. Four experts by experience (including carers and individuals with MCI) attended and meaningfully participated in the workshops to develop the training and care pathway. The peer research group in the Restore Support Network assisted in the development of participant information sheets and will assist in the development of newsletter-style reports to be distributed to prisoners to inform them about the findings of the research. The peer research group will also participate in presentations to disseminate the research to commissioners, prison staff and health-care staff. Dr Ware completed his Doctor of Philosophy degree on the needs of older prisoners and has experience of supporting and training ex-service users.
In addition, a post-diagnostic dementia support group at Greater Manchester Mental Health NHS Foundation Trust assisted in the development of information sheets, consent forms, etc. This helped to ensure that these documents were formatted appropriately for individuals with MCI and dementia.
Acknowledgements
Independent Steering Committee members who advised as per their area of expertise: Peer Bathi, Sue Gauge, Julian Hughes, Nigel Hunt, Rachel Hunter, Margaret Hurley, Kathryn Norris, Joanne Rance, Louise Ridley, Claire Surr and Vicky Tuck.
Florian Walter (Research Associate) assisted with questionnaire follow-up.
Levi Calvo-Dobbs (Research Assistant) assisted with questionnaire follow-up.
Contributions of authors
Katrina Forsyth (https://orcid.org/0000-0001-9980-9464) (Research Associate) was the project manager, assisted in the design of the study, supervised research assistants, conducted qualitative and quantitative data collection, advised as per her expertise and drafted sections of the report.
Leanne Heathcote (https://orcid.org/0000-0002-2279-9621) (Research Assistant) conducted quantitative and qualitative data collection, assisted in the development of the training and drafted sections of the report.
Jane Senior (https://orcid.org/0000-0002-7133-4898) (Senior Lecturer) assisted in the design of the study, managed the project budget, undertook qualitative analyses, drafted sections of report, commented on draft versions and supervised researchers.
Baber Malik (https://orcid.org/0000-0002-7153-7003) (Research Assistant) conducted quantitative data collection and statistical analysis.
Rachel Meacock (https://orcid.org/0000-0001-8933-5058) (Research Fellow, Health Economics) conducted the health economics analyses and contributed to the report.
Katherine Perryman (https://orcid.org/0000-0003-1275-6991) (Research Fellow) developed and advised on training packages, and drafted sections of the report.
Sue Tucker (https://orcid.org/0000-0001-7986-0844) (Research Fellow) drafted sections of the report and advised as per her expertise.
Rachel Domone (https://orcid.org/0000-0001-5083-7966) (Consultant Clinical Neuropsychologist) trained researches in the use of the tools, conducted checks on the use of the cognitive assessments, attended steering groups, assisted in the development of the training, commented on draft reports and advised as per her expertise.
Matthew Carr (https://orcid.org/0000-0001-7336-1606) (Research Fellow) conducted statistical analysis and advised as per his expertise.
Helen Hayes (https://orcid.org/0000-0002-6081-5266) (Research Assistant) conducted the health economics section and drafted sections of the report.
Roger Webb (https://orcid.org/0000-0001-8532-2647) (Professor in Mental Health Epidemiology) advised as per his expertise and commented on draft sections of the report.
Laura Archer-Power (https://orcid.org/0000-0002-4283-9264) (Research Assistant) assisted in the design of the study, quantitative data collection and drafting sections of the report.
Alice Dawson (https://orcid.org/0000-0001-8821-9346) (Research Assistant) conducted quantitative data collection and analysis, and drafted a section of the report.
Sarah Leonard (https://orcid.org/0000-0002-1729-0556) (Research Associate) drafted sections of the training and report.
David Challis (https://orcid.org/0000-0002-6464-2286) (Professor, Community Care Research) attended steering groups and advised as per his expertise.
Stuart Ware (https://orcid.org/0000-0002-1466-1120) (Chief Executive, Restore charity) attended steering groups and advised as per expertise.
Richard Emsley (https://orcid.org/0000-0002-1218-675X) (Professor, Medical Statistics) advised on statistical issues.
Caroline Sanders (https://orcid.org/0000-0002-0539-928X) (Professor, Primary Care Research) attended steering groups and advised as per his expertise.
Salman Karim (https://orcid.org/0000-0002-4643-0677) (Psychiatrist, Adult Mental Health) attended steering groups and advised as per his expertise.
Seena Fazel (https://orcid.org/0000-0002-5383-5365) (Professor, Forensic Psychiatry) attended steering groups and advised as per his expertise.
Adrian Hayes (https://orcid.org/0000-0002-3153-6348) (Academic Clinical Fellow, Psychiatry) attended steering groups and advised as per his expertise.
Alistair Burns (https://orcid.org/0000-0002-9837-0645) (Professor, Old Age Psychiatry) attended steering groups and advised as per his expertise.
Mary Piper (Honorary Research Fellow) attended steering groups and advised as per her expertise.
Jenny Shaw (https://orcid.org/0000-0003-2569-7687) (Professor, Forensic Psychiatry) was responsible for the delivery of the project, supervision of researchers, providing comments on draft versions and writing report sections.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Prince M, Knapp M, Guerchet M, McCrone P, Prina M, Comas-Herrera, et al. Dementia UK: Update. London: Alzheimer’s Society; 2014.
- Burns A. Major Strides in Tackling Dementia. London: NHS England; 2014.
- Heward M, Innes A, Cutler C, Hambidge S. Dementia-friendly communities: challenges and strategies for achieving stakeholder involvement. Health Soc Care Community 2017;25:858-67. https://doi.org/10.1111/hsc.12371.
- O’Shea E, Monaghan C. An economic analysis of a community-based model for dementia care in Ireland: a balance of care approach. Int Psychogeriatr 2017;29:1175-84. https://doi.org/10.1017/S1041610217000400.
- Monkhouse C. Beyond the medical model – the Eden Alternative in practice: a Swiss experience. J Soc Work Long Term Care 2003;2:339-53. https://doi.org/10.1300/J181v02n03_11.
- National Institute for Health and Care Excellence (NICE) . NICE Pathways: Dementia 2018. https://pathways.nice.org.uk/pathways/dementia#path=view%3A/pathways/dementia/dementia-overview.xml&content=view-index (accessed 3 January 2020).
- Robinson L. How to recognise the early signs of dementia. Pract Nurs 2009;20:S7-S10. https://doi.org/10.12968/pnur.2009.20.Sup1.42562.
- Moll A. Losing Track of Time: Dementia and the Ageing Prison Population – Treatment Challenges and Examples of Good Practice. London: Mental Health Foundation; 2013.
- GOV.UK . Offender Management Statistics Quarterly: October to December 2018 n.d. www.gov.uk/government/statistics/offender-management-statistics-quarterly-october-to-december-2018 (accessed 3 January 2020).
- West HC, Sabol WJ, Greenman SJ. Prisoners in 2009. Washington, DC: US Department of Justice; 2010.
- Grant A. Elderly Inmates: Issues for Australia. Canberra, ACT: Australian Institute of Criminology; 1999.
- Yamaguchi M. Japanese Prisons Face Swelling Elderly Population 2011. www.washingtontimes.com/news/2011/jan/6/japanese-prisons-face-swelling-elderly-population/ (accessed 1 June 2015).
- Uzoaba JHE. Managing Older Offenders: Where Do We Stand?. Ottawa, ON: Correctional Service Canada; 1998.
- Prison Reform Trust . Bromley Briefings Prison Factfile Autumn 2018 2019. www.prisonreformtrust.org.uk/Portals/0/Documents/Bromley%20Briefings/Autumn%202018%20Factfile.pdf (accessed 3 January 2020).
- Howse K. Growing Old in Prison: A Scoping Study on Older Prisoners. Centre for Policy on Ageing and Prison Reform Trust; 2011.
- National Institute of Corrections . A Resource Pack for Working With Older-Prisoners 2009. https://nicic.gov/resource-pack-working-older-prisoners (accessed 1 April 2020).
- Ginn S. The challenge of providing prison healthcare. BMJ 2012;345:26-8. https://doi.org/10.1136/bmj.e5921.
- Atkinson L. Old and inside, older people in prison. Work Older People 2008;12:34-7. https://doi.org/10.1108/13663666200800050.
- Kingston P, Le Mesurier N, Yorston G, Wardle SHL. Psychiatric morbidity in older-prisoners: unrecognised and undertreated. Int Psychogeriatr 2011;23:1354-60. https://doi.org/10.1017/S1041610211000378.
- Williams J. Social care and older-prisoners. J Soc Work 2012;13:471-91. https://doi.org/10.1177/1468017311434886.
- Her Majesty’s Inspectorate of Prisons (HMIP) . ‘No Problems – Old and Quiet’: Older Prisoners in England and Wales 2004.
- Crawley E, Sparks R. Hidden injuries? Researching the experiences of older men in English prisons. Howard J Crim Justice 2005;44:345-56. https://doi.org/10.1111/j.1468-2311.2005.00380.x.
- Fazel S, Hope T, O’Donnell I, Jacoby R. Hidden psychiatric morbidity in elderly prisoners. Br J Psychiatry 2001;179:535-9. https://doi.org/10.1192/bjp.179.6.535.
- Fazel S, Hope T, O’Donnell I, Piper M, Jacoby R. Health of elderly male prisoners: worse than the general population, worse than younger prisoners. Age Ageing 2001;30:403-7. https://doi.org/10.1093/ageing/30.5.403.
- Hayes AJ, Burns A, Turnbull P, Shaw JJ. The health and social needs of older male prisoners. Int J Geriatr Psychiatry 2012;27:1155-62. https://doi.org/10.1002/gps.3761.
- Wahidin A. Older Women in the Criminal Justice System: Running Out of Time. London: Jessica Kingsley Publishers; 2004.
- Ware S. The development of care services for older people in prison. J Care Serv Manag 2009;3:364-74. https://doi.org/10.1179/csm.2009.3.4.364.
- Bowden P. The future organisation of prison health care. J Forens Psychiatry 1999;11:473-6. https://doi.org/10.1080/09585180050142697.
- Till A, Forrester A, Exworthy T. The development of equivalence as a mechanism to improve prison healthcare. J R Soc Med 2014;107:179-82. https://doi.org/10.1177/0141076814523949.
- Department of Health and Social Care (DHSC) . National Service Framework for Older People 2001.
- Earthrowl M. Providing treatment to prisoners with mental disorders: development of a policy. B J Psychiatry 2003;182:299-302. https://doi.org/10.1192/bjp.182.4.299.
- Hayes A, Elger BS, Ritter C, Stover H. Emerging Issues in Prison Health. New York, NY: Springer; 2016.
- Sumner A. Assessment and management of older prisoners. Nurs Older People 2012;24:16-21. https://doi.org/10.7748/nop2012.04.24.3.16.c9016.
- Folstein MF, Folstein SE, McHugh PR. ‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189-98. https://doi.org/10.1016/0022-3956(75)90026-6.
- Dawes J. Aging prisoners: issues for social work. Aust Soc Work 2009;62:258-71. https://doi.org/10.1080/03124070902803475.
- Stojkovic S. Elderly prisoners: a growing and forgotten group within correctional systems vulnerable to elder abuse. J Elder Abuse Negl 2007;19:97-117. https://doi.org/10.1300/J084v19n03_06.
- Social Care Institute for Excellence . Dementia Friendly Environments – Lighting 2015. www.scie.org.uk/dementia/supporting-people-with-dementia/dementia-friendly-environments/lighting.asp (accessed 20 July 2018).
- Baidawi S, Trotter C, Flynn C. Prison experiences and psychological distress among older inmates. J Gerontol Soc Work 2016;59:252-70. https://doi.org/10.1080/01634372.2016.1197353.
- Durcan G, Saunders S, Gadsby B, Hazard A. The Bradley Report Five Years On: An Independent Review of Progress to Date and Priorities for Further Development 2014. www.mentalhealthchallenge.org.uk/library-files/MHC151-Bradley_report_five_years_on.pdf (accessed 3 January 2020).
- Caulfield LS, Twort H. Implementing change: staff experiences of changes to prison mental healthcare in England and Wales. Int J Prison Health 2012;8:7-15. https://doi.org/10.1108/17449201211268246.
- Sindano N. The Prison Project: Raising Awareness of Dementia in Prisons. 2016. www.alzheimers.org.uk/blog/prison-project-raising-awareness-dementia-prisons (accessed 3 January 2020).
- Alzheimer’s Society . Reducing and Managing Behaviour That Challenges. 2019. www.alzheimers.org.uk/about-dementia/symptoms-and-diagnosis/symptoms/managing-behaviour-changes#content-start (accessed 3 January 2020).
- Health Education England and Skills for Care . Dementia Training Standards Framework 2018.
- Surr CA, Gates C, Irving D, Oyebode J, Smith SJ, Parveen S, et al. Effective dementia education and training for the health and social care workforce: a systematic review of the literature. Rev Educ Res 2017;87:966-1002. https://doi.org/10.3102/0034654317723305.
- Cipriani G, Danti S, Carlesi C, Di Fiorino M. Old and dangerous: prison and dementia. J Forensic Leg Med 2017;51:40-4. https://doi.org/10.1016/j.jflm.2017.07.004.
- Patterson H. Forget me not. Midwives 2012;15.
- Great Britain . Mental Capacity Act 2005 2005.
- Dewing J. Participatory research: a method for process consent with persons who have dementia. Dementia 2007;6:11-25. https://doi.org/10.1177/1471301207075625.
- Jorm AF, Jolley D. The incidence of dementia: a meta-analysis. Neurology 1998;51:728-33. https://doi.org/10.1212/wnl.51.3.728.
- Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 2005;53:695-9. https://doi.org/10.1111/j.1532-5415.2005.53221.x.
- Roalf DR, Moberg PJ, Xie SX, Wolk DA, Moelter ST, Arnold SE. Comparative accuracies of two common screening instruments for classification of Alzheimer’s disease, mild cognitive impairment, and healthy aging. Alzheimers Dement 2013;9:529-37. https://doi.org/10.1016/j.jalz.2012.10.001.
- Freitas S, Simões MR, Alves L, Santana I. Montreal Cognitive Assessment (MoCA): normative study for the Portuguese population. J Clin Exp Neuropsychol 2011;33:989-96. https://doi.org/10.1080/13803395.2011.589374.
- Waldron-Perrine B, Axelrod BN. Determining an appropriate cutting score for indication of impairment on the Montreal Cognitive Assessment. Int J Geriatr Psychiatry 2012;27:1189-94. https://doi.org/10.1002/gps.3768.
- Larner AJ. Screening utility of the Montreal Cognitive Assessment (MoCA): in place of – or as well as – the MMSE?. Int Psychogeriatr 2012;24:391-6. https://doi.org/10.1017/S1041610211001839.
- Luis CA, Keegan AP, Mullan M. Cross validation of the Montreal Cognitive Assessment in community dwelling older adults residing in the Southeastern US. Int J Geriatr Psychiatry 2009;24:197-201. https://doi.org/10.1002/gps.2101.
- Lee JY, Dong Woo L, Cho SJ, Na D L, Hong Jin J, Kim SK, et al. Brief screening for mild cognitive impairment in elderly outpatient clinic: validation of the Korean version of the Montreal Cognitive Assessment. J Geriatr Psychiatry Neurol 2008;21:104-10. https://doi.org/10.1177/0891988708316855.
- Brooke P, Bullock R. Validation of a 6 item cognitive impairment test with a view to primary care usage. Int J Geriatr Psychiatry 1999;14:936-40. https://doi.org/10.1002/(SICI)1099-1166(199911)14:11%3C936::AID-GPS39%3E3.0.CO;2-1.
- Hsieh S, Schubert S, Hoon C, Mioshi E, Hodges JR. Validation of the Addenbrooke’s Cognitive Examination III in frontotemporal dementia and Alzheimer’s disease. Dement Geriatr Cogn Disord 2013;36:242-50. https://doi.org/10.1159/000351671.
- Noone P. Addenbrooke’s Cognitive Examination-III. Occup Med 2015;65:418-20. https://doi.org/10.1093/occmed/kqv041.
- Bucks RS, Ashworth DL, Wilcock GK, Siegfried K. Assessment of activities of daily living in dementia: development of the Bristol Activities of Daily Living Scale. Age Ageing 1996;25:113-20. https://doi.org/10.1093/ageing/25.2.113.
- Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS). Recent evidence and development of a shorter version. Clin Gerontol 1986;5:165-73. https://doi.org/10.1300/J018v05n01_09.
- Shaw J, Tomenson BM, Creed FH. A screening questionnaire for the detection of serious mental illness in the criminal justice system. J Forens Psychiatry Psychol 2003;14:138-50. https://doi.org/10.1080/1478994031000077943.
- King NS, Crawford S, Wenden FJ, Moss NE, Wade DT. The Rivermead Post Concussion Symptoms Questionnaire: a measure of symptoms commonly experienced after head injury and its reliability. J Neurol 1995;242:587-92. https://doi.org/10.1007/bf00868811.
- Lubben J. Assessing social networks among elderly populations. Fam Community Health 1988;11:42-5. https://doi.org/10.1097/00003727-198811000-00008.
- Matthews FE, Arthur A, Barnes LE, Bond J, Jagger C, Robinson L, et al. Medical Research Council Cognitive Function and Ageing Collaboration. A two-decade comparison of prevalence of dementia in individuals aged 65 years and older from three geographical areas of England: results of the Cognitive Function and Ageing Study I and II. Lancet 2013;382:1405-12. https://doi.org/10.1016/S0140-6736(13)61570-6.
- Cohen JA. Coefficient of agreement for nominal scales. Educ Psychol Meas 1960;20:37-46. https://doi.org/10.1177/001316446002000104.
- Fleiss JL. Measuring agreement between two judges on the presence or absence of a trait. Biometrics 1975;31:651-9. https://doi.org/10.2307/2529549.
- Kraemer HC. Measurement of reliability for categorical data in medical research. Stat Methods Med Res 1992;1:183-99. https://doi.org/10.1177/096228029200100204.
- Cohen J. Weighted kappa: nominal scale agreement with provision for scaled disagreement or partial credit. Psychol Bull 1968;70:213-20. https://doi.org/10.1037/h0026256.
- Dunn G. Design and analysis of reliability studies. Stat Methods Med Res 1992;1:123-57. https://doi.org/10.1177/096228029200100202.
- Ministry of Justice . Prison Population Projections 2018 to 2023, England and Wales 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/735428/prison-population-projections-2018-2023.PDF (accessed 3 January 2020).
- Sturge G. UK Prison Population Statistics (Briefing Paper Number CBP-04334). London: House of Commons Library; 2018.
- Prison Reform Trust . Bromley Briefings Prison Factfile: Autumn 2018 2018.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Great Britain . Social Care Act 2014 2014.
- Gustafsson M, Kristensson J, Holst G, Willman A, Bohman D. Case managers for older persons with multi-morbidity and their everyday work – a focused ethnography. BMC Health Serv Res 2013;13. https://doi.org/10.1186/1472-6963-13-496.
- Hubbard G, Downs MG, Tester S. Including older people with dementia in research: challenges and strategies. Aging Ment Health 2003;7:351-62. https://doi.org/10.1080/1360786031000150685.
- Holthe T, Thorsen K, Josephsson S. Occupational patterns of people with dementia in residential care: an ethnographic study. Scand J Occup Ther 2007;14:96-107. https://doi.org/10.1080/11038120600963796.
- Sarangi S, Roberts C. Talk, Work and Institutional Order. New York, NY: Mouton de Gruyter; 1999.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-117.
- Ministry of Justice . Population Bulletin: March 2019 n.d. www.gov.uk/government/statistics/prison-population-figures-2019 (accessed 15 May 2020).
- Mooney GH. Planning for balance of care of the elderly. Scott J Polit Econ 1978;25:149-64. https://doi.org/10.1111/j.1467-9485.1978.tb00242.x.
- Tucker S, Brand C, Wilberforce M, Abendstern M, Challis D. Identifying alternatives to old age psychiatry inpatient admission: an application of the balance of care approach to health and social care planning. BMC Health Serv Res 2015;15. https://doi.org/10.1186/s12913-015-0913-1.
- Tucker S, Hughes J, Jolley D, Buck D, Hargreaves C, Challis D. Reconfiguring in-patient services for adults with mental health problems: changing the balance of care. BJPsch Open 2018;4:420-6. https://doi.org/10.1192/bjo.2018.60.
- Morgan D. Focus groups . Ann Rev Sociol 1996;22:129-52. https://doi.org/10.1146/annurev.soc.22.1.129.
- Resettlement and Care of Older ex-Offenders and Prisoners (RECOOP) . Good Practice Guide: Working With Older Prisoners n.d. www.recoop.org.uk/dbfiles/pages/54/FINAL-Older-Prisoners-Good-Practice-Guide-2017.pdf (accessed 11 May 2020).
- Great Britain . Mental Health Act 1983 1983.
- Perryman K. Synthesising Existing and Developing New Evidence on Effective Healthcare Professional Training That Aims to Improve the Management of Psychological Distress in Primary Care 2014.
- National Institute for Health and Care Excellence (NICE) . Developing NICE Guidelines: The Manual 2014. www.nice.org.uk/media/default/about/what-we-do/our-programmes/developing-nice-guidelines-the-manual.pdf (accessed 3 January 2020).
- Office for National Statistics . Consumer Price Inflation Time Series 2019. www.ons.gov.uk/economy/inflationandpriceindices/datasets/consumerpriceindices (accessed 3 January 2020).
- Brookes N, Barrett B, Netten A, Knapp E. Unit Costs in Criminal Justice (UCCJ). Canterbury: PSSRU, University of Kent; 2013.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2018. Canterbury: PSSRU, University of Kent; 2018.
- NHS Improvement . 2017/18/Reference/Costs 2018. https://improvement.nhs.uk/resources/reference-costs/ (accessed 3 January 2020).
- Prison Service Pay Review Body . Seventeenth Report on England and Wales 2018 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/728364/CCS207_CCS0618944474-00_Prison_Service_Accessible_Web.pdf (accessed 3 January 2020).
- Her Majesty’s Prison and Probation Service . Annual Report and Accounts 2017–18 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/720863/HMPPS_ARA_2017-18__web_.pdf (accessed 3 January 2020).
- National Institute for Health and Care Excellence . Donepezil Hydrochloride 2019. https://bnf.nice.org.uk/drug/donepezil-hydrochloride.html#medicinalForms (accessed 3 January 2020).
- National Institute for Health and Care Excellence . Galantamine 2019. https://bnf.nice.org.uk/drug/galantamine.html (accessed 3 January 2020).
- National Institute for Health and Care Excellence . Memantine Hydrochloride 2019. https://bnf.nice.org.uk/drug/memantine-hydrochloride.html (accessed 3 January 2020).
- National Institute for Health and Care Excellence . Rivastigmine 2019. https://bnf.nice.org.uk/drug/rivastigmine.html#indicationsAndDoses (accessed 3 January 2020).
- Fazel S, Jacoby R, Oppenheimer C, Dening T. Oxford Textbook of Old Age Psychiatry. Oxford: Oxford University Press; 2007.
Appendix 1 Links to videos for training slides
Behaviour that interrupts the regime
1a: bad response
URL: https://youtu.be/uQjtfOxhkaQ (accessed 2 April 2020).
1b: good response
URL: https://youtu.be/lGFKU7KiSNM (accessed 2 April 2020).
Forgetting why they are in prison
2a: bad response
URL: https://youtu.be/rYwPg42mCMI (accessed 2 April 2020).
2b: good response
URL: https://youtu.be/Alv-Egco-BQ (accessed 2 April 2020).
Forgetting how to eat
2c: bad response
URL: https://youtu.be/wkNTOqvlb4s (accessed 2 April 2020).
2d: good response
URL: https://youtu.be/r93U1QRPTyM (accessed 2 April 2020).
Appendix 2 Tier 1 training slides
Appendix 3 Tier 2 training: session 1 slides
Appendix 4 Tier 2 training: session 2 slides
Appendix 5 Peer training slides
Glossary
- Dementia
- Describes a set of symptoms that may include memory loss and difficulties with thinking, problem-solving or language. These changes are often small to start with, but they have become severe enough to affect daily life. A person with dementia may also experience changes in their mood or behaviour.
- Mild cognitive impairment
- A condition in which someone has minor problems with cognition (i.e. their mental abilities, such as memory or thinking) that are worse than would normally be expected for a healthy person of their age. However, the symptoms are not severe enough to interfere significantly with daily life and so are not defined as dementia.
List of abbreviations
- 6-CIT
- six-item cognitive impairment test
- ACE-III
- Addenbrooke’s Cognitive Examination – Third Revision
- ADL
- activities of daily living
- BADLS
- Bristol Activities of Daily Living Survey
- BoC
- balance of care
- CI
- confidence interval
- GDS-15
- Geriatric Depression Scale-15
- GP
- general practitioner
- HEE
- Health Education England
- ID
- identification
- MAS
- memory assessment service
- MCA
- Mental Capacity Act
- MCI
- mild cognitive impairment
- MMSE
- Mini Mental State Examination
- MoCA
- Montreal Cognitive Assessment
- OASys
- Offender Assessment System
- OHRN
- Offender Health Research Network
- PSSRU
- Personal Social Services Research Unit
- SPOC
- single point of contact
Notes
-
Participant information sheet for those who know prisoners considering taking part in interviews
-
Participant information sheet for prisoners considering taking part in observations
-
Consent form for those who know prisoners taking part in interviews
-
Offender Health Research Network and Prison and Offender Research in Social Care and Health circulatory e-mail
-
Participant consent form for individuals considering participating in the expert panels
-
Decision training description containing training components, definitions and associated theory
-
Cost of the dementia and mild cognitive impairment in prison care pathway elements
-
Estimation of the average annual cost of dementia medication
-
Costs of typical pathway for standard dementia care (vignettes 1–4)
-
Costs of typical pathway for standard mild cognitive impairment care (vignettes 7 and 8)
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/hsdr08270).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
